1. Introduction
The level of preparedness of the scientific
community for the next pandemic remains a critical concern. The
ways in which the international scientific community can contribute
to minimizing the public health impact of a new pandemic require
careful consideration. The evaluation of the recent coronavirus
disease 2019 (COVID-19) pandemic is indeed crucial (1-6).
Belonging to the broad family of coronaviruses, a well-known family
of viruses to the paediatric population, severe acute respiratory
syndrome coronavirus 2 (SARS-CoV-2), a positive-sense
single-stranded RNA (+ssRNA) virus, emerged as one of the most
dangerous pathogens in human history (2). The simple structure of the virus,
typical of RNA viruses, such as influenza viruses, human
immunodeficiency virus (HIV) and cancer-associated viruses,
hindered the ability of the immune system to identify its invasion
(2,7). In addition, global genetic variations
influenced morbidity and mortality rates related to
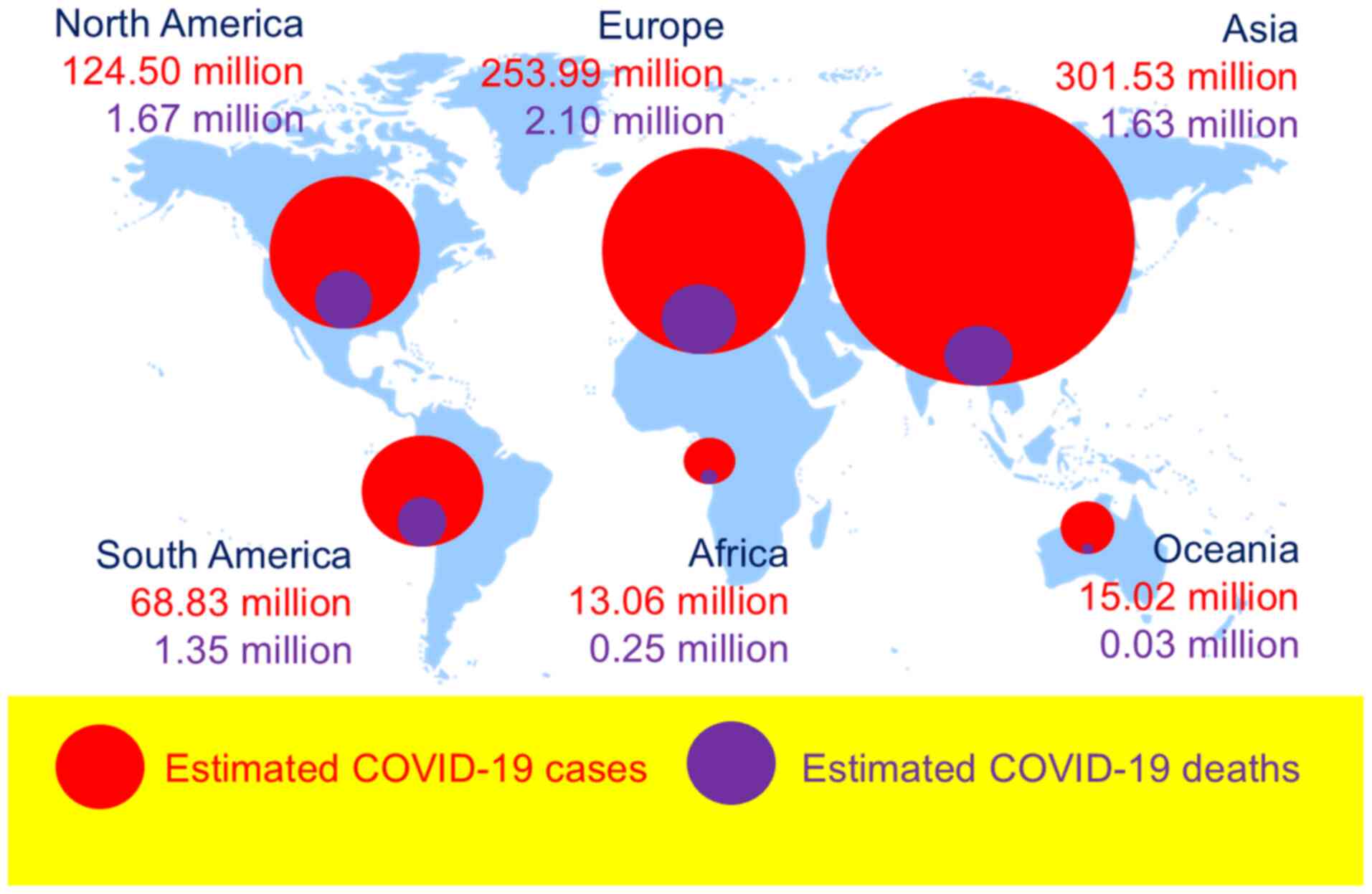
COVID-19(2). The global distribution
of SARS-CoV-2, which since the end of 2019 spread immediately
around the globe, causing an enormous health and economic
catastrophe (https://ourworldindata.org/grapher/cumulative-covid-cases-region
and https://ourworldindata.org/grapher/cumulative-covid-deaths-region)
is presented in Fig. 1.
From the very beginning of the pandemic, there was a
critical need to develop secure, reliable and effective vaccines
and therapeutic agents against SARS-CoV-2 (2,8).
Lockdown and social distancing significantly influenced social and
behavioral aspects of human life. Concurrently, COVID-19 affected
the prevalence of other diseases, including cardiovascular diseases
and cancer, while in tropical and subtropical areas of the world,
COVID-19 lockdown resulted in a significant reduction in the rates
of other infections, such as the Dengue fever (9). The mutations of SARS-CoV-2 resulted in
the continuing emergence of new COVID-19 cases in all age groups,
including children, for several months (7). SARS-CoV-2 infection remains prevalent,
while efforts to fund research on COVID-19 have continued to the
present day. Research has also focused on post-COVID-19 syndrome
and its management (10).
Medical advances and improvements, as well as
management limitations, weaknesses and challenges, encountered
during the COVID-19 pandemic, require an up-to-date evaluation. In
addition to the medical aspects of the pandemic and issues
pertaining to strategic preparedness and response planning
(1-5),
it is also important to systematically analyze non-medical issues,
including politics and science communication. The lessons derived
from this evaluation will help the prioritisation of research and
strategic planning in the event of a future pandemic. Moreover,
this analysis will guide the development of up-to-date educational
programs to be integrated in both undergraduate and postgraduate
medical training, worldwide.
The purpose of the present review article is to
summarize the key messages on the lessons learnt from the recent
COVID-19 pandemic, one of the most critical and disruptive events
of modern times. The main topics on COVID-19 that are discussed
herein are: i) Advances in intensive medicine during the COVID-19
pandemic, focusing on high flow nasal oxygen therapy (HFNOT); ii)
COVID-19 and politics; and iii) COVID-19 and science communication
(Table I).
 | Table IKey lessons from the COVID-19
pandemic: The role of intensive care, politics and science
communication. |
Table I
Key lessons from the COVID-19
pandemic: The role of intensive care, politics and science
communication.
| Topic | Main points and
take-home messages (Refs.) |
|---|
| COVID-19 and
intensive care medicine | HFNOT is a
relatively novel technique for delivering warm, humidified oxygen
at high flow rates to patients with acute hypoxaemic respiratory
failure, including COVID-19 cases (11-32). |
| | HFNOT is supported
by strong physiological evidence; HFNOT has been shown to improve
oxygenation, reduce the work of breathing and enhance lung function
(12-15). |
| | During the recent
COVID-19 pandemic, HFNOT has been increasingly used in ICU and PICU
patients due to its effectiveness and particularly its tolerability
(27-32). |
| | Meta-analyses on
the use of HFNOT in acute hypoxaemic respiratory failure and
COVID-19 infection have generally shown that HFNOT is more
effective than COT in reducing the need for higher respiratory
support and comparable to NIV (27-30). |
| | HFNOT can be
applied in the early management of hypoxemia and respiratory
distress in children admitted to the PICU (23-26,31,32). |
| COVID-19 and
politics | The COVID-19
pandemic highlighted the deep interactions between science,
society, and politics; the rapid development of vaccines was a
significant scientific achievement, driven by the collaboration of
scientists, governments and international organizations (33-47). |
| | Despite various
international efforts, inequalities in vaccine access underscored
the economic and geopolitical aspects of the COVID-19 pandemic
(41). |
| | Politics played a
crucial role in managing the pandemic, with decisions regarding
lockdowns and vaccination programs often influenced by political
calculations, such as economic stability and social pressure,
rather than solely by scientific data (33-47). |
| | The conflict
between science and politics, as well as misinformation, undermined
public trust and complicated the implementation of necessary
measures (44). |
| | The need for
political focus on the updated training of healthcare professionals
was another key message from the recent COVID-19 pandemic (45-47). |
| COVID-19 and
science communication | During the COVID-19
pandemic, frontline researchers around the globe, along with their
official institutions and scientific societies, had the principal
role in transparently communicating information about SARS-CoV-2 to
the public (50-62). |
| | However, throughout
the pandemic, non-specialist scientists and others also assumed a
key role in public communication, while an unprecedented surge of
information, disinformation and misinfor- mation about SARS-CoV-2
was spread especially via the social media platforms (52-54). |
| | Science
communication on COVID-19 was another example that required
multidisciplinary collaboration with communication experts leading
to the urgent development and usage of innovative communication
strategies (50-62). |
| | The post-COVID-19
pandemic period provides a valuable opportunity to evaluate the
relationship between science communication and society to improve
the preparedness of the international scientific community for the
next pandemic (61,62). |
2. High flow nasal oxygen therapy: Not just
another oxygen delivering modality
During the recent COVID-19 pandemic, intensive care
medicine came to the forefront of the fight against SARS-CoV-2.
Thus far, the learning experience has been intense and has affected
every aspect of this medical specialty, from therapeutic tools to
management strategies and protocols. HFNOT is a relatively novel
method for delivering warm humidified oxygen at high flows to
patients with acute hypoxaemic respiratory failure (11). The interest in HFNOT and its
potential has been further increased during the COVID-19 pandemic,
which imposed significant demands on hospital resources,
necessitating prudent patient prioritization and careful allocation
of respiratory care equipment and intensive care unit (ICU) beds
(12).
The HFNOT system setup is simple: It requires only a
flow generator, an active heated humidifier, a single heated
circuit with a servo-controlled heating wire, and a silicone nasal
cannula (11). HFNOT has emerged as
an effective and well-tolerated respiratory support technique in
various clinical scenarios, although the optimal method for
managing acute hypoxaemic respiratory failure remains under debate.
Physiological studies have demonstrated that HFNOT, apart from
being an effective oxygenator, reduces the work of breathing and
respiratory resistance, increases positive end-expiratory pressure
and end-inspiratory lung volume, washes off anatomic dead space and
improves secretion clearance (12).
A common practice is to start HFNOT with a fraction of inspired
oxygen (FiO2) of 100% and a flow of 60 l/min and then
adjust FiO2 and the flow to achieve an oxygen saturation
(SpO2) >88-90% and an age-appropriate respiratory
rate (RR) (13). A ROX index
(calculated as the SpO2/FiO2 ratio divided by
the RR of the patient) >4.88 at 12 h has a high positive
predictive value (89.4%) in predicting treatment success (14). The only absolute contraindication for
HFNOT is any indication for invasive mechanical ventilation
including shock, respiratory and cardiac arrest, bradycardia,
severe arrhythmias and an impaired level of consciousness. Facial
erythema, skin breakdown and barotrauma may occur in HFNOT users,
although these represent less common complications compared with
non-invasive ventilation (NIV). Overall, HFNOT is better tolerated
than NIV (15).
Prior to the COVID-19 era, Hernández et al
(16,17) demonstrated that HFNOT compared with
conventional oxygen therapy (COT) decreases the risk of
reintubation and post-extubation respiratory failure in ‘low-risk’
ICU patients, while in ‘high-risk’ patients HFNOT was not inferior
to NIV in averting reintubation and post-extubation respiratory
failure. However, neither of these two studies (16,17)
noted any benefit in terms of mortality rates. In a meta-analysis
by Zhu et al (18) that
followed, HFNOT reduced the risk of post-extubation respiratory
failure, improved oxygenation and reduced respiratory rates in
post-extubated ICU patients. Moreover, in another meta-analysis by
Granton et al (19), HFNOT
reduced re-intubation rates compared with COT, but not when
compared with NIV. However, other researchers have failed to
duplicate these findings (20).
Thus, in another meta-analysis by Maitra et al (21) comparing HFNOT with NIV and COT in
patients with acute hypoxaemic respiratory failure, no benefit was
shown for HFNOT in decreasing requirements for higher respiratory
support. Nevertheless, more recently Seow et al (22) reviewed a total of 63 studies
[including 23 randomized controlled trials (RCTs)], which compared
HFNOT with COT and showed that HFNOT decreased the risk for
escalating to NIV or invasive respiratory support. In the
paediatric population, several RCTs have suggested that compared
with COT, HFNOT reduced the rates of intubation and mechanical
ventilation in children with moderate-to-severe bronchiolitis and
hypoxaemic respiratory failure (23-26).
HFNOT is a growing respiratory treatment for children, particularly
for those with respiratory distress, bronchiolitis, or other
respiratory illnesses.
Focusing on acute hypoxaemic respiratory failure in
patients with COVID-19, a meta-analysis of 40 studies including two
RCTs by Arruda et al (27),
suggested that HFNOT reduced the risk of intubation compared with
COT, but showed no additional benefit when compared with NIV. In
another meta-analysis by Li et al (28), again focusing on patients with
COVID-19, HFNOT was demonstrated to reduce the rate of intubation,
28-day mortality and ventilator-free days compared with COT.
However, these results were not reproduced by a recent
meta-analysis by Pisciotta et al (29) involving patients with
COVID-19-induced hypoxaemic respiratory failure, which showed no
benefit in terms of treatment failure for HFNOT compared with NIV
and COT.
Recent guidelines issued by the European Respiratory
Society (ERS) suggest HFNOT over NIV or COT for the management of
acute hypoxaemic respiratory failure. However, although they favor
HFNOT over COT for post-extubated ICU patients with ‘low-’ or
‘moderate-risk’ for re-intubation, they suggest NIV over HFNOT for
‘high-risk’ patients (30). During
the COVID-19 pandemic, HFNC was also widely applied in the early
management of hypoxemia and respiratory distress in children with
COVID-19 requiring paediatric intensive care (31,32).
3. COVID-19 and politics: Challenges,
dilemmas and lessons
Politics was one of the most significant,
non-medical issues of the recent COVID-19 pandemic, which
demonstrated the interactions between science, society and politics
(33). Since the onset of this
unprecedented global health challenge, numerous countries designed
and implemented various and controversial policies against
SARS-CoV-2(34). For example, the
‘zero-COVID-19 policy’, which was adopted by China as well as other
countries, tried strictly to eliminate local transmission of the
virus (35-37).
On the other hand, the ‘Swedish COVID-19 approach’, which did not
enforce strict lockdown measures, was based on voluntary
recommendations and guidelines (38). Concurrently, Latin American countries
appeared to struggle with implementing specific COVID-19 pandemic
policies for their citizens (39).
Politics influenced the development, distribution
and access of vaccines and therapeutic agents against SARS-CoV-2,
as well as public health management and social reaction. The
accomplishment of this task would not have been possible without
the close collaboration between scientists, scientific institutions
and governments. Funding through state resources and support from
international organizations, such as the World Health Organization
(WHO), also played a fundamental role (40).
Although the scientific society responded promptly
by developing and approving novel vaccines and therapeutic agents
against SARS-CoV-2, the global community faced deep inequalities in
their access. For example, the European Union countries, including
Greece, succeeded in achieving timely access to a sufficient amount
of vaccine doses against SARS-CoV-2(2). The European Union prioritized the
introduction of vaccination programs against SARS-CoV-2 as its
principal political strategy against COVID-19 (https://health.ec.europa.eu/vaccination/overview_en).
Developed countries gained privileged access to the first batches
of vaccines, securing deals with pharmaceutical companies long
before their release (41). The
European Union countries responded quickly and prioritized
solidarity in order to provide access to vaccines against
SARS-CoV-2 to all the European citizens (https://commission.europa.eu/strategy-and-policy/coronavirus-response/coronavirus-european-solidarity-action_en).
Moreover, international efforts, such as the global initiative
COVAX, co-led by Gavi, the Vaccine Alliance, the Coalition for
Epidemic Preparedness Innovations (CEPI), the WHO and UNICEF,
sought to ensure equitable distribution of vaccines to developed
and developing countries (41).
However, all these efforts failed to meet their goals adequately.
‘Vaccine nationalism’ prominently affected the allocation of
resources, as numerous governments chose to secure the needs of
their populations neglecting international commitments. ‘Vaccine
diplomacy’, as a political tool for foreign policy and
international influence was also used as leverage to promote
political and economic interests. These inequalities highlighted
the gap between rich and poor countries and raised ethical and
practical issues that may resonate and affect healthcare management
of future crises.
The pandemic exposed the reciprocal relationship
between politics and public health (42-44).
Political leaders worldwide were challenged to make decisions that
directly affected the spread of the virus, healthcare provision and
the public perception of the pandemic. In numerous countries,
decisions to impose lockdowns or lift restrictions were based on
political calculations, such as the need to stabilize the economy
or to respond to social pressure, rather than solely on scientific
data and advice. The conflict between science and politics proved
particularly harmful in cases where politicians downplayed the
threat of the pandemic or spread misinformation, as witnessed in
some countries with strong populist movements. These decisions
undermined public trust in scientific authorities and challenged
the implementation of necessary health measures. In several
countries, political polarization and misinformation about vaccine
safety increased vaccine hesitancy (45).
The need for updated training of healthcare
professionals was another clear message from the recent COVID-19
pandemic (46,47). Political fora are expected to support
the adjustment of medical educational programs to new realities and
organize targeted actions involving the institutions responsible
for providing ongoing medical education. Continuing medical
education is critical as this could promote the value of medical
education in paediatric viral infections as well, including
COVID-19 (48,49). If the next pandemic disproportionally
affects the paediatric population, this effort will play a key role
for the preparedness of the paediatric personnel and healthcare
system of each country.
For the post-COVID-19 era, long-term policies are
required to prepare humanity for future health crises. The
international community must ensure equal access to vaccines and
therapeutic agents, regardless of the economic strength of a
country. Governments need to collaborate with international
organizations and the private sector to create a more resilient
global public health system that can respond quickly and
effectively to new threats and challenges (47). Our experience from the COVID-19
pandemic has taught us that health cannot be separated from
politics and that protecting human life should be the highest
priority, beyond economic or political calculations.
4. COVID-19 and science communication
Science communication-is a highly demanding process,
which deals with complex information, dynamic uncertainty and
diverse audiences, with varying educational levels, cultural
beliefs, attitudes and behaviours, that impact the understanding of
science (50). Effective science
communication is now established as an important tool that provides
accurate scientific knowledge to the public and helps them identify
false information. Ineffective communication, on the other hand,
can be detrimental to both science and society in general.
During the recent COVID-19 pandemic, science
communication demonstrated its critical influence on public health.
Since the beginning of the COVID-19 pandemic threat, healthcare
professionals strived to translate science and communicate its
ongoing findings in a timely and accessible manner to various
audiences (51). Frontline
researchers, alongside organizations such as the WHO, played the
principal role to transparently communicate their findings and
explain them to the public in a meaningful and understandable way.
There was an unprecedented demand for scientific knowledge; in
fact, the overwhelming requests from journalists for
epidemiological and research updates threatened to shift focus and
resources from viral research to media demands.
However, throughout the pandemic, non-specialist
scientists, academics, journalists, and others played a key role in
the communication of SARS-CoV-2 and COVID-19 advances,
recommendations and challenges. Despite newspapers and press
websites typically being reliable sources, the COVID-19 pandemic
witnessed an unparalleled surge of both accurate and inaccurate
information, largely spread via digital channels and platforms,
such as Twitter/X, Facebook, Instagram and TikTok (52-54).
Official scientific institutions and societies had to address
issues, such as ‘fake news’ and uncertainty, the latter being a
typical characteristic of scientific research, which was however
misinterpreted and perceived as inaccuracy or even unreliability.
Misinformation and disinformation regarding COVID-19 vaccine safety
were strongly related to increased vaccine hesitancy (55-57).
Science communication with the aid of reliable and
accessible official social media platforms was also encouraged
(58). Innovative new communication
strategies were proposed and used, including social media and
podcasts (59). These tools were
more effective at targeting specific audiences, such as adolescents
and the young population. Science communication on COVID-19
pandemic required multidisciplinary scientific collaboration.
Collaboration with visual communicators and design experts produced
digital illustrations and demonstrations of SARS-CoV-2, which
improved the understanding of the virus and health safety measures
and improved vaccine confidence (60).
The post COVID-19 era offers a chance to assess the
social impact of science communication and improve its future
effectiveness. Researchers and scientific institutions need to
design and develop novel communication strategies in order to
respond effectively to future potential crises. Scientists with
communication skills, passion and training should be motivated.
Moreover, scientific societies should create improved links with
the media and ensure that healthcare journalists are well informed
and trained. Despite its devastating health, social, and financial
ramifications, the COVID-19 pandemic presents a genuine opportunity
to improve pandemic preparedness (61,62).
5. Conclusions
Pandemic evaluation and planning perspectives
towards future infectious threats remain challenging. HFNOT, a
non-invasive ventilation modality increasingly used prior to the
COVID-19 era in both ward-based and critical care management of
respiratory failure (11-25),
represents an excellent clinical example of how the COVD-19
pandemic enriched medical knowledge and experience (26-32).
The medical experience gained from the treatment of critically ill
patients with COVID-19, should be further evaluated for the
establishment of state-of-the-art, evidence-based medical
consensuses and protocols. These tools are essential for the
effective and precise management of adults and paediatric patients
and should be integrated in current clinical practice.
The COVID-19 pandemic was a pivotal moment for
global health and politics (33-47).
The collaboration between science and politics contributed to the
rapid development of vaccines and therapeutic agents against
SARS-CoV-2, however global distribution was uneven due to national
policies and geopolitical tensions. Different political agendas
influenced not only the distribution of vaccines but also the
public perception of their safety and efficacy. Therefore, the
international community must be taught from these errors and work
towards a more equitable and resilient approach to future health
crises. Public health safety necessitates collaboration and
impartiality, prioritizing global solidarity and equality above
national and political agendas. Political decisions focusing on
increasing the financial health resources in primary health care
and advancing secondary and tertiary hospital-based care should be
encouraged. Health policies should also focus on enhancing
specialized as well as continuing medical education (46-49).
Science communication also demonstrated its
potential usefulness and effectiveness during the recent pandemic
(50-62).
This burgeoning scientific discipline should be further developed
and integrated into both undergraduate and postgraduate medical
education. Health professionals must develop effective
communication skills and become adept in providing accurate and
useful information to their patients and the general population, as
well. In the unfortunate event of a future pandemic, effective
science communication will depend on multi-disciplinary
collaboration between clinical and research scientists and
communication experts; this task requires improved digital tools
and innovative strategies to address public misinformation and
disinformation.
The aim of the present review article was to
stimulate further discussion within the international scientific
community on the evaluation of the management of the recent
COVID-19 pandemic. A careful interpretation of the lessons learned
may help promote strategic planning and preparedness, and advance
public health, translational research and future medicine.
Acknowledgements
This article is published in the context of the
‘10th Workshop on Paediatric Virology’, organized on November 9,
2024 by the Institute of Paediatric Virology (IPV, https://www.paediatricvirology.org), which is
based on the island of Euboea in Greece. The authors would like to
thank Professor Anna Kramvis, Professor Emerita of Virology at the
Department of Internal Medicine at the University of the
Witwatersrand in Johannesburg, South Africa and Member of the
Academic Advisory Board of the IPV for her valuable comments,
corrections and feedback. The authors would also like to thank Ms.
Aikaterini Kalaitzoglou, Parliamentary Associate, as well as all
members of the Paediatric Virology Study Group (PVSG) and the IPV
for their valuable contribution in the preparation of the
manuscript.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
All authors (INM, MA, AK, CK, AP, SBD, MT, and DAS)
contributed equally to the conception and design of this
manuscript, wrote the original draft, edited and critically revised
the manuscript. All authors have read and approved the final
manuscript. Data authentication is not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
World Health Organization: COVID-19
strategic preparedness and response plan: Operational planning
guidelines to support country preparedness and response. Geneva:
World Health Organization, 2020.
|
|
2
|
Zoumpourlis V, Goulielmaki M, Rizos E,
Baliou S and Spandidos DA: The COVID-19 pandemic as a scientific
and social challenge in the 21st century. Mol Med Rep.
22:2035–3048. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Jentsch PC, Anand M and Bauch CT:
Prioritising COVID-19 vaccination in changing social and
epidemiological landscapes: A mathematical modelling study. Lancet
Infect Dis. 21:1097–1106. 2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
O'Callaghan C, Cloutman-Green E and
Brierley J: Pandemic preparedness: Is the UK ready for a pandemic
that affects children? BMJ. 383(2804)2023.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Qin Z, Sun Y, Zhang J, Zhou L, Chen Y and
Huang C: Lessons from SARS-CoV-2 and its variants (review). Mol Med
Rep. 26(263)2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Quinn GA, Connolly R, ÓhAiseadha C, Hynds
P, Bagus P, Brown RB, Cáceres CF, Craig C, Connolly M, Domingo JL,
et al: What lessons can be learned from the management of the
COVID-19 pandemic? Int J Public Health. 70(1607727)2025.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Markiewicz L, Drazkowska K and Sikorski
PJ: Tricks and threats of RNA viruses-towards understanding the
fate of viral RNA. RNA Biol. 18:669–687. 2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Singh M, Jayant K, Singh D, Bhutani S,
Poddar NK, Chaudhary AA, Khan SU, Adnan M, Siddiqui AJ, Hassan MI,
et al: Withania somnifera (L.) Dunal (Ashwagandha) for the possible
therapeutics and clinical management of SARS-CoV-2 infection:
Plant-based drug discovery and targeted therapy. Front Cell Infect
Microbiol. 12(933824)2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Sharma H, Ilyas A, Chowdhury A, Poddar NK,
Chaudhary AA, Shilbayeh SAR, Ibrahim AA and Khan S: Does COVID-19
lockdowns have impacted on global dengue burden? A special focus to
India. BMC Public Health. 22(1402)2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
No authors listed: Post-COVID-19 Condition
Treatment and Management Rapid Scoping Review: Scoping review.
CADTH Health Technology Review. Canadian Agency for Drugs and
Technologies in Health, Ottawa, ON, 2022.
|
|
11
|
Nishimura M: High-flow nasal cannula
oxygen therapy devices. Respir Care. 64:735–742. 2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Crimi C, Pierucci P, Renda T, Pisani L and
Carlucci A: High-flow nasal cannula and COVID-19: A clinical
review. Respir Care. 67:227–240. 2022.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Ischaki E, Pantazopoulos I and Zakynthinos
S: Nasal high flow therapy: A novel treatment rather than a more
expensive oxygen device. Eur Respir Rev. 26(170028)2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Roca O, Messika J, Caralt B,
García-de-Acilu M, Sztrymf B, Ricard JD and Masclans JR: Predicting
success of high-flow nasal cannula in pneumonia patients with
hypoxemic respiratory failure: The utility of the ROX index. J Crit
Care. 35:200–205. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
D'Cruz RF, Hart N and Kaltsakas G:
High-flow therapy: Physiological effects and clinical applications.
Breathe (Sheff). 16(200224)2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Hernández G, Vaquero C, González P, Subira
C, Frutos-Vivar F, Rialp G, Laborda C, Colinas L, Cuena R and
Fernández R: Effect of postextubation high-flow nasal cannula vs
conventional oxygen therapy on reintubation in low-risk patients: A
randomized clinical trial. JAMA. 315:1354–1361. 2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Hernández G, Vaquero C, Colinas L, Cuena
R, González P, Canabal A, Sanchez S, Rodriguez ML, Villasclaras A
and Fernández R: Effect of postextubation high-flow nasal cannula
vs noninvasive ventilation on reintubation and postextubation
respiratory failure in high-risk patients: A randomized clinical
trial. JAMA. 316:1565–1574. 2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Zhu Y, Yin H, Zhang R, Ye X and Wei J:
High-flow nasal cannula oxygen therapy versus conventional oxygen
therapy in patients after planned extubation: A systematic review
and meta-analysis. Crit Care. 23(180)2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Granton D, Chaudhuri D, Wang D, Einav S,
Helviz Y, Mauri T, Mancebo J, Frat JP, Jog S, Hernandez G, et al:
High-flow nasal cannula compared with conventional oxygen therapy
or noninvasive ventilation immediately postextubation: A systematic
review and meta-analysis. Crit Care Med. 48:e1129–1136.
2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Douglas N, Ng I, Nazeem F, Lee K, Mezzavia
P, Krieser R, Steinfort D, Irving L and Segal R: A randomised
controlled trial comparing high-flow nasal oxygen with standard
management for conscious sedation during bronchoscopy. Anaesthesia.
73:169–176. 2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Maitra S, Som A, Bhattacharjee S, Arora MK
and Baidya DK: Comparison of high-flow nasal oxygen therapy with
conventional oxygen therapy and noninvasive ventilation in adult
patients with acute hypoxemic respiratory failure: A meta-analysis
and systematic review. J Crit Care. 35:138–144. 2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Seow D, Khor YH, Khung SW, Smallwood DM,
Ng Y, Pascoe A and Smallwood N: High-flow nasal oxygen therapy
compared with conventional oxygen therapy in hospitalised patients
with respiratory illness: A systematic review and meta-analysis.
BMJ Open Respir Res. 11(e002342)2024.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Kepreotes E, Whitehead B, Attia J,
Oldmeadow C, Collison A, Searles A, Goddard B, Hilton J, Lee M and
Mattes J: High-flow warm humidified oxygen versus standard low-flow
nasal cannula oxygen for moderate bronchiolitis (HFWHO RCT): An
open, phase 4, randomised controlled trial. Lancet. 389:930–939.
2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Franklin D, Babl FE, Schlapbach LJ, Oakley
E, Craig S, Neutze J, Furyk J, Fraser JF, Jones M, Whitty JA, et
al: A randomized trial of high-flow oxygen therapy in infants with
bronchiolitis. N Engl J Med. 378:1121–1131. 2018.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Kawaguchi A, Yasui Y, deCaen A and Garros
D: The clinical impact of heated humidified high-flow nasal cannula
on pediatric respiratory distress. Pediatr Crit Care Med.
18:112–119. 2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Kwon JW: High-flow nasal cannula oxygen
therapy in children: A clinical review. Clin Exp Pediatr. 63:3–7.
2020.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Arruda DG, Kieling GA and Melo-Diaz LL:
Effectiveness of high-flow nasal cannula therapy on clinical
outcomes in adults with COVID-19: A systematic review. Can J Respir
Ther. 59:52–65. 2023.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Li Y, Li C, Chang W and Liu L: High-flow
nasal cannula reduces intubation rate in patients with COVID-19
with acute respiratory failure: A meta-analysis and systematic
review. BMJ Open. 13(e067879)2023.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Pisciotta W, Passannante A, Arina P,
Alotaibi K, Ambler G and Arulkumaran N: High-flow nasal oxygen
versus conventional oxygen therapy and noninvasive ventilation in
COVID-19 respiratory failure: A systematic review and network
meta-analysis of randomised controlled trials. Br J Anaesth.
132:936–944. 2024.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Oczkowski S, Ergan B, Bos L, Chatwin M,
Ferrer M, Gregoretti C, Heunks L, Frat JP, Longhini F, Nava S, et
al: ERS clinical practice guidelines: High-flow nasal cannula in
acute respiratory failure. Eur Respir J. 59(2101574)2022.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Loomba RS, Villarreal EG, Farias JS,
Bronicki RA and Flores S: Pediatric intensive care unit admissions
for COVID-19: Insights using state-level data. Int J Pediatr.
2020(9680905)2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Wu JH, Wang CC, Lu FL, Huang SC and Wu ET:
The applications of high-flow nasal cannulas in pediatric intensive
care units in Taiwan. J Formos Med Assoc. 124:15–21.
2025.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Albrecht D: Vaccination, politics and
COVID-19 impacts. BMC Public Health. 22(96)2022.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Chung HW, Apio C, Goo T, Heo G, Han K, Kim
T, Kim H, Ko Y, Lee D, Lim J, et al: Effects of government policies
on the spread of COVID-19 worldwide. Sci Rep.
11(20495)2021.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Bai W, Sha S, Cheung T, Su Z, Jackson T
and Xiang YT: Optimizing the dynamic zero-COVID policy in China.
Int J Biol Sci. 18:5314–5316. 2022.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Chen JM and Chen YQ: China can prepare to
end its zero-COVID policy. Nat Med. 28:1104–1105. 2022.PubMed/NCBI View Article : Google Scholar
|
|
37
|
The Lancet Regional Health-Western
Pacific. The end of zero-COVID-19 policy is not the end of COVID-19
for China. Lancet Reg Health West Pac. 30(100702)2023.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Petridou E: Politics and administration in
times of crisis: Explaining the Swedish response to the COVID-19
crisis. Eur Policy Anal. 6:147–158. 2020.
|
|
39
|
Martinez-Valle A: Public health matters:
Why is Latin America struggling in addressing the pandemic? J
Public Health Policy. 42:27–40. 2021.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Emanuel EJ, Luna F, Schaefer GO, Tan KC
and Wolff J: Enhancing the WHO's proposed framework for
distributing COVID-19 vaccines among countries. Am J Public Health.
111:371–373. 2021.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Yoo KJ, Mehta A, Mak J, Bishai D, Chansa C
and Patenaude B: COVAX and equitable access to COVID-19 vaccines.
Bull World Health Organ. 100:315–328. 2022.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Gonsalves G and Yamey G: Political
interference in public health science during the COVID-19. BMJ.
371(M3878)2020.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Fedson DS: COVID-19, host response
treatment, and the need for political leadership. J Publ Health
Policy. 42:6–14. 2021.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Greer SL, King EJ, Massard da Fonseca E
and Peralta-Santos A (eds): Coronavirus politics: The comparative
politics and policy of COVID-19. University of Michigan Press,
2021.
|
|
45
|
Lazarus JV, Wyka K, White TM, Picchio CA,
Rabin K, Ratzan SC, Parsons Leigh J, Hu J and El-Mohandes A:
Revisiting COVID-19 vaccine hesitancy around the world using data
from 23 countries in 2021. Nat Commun. 13(3801)2022.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Lucey CR and Johnston SC: The
transformational effects of COVID-19 on medical education. JAMA.
324:1033–1034. 2020.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Frenk J, Chen LC, Chandran L, Groff EOH,
King R, Meleis A and Fineberg HV: Challenges and opportunities for
educating health professionals after the COVID-19 pandemic. Lancet.
400:1539–1556. 2022.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Mammas IN, Liston M, Koletsi P, Vitoratou
DI, Koutsaftiki C, Papatheodoropoulou A, Kornarou H, Theodoridou M,
Kramvis A, Drysdale SB and Spandidos DA: Insights in paediatric
virology during the COVID-19 era (review). Med Int (Lond).
2(17)2022.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Mammas IN, Drysdale SB, Charalampous C,
Koletsi P, Papatheodoropoulou A, Koutsaftiki C, Sergentanis T,
Merakou K, Kornarou H, Papaioannou G, et al: Navigating paediatric
virology through the COVID-19 era (Review). Int J Mol Med.
52(83)2023.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Fischhoff B and Scheufele DA: The science
of science communication. Introduction. Proc Natl Acad Sci USA. 110
(Suppl 3):S14031–S14032. 2013.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Amer P: Coronavirus conversations: Science
communication during a pandemic. Nature: May 27, 2020 (Epub ahead
of print).
|
|
52
|
Rubin R: When physicians spread
unscientific information about COVID-19. JAMA. 327:904–906.
2022.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Joseph AM, Fernandez V, Kritzman S, Eaddy
I, Cook OM, Lambros S, Jara Silva CE, Arguelles D, Abraham C,
Dorgham N, et al: COVID-19 Misinformation on social media: A
scoping review. Cureus. 14(e24601)2022.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Lurie P, Adams J, Lynas M, Stockert K,
Carlyle RC, Pisani A and Evanega SD: COVID-19 vaccine
misinformation in English-language news media: Retrospective cohort
study. BMJ Open. 12(e058956)2022.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Wilson SL and Wiysonge C: Social media and
vaccine hesitancy. BMJ Glob Health. 5(e004206)2020.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Schwarzinger M and Luchini S: Addressing
COVID-19 vaccine hesitancy: Is official communication the key?
Lancet Public Health. 6:e353–e354. 2021.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Karafilakis E, Van Damme P, Hendrickx G
and Larson HJ: COVID-19 in Europe: New challenges for addressing
vaccine hesitancy. Lancet. 399:699–701. 2022.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Heuss SC, Zachlod C and Miller BT:
‘Social’ media? How Swiss hospitals used social media platforms
during the early months of the COVID-19 pandemic crisis. Public
Health. 219:53–60. 2023.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Rubin EJ, Baden LR and Morrissey S: Audio
interview: Covid-19 takeaways at podcast 100. N Engl J Med.
386(e11)2022.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Boender TS, Louis-Ferdinand N and Duschek
G: Digital visual communication for public health: Design proposal
for a vaccinated emoji. J Med Internet Res.
24(e35786)2022.PubMed/NCBI View
Article : Google Scholar
|
|
61
|
Davies SC, Audi H and Cuddihy M:
Leveraging data and new digital tools to prepare for the next
pandemic. Lancet. 397:1349–1350. 2021.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Sachs JD, Karim SSA, Aknin L, Allen J,
Brosbøl K, Colombo F, Barron GC, Espinosa MF, Gaspar V, Gaviria A,
et al: The lancet commission on lessons for the future from the
COVID-19 pandemic. Lancet. 400:1244–1280. 2022.PubMed/NCBI View Article : Google Scholar
|