Introduction
Chitosan is a mucopolysaccharide, which is closely
associated with cellulose and is obtained by the deacetylation of
chitin, which is the predominant compound present in the
exoskeleton of crustaceans (1).
The biopolymer chitosan is defined as containing <50%
N-acetyl-glucosamine, whereas if the number of N-acetylglucosamine
units is >50%, the biopolymer is termed chitin (2). The biological activity of chitosan is
dependent on its molecular weight, extent of deacetylation,
chitosan derivatization, proportion of glucosamine units, pH and
its target (3–5).
Chitosan has been previously demonstrated to exhibit
therapeutic effects in the inhibition of inflammation in asthma
(6–9), in the strengthening of bones in
osteoporosis (10,11), as an antibacterial agent (7), a vector for gene delivery (12,13),
an antifungal agent (14), an
anti-malaria agent (15) and a
homeostatic agent in wound dressings (16). Low molecular weight (LMW) and
water-soluble chitosan, are efficient colloidal drug carriers
(17) due to high levels of water
solubility, non-toxicity, biocompatibility, biodegradability, and
bioadhesive and absorption enhancing properties (18). In addition, the potential
biological activities of LMW chitosan, including its antioxidative
and antitumorigenic properties, make it a suitable candidate for
biomedical applications (14,18,19).
Previous studies have indicated that chitosan exhibits
antitumorigenic activity (18,20).
Mushrooms are another natural product with medicinal uses, and have
been used for several years in Asian countries and their use is
increasing in western countries. The number of mushroom species on
the planet has been estimated at ~ 140,000, however, suggesting
that only 10% of species have been identified (21). Under the assumption that only 5% of
the unknown species of mushrooms will be beneficial to humans, this
indicates that ~7,000 useful species remain to be identified
(22). Among the known species,
the proportion which have been thoroughly investigated remains low.
Mushrooms require antibacterial and antifungal compounds in order
to survive in their natural environment (23), and these can be isolated from the
mushrooms to provide potential therapeutic benefits for humans
(24). Previous studies in Asia
and eastern Europe have indicated that mushrooms may be important
in preventing and treating cancer (25), and the antitumor effects of several
mushroom extracts and isolated compounds have been demonstrated in
tumor cell systems and in animal assays (26–33).
Mushroom extracts have been identified as
immunological, hypocholesterlemic, antiviral, antibacterial,
anticarcinogenic and anti-inflammatory (34). Agaricus blazei Murill (ABM)
is an edible mushroom, which is native to Brazil and is cultivated
in several countries, including Taiwan, Japan, Korea, China and
Indonesia (25). ABM has been
reported to possess antitumor activity (35,36),
however, the function of ABM in SK-Hep 1 hepatoma cells in mice
with severe combined immunodeficiency (SCID) has not been
investigated.
The aim of the present study was to investigate
whether ABM extract or LMW chitosan were effective antitumorigenic
compounds, and to determine whether the combination of ABM and
chitosan was more effective than either of the compounds alone in
reducing the size of tumors in mice injected with hepatoma
cells.
Materials and methods
Animals and housing conditions
Animals were maintained in accordance with the
guidelines approved by the National Science Council of the Republic
of China and the Committee for the Purpose of Control and
Supervision of Experiments on Animals. Experiments are performed in
accordance with the law, regulations and guidelines for animal
experiments in Taiwan, which are in agreement with the Declaration
of Helsinki. The investigations involving mice were approved by the
Institutional Animal Care and Use Committee of Chen Hsin General
Hospital (Taipei, Taiwan; CHIACUC 102-18). A total of 60 SCID mice
(male, weighing 22–26 g, four-weeks-old) were obtained from
BioLASCO Taiwan Co., Ltd. (Taipei, Taiwan). The mice were earmarked
and housed in polypropylene cages (five animals/cage) covered with
metallic grids in a room maintained under constant environmental
conditions, with air filter tops in a filtered laminar air flow, an
ambient temperature of 22±3°C, relative humidity of 55±15% and with
a 12-h light-dark cycle for a 2-week acclimatization period. The
mice received autoclaved water and laboratory pellet chow ad
libitum (37).
Chitosan and ABM preparation
Chitosan powder (molecular weight, 50,000–190,000;
cat. no. 448869; Sigma-Aldrich, St. Louis, MO, USA) was suspended
in 0.2 ml distilled water at 50°C for 10 min, and then cooled to
room temperature and stirred for 1 h at 200 rpm using a TS-560
orbital shaker (Yihder Technology Co., Ltd., Taipei, Taiwan) (low
dose 5 mg/kg/day; high dose 20 mg/kg/day). ABM powder was obtained
from S. Canaan Biotechnology Development Co. (Taipei, Taiwan) and
was separately suspended in 6 ml distilled water at 60°C for 10
min, then cooled to room temperature and stirred for 5 h at 200 rpm
to form solutions of 246 mg/kg body weight/0.2 ml or 984 mg/kg body
weight/0.2 ml which were 10 or 40 times of therapy doses cited by
package insert. The ABM supernatant solution was then filtered,
freeze dried, and stored at −50°C until use, as previously
described (38).
Hepatoma formation using SK-Hep 1 cells
in SCID mice and treatment with ABM and chitosan
All of the mice were injected subcutaneously with
SK-Hep 1 cells (Food Industry Research and Development Institute,
Hsunchu, Taiwan) (3×107 cells/mouse) in the dorsal area.
Tumors were allowed to develop for 2–3 weeks (week 0), and mice
with tumors measuring 1–3 mm in diameter were divided into the
following six groups (10 mice/group): Group 1, control group
(distilled water); group 2, chitosan 5 mg/kg/day; group 3, chitosan
20 mg/kg/day; group 4, ABM (246 mg/kg/day) and chitosan (5
mg/kg/day) combined; group 5, ABM (984 mg/kg/day) and chitosan (20
mg/kg/day) combined; and group 6, ABM (984 mg/kg/day). Following 6
weeks of treatment, the levels of serum glutamic oxaloacetic
transaminase (GOT), glutamic pyruvic transaminase (GPT) and
vascular endothelial growth factor (VEGF) were examined in the
surviving animals. The mice were then sacrificed using
CO2, and the tumors were surgically excised and weighed,
prior to histopathological analysis.
Serum biomarkers
Whole blood (0.5–1 ml) was collected from each mouse
via heart puncture. The collected blood was centri fuged (2,000 ×
g) for 10 min using the Kubota 2420 centrifuge (Kubota, Fujioka,
Japan). The serum levels of GOT and GPT were analyzed using a D×C
800 clinical chemistry analyzer with kits (GOT catalog no.,
M307050; GPT catalog no., M312240) purchased from Beckman Coulter
(Brea, CA, USA).
The quantification of murine VEGF in the serum was
determined using a mini ELISA development kit (900-M99; cat. no.
0812099-M), according to the manufacturer’s instructions
(PeproTech, Inc., Rocky Hill, NJ, USA). Briefly, for ELISA,
undiluted standard (1.5 ng/ml; from the ELISA kit) served as the
highest standard level and the calibrator diluents served as the
zero standard. For the measurement of VEGF, 100 μl undiluted
sample or standard was added to each well of the ELISA plate and
incubated at room temperature for a minimum of 2 h. Aspiration and
washing of the plate with buffer (0.05% Tween-20 in PBS; PeproTech)
were performed four times. The detection antibody (purified rabbit
anti-VEGF; 0812099-M; PeproTech, Inc.) was diluted in diluents
(0.05% Tween-20 + 0.1% bovine serum albumin in phosphate-buffered
saline; PeproTech) to a concentration of 0.5 μg/ml. A total
of 100 μl/well was added and the plate was incubated at room
temperature for 2 h. Aspiration and washing of the plate were
performed four times, and 5.5 μl avidin-horseradish
peroxidase conjugate (1:2,000) was added to the diluent to a total
volume of 11 ml, of which 100 μl was added per well and
incubated for 30 min at room temperature. The plate was then
aspirated and washed four more times, and 100 μl substrate
solution was added to each well prior to incubation at room
temperature for color development. The color development was
assessed using an ELISA plate reader (Bio Rad Laboratories, Inc.,
Hercules, CA, USA) at 405 nm with the wavelength correction set at
650 nm.
Histopathology
At the end of the 6 weeks treatment, the survival
rates of the mice were assessed. Histological analysis of the liver
tissues were also performed as follows: The tissue samples were
rinsed with 0.9% saline solution (Jye-Jiunn, Taipei, Taiwan) and
fixed in 10% formalin (Avantor Performance Materials, Deventer,
Netherlands). The liver sections were then prepared and processed
(TP1020; Leica Microsystems KK, Tokyo, Japan) as follows: The
sections were incubated twice with 10% neutral buffered formalin
for 30 min each, 75% alcohol (Jye-Jiunn) at room temperature for 1
h, 85% alcohol at room temperature for 1 h, twice with 95% alcohol
at room temperature for 1 h, twice with 100% alcohol at 40°C for 1
h, twice with xylene (Surgipath, Leica Microsystems, Inc., Buffalo
Grove, IL, USA) at 40°C for 1 h and in molten wax (Surgipath, Leica
Microsystems, Inc.) at 60°C for 30 min repeated 4 times. The
samples were embedded in paraffin (Leica Biosystems Richmond, Inc.,
Richmond, IL, USA), sectioned (4 μm), placed on frosted
glass slides (Muto Pure Chemicals Co., Ltd., Tokyo, Japan), dried
using a 70°C hot plate (Yihder Technology Co., Ltd.) for 30 min and
stained with hematoxylin and eosin (H&E; Muto Pure Chemicals
Co., Ltd.).
Statistics
The data are presented as the mean ± standard
deviation. One way analysis of variance was used to determine
significant differences between the control and treated groups.
Student’s t-test was used to compare the means from two independent
groups. P<0.05 was considered to indicate a statistically
significant difference.
Results
Following treatment for 6 weeks, the survival rates
of the mice in the different groups were as follows: Group 1, 90%
(9/10); group 2, 100% (10/10); group 3 100% (10/10); group 4, 100%
(10/10); group 5, 70% (7/10); and group 6, 70% (7/10). A blood
sample was not obtained from this animal, however, the tumor was
weighed.
The serum concentrations of the GOT and GPT
biochemical markers were analyzed to evaluate liver function. The
levels of VEGF, which is a key angiogenic factor, were also
examined. In addition, tumor weights and histopathological changes
were evaluated.
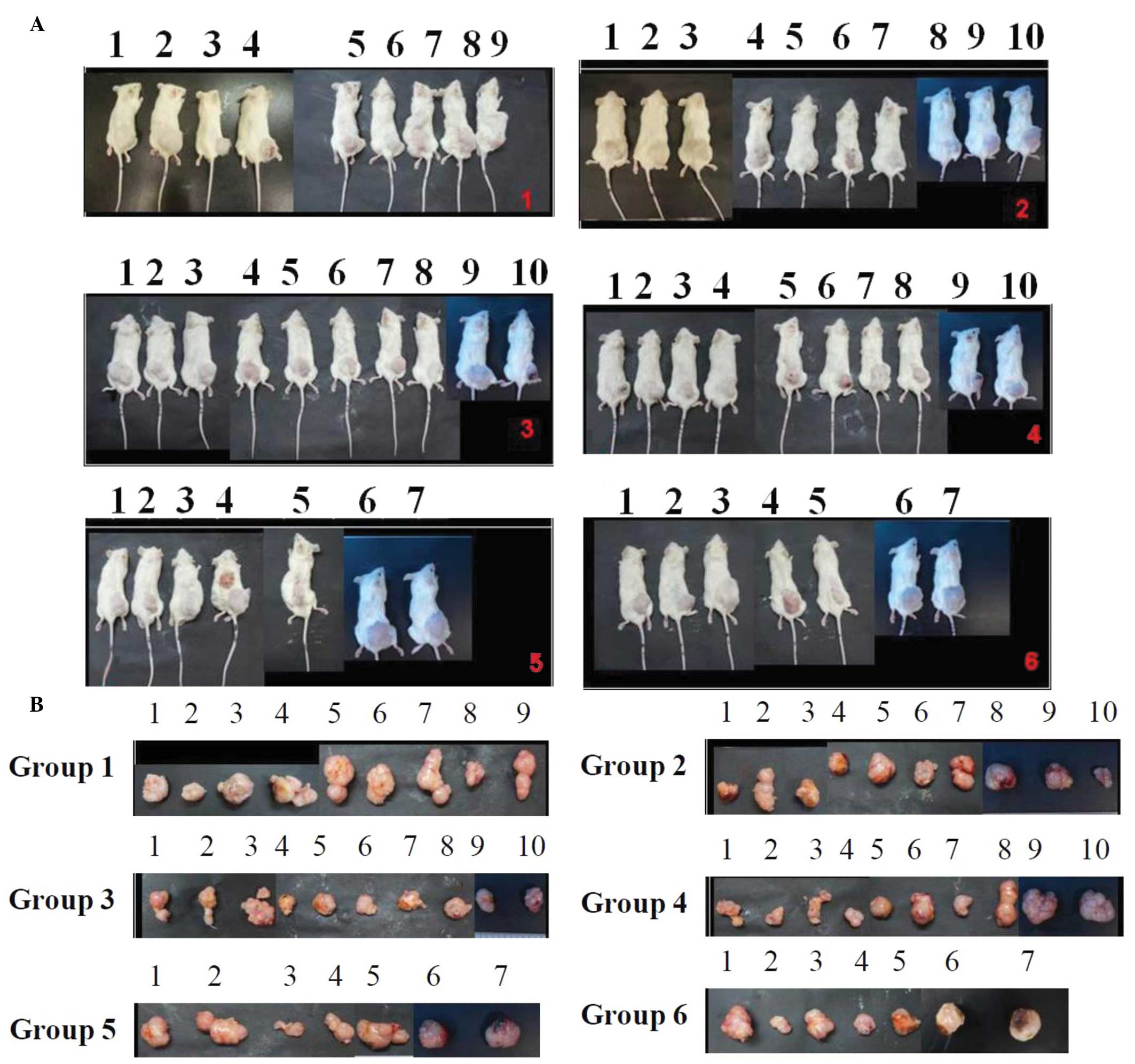
Following the injections with SK-Hep 1 cells to
induce tumor growth, the mice were orally administered different
doses of LMW chitosan combined with ABM. Following 6 weeks
treatment, blood samples were collected from all the surviving
mice, which were then sacrificed, and the weights of the tumors
were assessed (Fig. 1). The tumor
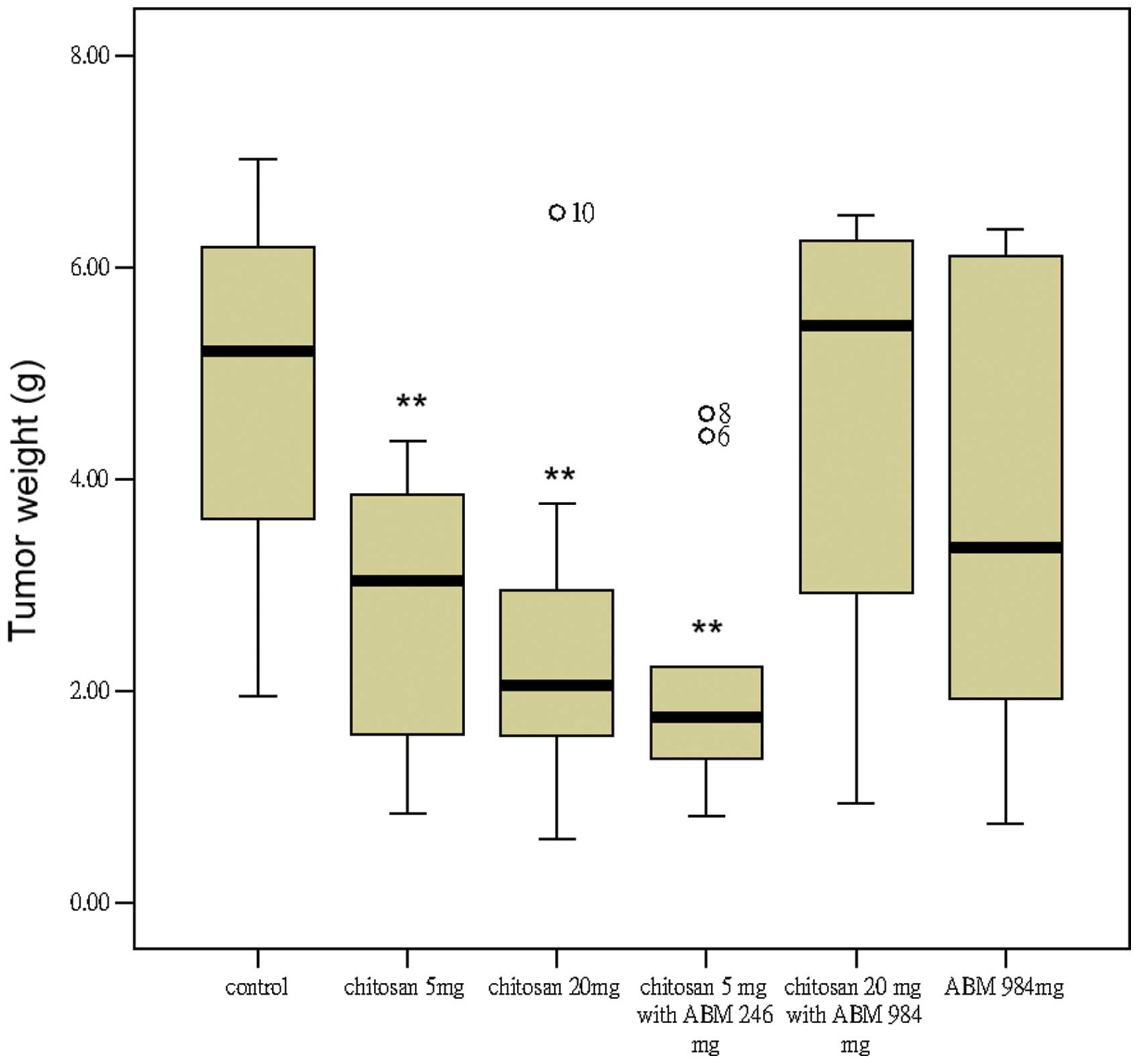
weights were 4.81±1.84, 2.83±1.23, 2.56±1.65, 2.15±1.33, 4.59±2.11
and 3.79±2.39 g for groups 1-5, respectively. Groups 2, 3 and 4
exhibited significantly reduced tumor growth compared with the
control group (P<0.05; Table
I). No significant differences were observed among these three
groups in the reduction of tumor weights.
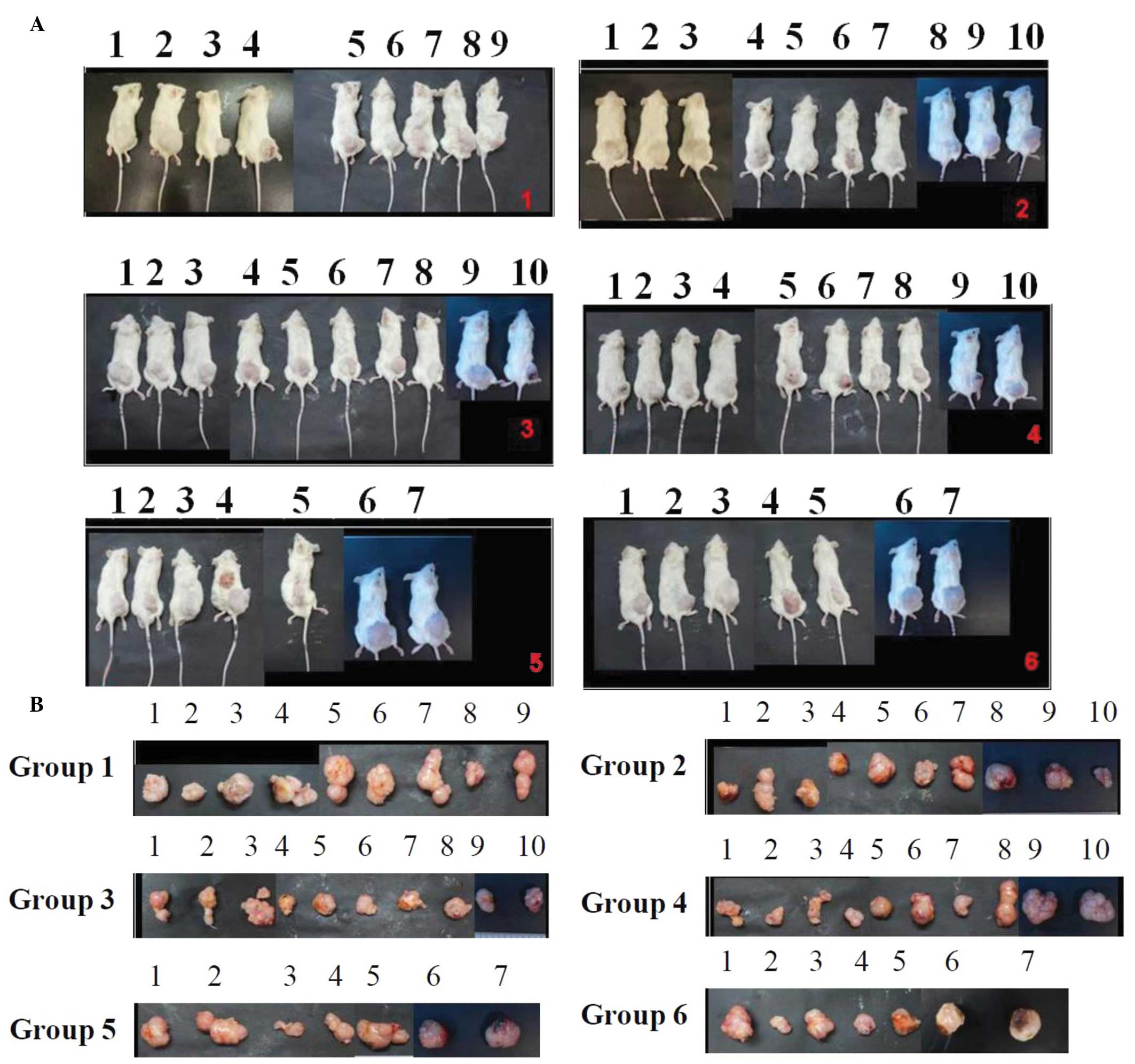 | Figure 1Treatment with chitosan and ABM
affects subcutaneously implantated SK-Hep 1 cells in SCID mice
in vivo. SK-Hep 1 cancer cells were inoculated
subcutaneously into the dorsal area of each mouse. At 2 3 weeks
after inoculation, each mouse had produced one palpable tumor of
1–3 mm in diameter. The mice were randomly divided into six groups,
each containing 10 animals, one of which animal did not survive to
the end of the experiment. Images of the (A) live mice and (B)
representative tumors were captured. Group 1, control group; group
2, chitosan 5 mg/kg/day; group 3, chitosan 20 mg/kg/day; group 4,
ABM (246 mg/kg/day) and chitosan (5 mg/kg/day) ; group 5, ABM (984
mg/kg/day) and chitosan (20 mg/kg/day); group 6, ABM (984
mg/kg/day). ABM, Agaricus blazei Murill; SCID, severe
combined immunodeficiency. |
 | Table IAnticancer effects of low molecular
weight chitosan oligosaccharides in combination with ABM extract on
the reduction of hepatoma formation by SK-Hep 1 cells in SCID
mice. |
Table I
Anticancer effects of low molecular
weight chitosan oligosaccharides in combination with ABM extract on
the reduction of hepatoma formation by SK-Hep 1 cells in SCID
mice.
| Group | Treatment (mg) | Tumor weight
(g) | GOT (IU/l) | GPT (IU/l) | VEGF (ng/ml) |
|---|
| 1 | 0 | 4.81±1.84 | 162±80 | 17±4 | 0.572±0.054 |
| 2 | 5 chitosan+0
ABM | 2.83±1.23a
(P=0.0083) | 148±69 | 35±31 | 0.510±0.136 |
| 3 | 20 chitosan+0
ABM | 2.56±1.65a
(P=0.0065) | 91±19a
(P=0.020) | 15±4 | 0.520±0.140 |
| 4 | 5 chitosan+246
ABM | 2.15±1.33a
(P=0.0015) | 99±26a
(P=0.033) | 14±4 | 0.459±0.096a
(P=0.0191) |
| 5 | 20 chitosan+984
ABM | 4.59±2.11 | 152±77 | 18±7 | 0.572±0.164 |
| 6 | 984 ABM | 3.79±2.39 | 139±86 | 20±6 | 0.439±0.039a
(P=0.0167) |
The concentration of GOT was significantly reduced
in group 2 (91±19 IU/l; P=0.020) and group 3 (99±26 IU/l; P=0.033)
compared with the control group (162±80 IU/l) following 6 weeks
treatment. This suggested that treatment with 20 mg chitosan or 5
mg chitosan combined with 246 mg ABM improved liver function. The
levels of GOT in the control and ABM-only (139±86 IU/l) treatment
groups were not significantly different. The mice treated with
increasing doses of chitosan or ABM did not exhibit any gradual
elevation or reduction in serum levels of GPT. The GPT
concentrations were increased (35±31 IU/l) following administration
of 5 mg chitosan treatment compared with that in the control group
(17±4 IU/L), however, this was not statistical significant
(P=0.054; Table I). The
concentration of VEGF was significantly different in group 3
(0.459±0.096 ng/ml; P=0.0191) and group 5 (0.439±0.039 ng/ml,
P=0.0167) compared with the control group (0.572±0.054 ng/ml) after
6 weeks (Table I).
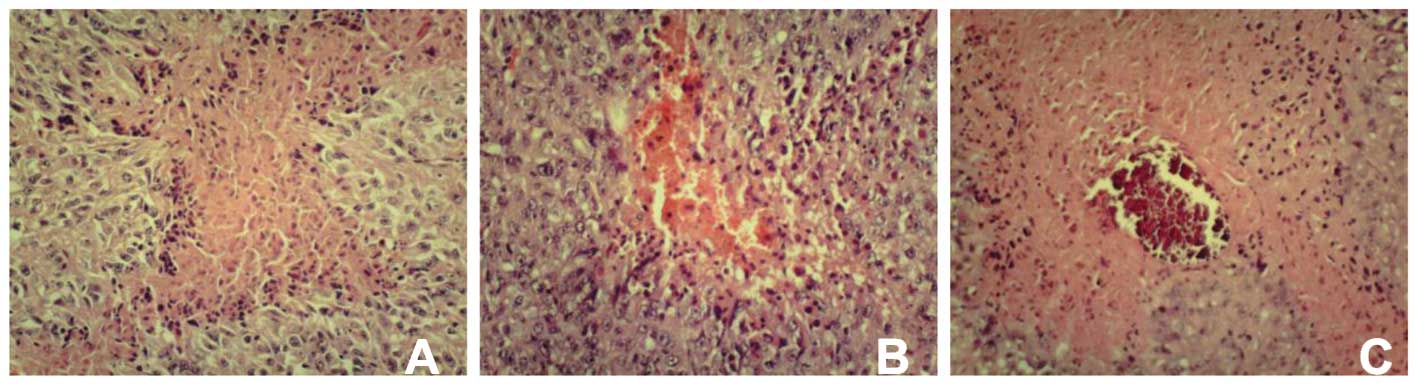
The histopathological assessments were performed in
the control and experimental groups. The tumor sections were
stained with H&E and exhibited dark eosinophilic cytoplasms and
small or large, darkly stained nuclei. The tissues from the mice in
the control and experimental groups exhibited necrosis,
calcification and hemorrhaging (Fig.
2). Irregular shapes of focal necrotic areas and loss of normal
architecture were characterized by necrotic cells with eosinophilic
cell debris and peripheral viable tissues. Foci of hemorrhage and
scarlet calcification were frequently observed in the center of
certain necrotic areas (Table
II).
 | Table IIPresence of necrosis, hemorrhage and
calcification determined by hematoxylin and eosin staining of 10
tumor samples from each treatment group. |
Table II
Presence of necrosis, hemorrhage and
calcification determined by hematoxylin and eosin staining of 10
tumor samples from each treatment group.
| Treatment | Pathology | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Average |
|---|
| Control | Necrotic rate | 0.6 | 0.4 | 0.3 | 0.3 | 0.25 | 0.6 | 0.6 | 0.4 | 0.3 | | 0.42±0.15 |
| Hemorrhage | − | − | − | − | − | + | − | + | − | | 2/9 |
| Calcification | − | − | − | − | − | + | + | − | − | | 2/9 |
| 5 mg chitosan | Necrotic rate | 0.2 | 0.2 | 0.3 | 0.3 | 0.2 | 0.3 | 0.3 | 0.3 | 0.4 | 0.3 | 0.3±0.1 |
| Hemorrhage | − | + | + | + | − | + | + | + | + | + | 8/10 |
| Calcification | − | − | − | − | + | − | + | + | + | + | 5/10 |
| 20 mg chitosan | Necrotic rate | 0.2 | 0.3 | 0.2 | 0.3 | 0.2 | 0.3 | 0.3 | 0.3 | 0.2 | 0.2 | 0.3±0.1 |
| Hemorrhage | + | − | − | − | + | + | + | + | + | + | 7/10 |
| Calcification | − | − | − | − | − | − | − | − | + | + | 2/10 |
| 5 mg chitosan + 246
mg ABM | Necrotic rate | 0.4 | 0.3 | 0.2 | 0.3 | 0.3 | 0.2 | 0.3 | 0.3 | 0.4 | | 0.3±0.1 |
| Hemorrhage | + | + | − | + | − | + | − | + | + | | 6/9 |
| Calcification | − | − | − | − | + | − | + | + | − | | 3/9 |
| 20 mg chitosan +
984 mg ABM | Necrotic rate | 0.2 | 0.2 | 0.3 | 0.3 | 0.4 | 0.2 | 0.3 | 0.2 | | | 0.3±0.1 |
| Hemorrhage | − | − | − | − | − | − | + | + | | | 2/8 |
| Calcification | + | + | − | + | + | − | + | + | | | 6/8 |
| 984 mg ABM | Necrotic rate | 0.3 | 0.2 | 0.2 | 0.3 | 0.2 | 0.3 | 0.2 | | | | 0.2±0.1 |
| Hemorrhage | − | − | + | − | + | + | + | | | | 4/7 |
| Calcification | − | − | + | − | − | + | + | | | | 3/7 |
Discussion
In the present study, the results from the analysis
of tumor weights suggested that the 5 mg chitosan (group 2), 20 mg
chitosan (group 3) and 5 mg chitosan + 246 mg ABM (group 4)
possessed anticancer activity. The survival rates were another
important indicator. Following a 6-week treatment period, the
survival rates of the rats in the three positive effective groups
(3, 4 and 5) were all 100%. As no differences were observed in
tumor weight among these groups, 5 mg chitosan was suggested as a
first choice in treatment due to its low dose and single rather
than combination therapy. However, if sample 10 in group 3 and
samples 6 and 8 in group 4 were excluded, a greater reduction in
tumor weight was observed in groups 3 and 4 compared with group 2.
Therefore, 20 mg chitosan or 5 mg chitosan + 246 mg ABM were
suggested as more effective doses for treatment compared with 5 mg
(Fig. 3). This was further
supported by the observation that groups 3 and 4, but not group 2,
were able to reduce the levels of GOT (Table I).
Tumor weight is not proportional to tumor volume due
to necrosis and cavitation of the inner tumor mass. In the present
study, the tumor volumes were 2,849±1431, 1,764±877, 1,949±1581,
1,281±720, 2,352±1860 and 3,395±1934 mm3 in groups 1–6,
respectively. Notably, the treatments in groups 2, 3 and 4 were
able to reduce tumor volumes, of which group 4 was identified as
the most effective. This suggested that 5 mg chitosan + 246 mg AMB
was the optimal treatment strategy due to its reductions in tumor
weight and volume.
Folkman et al (39) identified tumor angiogenesis as a
potential target for the treatment of cancer, and studies have
identified the VEGF-VEGFR system as the major regulator in tumor
angiogenesis (40–42). Solid tumors often become hypoxic
due to a rapid growth of tumor cells (43). Hypoxic stress is an important
inducer of the VEGF gene via stabilization and activation of
the hypoxia inducible factor (HIF) transcription factor; the
5′-upstream sequence of the VEGF gene has a HIF-response
element motif, resulting in high levels of gene expression
(44). A previous study by Kim
et al (45) demonstrated
that anti-human VEGF antibody efficiently suppressed the growth of
human tumor xenografts transplanted into immune-deficient mice.
This antibody can inhibit only the human-type VEGF, derived from
tumor cells, and not the mouse VEGF, derived from the cells
surrounding the tumor; however, tumor growth was significantly
suppressed. These results suggested that tumor-derived VEGF is
important in tumor angiogenesis. Although the majority of previous
studies investigating VEGF and its receptors have focussed on their
functions in angiogenesis and in endothelial cells, the function of
VEGF in cancer biology appears to be an emerging area of importance
(46). VEGF mediates
vasculogenesis and angiogenesis through the promotion of
endothelial cell growth, migration and mitosis, and is involved in
the pathogenesis, progression and metastasis of cancer (47). The role of the VEGF signaling
pathway in liver regeneration and tumor growth remains unclear,
however, the use of antiangiogenic agents in combination with
surgical treatment is almost certaily beneficial (48). In the present study, only treatment
with 5 mg chitosan + 246 mg ABM was able to significantly reduce
the levels of VEGF. Therefore, 5 mg chitosan + 246 mg ABM may be
used as a first choice anticancer treatment, targeting VEGF-VEGFR
signaling.
Our previous study reported that mice injected with
Smmu 7721 cells in the dorsal area, followed by oral administration
of ABM extract at low (22.5 mg), medium (90 mg) or high (900 mg)
doses exhibited a dose-dependent effect on tumor growth (36). In the present study, the effects of
treatment were not dose-dependent. ABM is able to absorb the heavy
metals in soil or air. The products of ABM manufactured in Brazil
are a higher quality compared with those of in Taiwan due to lead
pollution. Chitosan is able to break down or excrete several types
of pollutants (49–51). As ABM and chitosan are capable of
inhibiting tumor growth, the aim of the present study was to
investigate whether ABM extract was effective against tumor growth
in mice, and to determine whether treatment with LMW chitosan
combined with ABM was able to enhance the inhibition of hepatoma
formation by SK-Hep 1 cells in SCID mice. To the best of our
knowledge, this is the first study to demonstrate the inhibition of
tumor growth by the combination of chitosan and ABM, and support
further investigation on the anticancer effects of these natural
compounds.
Acknowledgments
This study was supported by a grant (no. CH102 01)
from Cheng Hsin General Hospital.
References
|
1
|
Elsabee MZ and Abdou ES: Chitosan based
edible films and coatings. Mater Sci Eng C Mater Biol Appl.
33:1819–1841. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rouget C: Des substances amylacees dans le
tissu des animaux. specialement les articutes (chitine). Comp Rend.
48:792–795. 1859.
|
|
3
|
Minke R and Blackwell J: The structure of
alpha-chitin. J Mol Biol. 120:167–181. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kim S-K and Rajapakse N: Enzymatic
production and biological activities of chitosan oligosaccharides
(COS): A review. Carbohydrate Polymers. 62:357–368. 2005.
View Article : Google Scholar
|
|
5
|
Yin H, Du Y and Zhang J: Low molecular
weight and oligomeric chitosans and their bioactivities. Curr Top
Med Chem. 9:1546–1559. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Donnelly LE and Barnes PJ: Acidic
mammalian chitinase-a potential target for asthma therapy. Trends
Pharmacol Sci. 25:509–511. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Elias JA, Homer RJ, Hamid Q and Lee CG:
Chitinases and chitinase-like proteins in T(H)2 inflammation and
asthma. J Allergy Clin Immunol. 116:497–500. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kawada M, Hachiya Y, Arihiro A and
Mizoguchi E: Role of mammalian chitinases in inflammatory
conditions. Keio J Med. 56:21–27. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhu Z, Zheng T, Homer RJ, et al: Acidic
mammalian chitinase in asthmatic Th2 inflammation and IL-13 pathway
activation. Science. 304:1678–1682. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Klokkevold PR, Vandemark L, Kenney EB and
Bernard GW: Osteogenesis enhanced by chitosan (poly-N-acetyl
glucosaminoglycan) in vitro. J Periodontol. 67:1170–1175. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ratanavaraporn J, Kanokpanont S, Tabata Y
and Damrongsakkul S: Growth and osteogenic differentiation of
adipose-derived and bone marrow-derived stem cells on chitosan and
chitooligosaccharide films. Carbohydrate Polymers. 78:873–878.
2009. View Article : Google Scholar
|
|
12
|
Koping-Hoggard M, Mel’nikova YS, Varum KM,
Lindman B and Artursson P: Relationship between the physical shape
and the efficiency of oligomeric chitosan as a gene delivery system
in vitro and in vivo. J Gene Med. 5:130–141. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Koping-Hoggard M, Varum KM and Issa M:
Improved chitosan-mediated gene delivery based on easily
dissociated chitosan polyplexes of highly defined chitosan
oligomers. Gene Ther. 11:1441–1452. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Oliveira EN Jr, El Gueddari NE,
Moerschbacher BM, Peter MG and Franco TT: Growth of phytopathogenic
fungi in the presence of partially acetylated
chitooligosaccharides. Mycopathologia. 166:163–174. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Shahabuddin M, Toyoshima T, Aikawa M and
Kaslow DC: Transmission-blocking activity of a chitinase inhibitor
and activation of malarial parasite chitinase by mosquito protease.
Proc Natl Acad Sci U S A. 90:4266–4270. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ribeiro MP, Espiga A, Silva D, et al:
Development of a new chitosan hydrogel for wound dressing. Wound
Repair Regen. 17:817–824. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Feng C, Sun G, Wang Z, et al: Transport
mechanism of doxorubicin loaded chitosan based nanogels across
intestinal epithelium. Eur J Pharm Biopha. 2013.
|
|
18
|
Yeh MY, Wu MF, Shang HS, et al: Effects of
chitosan on xenograft models of melanoma in C57BL/6 mice and
hepatoma formation in SCID mice. Anticancer Res. 33:4867–4873.
2013.PubMed/NCBI
|
|
19
|
Kim HM, Hong SH, Yoo SJ, Baek KS, Jeon YJ
and Choung SY: Differential effects of chitooligosaccharides on
serum cytokine levels in aged subjects. J Med Food. 9:427–430.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Karagozlu MZ and Kim SK: Anticancer
effects of chitin and chitosan derivatives. Adv Food Nutr Res.
72:215–225. 2014.PubMed/NCBI
|
|
21
|
Lindequist U, Niedermeyer TH and Jülich
WD: The pharmacological potential of mushrooms. Evid Based
Complement Alternat Med. 2:285–299. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Hawksworth DL: Mushrooms: the extent of
the unexplored potential. Int J Med Mushrooms. 3:333–337. 2001.
View Article : Google Scholar
|
|
23
|
Hearst R, Nelson D, McCollum G, et al: An
examination of antibacterial and antifungal properties of
constituents of Shiitake (Lentinula edodes) and oyster (Pleurotus
ostreatus) mushrooms. Complement Ther Clin Pract. 15:5–7. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lindequist U, Teuscher E and Narbe G: Neue
Wirkstoffe aus Basidiomyceten. Z Phytother. 11:139–149. 1990.
|
|
25
|
Firenzuoli F, Gori L and Lombardo G: The
Medicinal Mushroom Agaricus blazei Murrill: Review of Literature
and Pharmaco-Toxicological Problems. Evid Based Complement Alternat
Med. 5:3–15. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kahlos K, Kangas L and Hiltunen R:
Antitumor activity of some compounds and fractions from an n-hexane
extract of Inonotus obliquus in vitro. Acta Pharm Fennica.
96:33–40. 1987.
|
|
27
|
Burczyk J, Gawron A, Slotwinska M,
Smietana B and Terminska K: Antimitotic activity of aqueous
extracts of Inonotus obliquus. Boll Chim Farm. 135:306–309.
1996.PubMed/NCBI
|
|
28
|
Chihara G, Maeda Y, Hamuro J, Sasaki T and
Fukuoka F: Inhibition of mouse sarcoma 180 by polysaccharides from
Lentinus edodes (Berk.). sing Nature. 222:687–688. 1969. View Article : Google Scholar
|
|
29
|
Mizuno T: The extraction and development
of antitumor-active polysaccharides from medicinal mushrooms in
Japan (review). Int J Med Mushrooms. 1:9–30. 1999. View Article : Google Scholar
|
|
30
|
Wasser SP and Weis AL: Medicinal
properties of substances occurring in higher Basidiomycetes
mushrooms: current perspectives (review). Int J Med Mushrooms.
1:31–62. 1999. View Article : Google Scholar
|
|
31
|
Reshetnikov SV, Wasser SP and Tan KK:
Higher basidiomycetes as a source of antitumor and
immunostimulating polysaccharides (review). Int J Med Mushrooms.
3:361–394. 2001. View Article : Google Scholar
|
|
32
|
Fujimiya Y, Suzuki Y, Oshiman K, et al:
Selective tumoricidal effect of soluble proteoglucan extracted from
the basidiomycete, Agaricus blazei Murill, mediated via natural
killer cell activation and apoptosis. Cancer Immunol Immunother.
46:147–159. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ito H, Shimura K, Itoh H and Kawade M:
Antitumor effects of a new polysaccharide-protein complex (ATOM)
prepared from Agaricus blazei (Iwade strain 101) ‘Himematsutake’
and its mechanisms in tumor-bearing mice. Anticancer Res.
17:277–284. 1997.PubMed/NCBI
|
|
34
|
Patel S and Goyal A: Recent developments
in mushrooms as anti cancer therapeutics: a review. 3 Biotech.
2:1–15. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Wu MF, Chen YL, Lee MH, et al: Effect of
Agaricus blazei Murrill extract on HT 29 human colon cancer cells
in SCID mice in vivo. In Vivo. 25:673–677. 2011.PubMed/NCBI
|
|
36
|
Wu MF, Lu HF, Hsu YM, et al: Possible
reduction of hepatoma formation by Smmu 7721 cells in SCID mice and
metastasis formation by B16F10 melanoma cells in C57BL/6 mice by
Agaricus blazei murill extract. In Vivo. 25:399–404.
2011.PubMed/NCBI
|
|
37
|
Chen WT, Yang CL and Yin MC: Protective
effects from Houttuynia cordata aqueous extract against
acetaminophen-induced liver injury. Biomedicine. 4:24–28. 2014.
View Article : Google Scholar
|
|
38
|
Jin CY, Moon DO, Choi YH, Lee JD and Kim
GY: Bcl-2 and caspase-3 are major regulators in Agaricus
blazei-induced human leukemia U937 cell apoptosis through
dephoshorylation of Akt. Biol Pharm Bull. 30:1432–1437. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Hanahan D and Folkman J: Patterns and
emerging mechanisms of the angiogenic switch during tumorigenesis.
Cell. 86:353–364. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Shibuya M: Involvement of Flt 1 (VEGF
receptor-1) in cancer and preeclampsia. Proc Jpn Acad Ser B Phys
Biol Sci. 87:167–178. 2011. View Article : Google Scholar :
|
|
41
|
Shibuya M and Claesson-Welsh L: Signal
transduction by VEGF receptors in regulation of angiogenesis and
lymphangiogenesis. Exp Cell Res. 312:549–560. 2006. View Article : Google Scholar
|
|
42
|
Alitalo K and Carmeliet P: Molecular
mechanisms of lymphangiogenesis in health and disease. Cancer Cell.
1:219–227. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Li Y, Fu L, Li JB, et al: Increased
expression of EIF5A2, via hypoxia or gene amplification,
contributes to metastasis and angiogenesis of esophageal squamous
cell carcinoma. Gastroenterology. 146:1701–1713. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Shibuya M: Vascular endothelial growth
factor and its receptor system: physiological functions in
angiogenesis and pathological roles in various diseases. J Biochem.
153:13–19. 2013. View Article : Google Scholar
|
|
45
|
Kim KJ, Li B, Winer J, et al: Inhibition
of vascular endothelial growth factor-induced angiogenesis
suppresses tumour growth in vivo. Nature. 362:841–844. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Perrot-Applanat M and Di Benedetto M:
Autocrine functions of VEGF in breast tumor cells: adhesion,
survival, migration and invasion. Cell Adh Migr. 6:547–553. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Wang K, Peng HL and Li LK: Prognostic
value of vascular endothelial growth factor expression in patients
with prostate cancer: a systematic review with meta-analysis. Asian
Pac J Cancer Prev. 13:5665–5669. 2012. View Article : Google Scholar
|
|
48
|
Eveno C and Pocard M: VEGF levels and the
angiogenic potential of the microenvironment can affect surgical
strategy for colorectal liver metastasis. Cell Adh Migr. 6:569–573.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Li M, Xu J, Li R, et al: Simple
preparation of aminothiourea-modified chitosan as corrosion
inhibitor and heavy metal ion adsorbent. J Colloid Interface Sci.
417:131–136. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Liu J, Wen XY, Lu JF, Kan J and Jin CH:
Free radical mediated grafting of chitosan with caffeic and ferulic
acids: Structures and antioxidant activity. Int J Biol Macromol.
65C:97–106. 2014. View Article : Google Scholar
|
|
51
|
Seo DJ, Nguyen DM, Park RD and Jung WJ:
chitosan-cinnamon beads enhance suppressive activity against
Rhizoctonia solani and Meloidogyne incognita in vitro. Microb
Pathog. 66:44–47. 2014. View Article : Google Scholar : PubMed/NCBI
|