Introduction
Tuberculosis is a systemic infection caused by
Mycobacterium tuberculosis, primarily affecting the
pulmonary parenchyma (1). Recognized
as a global public health issue (2),
it ranks among the top 10 causes of mortality from infectious
diseases and is characterized by high transmissibility, potential
for dissemination, and significant lethality (3,4). An
estimated one-quarter of the world's population is at risk of
developing tuberculosis, with ~10 million active cases and 1.4
million related deaths annually attributable to the disease
(5). In Mexico, the incidence is 24
cases per 100,000 inhabitants, with up to 80% of strains reported
as resistant to standard treatment and ~10% classified as
multidrug-resistant (6). Several
predisposing factors, such as a low socioeconomic status,
overcrowding, substance abuse, homelessness and poor living
conditions are associated with an increased risk of the development
of the disease (7). Although
addressing these social determinants has helped reduce incidence
rates, significant challenges remain, particularly related to the
delayed diagnosis of new cases, particularly those with atypical
clinical presentations (8).
Although pulmonary tuberculosis is the most common
clinical manifestation, the hematogenous dissemination of
Mycobacterium tuberculosis can lead to extrapulmonary forms,
with abdominal tuberculosis being the most frequent presentation
(9). This extrapulmonary form poses
a diagnostic challenge, as it may occur in otherwise healthy
individuals presenting with non-specific symptoms, such as fever,
diarrhea, constipation and weight loss, often mimicking abdominal
or peritoneal malignancies (10,11).
Given that misdiagnosis can worsen the clinical course, accurate
identification relies on radiological, histopathological and
molecular criteria. For these reasons, abdominal tuberculosis is
often considered a diagnosis of exclusion (12-14).
However, despite thorough diagnostic efforts, the
majority of cases of abdominal tuberculosis without pulmonary
involvement often remain undetected, allowing disease progression.
In this context, up to 25% of patients develop gastrointestinal
tuberculosis complicated by stenosis, and ~20% ultimately require
surgical intervention (15). Among
the most severe, yet rare complications is intestinal perforation,
which can be life-threatening and requires urgent surgical
management. Due to its non-specific symptoms and potential
severity, abdominal tuberculosis often remains unrecognized. The
present case report describes an uncommon manifestation of
intestinal tuberculosis in an immunocompetent adult, complicated by
bowel perforation. By highlighting the clinical course, diagnostic
process and surgical findings, the present study aimed to raise
awareness of this rare, yet severe presentation, and emphasize the
need to consider abdominal tuberculosis in the differential
diagnosis of chronic abdominal pain, particularly in endemic
regions.
Case report
A 39-year-old male patient with a history of chronic
tobacco use (25 pack-year index) and habitual alcohol consumption
for 23 years, both discontinued 2 years prior to presentation in
January, 2025 at Hospital General Regional No 1, Unidad Morelos del
Instituto Mexicano Del Seguro Social, Chihuahua, Mexico. He
reported occasional cannabis use and multiple tattoos performed
under poor hygienic conditions. His family history was notable for
the death of a sister due to pulmonary tuberculosis in 2006.
The patient was admitted to the hospital due to the
exacerbation of chronic abdominal pain that had persisted for 2
years. The pain was colicky in nature and mild in intensity (3/10
on the visual analog scale), worsened by food intake and improved
with fasting. Upon admission, the patient was febrile (38.5˚C),
with a heart rate of 112 bpm, blood pressure of 100/65 mmHg, a
respiratory rate of 24 breaths per minute and ab oxygen saturation
of 94% on room air. He appeared pale, diaphoretic and in visible
discomfort. An abdominal examination confirmed moderate distension,
involuntary guarding and a board-like abdomen.
Laboratory tests revealed leukocytosis (15,600/µl)
with left shift (90% neutrophils), normocytic normochromic anemia
(Hb 9.2 g/dl), thrombocytosis (420,000/µl), an elevated erythrocyte
sedimentation rate (86 mm/h), a high level of C-reactive protein
(132 mg/l) and hypoalbuminemia (2.8 g/dl). Liver and renal function
tests yielded results which were within normal limits. HIV testing
was negative.
The condition was accompanied by general symptoms,
including asthenia, adynamia and decreased appetite. Over the past
3 months, he reported a progressive increase in pain intensity,
along with an estimated weight loss of ~20% of his usual body
weight. He had previously received symptomatic treatment without
significant clinical improvement.
Given the clinical context and the history of the
patient, complementary analyses were requested. Viral serology
yielded a positive result for hepatitis C, although with no
detectable viral load. An abdominal computed tomography (CT)
angiography ruled out mesenteric ischemia, and the patient was
admitted to the Internal Medicine service at Hospital General
Regional No 1, Unidad Morelos for further diagnostic workup. Upon
admission, a physical examination revealed a rigid abdomen, the
absence of bowel sounds and severe abdominal pain (10/10 on the
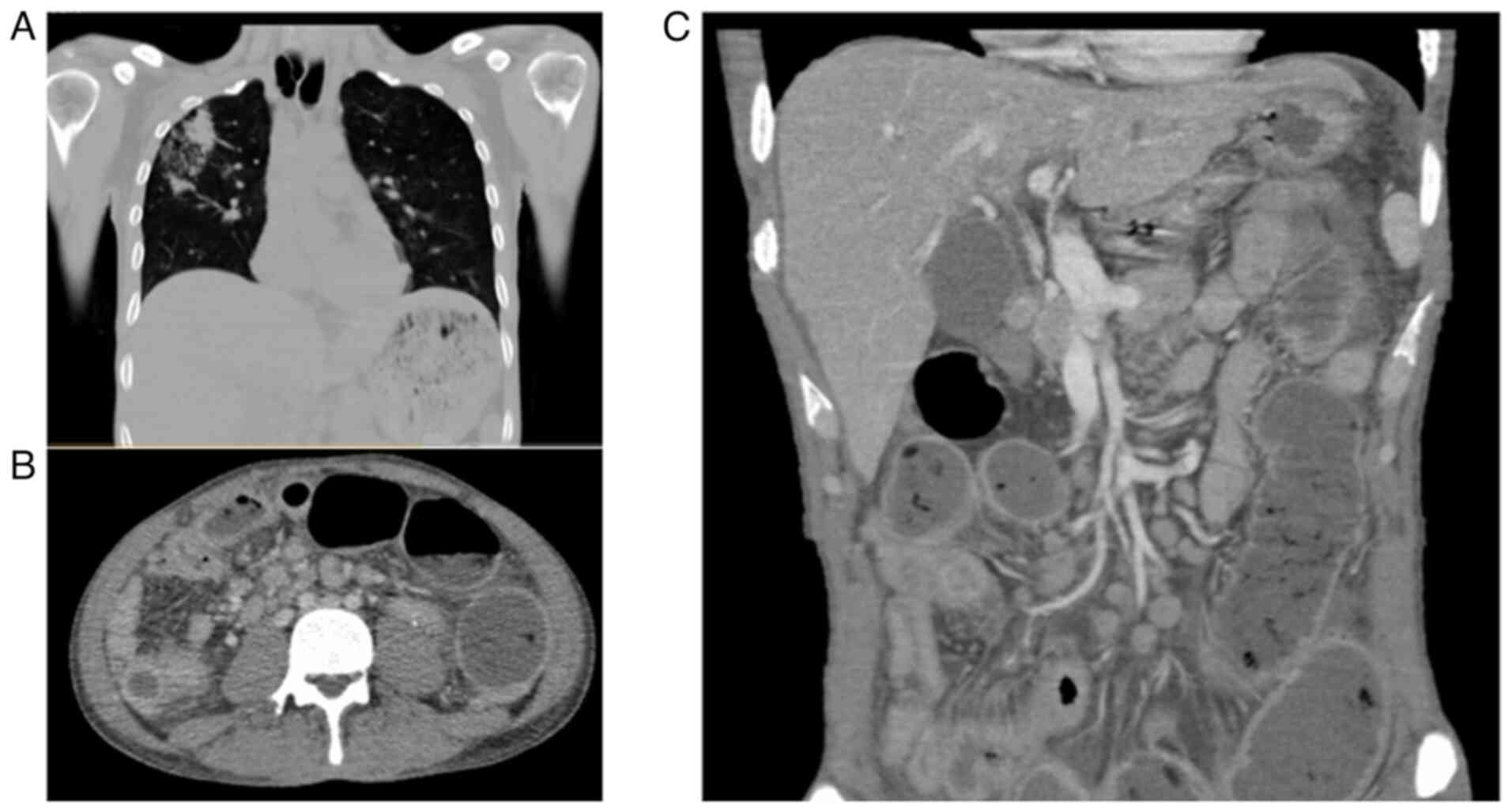
visual analog scale). A non-contrast abdominal CT scan revealed
dilated loops of small bowel, irregular mural thickening of the
terminal ileum, moderate amounts of free peritoneal fluid, and
mesenteric fat stranding, findings suggestive of secondary
peritonitis due to intestinal perforation. A chest CT scan revealed
a thick-walled cavitary lesion in the upper right lobe with central
consolidation, internal air and bilateral areas of ground-glass
opacity with heterogeneous distribution. These findings were
compatible with active pulmonary tuberculosis (Fig. 1).
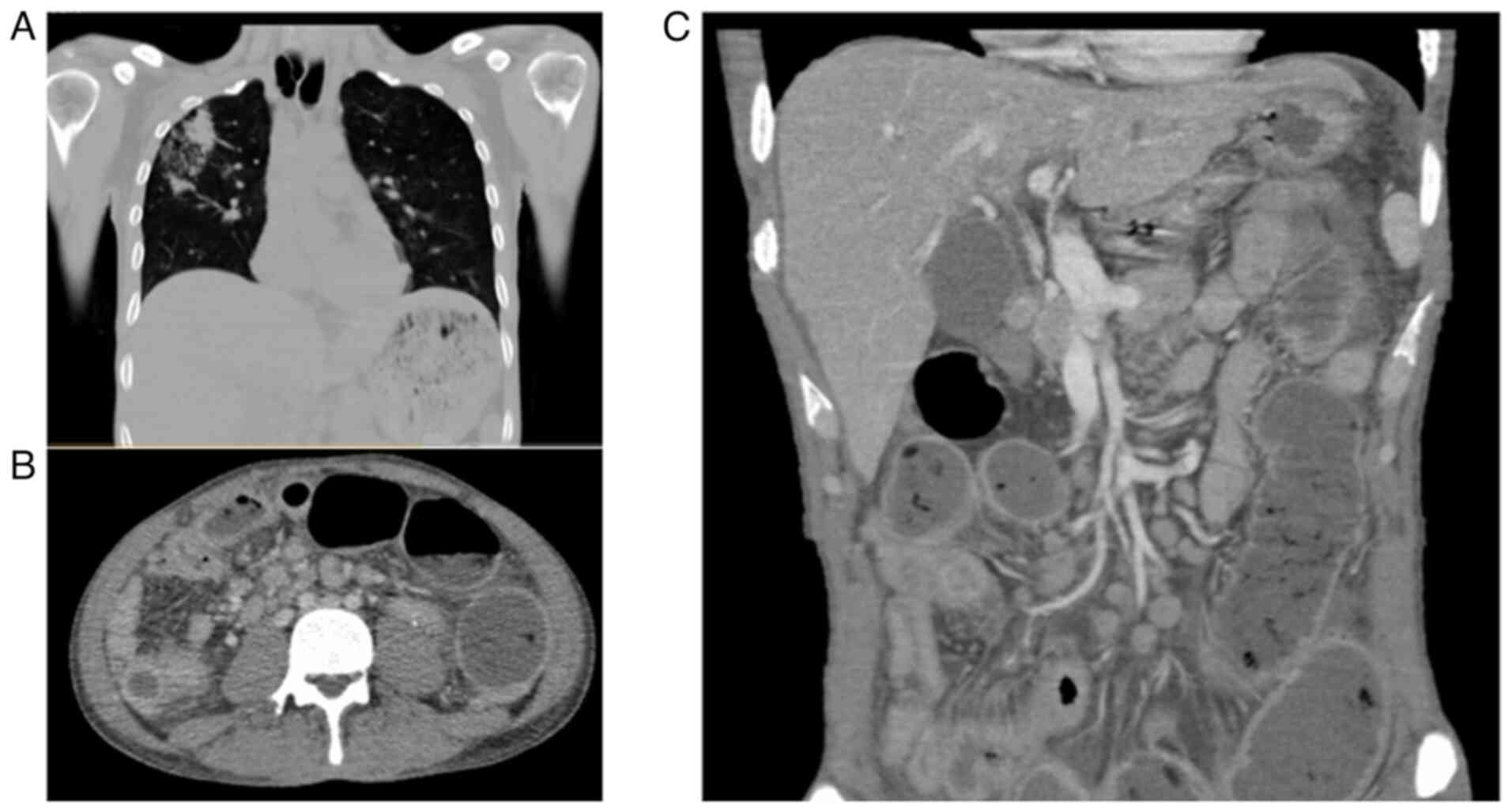 | Figure 1Non-contrast CT scan of the chest and
abdomen: (A) Chest CT illustrating a cavitary lesion in the right
upper lobe with central consolidation, intralesional air, multiple
areas of increased attenuation and regions of ground-glass opacity
with heterogeneous distribution, findings consistent with active
pulmonary tuberculosis. (B) Axial CT scan demonstrating marked
mural thickening and luminal narrowing of small bowel loops, with
adjacent mesenteric fat stranding suggestive of active
inflammation. Multiple enlarged mesenteric lymph nodes with a
hypodense center (characteristic of caseating necrosis) are
visualized, consistent with tuberculous lymphadenitis. (C) Coronal
abdominal CT scan illustrating multiple dilated small bowel loops
with heterogeneous wall thickening, suggestive of inflammatory or
infectious involvement. Notably, there is the presence of free
intraperitoneal air adjacent to the left flank, indicative of a
perforated viscus. Several mesenteric lymph nodes appear enlarged,
consistent with reactive or granulomatous lymphadenopathy. These
radiologic features are consistent with advanced abdominal
tuberculosis complicated by intestinal perforation. CT, computed
tomography. |
An exploratory laparotomy was performed, revealing
the following intraoperative findings: A total of 100 ml of
purulent free fluid, dilated small bowel loops, mural thickening,
multiple interloop adhesions, intestinal granulomatosis, a 5-mm
perforation located ~150 cm from the Treitz angle, indurated
mesenteric lymph nodes, fibrotic rings in the ileum 50 cm from the
ileocecal valve and cecal induration. The affected bowel segment
was resected, followed by terminal ileostomy creation, mucous
fistula formation and abdominal cavity lavage. The surgical
specimens were submitted to the pathology laboratory of the
hospital for comprehensive gross and histopathological
analysis.
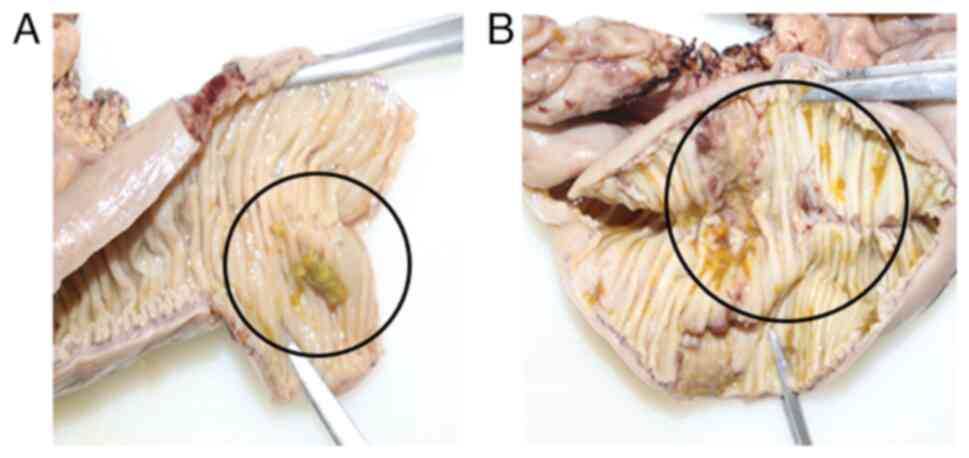
Histopathology reported ulcerated chronic
granulomatous enteritis with caseous necrosis and intestinal
perforation of tuberculous etiology. Surgical margins exhibited
acute inflammatory changes with the formation of sinus tracts,
indicating active infectious involvement rather than sterile
perforation. The mesentery contained 14 lymph nodes with caseating
granulomatous lymphadenitis, as well as multiple granulomas in the
adjacent adipose tissue (Fig. 2).
Ziehl-Neelsen staining revealed sparse acid-fast bacilli. Based on
these findings, a diagnosis of intestinal tuberculosis with
perforation was established, and treatment was initiated according
to the DOTBAL regimen (rifampicin, 10 mg/kg/day; isoniazid, 5
mg/kg/day; pyrazinamide, 25 mg/kg/day; and ethambutol, 15
mg/kg/day), supplemented with vitamin B12 (1,000 µg/day). The
patient was discharged with scheduled follow-up in the outpatient
clinic.
Discussion
The present case report describes the diagnostic
approach in a middle-aged, immunocompetent male with risk factors
for tuberculosis who presented with chronic, nonspecific abdominal
symptoms that culminated in intestinal perforation secondary to
undiagnosed abdominal tuberculosis.
Given the clinical and pathological findings, a
comprehensive review of similar cases and diagnostic challenges is
warranted. Reports in the literature have documented similar
presentations of intestinal tuberculosis in immunocompetent adults,
often involving chronic, vague abdominal symptoms that mimic other
gastrointestinal pathologies. The review article by Debi et
al (16) indicated that the
ileocecal region is the most commonly affected site, with
perforation occurring in <5% of cases, typically in advanced or
undiagnosed disease. In the study by Ahmed et al (17), patients with intestinal tuberculosis
presented with abdominal pain, altered bowel habits, fever and
weight loss, features that overlap with malignancies or
inflammatory bowel diseases, such as Crohn's disease. Moreover, the
majority of cases required surgical exploration for definitive
diagnosis, as preoperative imaging and laboratory tests often
failed to confirm the etiology (17).
In the case series by Chan and Lee (18), several patients without HIV or other
known causes of immunosuppression presented with perforation due to
intestinal tuberculosis, with diagnosis achieved only
postoperatively via histopathology. These findings align with the
present case, where the lack of specific clinical indicators, the
gradual onset of symptoms, and a non-specific response to initial
symptomatic treatment delayed appropriate intervention. This
underscores the necessity of considering abdominal tuberculosis in
the differential diagnosis of chronic abdominal pain, even in the
absence of clear immunosuppressive factors, particularly in regions
with an intermediate or high prevalence of tuberculosis.
Additionally, the increasing incidence of atypical
and extrapulmonary tuberculosis in younger populations without
classic risk factors highlights the evolving epidemiological
landscape of this disease (19).
This reinforces the importance of a multidisciplinary diagnostic
strategy and heightened clinical suspicion, particularly when
non-specific gastrointestinal symptoms are accompanied by weight
loss, systemic signs, or a suggestive family or epidemiological
background.
Tuberculosis is an infectious disease known since
antiquity; its causative agent was identified in the 19th century,
a period marked by significant disease spread. Due to its
predominant respiratory manifestations, tuberculosis was soon
recognized as one of the first major global public health
challenges (20). Although its
incidence has declined in recent decades, tuberculosis remains one
of the leading causes of mortality from infectious diseases.
Currently, up to 15% of all cases are extrapulmonary, with
abdominal tuberculosis being the most common form, prompting the
WHO to prioritize its early identification (21).
Abdominal tuberculosis may result from the direct
ingestion of the pathogen or hematogenous dissemination from a
primary pulmonary focus, mediated by immune cells (22). Once in the abdominal cavity,
Mycobacterium tuberculosis can affect the gastrointestinal
tract, peritoneum, solid abdominal organs and mesenteric lymph
nodes. Although it shares risk factors with pulmonary tuberculosis,
it also presents distinct characteristics, being more commonly
observed in women and in patients with chronic conditions that
induce a pro-inflammatory state, even in the absence of overt
immunosuppression (23).
In the case presented herein, the identified risk
factors did not fully align with those typically described for
abdominal tuberculosis. The absence of prolonged, specific symptoms
and the abrupt clinical worsening hindered the initial diagnosis.
This aligns with previous reports highlighting the difficulty of
establishing an etiologic diagnosis in immunocompetent individuals,
where confirmation is achieved only after a thorough clinical
history is obtained (24,25). Similar cases have been described in
patients of comparable age and immune status, without evident risk
factors, who developed acute disease following nonspecific
constitutional and gastrointestinal symptoms. In such instances,
diagnosis was only reached after comprehensive imaging, serologic
testing and histopathologic evaluation (26).
Beyond clinical features, the patient in the present
study exhibited unconventional, yet relevant risk factors, such as
high-risk behaviors and a history of poor hygiene (27,28).
Additionally, prior epidemiological research has reported that in
northern and northeastern regions of Mexico, where the patient was
originally from, latent or oligosymptomatic tuberculosis is
prevalent, particularly among young and middle-aged males, possibly
explaining the primary infection in this case (29).
Although the patient described herein did not
present with respiratory symptoms, imaging analyses revealed a
pulmonary cavitation, consistent with latent tuberculosis. This
finding may contribute to the development of extrapulmonary forms
of the disease (30). Household
exposure, particularly the history of a sister who succumbed due to
pulmonary tuberculosis, supports the hypothesis of prior latent
infection (31). Notably, a number
of young patients discontinue prophylactic treatment or follow-up,
even when a direct family history is present, particularly in
contexts lacking support networks or with gaps in epidemiologic
surveillance (32).
It is also worth noting that the onset of symptoms
in this patient coincided with the COVID-19 pandemic in Mexico. In
this context, it is reasonable to consider that the tuberculosis
diagnosis may have been delayed due to prioritization of COVID-19
cases and the suspension of screening programs in high-risk
populations (33). While the
pandemic highlighted the importance of infectious diseases, it also
negatively affected the care of other conditions, particularly
respiratory illnesses (34). The
strain placed on epidemiological surveillance systems led to
under-diagnosis and clinical deterioration in patients with
tuberculosis, which may have influenced the outcome in the case
described herein (35).
The present case report is subject to several
limitations. First, the diagnosis of intestinal tuberculosis was
only confirmed post-operatively through histopathology, as
microbiological cultures or PCR testing were not performed. Second,
the clinical course of the patient was documented over a limited
follow-up period, which restricts the evaluation of a long-term
treatment response. Additionally, healthcare disruptions during the
COVID-19 pandemic may have contributed to diagnostic delays. As
with all single-case reports, generalizability to broader
populations is limited.
Although detecting latent tuberculosis could aid in
identifying non-specific clinical presentations and preventing
extrapulmonary forms, its diagnosis remains challenging. The wide
variability in the sensitivity of available tests, compounded by
diverse immunological and inflammatory conditions in the Mexican
population, limits the feasibility of mass screening strategies
(36). Nevertheless, the complex
interaction between Mycobacterium tuberculosis and its host
promotes mutations that confer antimicrobial resistance (37). The rising prevalence of
multidrug-resistant strains has renewed interest in the follow-up
and treatment of latent tuberculosis infections (38). In this context, case reports, such as
the present one underscore the need to strengthen adherence to
therapeutic and prophylactic regimens among contacts of diagnosed
patients, and to consider tuberculosis in the differential
diagnosis of acute abdominal syndromes, even in young,
immunocompetent men with no specific clinical history (39). The present case report serves as a
valuable reminder of the varied presentations of tuberculosis and
the need for vigilance even in non-immunocompromised
individuals.
In conclusion, intestinal tuberculosis remains a
diagnostic challenge, particularly in immunocompetent patients
presenting with non-specific abdominal symptoms and no clear
history of recent exposure. The case described in the present study
highlights the importance of maintaining a high index of clinical
suspicion in atypical abdominal presentations, particularly in
endemic regions and among individuals with unconventional risk
factors, such as poor hygienic conditions or a family history of
tuberculosis. The surgical outcome resulting from an advanced form
of abdominal tuberculosis underscores the need to strengthen early
detection systems, particularly in settings where epidemiologic
surveillance has been weakened, such as during the COVID-19
pandemic. The timely identification of latent tuberculosis and
adherence to prophylactic treatment protocols could help prevent
severe complications, including intestinal perforation. The present
case report emphasizes the value of a multidisciplinary approach
and the combined use of clinical, radiological and
histopathological tools for the comprehensive diagnosis of this
condition.
Acknowledgements
The authors would like to thank our host institution
Hospital General Regional No. 1, Unidad Morelos of the Instituto
Mexicano del Seguro Social (IMSS), Chihuahua, Mexico, for its
logistical support in providing access to the patient's clinical
information during the preparation of this manuscript.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
HARL and LFMB participated equally in the
preparation of this manuscript, both in the medical care process
and during data collection, literature search, information
synthesis, and writing of this manuscript. HARL and LFMB confirm
the authenticity of all the raw data. Both authors have read and
approved the final manuscript.
Ethics approval and consent for
participation
The present study was performed in accordance with
the ethical standards of the Declaration of Helsinki, 1964. Ethics
approval was waived by the local committee as no personal data was
used. Informed consent was obtained from the patient for inclusion
in the study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
related images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Chaudhary P, Kumar R, Ahirwar N, Nabi I,
Gautam S, Munjewar C and Kumar A: A retrospective cohort study of
756 cases of abdominal tuberculosis: Two decades single centre
experience. Indian J Tuberc. 63:245–250. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Udgirkar S, Jain S, Pawar S, Chandnani S,
Contractor Q and Rathi P: Clinical profile, drug resistance pattern
and treatment outcomes of abdominal tuberculosis patients in
western india. Arq Gastroenterol. 56:178–183. 2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Ionescu S, Nicolescu AC, Madge OL,
Marincas M, Radu M and Simion L: Differential diagnosis of
abdominal tuberculosis in the adult-literature review. Diagnostics
(Basel). 11(2362)2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
World Health Organization (WHO): Global
tuberculosis report 2022. WHO, Geneva, 2022. https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022.
|
|
5
|
Ordaz-Vázquez A, Torres-González P,
Cruz-Hervert P, Ferreyra-Reyes L, Delgado-Sánchez G, García-García
L, Kato-Maeda M, Ponce-De-León A, Sifuentes-Osornio J and
Bobadilla-Del-Valle M: Genetic diversity and primary drug
resistance transmission in Mycobacterium tuberculosis in southern
Mexico. Infect Genet Evol. 93(104994)2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Centers for Disease Control and Prevention
(CDC): Trends in Tuberculosis. CDC, Atlanta, GA, 2021. https://www.cdc.gov/tb/publications/factsheets/statistics/tbtre
nds.html.
|
|
7
|
Busatto C, Bierhals DV, Vianna JS, Silva
PEAD, Possuelo LG and Ramis IB: Epidemiology and control strategies
for tuberculosis in countries with the largest prison populations.
Rev Soc Bras Med Trop. 55(e00602022)2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Cheng MP, Abou Chakra CN, Yansouni CP,
Cnossen S, Shrier I, Menzies D and Greenaway C: Risk of active
tuberculosis in patients with cancer: A systematic review and
meta-analysis. Clin Infect Dis. 64:635–644. 2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Jha DK, Pathiyil MM and Sharma V:
Evidence-based approach to diagnosis and management of abdominal
tuberculosis. Indian J Gastroenterol. 42:17–31. 2023.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Wenting J, Yuyan M, Qingfeng S, Yao Z,
Yumeng Y, Yi S, Yingnan H, Qing M, Qingqing W, Mengran W, et al:
Clinical features and diagnostic approaches for abdominal
tuberculosis: Five-year experience from a
non-tuberculosis-designated hospital in China. Rev Esp Enferm Dig.
114:461–467. 2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Das CJ, Rednam N, Vora Z, Aggarwal A,
Chandrashekhara SH and Kundra V: Abdominal visceral tuberculosis: A
malignancy mimic. Abdom Radiol (NY). 48:2705–2715. 2023.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Dahale AS and Dalal A: Evidence-based
commentary: Ascitic adenosine deaminase in the diagnosis of
peritoneal tuberculosis. J Gastrointest Infect. 12:57–60. 2022.
|
|
13
|
Brehm TT, Schmiedel S and Lohse AW:
Diagnosis of abdominal tuberculosis by mini-laparoscopy. Infection.
50:1049–1050. 2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Stein CM: Genetic epidemiology of
resistance to M. tuberculosis Infection: Importance of study design
and recent findings. Genes Immun. 24:117–123. 2023.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Jena A, Mohindra R, Rana K, Neelam PB,
Thakur DC, Singh H, Gupta P, Suri V and Sharma V: Frequency,
outcomes, and need for intervention in stricturing gastrointestinal
tuberculosis: A systematic review and meta-analysis. BMC
Gastroenterol. 23(46)2023.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Debi U, Ravisankar V, Prasad KK, Sinha SK
and Sharma AK: Abdominal tuberculosis of the gastrointestinal
tract: Revisited. World J Gastroenterol. 20:14831–14840.
2014.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ahmed S, Hafez W, El Chayeb J, Al Jassem
N, Massoud A, Nader S and Aboushady R: Intestinal tuberculosis and
inflammatory bowel disease; the usual challenging differential
diagnoses: A case report. Radiol Case Rep. 18:3680–3685.
2023.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kok-Hong Chan D and Lee KC: Perforated
intestinal tuberculosis in a non-AIDS immunocompromised patient. Am
J Case Rep. 16:719–722. 2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Rolo M, González-Blanco B, Reyes CA,
Rosillo N and López-Roa P: Epidemiology and factors associated with
Extra-pulmonary tuberculosis in a Low-prevalence area. J Clin
Tuberc Other Mycobact Dis. 32(100377)2023.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Barbier M and Wirth T: The Evolutionary
History, Demography, and Spread of the Mycobacterium tuberculosis
Complex. Microbiol Spectr 4, 2016. https://doi.org/10.1128/microbiolspec.tbtb2-0008-2016.
|
|
21
|
World Health Organization (WHO): Global
tuberculosis report 2023. WHO, Geneva, 2023. https://iris.who.int/handle/10665/373828.
|
|
22
|
Cho JK, Choi YM, Lee SS, Park HK, Cha RR,
Kim WS, Kim JJ, Lee JM, Kim HJ, Ha CY, et al: Clinical features and
outcomes of abdominal tuberculosis in southeastern Korea: 12 years
of experience. BMC Infect Dis. 18(699)2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Al-Zanbagi AB and Shariff MK:
Gastrointestinal tuberculosis: A systematic review of epidemiology,
presentation, diagnosis and treatment. Saudi J Gastroenterol.
27:261–274. 2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Niu T, He F, Yang J, Ma C, Xu J, Sun T,
Zhang X, Chen S and Ru C: The epidemiological characteristics and
infection risk factors for extrapulmonary tuberculosis in patients
hospitalized with pulmonary tuberculosis infection in China from
2017 to 2021. BMC Infect Dis. 23(488)2023.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Mirijello A, Ritrovato N, D'Agruma A, de
Matthaeis A, Pazienza L, Parente P, Cassano DP, Biancofiore A,
Ambrosio A and Carosi I: , et al: Abdominal
lymphadenopathies: Lymphoma, brucellosis or tuberculosis?
Multidisciplinary approach-case report and review of the
literature. Medicina (Kaunas). 59(293)2023.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Meregildo-Rodriguez ED, Tafur-Ramirez RC,
Espino-Saavedra WG and Angulo-Prentice SF: Abdominal tuberculosis
misdiagnosed as acute surgical abdomen and carcinomatosis.
F1000Res. 10(355)2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Chien K, Seemangal J, Batt J and Vozoris
NT: Abdominal tuberculosis: A descriptive case series of the
experience in a Canadian tuberculosis clinic. Int J Tuberc Lung
Dis. 22:681–685. 2018.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Curry J, Abdelbary B, Garcia-Viveros M,
Garcia JI, Yotebieng M, Rendon A, Torrelles JB and Restrepo BI:
South to north migration patterns of tuberculosis patients
diagnosed in the Mexican border with Texas. J Immigr Minor Health.
24:1113–1121. 2022.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Flores-Aréchiga A, Zacarías-Hernández JL,
Vázquez-Cortés CG, Tamez-Guerra RS, De la O-Cavazos M,
Rivera-Morales LG, Llaca-Díaz JM, Castro-Garza J, Casillas-Vega N,
Vázquez-Guillén JM and Rodríguez-Padilla C: Molecular epidemiology
and drug resistance of Mycobacterium tuberculosis in a tertiary
care hospital in northeastern Mexico. J Infect Dev Ctries.
17:1753–1760. 2023.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Schwartz NG, Price SF, Pratt RH and Langer
AJ: Tuberculosis-United States, 2019. MMWR Morb Mortal Wkly Rep.
69:286–289. 2020.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Behr MA, Edelstein PH and Ramakrishnan L:
Revisiting the timetable of tuberculosis. BMJ.
362(k2738)2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Medrano BA, Lee M, Gemeinhardt G,
Rodríguez-Herrera JE, García-Viveros M and Restrepo BI:
Tuberculosis presentation and outcomes in older Hispanic adults
from Tamaulipas, Mexico. Medicine (Baltimore).
102(e35458)2023.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Muñiz-Salazar R, Le T, Cuevas-Mota J,
González-Fagoaga JE, Zapata-Garibay R, Ruiz-Tamayo PS,
Robles-Flores J and Garfein RS: Impact of COVID-19 on tuberculosis
detection and treatment in Baja California, México. Front Public
Health. 10(921596)2022.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Bi K, Cao D, Ding C, Lu S, Lu H, Zhang G,
Zhang W, Li L, Xu K, Li L and Zhang Y: The past, present and future
of tuberculosis treatment. Zhejiang Da Xue Xue Bao Yi Xue Ban.
51:657–668. 2022.PubMed/NCBI View Article : Google Scholar : (In English).
|
|
35
|
Dheda K, Perumal T, Moultrie H, Perumal R,
Esmail A, Scott AJ, Udwadia Z, Chang KC, Peter J, Pooran A, et al:
The intersecting pandemics of tuberculosis and COVID-19:
population-level and patient-level impact, clinical presentation,
and corrective interventions. Lancet Respir Med. 10:603–622.
2022.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Carranza C, Pedraza-Sanchez S, de
Oyarzabal-Mendez E and Torres M: Diagnosis for latent tuberculosis
infection: New alternatives. Front Immunol. 11(2006)2020.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Liebenberg D, Gordhan BG and Kana BD: Drug
resistant tuberculosis: Implications for transmission, diagnosis,
and disease management. Front Cell Infect Microbiol.
12(943545)2022.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Esaulova E, Das S, Singh DK, Choreño-Parra
JA, Swain A, Arthur L, Rangel-Moreno J, Ahmed M, Singh B, Gupta A,
et al: The immune landscape in tuberculosis reveals populations
linked to disease and latency. Cell Host Microbe. 29:165–178.e8.
2021.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Rahman SMM, Rahman A, Nasrin R, Ather MF,
Ferdous SS, Ahmed S, Uddin MKM, Khatun R, Sarker MS, Mahmud AM, et
al: Molecular epidemiology and genetic diversity of
multidrug-resistant mycobacterium tuberculosis Isolates in
Bangladesh. Microbiol Spectr. 10(e0184821)2022.PubMed/NCBI View Article : Google Scholar
|