Introduction
In the coronavirus 2019 era, individuals who suffer
from headaches and neurologic deficits may have an increased risk
of developing acute cerebrovascular disease, particularly after
receiving the COVID-19 vaccine (1).
In a previous study performed in Mexico in May 2022 found that
patients vaccinated with the AstraZeneca-Oxford vaccine with
vaccination-induced immune thrombotic thrombocytopenia (VITT) were
more likely to be young females (aged 21 to 77 years), who were
administered the vaccine 5-14 days prior to the presentation of
symptoms (2). The patients' signs,
symptoms and imaging findings were consistent with those of
cerebral sinovenous thrombosis (CSVT), or with thrombosis of the
deep vein, lung and other sites. The laboratory findings of that
study revealed thrombocytopenia, low fibrinogen levels and elevated
D-dimer levels, while antibodies against platelet factor 4 were
positive in the majority of assays performed (2). However, it should be noted that
sometimes, in certain age groups of patients, these symptoms may be
associated with congenital vascular anomalies or drug abuse
(3,4). Carbon monoxide, viper envenomation,
methylenedioxymethamphetamine have been reported to lead to acute
cerebral venous thrombosis (5-7).
The present study described the case of a young male
who was a nitrous oxide (N2O) abuser with CSVT. The
patient had received the second dose of the AstraZeneca COVID-19
vaccine at ~1 month prior to his presentation to the emergency
department. His laboratory findings was not compatible with
VITT.
Case report
A 25-year-old male patient presented to the
Emergency Department of Tao-Yuan General Hospital (Taoyuan City,
Taiwan) with a severe headache and vertigo lasting for 3 days. He
had a history of recurrent pulmonary embolism without regular
medical follow-up and vitamin B12 deficiency due to N2O
abuse. He had no recent trauma history. He had been vaccinated with
the second dose of the AstraZeneca COVID-19 vaccine at ~1 month
prior to his admission.
Upon an examination of his vital signs, he was found
to have a body temperature of 36.4˚C, a pulse rate of 64
beats per minute, a respiratory rate of 18 breaths per minute and a
blood pressure of 119/68 mmHg. A neurological examination only
revealed left homonymous upper quadrantanopia. His serum white
blood cell count was 12.58x103/µl with a neutrophil
percentage of 68.7%, C-reactive protein level of 1.34 mg/l, a
platelet count of 361x103/µl and elevated D-dimer levels
(0.98 µg/ml). A provisional clinical diagnosis of acute
cerebrovascular accident was thus made.
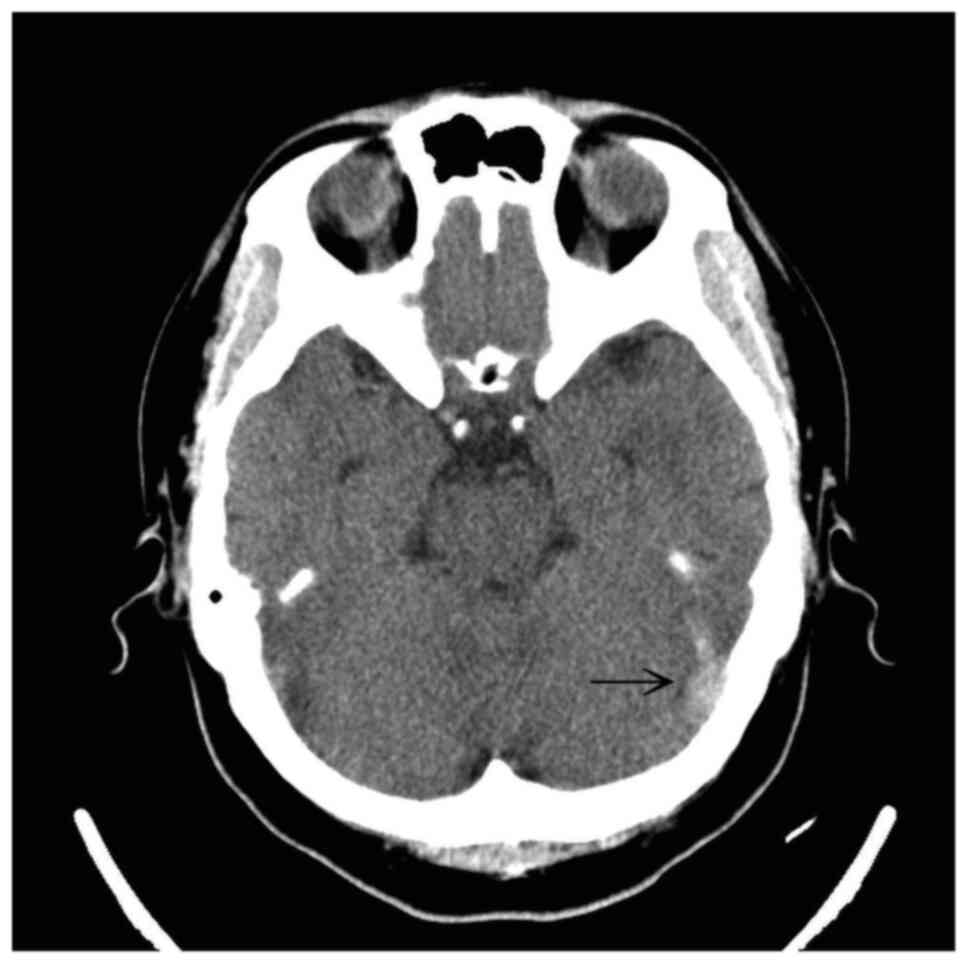
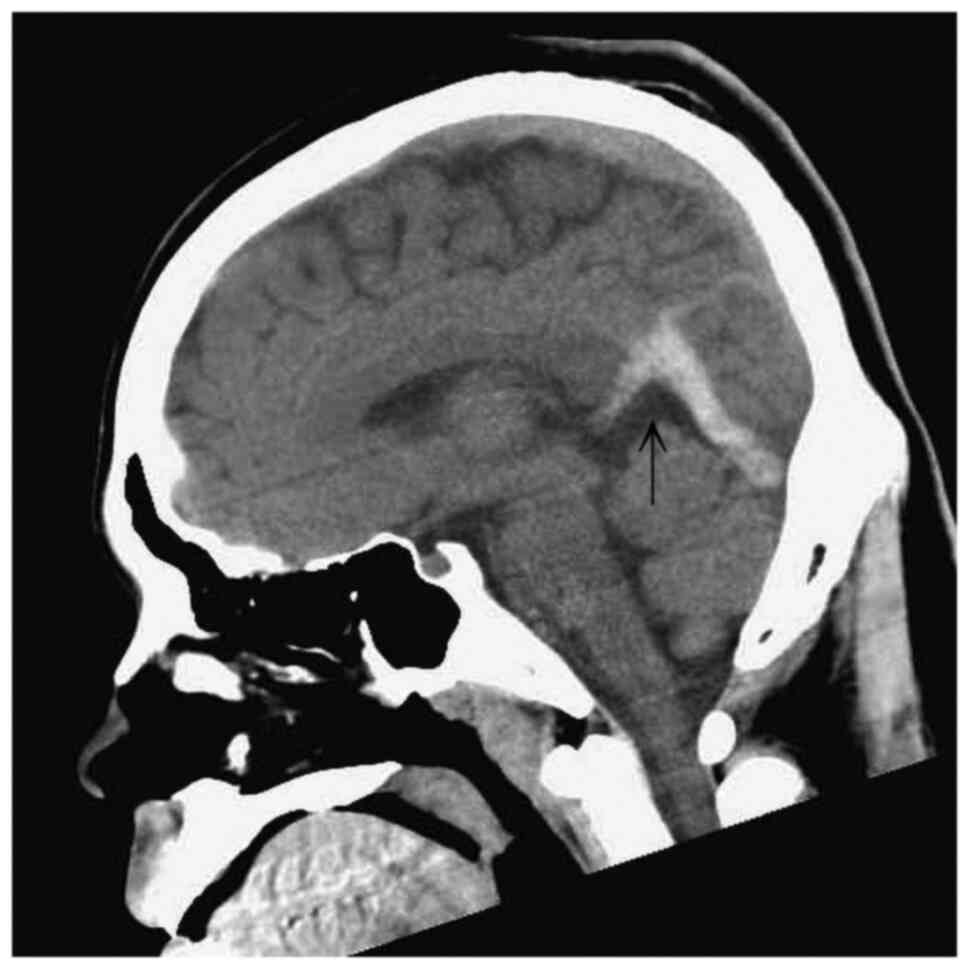
A computed tomography (CT) scan of the head revealed
an abnormal hyperattenuation in the straight sinus and bilateral
transverse sinuses (Figs. 1 and
2). A diagnosis of CSVT was made
following a consultation with a neurologist. The patient was
treated with enoxaparin at 6,000 IU, levetiracetam at 1,000 mg and
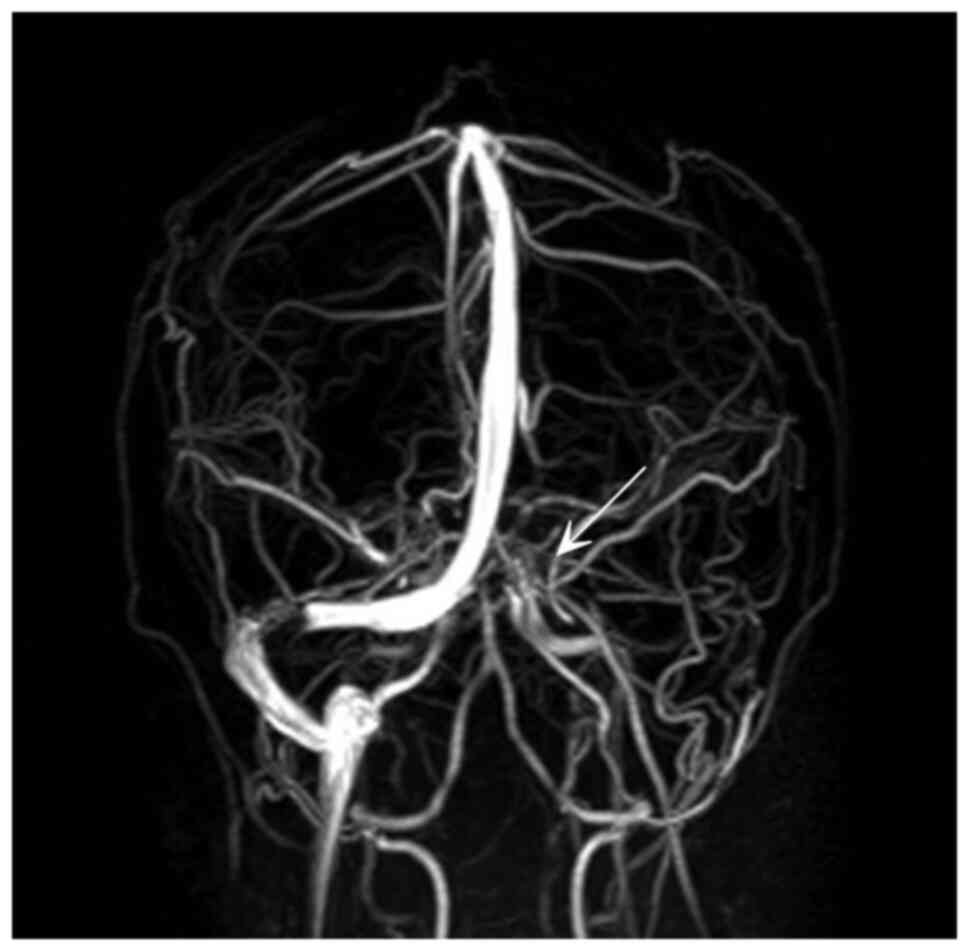
mannitol at 100 ml via an intravenous drip. Following admission, a
magnetic resonance venography revealed the absence of flow in the
straight sinus and bilateral transverse sinuses (Fig. 3). A thrombophilic investigation
revealed a plasma homocysteine level of 59.03 µmol/l (upper normal
limit, 15.39 µmol/l) and a vitamin B12 level of <148 (lower
normal limit, 187 pg/ml). The levels of protein C (70-140%),
protein S (60-130%) and antithrombin III (75-125%) were within the
normal range. CSVT secondary to homocystinemia was diagnosed, which
is an unusual, yet treatable condition.
The treatment administered included anticoagulation
and vitamin B12 supplementation. The patient was administered
vitamin B12 at 500 mcg twice per day, pyridoxine at 50 mg per day,
folic acid at 5 mg two times per day and edoxaban at 60 mg per day.
After 7 days of treatment, his headache and quadrantanopia were
improved, and the patient was discharged.
Discussion
N2O is a recreational inhalant which
exerts euphoric and hallucinatory effects and has recently become
popular among adolescents and young adults in Taiwan. Previous
studies have found several adverse effects related to the
dysfunction of vitamin B12 metabolism, such as macrocytic anemia,
peripheral neuropathy, skin hyperpigmentation, subacute combined
degeneration of the spinal cord, deep vein thrombosis, pulmonary
embolism, aortic thrombosis and bone marrow suppression. CSVT has
an estimated incidence of 3-4 per million adults and 7 per million
children per year, with a predominance among younger individuals
(8). N2O irreversibly
oxidizes the cobalt atom of vitamin B12 and inhibits the methionine
synthase, leading to an increased blood homocysteine level.
Hyperhomocysteinemia and vitamin B12 deficiency are considered as
risk factors for venous thrombosis (9-11).
During the COVID-19 era, post-vaccination cerebral
venous thrombosis is the most common manifestation of VITT. In
particularly, individuals who received the vaccine were found to
suffer from headache with the acute onset of neurological deficits
such as weakness, visual loss and hypotonia (1).
VITT commonly occurs at 7-10 days after the first
dose of the vaccine; however, in the patient described herein, it
occurred at 1 month after the second dose of the vaccine. The blood
test did not meet the diagnostic criteria for VITT (platelet count
<15x103/Ul and D-dimer levels >2 µg/ml); thus, the
consumption of N2O was considered the leading cause of
cerebral venous thrombosis rather than the COVID-19 vaccine
(12). The treatment of the patient
included anticoagulation and vitamin B12 supplementation (13). In the present study, the patient was
administered vitamin B12 at 500 mcg twice per day, pyridoxine at 50
mg per day, folic acid at 5 mg two times per day and edoxaban at 60
mg per day. After 7 days of treatment, his headache and
quadrantanopia were improved, and the patient was discharged.
Apart from CSVT, nitrous oxide can damage multiple
systems, particularly the nervous system; however, the exact
mechanisms of N2O-induced toxicity remain controversial.
The discontinuation of N2O use and the timely
supplementation of vitamin B12 are essential for a good prognosis
(14).
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SSL was involved in the writing of the manuscript
and in obtaining patient data. IWF was involved in obtaining
patient data and in the treatment of the patient. CYC was involved
in editing of the manuscript and in obtaining patient data. YJS was
involved in the writing and editing of the manuscript, in the
conception of the study and in the revision of the manuscript and
correspondence. SSL and IWF confirm the authenticity of all the raw
data. All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The patient provided written informed consent for
his participation in the present case report.
Patient consent for publication
The patient provided written informed consent for
his data to be published.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Qureshi MIA, Azam B, Waheed MA and Imran
A: Venous sinus thrombosis after the first dose of Pfizer BioNTech
vaccine. BMJ Case Rep. 15(e247493)2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ornelas-Aguirre JM, Gómez-Alcalá AV and
Ramírez-Leyva DH: Increment of D-dimer Associated with Immune
Thrombotic Thrombocytopenia in ChAdOx1 nCoV-19 Vaccinated
Individuals. Arch Med Res. 53:341–351. 2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Rasyid A, Mesiano T, Kurniawan M, Hidayat
R, Mulyadi R, Nugroho SW, Yolanda S, Wiyarta E and Harris S:
Spontaneous subarachnoid hemorrhage due to arteriovenous
malformation mimicking migraine: A case report. Radiol Case Rep.
17:790–793. 2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ohta K, Mori M, Yoritaka A, Okamoto K and
Kishida S: Delayed ischemic stroke associated with methamphetamine
use. J Emerg Med. 28:165–167. 2005.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Phinney TA, Gibb GJ and Laghari FJ: CO
poisoning as an associated risk factor for CVT. Am J Emerg Med.
36:1123.e1–1123.e3. 2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Senthilkumaran S, Balamurugan N and
Thirumalaikolandusubramanian P: Viper envenomation and cerebral
venous thrombosis. J Postgrad Med. 59:171–172. 2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Goldstein LH, Mordish Y, Abu-Kishak I,
Toledano M and Berkovitch M: Acute paralysis following recreational
MDMA (Ecstasy) use. Clin Toxicol (Phila). 44:339–341.
2006.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Alvis-Miranda HR, Milena Castellar-Leones
S, Alcala-Cerra G and Rafael Moscote-Salazar L: Cerebral Sinus
venous thrombosis. J Neurosci Rural Pract. 4:427–438.
2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Gatt A and Makris M: Hyperhomocysteinemia
and venous thrombosis. Semin Hematol. 44:70–76. 2007.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Farhat W, Pariente A and Mijahed R:
Extensive cerebral venous thrombosis secondary to recreational
nitrous oxide abuse. Cerebrovasc Dis. 51:114–117. 2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
de Valck L, Defelippe VM and Bouwman NAMG:
Cerebral venous sinus thrombosis: A complication of nitrous oxide
abuse. BMJ Case Rep. 14(e244478)2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Perry RJ, Tamborska A, Singh B, Craven B,
Marigold R, Arthur-Farraj P, Yeo JM, Zhang L, Hassan-Smith G, Jones
M, et al: Cerebral venous thrombosis after vaccination against
COVID-19 in the UK: A multicentre cohort study. Lancet.
398:1147–1156. 2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Pratt DN, Patterson KC and Quin K: Venous
thrombosis after nitrous oxide abuse, a case report. J Thromb
Thrombolysis. 49:501–503. 2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Xiang Y, Li L, Ma X, Li S, Xue Y, Yan P,
Chen M and Wu J: Recreational nitrous oxide abuse: Prevalence,
neurotoxicity, and treatment. Neurotox Res. 39:975–985.
2021.PubMed/NCBI View Article : Google Scholar
|