Introduction
Due to the concealed location of onset and a lack of
clear symptoms in the early stages, the majority of hypopharyngeal
carcinoma patients are in the advanced stage when diagnosed and
this results in substantial morbidity and mortality (1). The traditional treatment option for
terminal hypopharyngeal carcinoma is surgical resection (2). This strategy, however, has evolved
from the point of view of pure treatment to maximize preservation
of hypopharyngeal function, placing emphasis upon the quality of
life of these patients. Consequently, the standard approach for the
treatment of these patients is radiotherapy and chemotherapy
(3). Taxol or cisplatin (DDP) are
used for treatment. However, chemoresistance and anti-apoptotic
characteristics of cancer cells are a major obstacle for effective
chemotherapy. A study has demonstrated that several molecules,
including ATP-binding cassette (ABC) genes and
anti-apoptotic-associated proteins have lead to the development of
the multi-drug resistance (MDR) phenotype of cancer cells. The
expression of ABC transporters and anti-apoptotic proteins result
in an ATP-driven efflux of antitumor drugs from the interior of
cancer cells and thereby led to decreased intracellular drug
accumulation and failure to induce apoptosis (4).
To reverse these malignant characteristics, a
substantial amount of effort has been dedicated to developing novel
drugs. In recent years, increased attention has been paid to the
proteasome pathway, which is crucial in the regulation of the cell
cycle, differentiation and apoptosis in a number of normal cellular
processes (5). Several studies
have investigated the potential anticancer capacity of proteasome
inhibitors in vitro and in vivo. As a strong
proteasome inhibitor, MG132 has been verified to downregulate the
MDR protein P-glycoprotein (P-gp) and anti-apoptotic protein Bcl-2
(6). Furthermore, it is also able
to increase the expression of apoptosis-related proteins Bax and
caspase-3 (7,8). This has warranted further
investigation of MG132. However, at present, the mechanisms
underlying the effect of MG132 remain largely unknown, particularly
in head and neck squamous cell carcinoma (HNSCC). In the present
study, , to the best of our knowledge, MG132 was introduced for the
first time into the FaDu/T hypopharyngeal cancer cell line,
established by exposing hypopharyngeal carcinoma FaDu cell lines to
escalating concentrations of Taxol (FaDu/T) as demonstrated in our
previous study (9). In addition,
the present study aimed to determine whether MG132 is able to
further reverse malignant behavior, including MDR and
anti-apoptotic characteristics.
Materials and methods
Materials
The FaDu human hypopharyngeal carcinoma cell line
was obtained from the American Type Culture Collection (Manassas,
VA, USA). The media and serum were purchased from Gibco-BRL
(Carlsbad, CA, USA). The chemotherapeutic drugs DDP, 5-fluorouracil
(5-FU), doxorubicin (Dox) and vincristine (VCR) were purchased from
Sigma (St. Louis, MO, USA). Primary antibodies, including
anti-MDR1/P-gp, anti-β-actin, anti-nuclear factor
κ-light-chain-enhancer of activated B cells (NF-κB), anti-p53 and
anti-lamin A were all purchased from Santa Cruz Biotechnology, Inc.
(Santa Cruz, CA, USA). All other agents were obtained from
Sigma.
Cell culture and the establishment of the
resistant cell line FaDu/T
FaDu cells were cultured as a monolayer in
Dulbecco’s modified Eagle’s medium (Gibco-BRL) containing 10% fetal
calf serum (Gibco-BRL), 100 U/ml penicillin (Sigma) and 100 mg
streptomycin (Sigma) at 37°C in a humidified atmosphere composed of
95% air and 5% CO2.
The establishment methods of the resistant cell line
FaDu/T have been previously described (9).
Cytotoxicity test
A 3-[4,5-dimethylthiazol-2-yl]-2,5
diphenyltetrazolium bromide (MTT) assay was employed to assess the
drug resistance sensitivities of FaDu/T-200 nM (resistant cell line
FaDu/T with a tolerance to Taxol of 200 nM). FaDu, FaDu/T and
FaDu/T + MG32 cells were diluted at a density of
15×104/ml, subcultured in 96-well plates (Corning Inc.,
Corning, NY, USA) and treated with different concentrations of Dox,
VCR, 5-FU and DDP for 72 h. MTT (5 mg/ml; 20 μl) was added to each
well 4 h prior to the indicated time points. Following 4 h of
incubation at 37°C, the medium was removed and the precipitate was
dissolved in dimethylsulfoxide. Then, optical density (OD) values
were measured at 570 nm using an ELISA reader (Multiskan MK3;
Thermo Labsystem, Waltham, MA USA). The relative viabilities of
cells were calculated according to the following formula: Cell
relative viability (%) = ODexperiment /
ODcontrol × 100 (ODblank was used as the
control). The IC50 was defined as the concentration
required to decrease the relative viabilities of cells to 50% of
that of the control (no drug) value.
Reverse transcription-polymerase chain
reaction (RT-PCR)
Total RNA was extracted using TRIzol reagent
(Invitrogen Life Technologies, Carlsbad, CA, USA). The reverse
transcription reaction was performed using the ExScript RT reagent
kit (Takara Bio, Inc., Dalian, China) in a final volume of 20 μl
containing 1 μg of total RNA, 4 μl of 5X ExScript buffer, 1 μl dNTP
mixture, 1 μl Oligo(dT) primer, 0.5 μl ExScript RTase, 0.5 μl RNase
inhibitor and RNase-free water to reach a volume of 20 μl. The
reverse transcription reaction was performed at 42°C for 15 min and
the reaction was terminated by heating at 95°C for 2 min. PCR was
performed according to the manufacturer’s instructions of Takara
TaqTM under the following conditions: Pre-degeneration at 95°C for
3 min, degeneration at 95°C for 60 sec, renaturation at 58°C for 45
sec and elongation at 72°C for 60 sec, for a total of 25 cycles.
All the experiments were conducted three times. The primers used
were as follows: Forward: 5′-CTGCTCAAGTTAAAGGGGCTAT-3′ and reverse:
5′-AACGGTTCGGAAGTTTTCTATT-3′ for ABCB1/P-gp; forward:
5′-GCTACGAGTGGGATACTGGAGA-3′ and reverse:
5′-AGTCATCCACAGAGCGATGTT-3′ for Bcl-2; forward:
5′-TCATCCAGGATCGAGCAGA-3′ and reverse: 5′-AAAGTAGAAGAGGGCAACCAC-3′
for Bax; forward: 5′-TTTGGAACGGACCTGT-3′ and reverse:
5′-CACGGGATCTGTTTCTTTGC-3′ for caspase-3; and forward:
5′-GTGGGGCGCCCCAGGCACCA-3′ and reverse:
5′-CTCCTTAATGTCACGCACGATTT-3′ for actin.
Western blot analysis
Total protein was extracted using radioimmune
precipitation protein lysis buffer according to the Protein
Extraction Technology Guide. Nuclear proteins were solubilized and
then fractionated by sodium dodecyl sulfate-polyacrylamide gel
electrophoresis.
The Bradford method was used to determine the
protein concentration of the supernatant. The samples (40 μg of
each total protein) were used for western blot analysis with the
primary antibodies (P-gp, 1:400, mouse anti-human; Bcl-2, 1:400
mouse anti-human; Bax, 1:400, rabbit anti-human; caspase-3, 1:400,
rabbit anti-human; actin, 1:2000, mouse anti-human; NF-κB, 1:200,
rabbit anti-human; p53, 1:200, mouse anti-human and lamin A, 1:200
rabbit anti-human). The bands of P-gp, Bcl-2, Bax, caspase-3,
NF-κB, p53, lamin A and actin were visualized at apparent molecular
weights of 170, 26, 23, 32, 53, 76 and 43 kDa, respectively. The
relative OD ratio was calculated from three experiments by
comparison with actin with NIH software Image J (National
Institutes of Health, Bethesda, MD, USA).
Flow cytometric analysis for cell
apoptosis
For apoptosis assessment, Annexin V-fluorescein
isothiocyanate (FITC) and propidium iodide (PI) were used.
Following trypsinization, cells were resuspended in binding buffer
(20 μl) containing Annexin V-FITC (5 μl; 20 μg/ml) and PI (10 μl;
20 μg/ml) for at least 10 min at room temperature, and then binding
buffer (300 μl) was added prior to analysis with system II, version
3.0 software (Beckman Coulter, Miami, FL, USA).
Statistical analysis
Data are presented as the mean ± standard error of
the mean. Statistical calculations were performed using the SPSS
16.0 software package (SPSS Inc., Chicago, IL, USA). One-way
analysis of variance was applied for analysis. P<0.05 was
considered to indicate a statistically significant difference.
Results
Establishment of the taxol-resistant cell
line FaDu/T and cross-resistance profiles
As reported in our previous study, FaDu/T cells were
constructed and had MDR characteristics in Taxol, Dox, VCR, 5-FU
and DDP (9). However, this cross
resistance markedly decreased when FaDu/T cells were pretreated
with MG132 for 24 h and the respective IC50 values were
0.22±0.03, 2.52±0.28, 14.79±0.16, 2.07±0.23 and 5.87±0.49 μM. A
significant difference existed between FaDu and FaDu/T cells, and
FaDu/T and FaDu/T + MG132 cells (P<0.05; Table I).
 | Table IIC50 (mean ± standard
deviation). |
Table I
IC50 (mean ± standard
deviation).
| Chemotherapy
drug | FaDu | FaDu/T | FaDu/T + MG132 |
|---|
| Taxol (μM) | 0.13±0.02 |
15.32±3.22a |
0.22±0.03a |
| DDP (μg/ml) | 2.81±0.57 |
25.25±3.78a |
2.52±0.28a |
| 5-FU (μg/ml) | 15.85±3.61 |
347.99±46.95a |
14.79±0.16a |
| Dox (μM) | 1.88±0.59 |
59.07±9.03a |
2.07±0.23a |
| VCR (μM) | 6.70±2.31 |
66.97±4.84a |
5.87±0.49a |
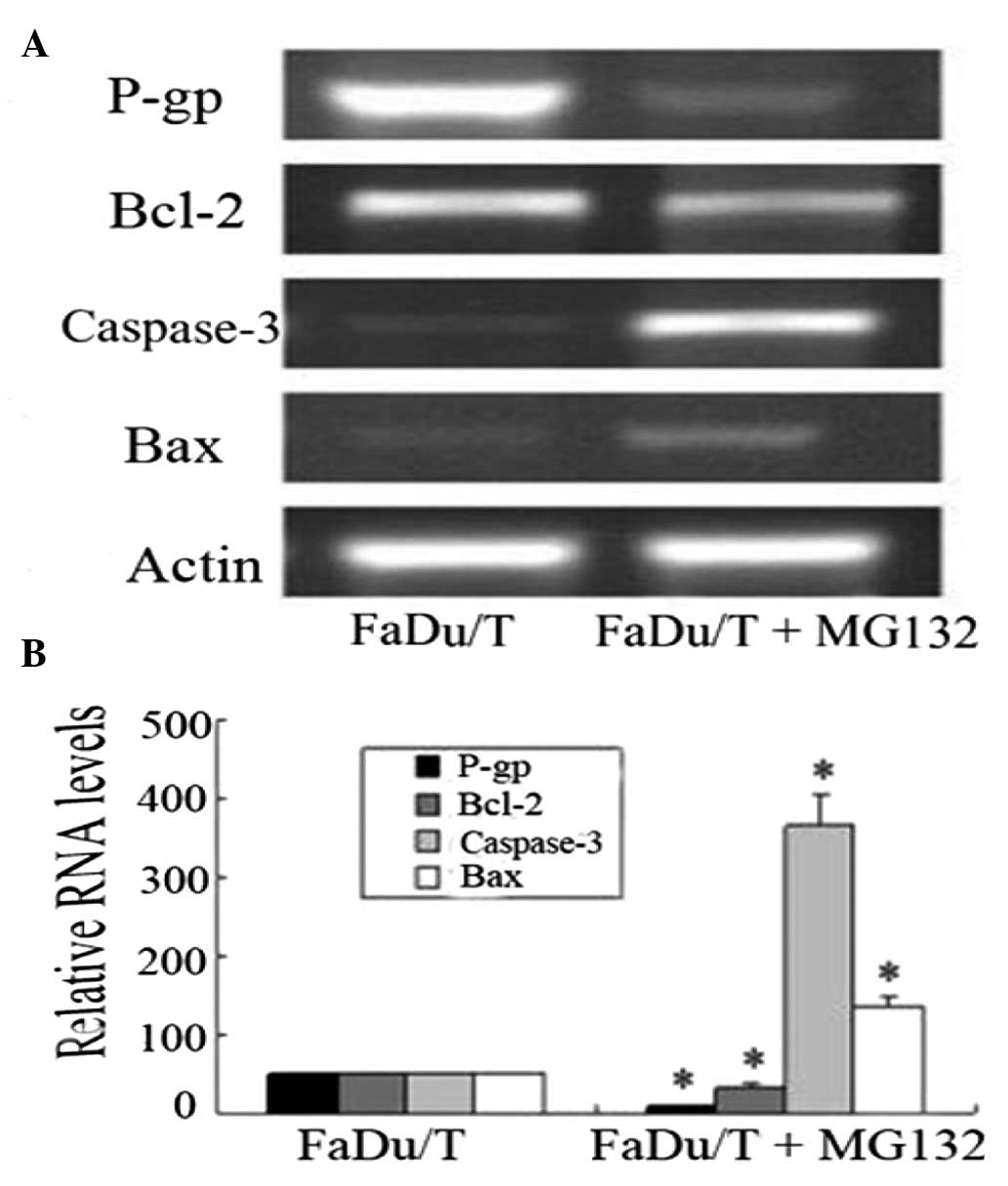
RNA levels of P-gp, Bcl-2, Bax and
caspase-3 in FaDu/T and FaDu/T + MG132 cells
Compared with FaDu/T cells, P-gp and Bcl-2 were
downregulated in FaDu/T + MG132 cells. However, the
apoptosis-related genes Bax and caspase-3, were upregulated. Image
J software was used to analyze the relative photo density, using
actin as a standard. Considering FaDu/T/actin as 100, the relative
photo densities of the FaDu/T + MG132 group was as follows:
P-gp/actin, 21.51±0.83; Bcl-2/actin, 38.89±2.96; caspase-3/actin,
733.52±79.29 and Bax/actin, 271.28±29.59. Statistical analysis
demonstrated that there was a significant difference in the levels
of all of these proteins between FaDu/T and FaDu/T + MG132 cells
(P<0.05; Fig. 1).
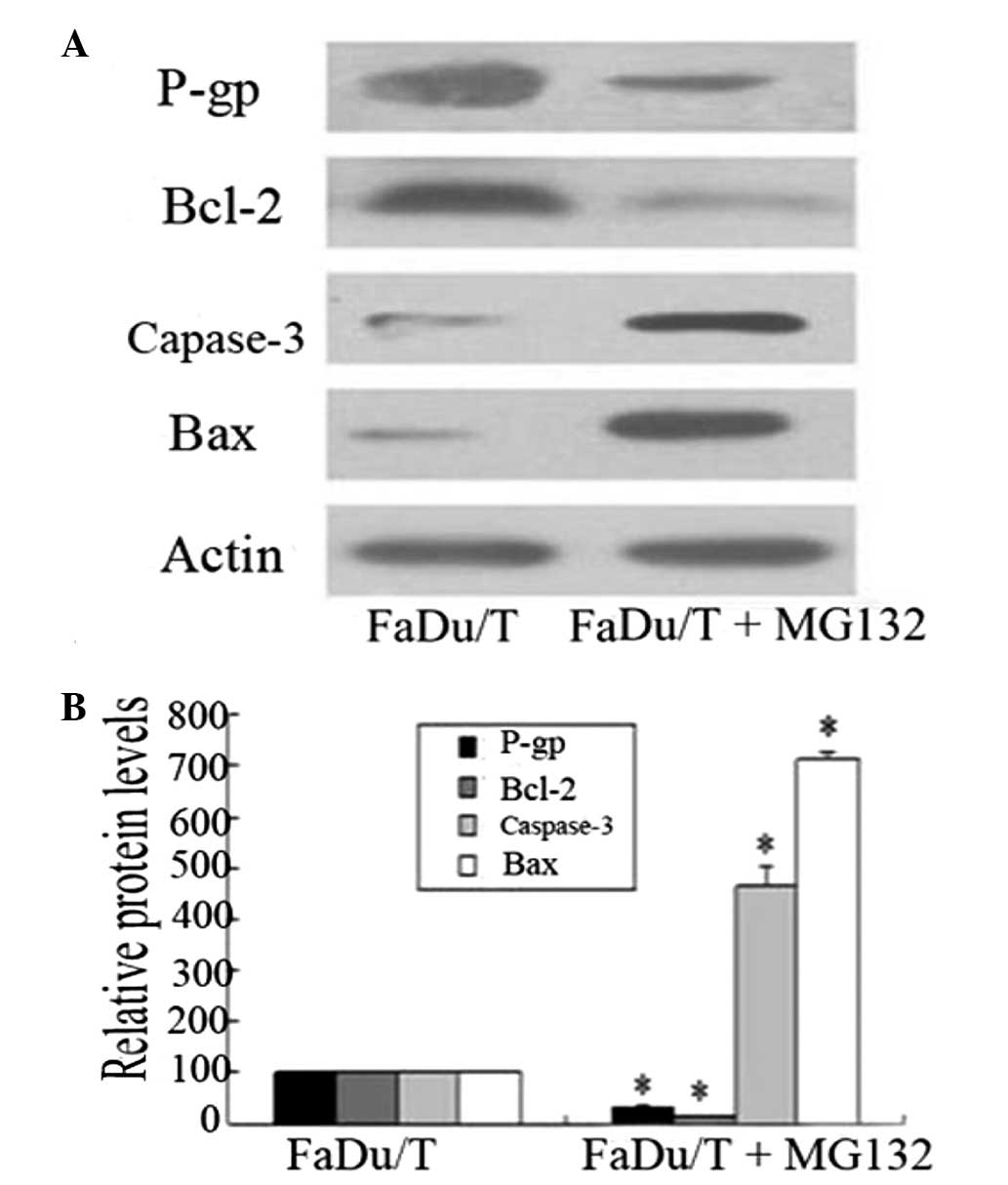
Protein levels of P-gp, Bcl-2, Bax and
caspase-3 in FaDu/T and FaDu/T + MG132 cells
The expression tendency of P-gp, Bcl-2, Bax and
caspase-3 protein levels was the same as the gene levels. Image J
software was used to analyze the relative photo density, using
actin as the standard. Considering FaDu/T/actin as 100, the
relative photo densities of the FaDu/T + MG132 groups were:
P-gp/actin, 33.73±3.67; Bcl-2/actin, 16.19±0.13; caspase-3/actin,
464.01 ± 38.38 and Bax/actin, 712.99 ± 13.28, respectively.
Statistical analysis demonstrated that there was a significant
difference between FaDu/T and FaDu/T + MG132 cells (P<0.05;
Fig. 2).
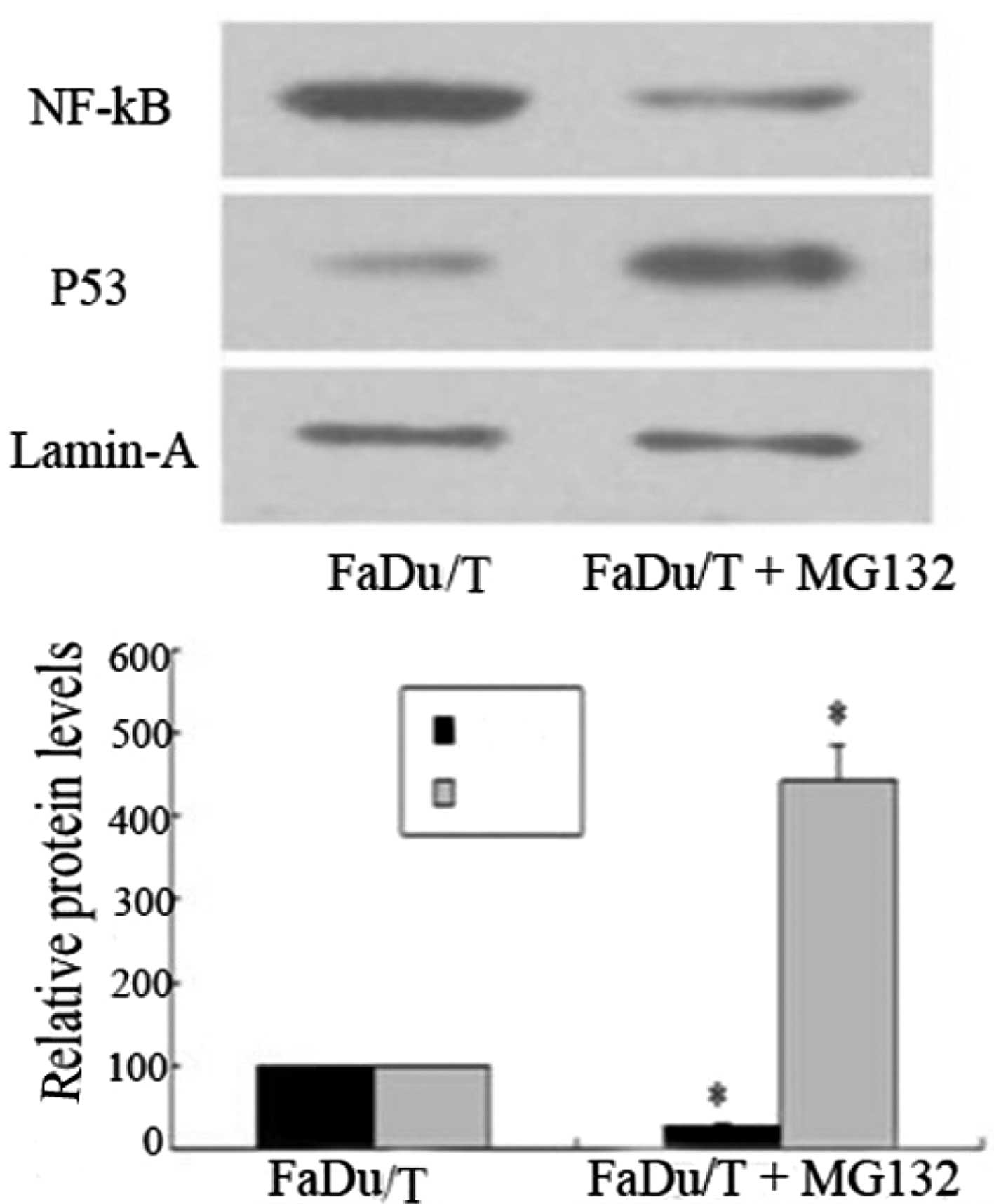
MG132 inhibits the nuclear translocation
of NF-κB, however, increases the expression of p53 in FaDu/T
cells
Compared with FaDu/T cells, the nuclear protein
levels of NF-κB expressed in the FaDu/T + MG132 cells increased
whereas the p53 levels decreased. Lamin A was used as the standard.
Considering FaDu/T/lamin A as 100, the relative photo densities of
FaDu/T + MG132/lamin A in NF-κB and p53 were 29.00±2.35 and
441.48±42.00, respectively. Statistical analysis demonstrated that
there was a significant difference between FaDu/T and FaDu/T +
MG132 cells (P<0.05; Fig.
3).
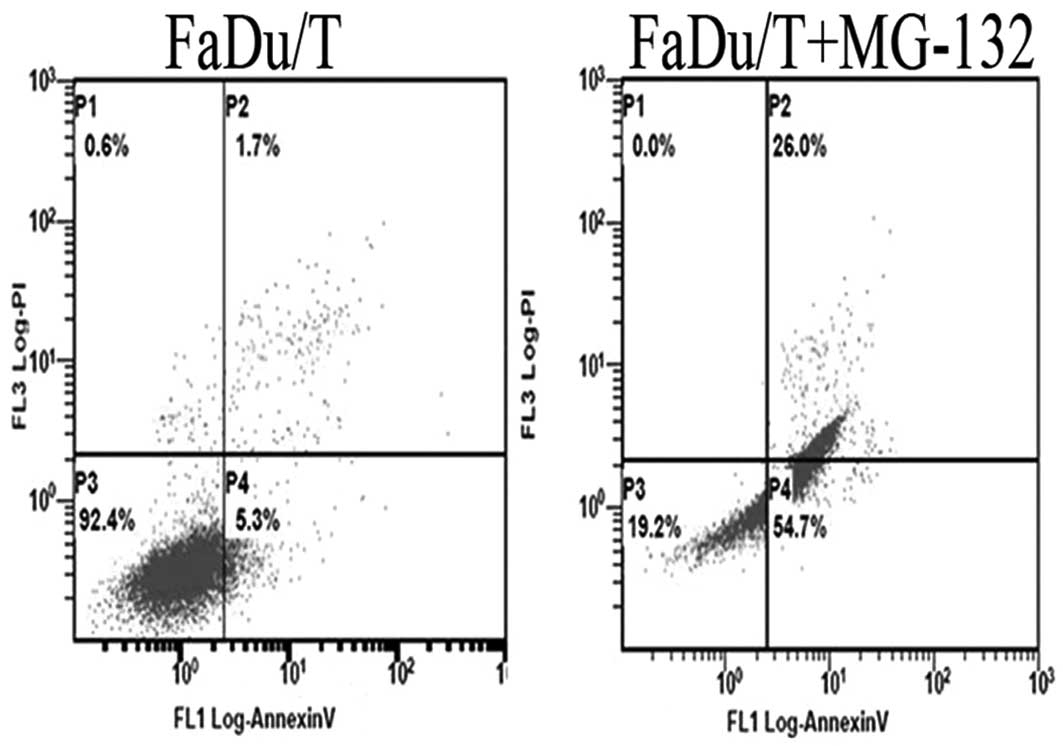
Different proportions of apoptotic cells
between FaDu/T and FaDu/T + MG132 cells
To assess the apoptotic induction capacity of MG132,
FaDu/T cells were treated with MG132 for 24 h and the proportions
of apoptotic cells were investigated. Compared with the apoptotic
rate of FaDu/T cells (4.45±1.60%), the rate in cells exposed to
MG132 was 32.9±2.39%. These results indicated that MG132 has a more
potent apoptotic induction capacity in FaDu/T cells (Fig. 4).
Discussion
Currently, the standard approach of advanced HNSCC
treatment, particularly hypopharyngeal carcinoma, is surgery
combined with radiotherapy and chemotherapy. In terms of
chemotherapy, MDR of cancer cells has always been a major problem
in treatment. To further investigate the MDR reversal of
hypopharyngeal cancer cells, based on the established MDR
hypopharyngeal carcinoma cell line FaDu/T, MG132 was introduced
into FaDu/T cells and the internal mechanisms of the effects of
MG132 were investigated.
Our previous study demonstrated that, compared with
FaDu cells, the expression of the MDR protein P-gp and
anti-apoptotic protein Bcl-2 markedly increased in FaDu/T cell
lines, whereas the apoptosis-related proteins caspase-3 and Bax
decreased. P-gp, encoded by the multi-drug resistance 1 (MDR1)
gene, is an efflux transporter, which is important in the MDR of
cancer cells and transports numerous substrates, including Taxol
and VCR. As an anti-apoptotic member of the Bcl family, Bcl-2
inhibits the release of apoptotic molecules, including the caspase
family members, by interacting with Bax (10). The increased expression of P-gp and
Bcl-2 appears to be a critical factor of chemotherapy and apoptosis
resistance in FaDu/T cells. In order to overcome the malignant
behavior of FaDu/T tumor cells, numerous chemotherapeutic drugs
have been demonstrated to be effective in vivo; however, the
toxicity and side effects largely limit the clinical application
over a long period. The results of previous in vitro trials
indicate that the proteasome inhibitor MG132 is a potent P-gp
inhibitor and apoptosis inducer in several types of tumor cells
(11). To verify whether MG132 has
the ability to reverse the MDR and anti-apoptotic properties of
FaDu/T cells, experiments were performed based on the previous
study. With the addition of MG132 to FaDu/T cells, P-gp was
markedly decreased, Bcl-2/Bax began to decrease and caspase-3
increased. The data from assays indicated that MG132 is able to
markedly reverse the malignant behavior of FaDu/T cells. However,
the molecular mechanisms underlying the effects of MG132 require
further investigation.
As a promising proteasome inhibitor, MG132 is able
to induce a range of antitumor activity, including the restoration
of sensitivity to chemotherapy and provocation of apoptosis
(12). It has been reported that
MG132 exerts these functions through inhibiting the degradation of
IκB proteins and therefore suppresses the nuclear translocation and
activation of NF-κB (13). As an
important transcription factor, the activation state of NF-κB
positively regulates the expression of P-gp and Bcl-2 in cancer
cells, as a binding site for NF-κB exists in the P-gp and Bcl-2
promoter region (14,15). Several studies have indicated that
p53, a transcription factor, is able to induce the expression of
the apoptotic factor Bax, which is also one of the most commonly
mutated genes in HNSCC (16). As
the substrate of the proteasome, the degradation of p53 may also be
inhibited by MG132 (17). As the
present study demonstrated, when MG132 was added to FaDu/T cells,
the nuclear translocation of NF-κB and the degradation of p53 were
all inhibited and consequently the expression of P-gp and Bcl-2
decreased. In addition, the expression of the apoptosis-related
proteins Bax and caspase-3 was markedly upregulated when FaDu/T
cells were treated with MG132. For caspase-3, certain studies have
indicated that MG132 is able to cause mitochondrial dysfunction and
subsequently cause cytochrome C release, which results in
the activation of caspase-3 and caspase-dependent apoptotic
processes (8).
To further investigate the apoptotic state of FaDu/T
cells affected by MG132, flow cytometry was conducted and it was
revealed that MG132 is able to significantly increase the apoptotic
ratio compared with FaDu/T cells. Additionally, in terms of MDR,
the present study also revealed that the multi-drug resistance of
FaDu/T cells to DDP, 5-FU, Dox and VCR was markedly decreased when
treated with MG132. This involved the reduction of P-gp and Bcl-2
accompanied by the upregulation of Bax and caspase-3, and led to
apoptosis of the majority of FaDu/T cells.
In conclusion, these observations indicated that the
upregulation of Bax and caspase-3 were involved in MG132-induced
apoptosis in the FaDu/T cancer cell line. In addition, decreased
P-gp and Bcl-2 levels were observed in FaDu/T cancer cells treated
with MG132. The mechanisms underlying the effects of MG132 are
based on the NF-κB and p53 pathways. All the alterations in
apoptosis and drug resistance relative genes are beneficial for
MG132 to reverse MDR in FaDu/T cells. These results may be valuable
for the prevention of MDR and anti-apoptosis derived from cancer
cells in clinical cancer chemotherapy.
Acknowledgements
This study was supported by the Shandong Provincial
Outstanding Young Scientist Research Award Fund of China (grant no.
BS2009YY013) and the Shandong Provincial International Science and
Technology Cooperation Project of China (grant no.
2010GHZ20202).
References
|
1
|
Bok GH, Cho WY, Cho JY, et al: Endoscopic
resection of hypopharyngeal squamous cell carcinoma. Clin Endosc.
46:189–192. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Clark JI, Hofmeister C, Choudhury A, et
al: Phase II evaluation of paclitaxel in combination with
carboplatin in advanced head and neck carcinoma. Cancer.
92:2334–2340. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yoshino T, Hasegawa Y, Takahashi S, et al:
Platinum-based chemotherapy plus cetuximab for the first-line
treatment of Japanese patients with recurrent and/or metastatic
squamous cell carcinoma of the head and neck: results of a phase II
trial. Jpn J Clin Oncol. 43:524–531. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rodrigues AC, Curi R, Genvigir FD, et al:
The expression of efflux and uptake transporters are regulated by
statins in Caco-2 and HepG2 cells. Acta Pharmacol Sin. 30:956–964.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ludwig H, Khayat D, Giaccone G, et al:
Proteasome inhibition and its clinical prospects in the treatment
of hematologic and solid malignancies. Cancer. 104:1794–1807. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wang W and Luo HS: Reversal of
chemoresistance to vincristine in gastric cancer cells by NF-kappaB
inhibitor. Zhonghua Zhong Liu Za Zhi. 27:335–338. 2005.(In
Chinese).
|
|
7
|
Fan XM, Wong BC, Wang WP, et al:
Inhibition of proteasome function induced apoptosis in gastric
cancer. Int J Cancer. 93:481–488. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Westerberg CM, Hägglund H and Nilsson G:
Proteasome inhibition upregulates Bim and induces
caspase-3-dependent apoptosis in human mast cells expressing the
Kit D816V mutation. Cell Death Dis. 3:e4172012. View Article : Google Scholar
|
|
9
|
Ma J, Lu S, Yu L, et al: FaDu cell
characteristics induced by multidrug resistance. Oncol Rep.
26:1189–1195. 2011.PubMed/NCBI
|
|
10
|
Youle RJ and Strasser A: The BCL-2 protein
family: opposing activities that mediate cell death. Nat Rev Mol
Cell Biol. 9:47–59. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chen YC, Huang WJ, Hsu JL, et al: A novel
hydroxysuberamide derivative potentiates MG132-mediated anticancer
activity against human hormone refractory prostate cancers - the
role of histone deacetylase and endoplasmic reticulum stress.
Prostate. 73:1270–1280. 2013. View Article : Google Scholar
|
|
12
|
Bravo-Cuellar A, Hernández-Flores G,
Lerma-Díaz JM, et al: Pentoxifylline and the proteasome inhibitor
MG132 induce apoptosis in human leukemia U937 cells through a
decrease in the expression of Bcl-2 and Bcl-XL and phosphorylation
of p65. J Biomed Sci. 20:132013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang Y, Sun W, Du B, et al: Therapeutic
effect of MG-132 on diabetic cardiomyopathy is associated with its
suppression of proteasomal activities: roles of Nrf2 and NF-κB. Am
J Physiol Heart Circ Physiol. 304:H567–H578. 2013.PubMed/NCBI
|
|
14
|
da Silva SV, Salama C, Renovato-Martins M,
et al: Increased leptin response and inhibition of apoptosis in
thymocytes of young rats offspring from protein deprived dams
during lactation. PLoS One. 8:e642202013.PubMed/NCBI
|
|
15
|
Kanagasabai R, Krishnamurthy K, Druhan LJ,
et al: Forced expression of heat shock protein 27 (Hsp27) reverses
P-glycoprotein (ABCB1)-mediated drug efflux and MDR1 gene
expression in Adriamycin-resistant human breast cancer cells. J
Biol Chem. 286:33289–33300. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chen Y, Zhang X, Dantas Machado AC, et al:
Structure of p53 binding to the BAX response element reveals DNA
unwinding and compression to accommodate base-pair insertion.
Nucleic Acids Res. 41:8368–8376. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Pigneux A, Mahon FX, Moreau-Gaudry F, et
al: Proteasome inhibition specifically sensitizes leukemic cells to
anthracyclin-induced apoptosis through the accumulation of Bim and
Bax proapoptotic proteins. Cancer Biol Ther. 6:603–611. 2007.
View Article : Google Scholar
|