Introduction
The ectopic ossification of the posterior
longitudinal ligament (OPLL) represents a localized form of
skeletal hyperostosis. Its annual incidence is as high as 3 and
1.3% for Asian and non-Asian populations, respectively (1). It frequently involves the cervical and
thoracic spine to a lesser extent.
The nature of this chronic disease is generally
benign. OPLL is commonly associated with significant stenosis of
the spinal canal. The majority of patients present with myelopathy
in the fifth and sixth decades of life. During the disease, up to
17% of the cases require some form of assistance in the activities
of daily living. Patients are at an increased risk of developing
quadriparesis following cervical spine trauma, reaching as high as
15% (1).
The present study describes the case of an
asymptomatic patient with OPLL who developed quadriparesis and
respiratory insufficiency following minor head trauma. The patient
succumbed shortly afterwards due to a respiratory infection.
Case report
During hospitalization for a urinary tract
infection, a 50-year-old obese male with ankylosing spondylitis
(AS), Scheuermann's kyphosis (KS) and a body mass index of 42.4,
lost consciousness and suffered a minor head injury at the
occipital region. The immediate clinical examination revealed that
the patient was hemodynamically stable (85 bpm and 123/85 mmHg) and
febrile (39˚C) (from a urinary tract infection with pyospheres; a
urine culture was positive for Escherichia. coli); he had
sufficient respiration (SAO2, 97%). After 1-2 min, the
patient regained consciousness but exhibit no contraction (0/5) in
all key muscle groups and sensory paralysis during the neurological
examination (ASIA A). A head computed tomography (CT) scan revealed
no evidence of intracranial hemorrhage or other intracranial
pathology and his Glasgow Coma Scale (GCS) score was 15/15.
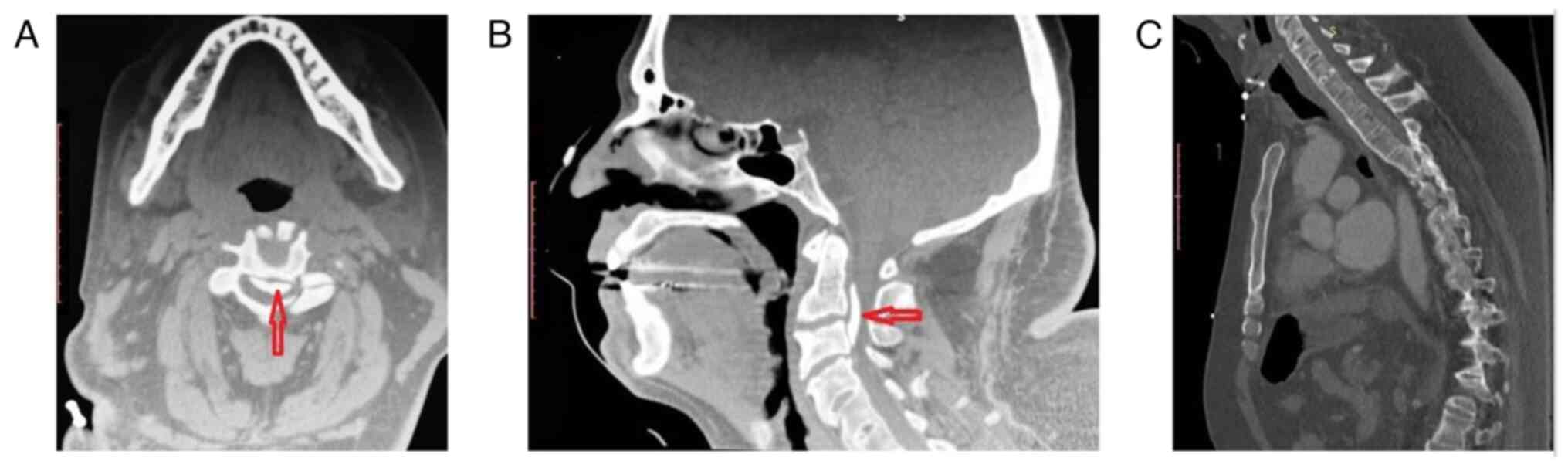
However, the CT scan of the cervical spine revealed an OPLL
associated with severe spinal canal stenosis (canal diameter, 4.18
mm) and extensive anterior ankylosis (Fig. 1). After 30 min, the patient developed
respiratory distress and was intubated using fiberoptic
technology.
At that time, the patient was transferred to the
University Hospital of Larissa (Larissa, Greece) with a cervical
rigid collar. In the operating room, he underwent posterior
cervical spine decompression with a laminectomy extending from C2
to C4. Following surgery, the patient was awakened and transferred
to the intensive care unit for further cardiopulmonary support. The
patient remained quadriplegic, with a minor improvement in the
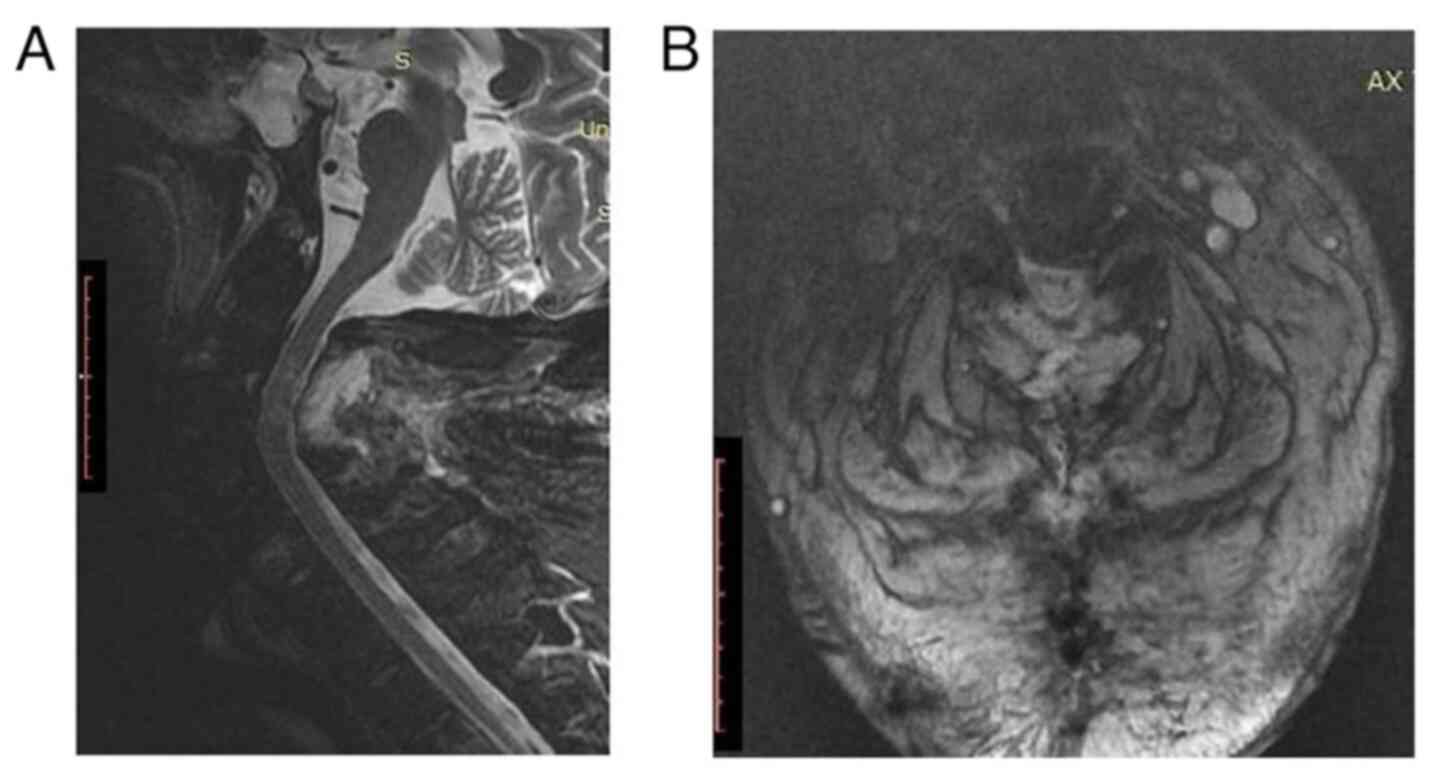
deltoid muscles (1/5). The post-operative magnetic resonance
imaging scan documented the adequacy of decompression (Fig. 2). Additionally, it revealed a spinal
cord with an increased signal intensity, compatible with edema. On
the 6th day, the patient suffered a cardiac arrest, which he
survived following half an hour of cardiopulmonary resuscitation.
Moreover, a cardiac pacemaker was inserted to avoid future
episodes. On the 11th day, the patient developed an acute abdomen
following gastrostomy tube placement, for which he underwent an
exploratory laparotomy. On the following day, the patient suffered
a massive pulmonary embolism despite adequate anticoagulation and
finally succumbed.
Discussion
Even though trauma to the cervical spine in patients
with OPLL is common, to the best of our knowledge, this is the
first reported case of an extensive osteophyte with a lethal
outcome after a syncope (1,2). The most common presentation of OPLL is
cervical myelopathy from the chronic narrowing of the spinal canal,
followed by quadriparesis precipitated by trauma (1-4).
The association between the OPLL and syncope is not
clear. Several pathogenetic mechanisms could be implicated. A
vasogenic origin cannot be excluded following the compression of
the anterior spinal arteries and blood stagnation in the
vertebrobasilar system. It is unclear whether vertigo caused by
vascular changes at the vertebrobasilar circulation causes syncope
(5). Moreover, a neurogenic
mechanism could be considered after an acute compression of the
vagal and glossopharyngeal nuclei in the higher cervical region
with parasympathetic over-discharge (5). Finally, the patient may have simply
lost consciousness due to a hypotensive episode during an acute
urinary tract infection or a latent arrhythmia.
In the present study, pre-operative imaging revealed
an OPLL at the C1, C2, and C3 vertebral levels, corresponding to a
continuous ossification based on the relevant classification
pattern (1). Of note, two additional
findings are worth noting, including a marked canal narrowing at
the levels corresponding to the canal compromise and ankylosis of
the subaxial spine compatible with AS (1,3). The
co-existence of AS, KS and OPLL is infrequent, but both have been
associated with human leukocyte antigen variants (1,3).
Symptomatic cases are usually treated surgically
(1-3).
Anterior procedures aim to remove the ossified ligament and
directly decompress the spinal canal, but with a high risk of
unintended durotomy (1-3). On
the other hand, posterior approaches decompress the spinal canal
indirectly (1,2). In the case presented herein, the
posterior approach was preferred based on the level of the lesion
and the curvature of the cervical spine. The K-line, a virtual line
between the midpoints of the anteroposterior canal diameter at C2
and C7, fell behind the osteophyte, necessitating a posterior
approach (6).
Studies have reported the association between
obesity and hyperostosis situations resembling OPLL and diffuse
idiopathic skeletal hyperostosis, where the mechanism of enormous
cumulatively formed osteophytes remains unclear (7,8).
However, the underlying mechanism may be connected with
insulin-resistant states, and the surplus adipose tissue via
mechanical, hormonal, and cytokine factors leads to bone
upregulation (9,10).
In conclusion, OPLL is a rare disease that usually
manifests with cervical myelopathy. In rare occasions, it may
present with syncope and potentially lethal outcomes, particularly
when precipitated by trauma. Therefore, the management of OPLL with
marked canal stenosis should not be unnecessarily delayed. Further
studies are required for the validation of the findings presented
herein.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
AGB and GF conceptualized the study. VEG, PS and NT
advised on patient treatment, wrote and prepared the draft of the
manuscript, and made a substantial contribution to the analysis of
the patient's data. AGB and GF analyzed the patient patient's data
and provided critical revisions. AGB and GF confirm the
authenticity of all the raw data. All authors contributed to
manuscript revision, and have read and approved the final version
of the manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient for his participation in the present case report.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of the present case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Matsunaga S and Sakou T: Ossification of
the posterior longitudinal ligament of the cervical spine: Etiology
and natural history. Spine (Phila Pa 1976). 37:E309–E314.
2012.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Head J, Rymarczuk G, Stricsek G,
Velagapudi L, Maulucci C, Hoelscher C and Harrop J: Ossification of
the posterior longitudinal ligament: Surgical approaches and
associated complications. Neurospine. 16:517–529. 2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Abiola R, Rubery P and Mesfin A:
Ossification of the posterior longitudinal ligament: Etiology,
diagnosis, and outcomes of nonoperative and operative management.
Global Spine J. 6:195–204. 2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hirai T, Yoshii T, Ushio S, Mori K, Maki
S, Katsumi K, Nagoshi N, Takeuchi K, Furuya T, Watanabe K, et al:
Clinical characteristics in patients with ossification of the
posterior longitudinal ligament: A prospective multi-institutional
cross-sectional study. Sci Rep. 10(5532)2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Verma SK, Yaseen M, Bharadwaj V and Pasha
A: Syncope: A rare presentation of Cervical spondylosis. IOSR J
Dent Med Sci. 13:90–92. 2014.
|
|
6
|
Ijima Y, Furuya T, Ota M, Maki S, Saito J,
Kitamura M, Miyamoto T, Ohtori S, Orita S, Inage K, et al: The
K-line in the cervical ossification of the posterior longitudinal
ligament is different on plain radiographs and CT images. J Spine
Surg. 4:403–407. 2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Wu JC, Liu L, Chen YC, Huang WC, Chen TJ
and Cheng H: Ossification of the posterior longitudinal ligament in
the cervical spine: An 11-year comprehensive national epidemiology
study. Neurosurg Focus. 30(E5)2011.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Wang PN, Chen SS, Liu HC, Fuh JL, Kuo BI
and Wang SJ: Ossification of the posterior longitudinal ligament of
the spine. A case-control risk factor study. Spine (Phila Pa 1976).
24:142–144. 1999.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Inamasu J, Guiot BH and Sachs DC:
Ossification of the posterior longitudinal ligament: An update on
its biology, epidemiology, and natural history. Neurosurgery.
58:1027–1039. 2006.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Harvey AE, Lashinger LM and Hursting SD:
The growing challenge of obesity and cancer: An inflammatory issue.
Ann N Y Acad Sci. 1229:45–52. 2011.PubMed/NCBI View Article : Google Scholar
|