Introduction
Lung ischemia-reperfusion injury (LIRI), a form of
acute sterile lung injury, remains a frequent complication
resulting in morbidity and mortality in lung transplantation
(1), cardiopulmonary bypass
(2), trauma (3), pulmonary embolism (4) and resuscitation from hemorrhagic
shock (5). Early activation of the
alveolar macrophages, the release of various proinflammatory
molecules and a large amount of neutrophil accumulation are
critical in the pathophysiology of LIRI, which leads to excessive
and uncontrolled inflammation and pulmonary tissue damage. Thus, it
is beneficial to inhibit the upregulation of pulmonary inflammation
for suppression of the development of lung injury (6).
Dexmedetomidine is a selective
α2-adrenergic agonist with sedative, antianxiety,
analgesic-sparing, sympatholytic and hemodynamic stability
characteristics (7). In addition,
it has been demonstrated to reduce endotoxine-induced systemic
inflammatory responses, inhibit upregulation of inflammatory
cytokines, including tumor necrosis factor-α (TNF-α),
interleukin-1β (IL-1β), IL-6 and macrophage inflammatory protein-2
(MIP-2); and relieve acute organ injuries in rats and patients with
sepsis (8,9). Moreover, dexmedetomidine has been
reported to significantly attenuate the pulmonary inflammation in
ventilator-induced lung injury in a rat model (10). Although the anti-inflammatory
capacity of dexmedetomidine has been demonstrated, the effect of
dexmedetomidine on the inflammatory molecules, including TNF-α,
IL-6 and monocyte chemoattractant protein (MCP)-1, correlated with
LIRI remains unclear. Therefore, it was hypothesized that
dexemedetomidine may attenuate the production of proinflammatory
chemokines and cytokines and protect the lung from acute I/R
injury.
Toll-like receptors (TLRs) are a family of
transmembranal proteins that are critical in the regulation of the
inflammatory and innate immune responses (11). Among these receptors, TLR4, widely
expressed on immune cells and non-immune cells, including dendritic
cells, neutrophils, macrophages, endothelial cells, epithelial
cells and natural killer cells, specifically recognizes endogenous
molecules released from damaged or ischemic tissues termed
danger-associated molecular patterns (DAMPs), and then activates
multiple intracellular signaling systems, including the
mitogen-activated protein kinase (MAPK) family [extracellular
signal-regulated kinase (ERK), c-Jun N-terminal kinase (JNK) or
p38], and the nuclear factor κB (NF-κB) pathways, all of which are
key regulators of the inflammatory responses during I/R of the
organs (3). In the mouse LIRI
model, the upregulation of TLR4 mRNA expression in alveolar
macrophages is vital in the generation of the early inflammatory
response to LIRI, which is paralleled by the observation of lung
neutrophil recruitment in histological findings and the generation
of cytokines and chemokines (12).
Shi et al (13) identified
that dexmedetomidine provides protection against LPS-induced acute
lung injury through the TLR4/NFκB signaling pathway, and reduces
the level of proinflammatory factors in lung homogenates, as well
as the lung damage observed in histological findings. Therefore,
the present study was conducted to determine whether the
pre-administration of dexemedetomidine may provide a significant
effect on relieving pulmonary damage induced by I/R, and to observe
whether TLR4 relevant signaling pathways may be involved in the
effects of dexemedetomidine on LIRI.
Materials and methods
Animals
The following investigations were performed using a
protocol approved by the Animal Care and Use Committee of the
Xiang-Ya Medical College of the Central South University (Changsha,
China). Adult male Sprague-Dawley rats (220–270 g) were housed in
individual cages in a temperature- and humidity-controlled room
with a 12-h light/dark cycle, and acclimated for one week prior to
the study. All rats were fed standard pellet food and water ad
libitum.
Induction of lung I/R, as described
previously (3)
All the rats were anesthetized with pentobarbital
sodium (50 mg/kg, intraperitoneal) and atropine (0.25 mg,
intramuscular). A tracheotomy was performed following anesthesia,
and the trachea was intubated with a 14-gauge intravenous (i.v.)
catheter (B. Braun Melsungen AG, Melsungen, Germany). The rats were
then mechanically ventilated with a small animal ventilator
(Beijing Zhongxi Yuanda Technology Inc., Beijing, China), adjusting
the tidal volume to 10 ml/kg of room air, the respiratory rate to
50 breaths/min and the inspiratory/expiratory ratio to 1:1. The
body temperature was maintained at 38–40°C using a heating pad. An
intravenous 24-gauge catheter was then installed in the tail vein
for drug and saline administration. Subsequently, a left
anterolateral thoracotomy was undertaken through the fourth
intercostal space, with a right lateral position. At 5 min after
the injection of heparin (100 U/kg, i.v.), the left pulmonary
hilum, including the left main bronchus, artery and vein, was
occluded at the end of an expiration/breath with a non-invasive
microvascular clip for 1 h. At the end of the ischemic period, the
clip was removed and the lung regained ventilation and reperfusion
for 2 h. The rats of the sham group underwent sham surgery
consisting of a thoracotomy without clamping of the left pulmonary
hilum. Maintenance fluids (0.9% saline) were administered at 1.0
ml/h by tail vein for the duration of the I/R phase. At the end of
each experiment, all the rats were sacrificed by bleeding in the
right ventricle of the heart.
Experimental protocol and drug
administration
A total of 72 rats were randomly allocated to six
groups (n=12 per group) as follows: i) The sham group,
saline-treatment (1 ml/h i.v.) without I/R; ii) the I/R group,
saline-treatment (1 ml/h i.v.) for 1 h prior to I/R; iii) the
Dex2.5 group, i.v. infusion of dexmedetomidine at a dose of 2.5
μg/kg/h for 1 h prior to I/R; i.v.) the Dex5 group, i.v. infusion
of dexmedetomidine at a dose of 5 μg/kg/h for 1 h prior to I/R;
i.v.) the Dex+Yoh group, i.v. infusion of yohimbine (1.0 mg/kg,
injection process lasting no less than 5 min) followed by infusion
of dexmedetomidine at a dose of 5 μg/kg/h for 1 h prior to I/R and
v) the Yoh group, i.v. infusion of yohimbine (1.0 mg/kg, injection
process lasting no less than 5 min) followed by infusion of saline
at 1 ml/h for 1 h prior to I/R.
Arterial blood gas (ABG) analysis
At the end of each experiment, 0.5 ml blood was
drawn from the left ventricle of the heart. ABG levels were
immediately measured with a blood gas analyzer (GEM Premier 3000;
Instrumentation Laboratory Co., Bedford, MA, USA).
Bronchoalveolar lavage (BAL)
For six rats of each group, the right main bronchus
was tied and the left lung was lavaged five times with 10 ml cold
sterile saline (14). Once the BAL
fluid (BALF) had been collected and centrifuged at 3,200 × g, 4°C
(Eppendorf 5840R; Eppendorf, Hamburg, Germany), the BALF
supernatant was obtained for further analysis of the levels of
TNF-α, IL-6 and MCP-1 by enzyme-linked immunosorbent assay (ELISA;
TNF-α, IL-6 and MCP-1 ELISA kits; R&D Systems, Inc.,
Minneapolis, MN, USA).
Perfusion fixation and histopathological
analysis
The left lung tissues from the six rats of each
group were perfused with 4% formaldehyde and then removed. The
formaldehyde-infused left lungs were embedded in paraffin wax,
sectioned (5 μm) and stained with hematoxylin and eosin. The
histological changes were scored by a pathologist in a blinded
manner. The lung injury was classed using a score of 0 to 12 (grade
0, 1, 2 or 3 standing for normal, mild, moderate or severe,
respectively) for intra-alveolar edema, intra-alveolar hemorrhage
and neutrophil infiltration (15).
Wet/dry (w/d) weight ratio and
myeloperoxidase (MPO) activity assay
For the other six rats of each group, the left main
bronchus was tied and the left lung was removed after the rats had
been sacrificed. The upper and lower lobes of the left lung were
divided, and the lower lobes were snap-frozen in liquid nitrogen
and stored at −70°C for the MPO activity assay and for total RNA
and protein extraction. The left upper lobe of the lung tissue was
immediately weighed following harvest to obtain the wet weight and
again following desiccation in an oven at 60°C for 48 h to obtain
the dry weight. The lung water content was assessed by the w/d
ratio. In addition, a 100 mg snap-frozen left lower lobe lung
sample was homogenized in cold saline, and the MPO activity was
measured with an MPO assay kit, according to the manufacturer’s
instructions (Nanjing Jiancheng Bioengineering Institute, Nanjing,
Jiangsu, China). The results are expressed as units per gram of
protein.
Quatitative PCR (qPCR) assay of TLR4 and
MyD88 mRNA
The mRNA expression of TLR4 and MyD88 was analyzed
by qPCR. The total RNA was extracted by homogenization of the lung
tissue in TRIzol reagent (Invitrogen Life Technologies, Carlsbad,
CA, USA). In total, 5 μg total RNA was reverse-transcribed into
cDNA, and the PCR reaction mixtures were prepared using SYBR Green
qPCR master mix (Toyobo Co., Ltd., Osaka, Japan). β-actin, a
housekeeping gene, was used as the internal control. Primers (Huada
Gene, Beijing, China) were designed with sequences as follows:
Forward: 5′-GAATGAGGACTGGGTGAGAAAC-3′ and reverse:
5′-ACCAACGGCTCTGGATAAAGT-3′ for TLR4; Forward:
5′-ACCGCATCGAGGAGGACTG-3′ and reverse: 5′-CTGTGGGACACTGCTCTCCA-3′
for MyD88; and forward: 5′-AGGCCCCTCTGAACCCTAAG-3′ and reverse:
5′-CCAGAGGCATACAGGGACAAC-3′ for β-actin. The relative expression
levels of TLR4 and MyD88 mRNA in the lung tissues were determined
by the 2−ΔΔCT method (16) following normalization to the
housekeeping gene, β-actin.
Western blotting
Snap-frozen lung tissue (50 mg) was homogenized and
centrifuged at 12,000 × g at 4°C for 20 min, and the supernatant
was collected. The protein concentration was determined by a
bicinchoninic acid protein assay (Proteintech, Wuhan, Hubei,
China). Samples with equal quantities of protein were mixed with 5X
SDS sample buffer (Dingguo Changsheng Biotechnology Co., Ltd,
Beijing, China) and then boiled for 5 min. Aliquots of the samples
were separated on a 10% Tris-glycine gel and electrophoresed.
Following transfer to nitrocellulose membranes, the samples were
blocked by 5% skimmed milk powder in Tris-buffered saline with
Tween 20 (30 mM Tris-HCl, 125 mM NaCl and 0.1% Tween-20) for 1 h at
room temperature, and then incubated overnight at 4°C with rabbit
polyclonal antibodies against phosphorylated ERK (P-ERK) or total
ERK and JNK (Santa Cruz Biotechnology, Inc., Santa Cruz, CA, USA).
Subsequent to being washed, the primary antibodies were
counterstained with horseradish peroxidase-conjugated
goat-anti-rabbit IgG antibody (Cell Signaling Technology, Inc.,
Danvers, MA, USA), visualized with enhanced chemiluminescence
detection reagents (Merck Milipore, Darmstadt, Germany) and finally
exposed to photographic film for a suitable length of time. The
images were analyzed using Image J software, and the ratios of
P-ERK/ERK and P-JNK/JNK provided a measurement of the ERK and JNK
phosphorylation levels.
Statistical analysis
All data are presented as the mean ± standard
deviation. The experimental results were analyzed by SPSS 17.0
software (SPSS, Inc., Chicago, IL, USA). The differences among
groups were assessed by one-way analysis of variance with the
Bonferroni test for variances. P<0.05 was considered to indicate
a statistically significant difference.
Results
Lung histology
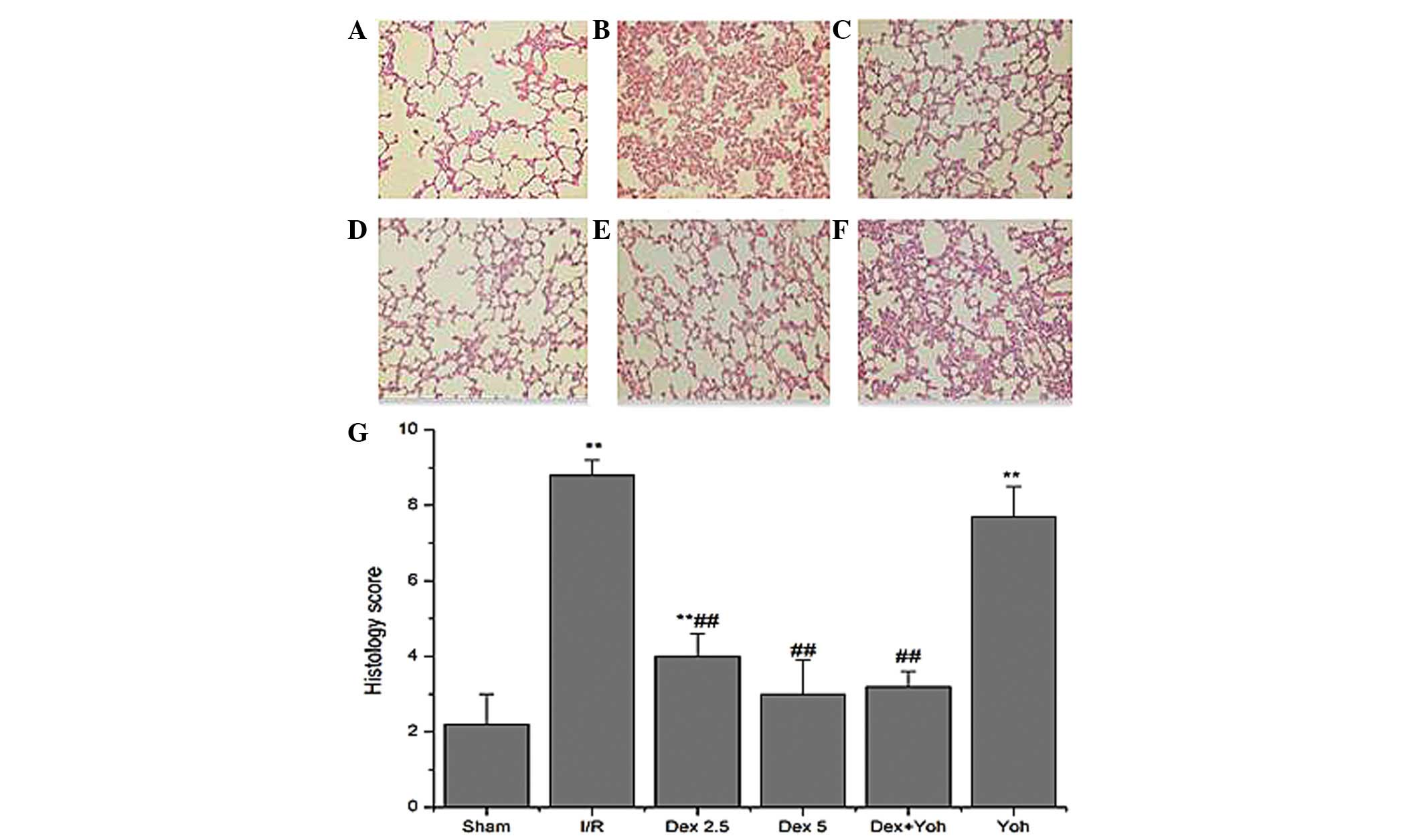
The histological analysis showed minimal lung injury
in the rats of the sham group (Fig.
1A) and severe lung injury in the rats of the I/R (Fig. 1B) and Yoh (Fig. 1F) groups. By contrast, the lung
tissues harvested from the rats of the Dex2.5 (Fig. 1C), Dex5 (Fig. 1D) and Dex+Yoh (Fig. 1E) groups revealed mild to moderate
damage compared with that of the sham group, respectively. The lung
injury scores paralleled the histological findings. The lung injury
scores of the I/R (8.8±0.4; P<0.01) and Yoh (7.7±0.8; P<0.01)
groups were significantly higher compared with that of the sham
group (2.2±0.8), whereas those of the Dex2.5 (4.0±0.6; P<0.01),
Dex5 (3.0±0.9; P<0.01) and Dex+Yoh (3.2±0.4; P<0.01) groups
were significantly lower compared with that of the I/R group, but
there was no significant difference among them (Fig. 1G).
ABG data, w/d weight ratio and MPO
activity
The pH, PaO2, PaCO2 and base
excess values exhibited no significant differences among the six
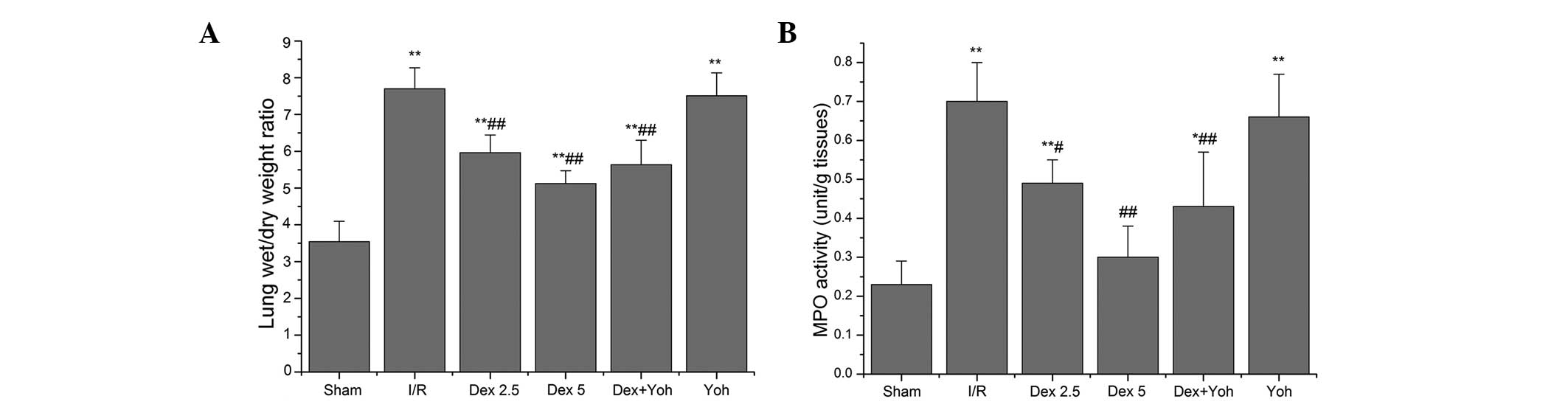
groups (Table I). The lung w/d
weight ratio was measured following reperfusion to evaluate the
I/R-induced lung edema. In the I/R group, the ratio (7.70±0.57) was
significantly increased compared with that of the sham group
(3.54±0.56; P<0.01). The ratio was significantly decreased
following pre-administration of dexmedetomidine (Dex2.5 group,
5.96±0.48; and Dex5 group, 5.12±0.35) prior to lung ischemia
compared with that of the I/R group (all P<0.01). However,
yohimbine failed to reverse the effect of dexmedetomidine on the
lung w/d weight ratio, and there was no significant difference in
the w/d ratio between the Yoh (7.51±0.62; P>0.05) and I/R groups
(Fig. 2A).
 | Table IABG data. |
Table I
ABG data.
| Group (n=12) | pH | PaO2,
mmHg | PaCO2,
mmHg | Base excess,
mM |
|---|
| Sham | 7.19±0.22 | 139.3±28.4 | 26.0±5.4 | −16.5±8.0 |
| I/R | 7.23±0.16 | 119.5±22.2 | 31.0±6.2 | −13.1±5.8 |
| Dex2.5 | 7.27±0.09 | 123.5±20.4 | 27.5±6.9 | −13.1±3.7 |
| Dex5 | 7.21±0.13 | 138.8±31.0 | 27.2±4.7 | −15.3±5.1 |
| Dex+Yoh | 7.28±0.07 | 128.7±11.7 | 27.7±4.2 | −11.8±1.9 |
| Yoh | 7.27±0.06 | 116.8±27.4 | 29.3±4.1 | −12.8±2.1 |
MPO activity, a biochemical marker of neutrophil
infiltration, rose to 0.70±0.10 in the lung of the I/R group
compared with that of the sham group (0.23±0.06; P<0.01).
Pre-treatment with dexmedetomidine resulted in a significant
reduction in the lung MPO activity of the Dex2.5 (0.49±0.06;
P<0.05) and Dex5 (0.30±0.08; P<0.01) groups compared with
that of the I/R group. However, yohimbine failed to reverse the
effect of dexmedetomidine on the lung MPO activity, and there was
no significant difference in MPO activity between the Yoh
(0.66±0.11; P>0.05) and I/R groups (Fig. 2B).
Effects of dexmedetomidine on the
concentration of TNF-α, IL-6 and MCP-1 in BALF
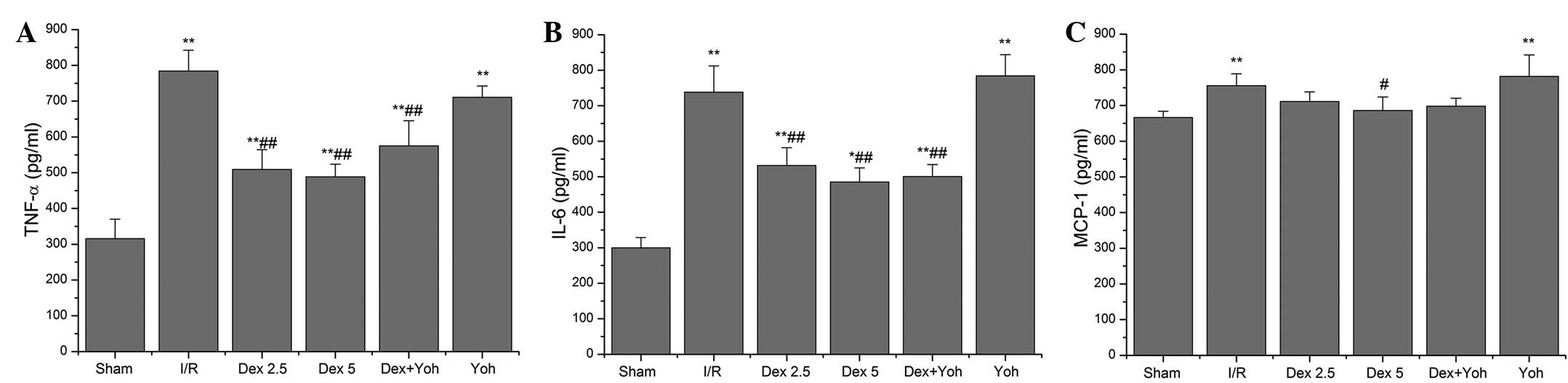
The ELISA analysis of BALF demonstrated that the
concentration of TNF-α, IL-6 and MCP-1 in the I/R (784.27±57.78,
738.02±73.84 and 755.55±33.36, respectively) and Yoh (710.71±31.67,
784.43±59.18 and 781.65±59.98, respectively) groups were
significantly higher compared with that of the sham group
(315.58±54.38, 299.79±28.90 and 666.31±17.16, respectively) (all
P<0.01) whereas the concentration of TNF-α, IL-6 and MCP-1 was
not significantly different between the I/R and Yoh groups. The
concentration of TNF-α and IL-6 in the Dex2.5 (509.21±55.10 and
531.56±49.97, respectively), Dex5 (488.13±35.93 and 484.94±39.96,
respectively) and Dex+Yoh (574.92±70.29 and 500.68±33.98,
respectively) groups were significantly lower compared with that of
the I/R group (all P<0.01), whereas the concentration of MCP-1
in the Dex2.5 (711.42±26.68) and Dex+Yoh (697.89±22.21) groups was
not significantly different compared with that of the I/R group
(all P>0.05), although dexmedetomidine significantly inhibited
the increase in MCP-1 concentration in the Dex5 group
(685.95±37.88; P<0.05) compared with that in the I/R group
(Fig. 3).
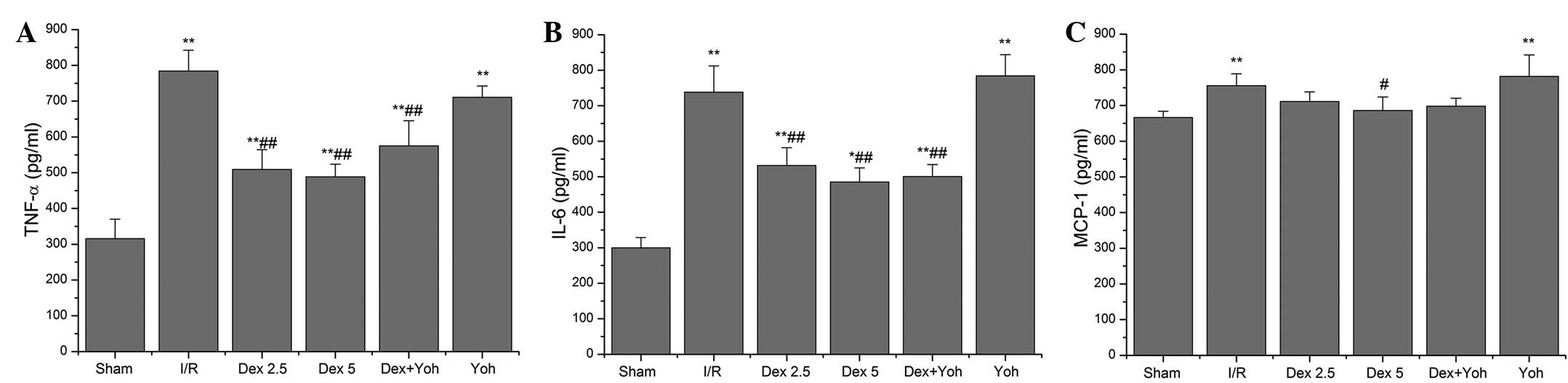 | Figure 3ELISA analysis of (A) TNF-α, (B)
IL-6, and (C) MCP-1 expression in BALF. The data are presented as
the mean ± standard deviation. *P<0.05 and
**P<0.01 vs. the sham group. TNF-α, tumor necrosis
factor α; IL-6, interleukin-6; MCP-1, monocyte chemoattractant
protein-1; BALF, bronchoalveolar lavage fluid; ELISA, enzyme-linked
immunosorbent assay; Dex, dexmedetomidine; Yoh, yohimbine; I/R,
ischemia-reperfusion. |
Dexmedetomidine relieves LIRI-induced
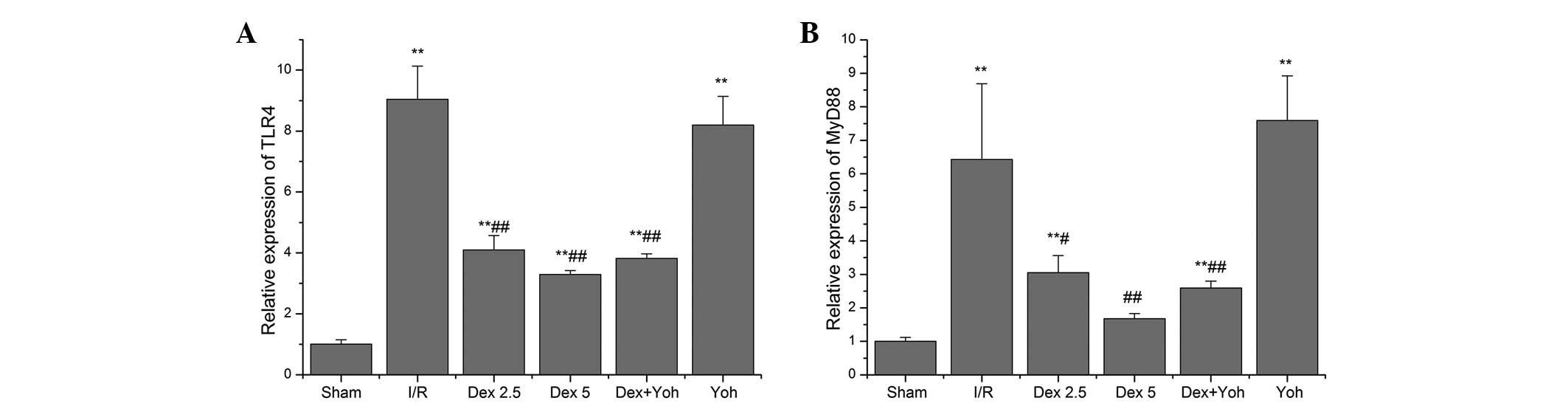
upregulation of TLR4 and MyD88 mRNA expression in the lung
The lung TLR4 mRNA expression of the I/R (9.04±1.09)
and Yoh (8.20±0.94) groups was significantly upregulated following
I/R compared with that of the sham group (1.01±0.14; P<0.01).
Pre-treatment with dexmedetomidine at a dose of either 2.5 μg/kg/h
(4.10±0.47; P<0.01, vs. the I/R group) or 5 μg/kg/h (3.29±0.13;
P<0.01, vs. the I/R group) significantly inhibited the
upregulation of TLR4 mRNA expression. However, yohimbine failed to
reverse the downregulative effects of dexmedetomidine on TLR4 mRNA
expression (Dex+Yoh group, 3.82±0.15; P<0.01, vs. the I/R group)
(Fig. 4A).
The change in MyD88 mRNA expression in the lung was
paralleled by that of the TLR4 mRNA expression (Fig. 4B). The MyD88 mRNA expression of the
I/R (6.43±2.26) and Yoh (7.59±1.33) groups was significantly
upregulated following I/R compared with that of the sham group
(1.0±0.12; P<0.01). Pre-treatment with dexmedetomidine at a dose
of either 2.5 μg/kg/h (3.05±0.51; P<0.05, vs. the I/R group) or
5μg/kg/h (1.68±0.15; P<0.01, vs. the I/R group) significantly
inhibited the upregulation of MyD88 mRNA expression. However,
yohimbine failed to reverse the downregulative effects of
dexmedetomidine on MyD88 mRNA expression (Dex+Yoh group, 2.59±0.21;
P<0.01, vs. the I/R group).
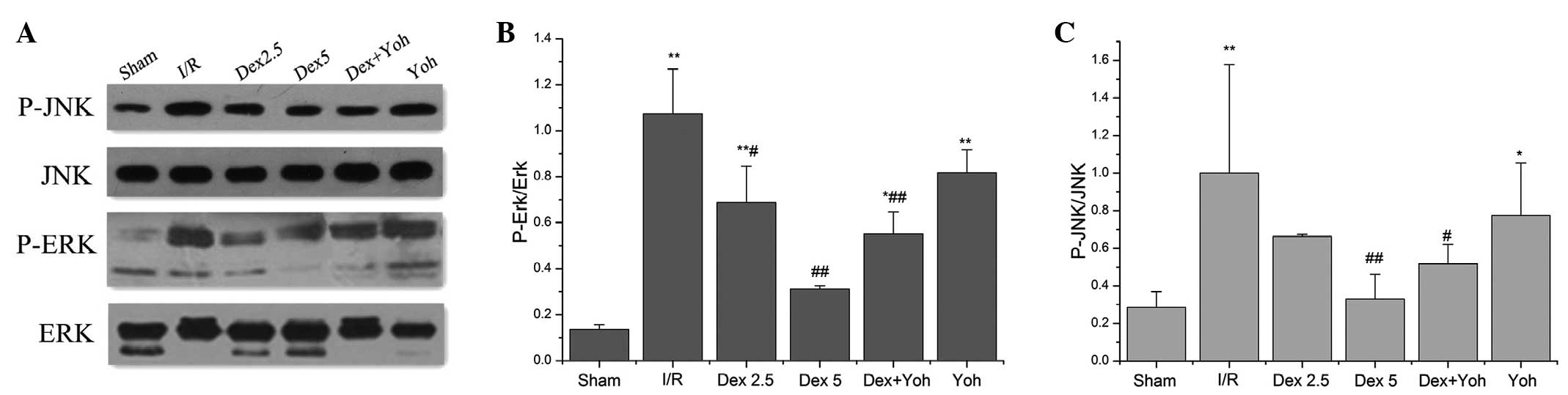
Effects of dexmedetomidine on P-JNK and
P-ERK
The levels of P-JNK in the I/R and Yoh groups were
significantly higher following I/R compared with that in the sham
group. Pre-treatment with dexmedetomidine at a dose of either 2.5
or 5 μg/kg/h significantly lowered the level of P-JNK compared with
that in the I/R group. However, yohimbine failed to reverse the
effect of dexmedetomidine on P-JNK, and yohimbine alone did not
affect the level of P-JNK compared with that in the I/R group
(Fig. 5).
The levels of P-ERK in the I/R and Yoh groups were
significantly higher following I/R compared with that in the sham
group. Pre-treatment with dexmedetomidine at a dose of 5 μg/kg/h
significantly lowered the level of P-ERK compared with that in the
I/R group, however, yohimbine failed to reverse its effect on
P-ERK. Notably, pre-treatment with dexmedetomidine at a dose of 2.5
μg/kg/h and yohimbine alone did not affect the level of P-ERK
compared with that in the I/R group (Fig. 5).
Discussion
LIRI is a complex phenomenon involving intracellular
injury processes, uncontrolled inflammatory processes and
biochemical changes. Human trials and animal experiments have
provided important descriptive information about the onset and
evolution of the physiological and inflammatory changes in the
lung. A body of evidence explains the possible mechanisms of LIRI
and multiple interventions, including pharmacological treatments,
such as adenosine α2 A agonist (17) and diazoxide (18), and other interventions, including
ischemic pre-conditioning (19)
and ischemic postconditioning (IPO) (20), have been administered to relieve
lung damage induced by I/R injury, which could compromise the full
benefit of reperfusion following ischemia. In the present study,
pre-administration of dexmedetomidine at a dose of 2.5 or 5 μg/kg/h
relieved the lung damage observed in the histological findings,
reduced the lung w/d weight ratio and MPO activity and decreased
the concentration level of inflammatory molecules, including TNF-α,
IL-6 and MCP-1, in BALF. Furthermore, the TLR4/MyD88/MAPK signaling
pathway was observed to be involved in the mechanism of the
protective effect of dexmedetomidine on the lung following I/R
injury, although an α2-adrenergic antagonist failed to
neutralize the effect of dexmedetomidine on acute ischemia-induced
lung injury.
High water content of the lung is a representative
symptom of acute lung injury. The present results demonstrated that
pre-administration of dexmedetomidine attenuated the development of
pulmonary edema, as indicated by the significant decrease in the
lung w/d weight ratio compared with the I/R group, although the ABG
result did not reveal a significant difference between the
pre-conditioned dexemdetomidine groups and the I/R group. In
addition, pre-treatment with dexmedetomidine suppressed the lung
MPO activity, which is a marker enzyme of neutrophils and is
released from azurophilic granules of neutrophils. The decrease in
MPO activity directly reflected the reduced infiltration of
neutrophils in the lung, contributing to reducing lung damage.
Dexmedetomidine also improved the lung histological examination.
These findings highlighted the potential protective effect of
dexmedetomidine on pulmonary injury induced by I/R, besides the
protection against brain I/R injury reported in previous studies
(21–24).
It is known that an increase in the level of
pro-inflammatory cytokines, including TNF-α and IL-6, is an early
feature of acute lung injury induced by clinical and experimental
I/R. The present data demonstrated that dexmedetomidine decreased
the concentrations of TNF-α, IL-6 and MCP-1 in BALF compared with
that of the I/R group. This anti-inflammatory action of
dexmedetomidine has been documented in previous studies. Nishina
et al (25) first reported
that clinically relevant concentrations of dexmedetomidine did not
affect the chemotaxis, phagocytosis or superoxide production by
human neutrophils or the intracellular calcium concentrations in
neutrophils stimulated by chemotaxin in vitro, indicating
that special precautions may not be required when using
dexmedetomidine in patients with infection, sepsis or systemic
inflammation. Subsequently, a body of animal and clinical trials
(26–29) reported that dexmedetomodine reduced
the level of plasma cytokines, including TNF-α, IL-1 and IL-6,
stimulated by endotoxemia, and that dexmedetomidine reduced the
mortality rate in endotoxemia-induced shock rat models in a
dose-dependent manner. In a lipopolysaccharide-induced acute lung
injury model (13),
dexmedetomidine improved congestion and edema and reduced the w/d
weight ratio and TNF-α, IL-1β and IL-6 levels in lung tissues. The
present study further revealed that dexmedetomidine may be involved
in the protection against sterile acute lung injury.
TLR4 is a transmembrane protein that is expressed in
alveolar macrophages, endothelial cells, monocytes and neutrophils,
and recognizes pathogen-associated molecular patterns and DAMPs
(30–32). A growing body of evidence links
TLR4/MyD88 signaling to the deleterious inflammatory effects
observed in organs following I/R injury (33–37).
In the LIRI mouse model, TLR4−/− mice demonstrated a
reduction in vascular permeability, lung MPO activity and the
levels of several proinflammatory cytokines/chemokines in BALF
samples compared with those from wild-type mice. In accordance with
that result, upregulation of TLR4 mRNA was observed in the lung in
the I/R group compared with that in the sham group, and
pre-treatment with dexmedetomidine downregulated the expression of
TLR4 and MyD88 mRNA, as the downstream signal molecule of TLR4 in
the lung, compared with that in the I/R group. Correspondingly, the
change trends of the TNF-α, IL-6 and MCP-1 concentrations in BALF
were consistent with the TLR4 and MyD88 mRNA expression in the
lung, indicating that TLR4/MyD88 signaling may be involved in the
anti-inflammatory mechanism of dexmedetomidine to inhibit LIRI.
TLR4/MyD88 signaling ultimately leads to the
activation of NF-κB and certain MAPKs, e.g., p38, ERK1/2 and JNK,
which result in the production of inflammatory cytokines, TNF-α and
IL-6, following I/R injury (38,39).
The present study demonstrated that LIRI increased the
phosphorylation of JNK and ERK rather than p38 (data not shown) in
the I/R group compared with the sham group. Pre-treatment with
dexmedetomidine reduced the expression of P-JNK and P-ERK1/2
proteins in the lung compared with those in the I/R group. However,
in an intestinal I/R-induced remote lung injury model, inhibition
of p38 activation has been shown to alleviate neutrophil
infiltration and lung cytokine expression rather than JNK or ERK1/2
(38). Zanotti et al
(39) reported that functioning
TLR4 results in the early phosphorylation of p38 observed during
ischemia and the early phosphorylation of ERK and JNK following
reperfusion, associated with inflammation rather than lung w/d
weight ratio in mouse LIRI. The difference in the MAPK activity
between the data of the present study and previous results may be
attributable to the difference in the models, the animals or the
observation time.
Notably, administration of the
α2-adrenoceptor antagonist, yohimbine, prior to
dexmedetomidine pre-treatment failed to completely eliminate the
effect of dexmedetomidine on TLR4 expression, the phosphorylation
of JNK and ERK and the production of inflammatory cytokines in
BALF, indicating that the anti-inflammatory mechanism of
dexmedetomidine may be associated with an
α2-adrenoceptor-independent signaling pathway, although
dexmedetomidine may attenuate the excessive release of plasma
noradrenaline induced by ischemia by the activation of presynaptic
α2-adrenoceptor, contributing to the relief of the
inflammatory response. Gu et al (7) demonstrated that dexmedetomidine
markedly reduces renal I/R induced pulmonary injuries and lowers
the MPO activity and cytokine expression, but the
α2-adrenoceptor antagonist, atipamezole, partially
reverses the protective effects of dexmedetomidine in the lung and
has no effect on the cytokine expression level. In addition, by
acting through the I1 imidazoline receptor, dexmedetomidine has
been shown to exhibit a pattern of neuroprotective action in
hippocampal slices obtained from rats (40), while its action through the I2
imidazoline receptor has been shown to reduce cell apoptosis and
necrosis to protect against oxygen-glucose deprivation-induced
injury in rat C6 cells in an in vitro model of ischemia
(41). The activation of the
varying receptors induced by dexmedetomidine may play a protective
role through a different mechanism to that of organ I/R injury.
Several limitations exist for the present study.
This study lacked analysis of the time-associated effects of
dexmedetomidine on the inflammatory response to LIRI. Therefore,
the possibility that dexmedetomidine affected the extent of
expression of various inflammatory cytokines and proteins may not
be ruled out. In addition, dexmedetomidine has an analgesic effect
(42). By contrast, no analgesic
was applied in the I/R group. Therefore, the question of whether
the analgesic peculiarity of dexmedetomidine is likely to play a
role remains to be elucidated. Furthermore, the effect of
dexmedetomidine on the activation of NF-κB following LIRI was not
examined, therefore the possibility that TLR4/NF-κB signaling is
involved in the anti-inflammatory mechanism of dexmedetomidine
against LIRI may not be ruled out.
The present study demonstrated that lung I/R
upregulated TLR4 and MyD88 mRNA expression and P-JNK and P-ERK1/2
protein expression in lung tissue, and increased the concentration
levels of TNF-α, IL-6 and MCP-1 in BALF. Pre-administration of
dexmedetomidine prior to I/R reduced pulmonary damage in the
histological results and decreased MPO activation in lung tissue
and the concentration levels of proinflammatory cytokines in BALF
through the TLR4/MyD88/MAPK signaling pathway. Our study provides a
potential clinical application of dexmedetomidine for reducing lung
ischemia-reperfusion injury in an experimental model.
References
|
1
|
Christie JD, Carby M, Bag R, Corris P,
Hertz M and Weill D; ISHLT Working Group on Primary Lung Graft
Dysfunction. Report of the ISHLT Working Group on Primary Lung
Graft Dysfunction part II: definition. A consensus statement of the
International Society for Heart and Lung Transplantation. J Heart
Lung Transplant. 24:1454–1459. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ng CS, Wan S, Yim AP and Arifi AA:
Pulmonary dysfunction after cardiac surgery. Chest. 121:1269–1277.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shimamoto A, Pohlman TH, Shomura S,
Tarukawa T, Takao M and Shimpo H: Toll-like receptor 4 mediates
lung ischemia-reperfusion injury. Ann Thorac Surg. 82:2017–2023.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ambrosio G and Tritto I: Reperfusion
injury: experimental evidence and clinical implications. Am Heart
J. 138:S69–S75. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Reino DC, Pisarenko V, Palange D, et al:
Trauma hemorrhagic shock-induced lung injury involves a
gut-lymph-induced TLR4 pathway in mice. PLoS One. 6:e148292011.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhao M, Fernandez LG, Doctor A, et al:
Alveolar macrophage activation is a key initiation signal for acute
lung ischemia-reperfusion injury. Am J Physiol Lung Cell Mol
Physiol. 291:L1018–L1026. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gu J, Chen J, Xia P, Tao G, Zhao H and Ma
D: Dexmedetomidine attenuates remote lung injury induced by renal
ischemia-reperfusion in mice. Acta Anaesthesiol Scand.
55:1272–1278. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Taniguchi T, Kidani Y, Kanakura H,
Takemoto Y and Yamamoto K: Effects of dexmedetomidine on mortality
rate and inflammatory responses to endotoxin-induced shock in rats.
Crit Care Med. 32:1322–1326. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Memis̨ D, Hekimoğlu S, Vatan I, Yandim T,
Yüksel M and Süt N: Effects of midazolam and dexmedetomidine on
inflammatory responses and gastric intramucosal pH to sepsis, in
critically ill patients. Br J Anaesth. 98:550–552. 2007.PubMed/NCBI
|
|
10
|
Yang CL, Tsai PS and Huang CJ: Effects of
dexmedetomidine on regulating pulmonary inflammation in a rat model
of ventilator-induced lung injury. Acta Anaesthesiol Taiwan.
46:151–159. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Arumugam TV, Okun E, Tang SC, Thundyil J,
Taylor SM and Woodruff TM: Toll-like receptors in
ischemia-reperfusion injury. Shock. 32:4–16. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Prakash A, Mesa KR, Wilhelmsen K, Xu F,
Dodd-o JM and Hellman J: Alveolar macrophages and Toll-like
receptor 4 mediate ventilated lung ischemia reperfusion injury in
mice. Anesthesiology. 117:822–835. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Shi QQ, Wang H and Fang H: Dose-response
and mechanism of protective functions of selective alpha-2 agonist
dexmedetomidine on acute lung injury in rats. Saudi Med J.
33:375–381. 2012.PubMed/NCBI
|
|
14
|
Yang CL, Chen CH, Tsai PS, Wang TY and
Huang CJ: Protective effects of dexmedetomidine-ketamine
combination against ventilator-induced lung injury in endotoxemia
rats. J Surg Res. 167:e273–e281. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yang CH, Tsai PS, Wang TY and Huang CJ:
Dexmedetomidine-ketamine combination mitigates acute lung injury in
haemorrhagic shock rats. Resuscitation. 80:1204–1210. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) Method. Methods. 25:402–408. 2001.
|
|
17
|
Emaminia A, Lapar DJ, Zhao Y, et al:
Adenosine A2A agonist improves lung function during ex
vivo lung perfusion. Ann Thorac Surg. 92:1840–1846. 2011.
|
|
18
|
Guo W, Ge D, Wang Q, et al: Diazoxide
decreases ischemia-reperfusion injury in a rat model of lung
transplantation. Transplant Proc. 43:2510–2516. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Jan WC, Chen CH, Tsai PS and Huang CJ:
Limb ischemic preconditioning mitigates lung injury induced by
haemorrhagic shock/resuscitation in rats. Resuscitation.
82:760–766. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Xu B, Gao X, Xu J, et al: Ischemic
postconditioning attenuates lung reperfusion injury and reduces
systemic proinflammatory cytokine release via heme oxygenase 1. J
Surg Res. 166:e157–e164. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Dahmani S, Rouelle D, Gressens P and Mantz
J: Characterization of the postconditioning effect of
dexmedetomidine in mouse organotypic hippocampal slice cultures
exposed to oxygen and glucose deprivation. Anesthesiology.
112:373–383. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Hoffman WE, Kochs E, Werner C, Thomas C
and Albrecht RF: Dexmedetomidine improves neurologic outcome from
incomplete ischemia in the rat. Reversal by the alpha 2-adrenergic
antagonist atipamezole. Anesthesiology. 75:328–332. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Eser O, Fidan H, Sahin O, et al: The
influence of dexmedetomidine on ischemic rat hippocampus. Brain
Res. 1218:250–256. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Cosar M, Eser O, Fidan H, et al: The
neuroprotective effect of dexmedetomidine in the hippocampus of
rabbits after subarachnoid hemorrhage. Surg Neurol. 71:54–59. 2009.
View Article : Google Scholar
|
|
25
|
Nishina K, Akamatsu H, Mikawa K, et al:
The effects of clonidine and dexmedetomidine on human neutrophil
functions. Anesth Analg. 88:452–458. 1999.
|
|
26
|
Tasdogan M, Memis D, Sut N and Yuksel M:
Results of a pilot study on the effects of propofol and
dexmedetomidine on inflammatory responses and intraabdominal
pressure in severe sepsis. J Clin Anesth. 21:394–400. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Taniguchi T, Kurita A, Kobayashi K,
Yamamoto K and Inaba H: Dose- and time-related effects of
dexmedetomidine on mortality and inflammatory responses to
endotoxin-induced shock in rats. J Anesth. 22:221–228. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Sezer A, Memis̨ D, Usta U and Süt N: The
effect of dexmedetomidine on liver histopathology in a rat sepsis
model: an experimental pilot study. Ulus Travma Acil Cerrahi Derg.
16:108–112. 2010.PubMed/NCBI
|
|
29
|
Qiao H, Sanders RD, Ma D, Wu X and Maze M:
Sedation improves early outcome in severely septic Sprague Dawley
rats. Crit Care. 13:R1362009. View
Article : Google Scholar : PubMed/NCBI
|
|
30
|
Arslan F, Keogh B, McGuirk P and Parker
AE: TLR2 and TLR4 in ischemia reperfusion injury. Mediators
Inflamm. 2010:7042022010. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Li Y, Xiang M, Yuan Y, et al: Hemorrhagic
shock augments lung endothelial cell activation: role of temporal
alterations of TLR4 and TLR2. Am J Physiol Regul Integr Comp
Physiol. 297:R1670–R1680. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Fan J, Li Y, Vodovotz Y, Billiar TR and
Wilson MA: Hemorrhagic shock-activated neutrophils augment TLR4
signaling-induced TLR2 upregulation in alveolar macrophages: role
in hemorrhage-primed lung inflammation. Am J Physiol Lung Cell Mol
Physiol. 290:L738–L746. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Gao Y, Fang X, Sun H, et al: Toll-like
receptor 4-mediated myeloid differentiation factor 88-dependent
signaling pathway is activated by cerebral ischemia-reperfusion in
hippocampal CA1 region in mice. Biol Pharm Bull. 32:1665–1671.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Feng Y, Zhao H, Xu X, et al: Innate immune
adaptor MyD88 mediates neutrophil recruitment and myocardial injury
after ischemia-reperfusion in mice. Am J Physiol Heart Circ
Physiol. 295:H1311–H1318. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Hua F, Ha T, Ma J, et al: Blocking the
MyD88-dependent pathway protects the myocardium from
ischemia/reperfusion injury in rat hearts. Biochem Biophys Res
Commun. 338:1118–1125. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Wang S, Schmaderer C, Kiss E, et al:
Recipient Toll-like receptors contribute to chronic graft
dysfunction by both MyD88- and TRIF-dependent signaling. Dis Model
Mech. 3:92–103. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Wu H, Chen G, Wyburn KR, et al: TLR4
activation mediates kidney ischemia/reperfusion injury. J Clin
Invest. 117:2847–2859. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ben DF, Yu XY, Ji GY, et al: TLR4 mediates
lung injury and inflammation in intestinal ischemia-reperfusion. J
Surg Res. 174:326–333. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Zanotti G, Casiraghi M, Abano JB, et al:
Novel critical role of Toll-like receptor 4 in lung
ischemia-reperfusion injury and edema. Am J Physiol Lung Cell Mol
Physiol. 297:L52–L63. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Dahmani S, Paris A, Jannier V, et al:
Dexmedetomidine increases hippocampal phosphorylated extracellular
signal-regulated protein kinase 1 and 2 content by an alpha
2-adrenoceptor-independent mechanism: evidence for the involvement
of imidazoline I1 receptors. Anesthesiology. 108:457–466. 2008.
View Article : Google Scholar
|
|
41
|
Zhang F, Ding T, Yu L, Zhong Y, Dai H and
Yan M: Dexmedetomidine protects against oxygen-glucose
deprivation-induced injury through the I2 imidazoline
receptor-PI3K/AKT pathway in rat C6 glioma cells. J Pharm
Pharmacol. 64:120–127. 2012. View Article : Google Scholar
|
|
42
|
Afonso J and Reis F: Dexmedetomidine:
current role in anesthesia and intensive care. Rev Bras Anestesiol.
62:118–133. 2012. View Article : Google Scholar : PubMed/NCBI
|