Introduction
Partial or total interruption of hepatic flow is
often required when liver surgery is performed. This interruption
of blood flow is termed as 'warm ischemia' and upon
re-vascularization, when molecular oxygen is re-introduced, the
organ undergoes a process called 're-perfusion injury', which
causes deterioration of organ function (1). The interruption of hepatic blood flow
followed by its restoration during re-perfusion clinically occurs
in a number of settings, including liver transplantation, liver
resection under inflow occlusion (Pringle maneuver) and hemorrhagic
shock with fluid resuscitation (2,3).
Although the mechanisms by which organ damage occurs in
ischemia/re-perfusion (IR) injury have not been fully elucidated,
ischemia results in the termination of oxidative phosphorylation
and adenosine triphosphate production through aerobic respiration.
Restoration of the blood flow during re-perfusion triggers the
activation of kupffer cells, causing oxygen free radical formation,
production of tumor necrosis factor-alpha (TNF-alpha) and
interleukin-1 (IL-1) (4). Elevated
levels of the pro-inflammatory cytokines TNF-alpha and IL-1 promote
polymorphonuclear neutrophil recruitment and activation, which also
generates reactive oxygen species (ROS) and leads to the release of
proteases (5,6).
Adherence of circulating blood cells to the vascular
endothelium is modulated by polyunsaturated fatty acids (PUFAs). An
increase in adherence and de-granulation of neutrophils was
observed when they were incubated with arachidonic acid (AA,
C20:4n-6) and dihomo-gamma-linolenic acid (DGLA, C20:3n-6)
(7). Likewise, the ability of
PUFAs to modulate endothelial activation was shown by a study in
which docosahexaenoic acid (DHA, C22:6n-3), when added to cultured
endothelial cells prior to stimulation with cytokines, reduced the
adhesion of monocytes and endothelial expression of vascular cell
adhesion molecule-1, E-selectin and intercellular adhesion
molecule-1 (8).
The human body can produce numerous fatty acids
except the two essential PUFAs, linoleic acid (LA, C18:2n6) and
alpha-linolenic acid (ALA, C18:3n3). Linoleic acid is the precursor
of the omega-6 (n-6) series of PUFAs, while ALA is the precursor of
the omega-3 (n-3) series of PUFAs. Eicosanoids derived from n-6
PUFAs, such as AA (C20:4n-6), have pro-inflammatory and
immunoactive functions, whereas eicosanoids derived from n-3 PUFAs,
such as eicosapentaenoic acid (EPA, C20:5n-3), have
anti-inflammatory properties, attributed to their ability to
inhibit the formation of n-6 PUFA-derived eicosanoids (9). Resolvins and protectins generated
from EPA (C20:5n-3) and DHA (C22:6n-3) display potent
anti-inflammatory properties and are recognized in the resolution
of inflammation (10).
Experimental studies have been performed on rats for
the investigation of the prevention of hepatic IR injury by
administering an n-3 PUFA-rich diet (11,12).
It was shown that n-3 PUFA treatment effectively reduced hepatic
steatosis and consequently attenuated hepatic IR injury in rats
(11). A diet enriched with n-3
has also been shown to have a pre-conditioning effect to reduce
liver IR injury in rats (12).
Liver pre-conditioning against IR injury by n-3 PUFA
supplementation has been reported to be mediated by the
antagonistic effect of peroxisome proliferator-activated receptor
alfa with the nuclear factor-kappa-B-controlled transcription of
pro-inflammatory mediators (13).
A recent study performed on 66 liver transplant patients showed
that post-transplant parenteral nutritional support combined with
n-3 fatty acids can significantly improve liver injury and shorten
post-transplant hospital stays (14).
Although the effect of n-3 PUFA supplementation on
liver IR injury has been extensively studied, changes in endogenous
PUFA levels following liver IR injury without n-3 or n-6 diet
supplementation has not been investigated. The aim of the present
study was to investigate changes in liver PUFA levels following
warm IR injury and determine prostaglandin E2 (PGE2) levels as well
as phospholipase A2 (PLA2) and cyclooxygenase (COX) activity after
re-perfusion.
Materials and methods
Animals
All experimental protocols conducted on rats were
performed in accordance with the standards established by the
Institutional Animal Care and Use Committee of Akdeniz University
Medical School (Antalya, Turkey). A total of 15 male Wistar rats
weighing 350–450 g, aged 5–8 months were housed in stainless steel
cages and were allowed free access to standard rat chow (Korkutelim
Yem, Antalya, Turkey) containing 6.05% crude fat which included
linoliec acid, linolenic acid, saturated fatty acids and
monounsaturated fatty acids. The animals were maintained at a 12-h
light/dark cycle and a constant temperature of 23±1°C at all
times.
Rat model of hepatic ischemia-reperfusion
injury
Animals were fasted 12 h prior to surgery, but
allowed to drink tap water ad libitum. Rats were
anesthetized with urethane anesthesia. Urethane (Sigma-Aldrich,
Steinheim, Germany) was dissolved in 0.9% NaCl and administered at
1.2 g/kg subcutaneously. A model of lobar (70%) hepatic warm
ischemia was performed according to a previously described method
(15,16). After shaving and disinfecting the
abdomen with betadine (Kimpa Kimya, Istanbul, Turkey), a complete
midline incision was made. The portal vein was exposed and vessels
supplying the median and left lateral hepatic lobes were clamped
for 60 min. Re-perfusion followed for 60 min via removal of the
microvascular clip. The caudal and right lobes retained an intact
portal and arterial blood flow, in addition to venous outflow.
These lobes served as a control and also prevented intestinal
congestion. The abdomen was kept closed throughout the experimental
period and the body temperature was maintained by placing rats
under warming lamps. Blood samples were obtained prior to and after
the experiment, from the tail vein and the right ventricle,
respectively. At the end of the experimental period, the liver was
perfused with 0.9% NaCl injected from the left ventricle via the
inferior vena cava. Tissue samples obtained from the left and
median lobes of the liver accounted for IR, while dissected right
lateral and caudate lobes served as non-ischemic samples. Obtained
liver tissues were either snap frozen in liquid nitrogen and stored
at −70°C or fixed for histological evaluation with neutral-buffered
formalin (Sigma-Aldrich). The rat model of hepatic IR injury
established in the present study allowed for obtaining control and
IR-injured tissue from the same liver. Via this method, control and
IR liver samples (n=10 each) were obtained from rats that underwent
IR injury. Sham livers (n=5) were obtained from rats in which only
laparotomy was performed.
Histopathological evaluation of liver
sections
Paraffin sections stained with hematoxylin and eosin
(Merck, Darmstadt, Germany) were evaluated by a pathologist blinded
to the experimental conditions using an Olympus 1X81 microscope
(Olympus, Tokyo, Japan). 20 high-power fields (magnification, ×200)
were evaluated in all sections for congestion, intracellular edema
and necrosis as previously described (17). Congestion and intracellular edema
were scored as follows: 0, none; 1, present in zone III; 2, present
in zones II-III; 3, present in zones I-III. Necrosis was scored as
follows: 0, none; 1, single or focal necrosis; 2, submassive
necrosis; 3, massive necrosis + infarction. Total
histopatho-logical score was obtained by summation of all scores
given for each parameter.
Measurement of serum alanine
aminotransferase
Serum alanine aminotransferase (ALT) activity was
measured via an alanine transaminase assay kit (cat no. 700260;
Cayman Chemical, Ann Arbor, MI, USA). The rate of nicotinamide
adenine dinucleotide (NADH) oxidation was monitored by a coupled
reaction system using lactate dehydrogenase (LDH). One unit of
enzyme activity was defined as the amount of enzyme that caused the
oxidation of 1 µmol NADH to NAD+ per minute at
37°C.
Electron spray ionization mass
spectrometry (ESI-MS)
Standards for AA (C20:4n-6), DGLA (C20:3n-6), EPA
(C20:5n-3) and DHA (C22:6n-3) were purchased from Sigma-Aldrich
(St. Louis, MO, USA). Deuterium-labeled AA-d8 internal standard
(5,6,8,9,11,12,14,15-AA-d8) was obtained from Santa Cruz
Biotechnology (Dallas, TX, USA). Solutions of AA, DGLA, EPA, DHA
and AA-d8 standards were prepared in analytical grade methanol
(Merck). An optimized multiple reaction monitoring (MRM) method was
developed using ultra-fast liquid chromatography (UFLC) coupled
with tandem mass spectrometry (MS/MS). A UFLC system (LC-20 AD UFLC
XR; Shimadzu Corporation, Kyoto, Japan) was coupled to an LCMS-8040
triple quadrupole mass spectrometer (Shimadzu Corporation).
Chromatographic separations were performed using an Inertsil
high-performance liquid chromatography column (ODS-4; 2.1×100 mm; 3
µm; GL Sciences Inc., Tokyo, Japan) maintained at 40°C. DHA,
EPA, AA and DGLA were separated using a gradient elution with a
flow rate of 0.45 ml/min. Mobile phase solvent A was 10 mM ammonium
acetate (Sigma-Aldrich) in water and solvent B was acetonitrile
(Sigma-Aldrich). The gradient program was solvent B, 70% (0 min),
90% (3 min), 100% (3.01–4 min) and 70% (4.01–8 min). MRM
transitions and responses were automatically optimized for
individual compounds in negative ion ESI mode. The m/z values for
the precursor and products of AA, DHA, EPA, DGLA and AA-d8 in the
negative ESI-MS mode are stated in the Results section. Responses
to AA, DHA, EPA and DGLA were optimized to a linear calibration
range from 100 ng/ml to 30 µg/ml and a sample analysis time
of 8 min.
Sample preparation for liquid
chromatography (LC)-MS/MS
Samples were prepared for LC-MS/MS analysis using
previously described method with certain modifications (18,19).
All tissues were weighed and homogenized in ice-cold 50 mmol/l
sodium phosphate buffer (pH 7.4). Homogenates were centrifuged
(10,000 xg for 15 min at 4°C) and supernatants were stored at
−80°C. Briefly, in a glass test tube, 200 µl tissue
supernatant was added to 200 µl AA-d8 internal standard
solution. 1 ml acetonitrile/37% hydrochloric acid (Cayman Chemical)
was added to the mixture at a 4:1 v/v ratio. Tubes were capped with
re-usable teflon liner screw caps and samples were hydrolyzed by
incubating at 90°C for 2 h in a heating block (VLM, Bielefeld,
Germany). After cooling down to room temperature, fatty acids were
extracted with 2 ml hexane. Samples were vortex-mixed for 20 sec,
left at room temperature for 5 min and centrifuged at 825 x g for 1
min. The upper phase containing free fatty acids was transferred to
a glass tube and evaporated at room temperature under a constant
stream of nitrogen with a height-adjustable gas distribution unit
(VLM). Fatty acids were dissolved in 200 µl methanol-water
(180:20, v/v) filtered via 0,2-µm polytetrafluoroethylene
syringe filters (Whatman, GE Healthcare Bio-Sciences, Pittsburgh,
USA) and transferred to autosampler vials (Vertical Chromatography,
Nonthaburi, Thailand).
Measurement of total PLA2 in the
liver
The activity of liver PLA2 was measured via a PLA2
assay kit (cat no. ab133090; Abcam, Cambridge, MA, USA). Liver
tissues were weighed and homogenized in ice-cold 50 mmol/l sodium
phosphate buffer (pH 7.4) containing 1 mM EDTA. Homogenates were
centrifuged (10,000 xg for 15 min at 4°C) and supernatants were
stored at −80°C. Prior to performing the assay,
low-molecular-weight contaminants were removed from the samples
using an ultra-filtration unit via centrifugation through a 10-kDa
molecular mass cut-off filter (Amicon, Millipore Corporation,
Bedford, MA, USA) for 30 min at 25°C. Samples were re-constituted
with 50 mmol/l sodium phosphate buffer (pH 7.4) containing 1 mM
EDTA. Arachidonoyl thio-PC synthetic substrate was used to detect
PLA2 activity. Hydrolysis of the arachidonoyl thioester bond
releases a free thiol, which was detected by
5,5′-dithiobis-(2)-nitrobenzoic
acid. One unit of enzyme activity was defined as the amount of
enzyme that hydrolyzed one µmol of arachidonoyl thio-PC per
minute at 25°C.
Measurement of COX activity in the
liver
Liver tissues were weighed and homogenized in 0.1 M
ice-cold Tris-HCl buffer at pH 7.8 containing 1 mM EDTA. Tissue
homogenates were centrifuged at 10,000 xg for 15 min at 4°C and
supernatants were kept at −80°C until assayed. COX activity was
measured using a COX activity assay kit (cat no. 760151; Cayman
Chemical) according to manufacturer's instructions. The COX
activity assay kit measures enzyme activity colorimetrically by
monitoring the appearance of oxidized
N,N,N′,N′-tetramethyl-p-phenylenediamine (TMPD) at 590 nm on
a microplate spectrophotometer (BioTek Instruments, Inc., Winooski,
VT, USA). One unit of enzyme activity was defined as the amount of
enzyme that caused the oxidation of 1 nmol of TMPD per minute at
25°C.
Determination of PGE2
PGE2 was quantified in tissue samples by a
commercial enzyme immunoassay test kit (cat no. 514010; Cayman
Chemical) according to manufacturer's instructions. Liver tissues
were weighed and homogenized in 0.1 M ice-cold phosphate buffer at
pH 7.4 containing 1 mM EDTA and 10 µM indomethacin. Tissue
homogenates were centrifuged at 10,000 xg for 15 min at 4°C and
supernatants were kept at −80°C until assayed. Briefly, PGE2
present in the sample competes with acetylcholinesterase-labeled
PGE2 antibody for binding sites on a goat polyclonal anti-mouse
antibody. Following washing to remove unbound materials, a
substrate solution was added to the wells to determine the bound
enzyme activity. The color development was stopped, and the
absorbance was read at 412 nm. The intensity of the color was
inversely proportional to the concentration of PGE2 in the sample.
A standard curve of absorbance values of known PGE2 standards was
plotted as a function of the logarithm of PGE2 standard
concentrations (pg/ml) using the GraphPad Prism Software program
for windows version 5,03. (GraphPad Software Inc, La Jolla, CA,
USA). PGE2 concentrations in the samples were calculated from their
corresponding absorbance values via the standard curve.
Protein measurements
Protein concentrations were measured at 595 nm by a
modified Bradford assay using Coomassie Plus reagent with bovine
serum albumin as a standard (Pierce Chemical Company, Rockford, IL,
USA).
Statistical analysis
Data were analyzed using Sigma Stat (version 2.03;
SyStat Software, Inc., San Jose, CA, USA) statistical software for
Windows, and P<0.05 was considered to indicate a statistically
significant difference between values. Values are expressed as the
mean ± standard deviation. Statistical analyses for each
measurement are specified in the figure and table legends.
Results
Confirmation of IR-induced liver
injury
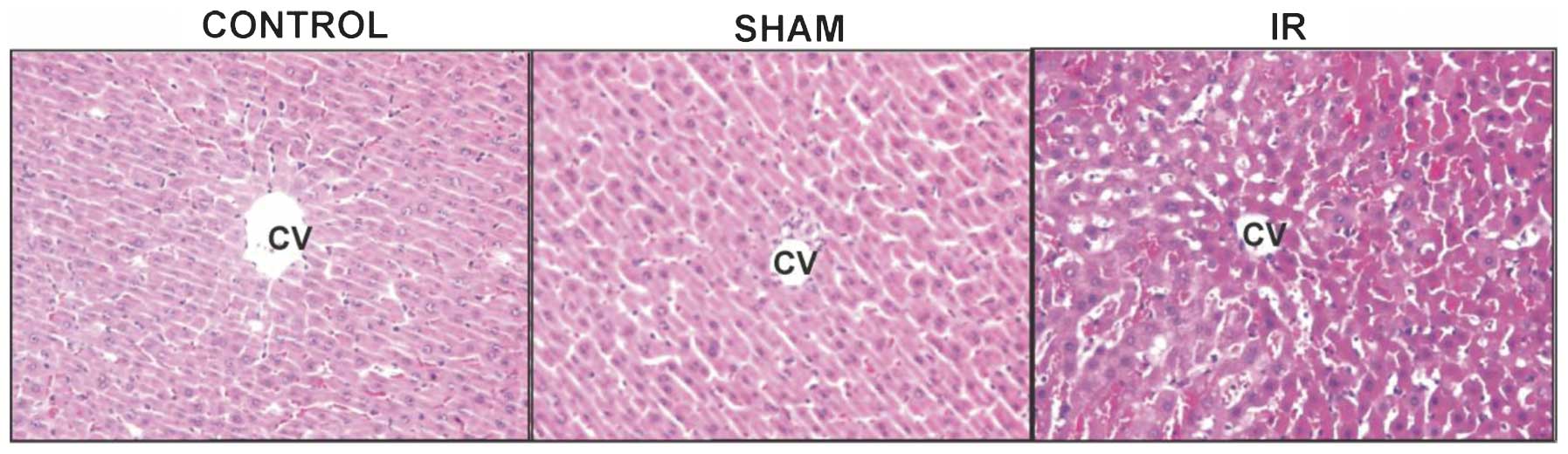
Representative hepatic photomicrographs of rats from
each group are shown in Fig. 1.
Histopathological scores of IR-induced liver injury are listed in
Table I. Intracellular edema,
necrosis and total histopathological score were significantly
greater (P<0.05) in the IR group compared to those in the sham
and control groups. ALT levels following IR-induced liver injury
are stated in Table II. Serum ALT
levels were significantly increased in the IR group compared with
those in the other groups, confirming the presence of hepatic
injury.
 | Table IHistopathological scores of liver
sections. |
Table I
Histopathological scores of liver
sections.
| Group | Congestion | Intracellular
edema | Necrosis | Total score |
|---|
| Sham (n=4) | 0.50±0.58 | 0.50±0.58 | 0.75±0.50 | 1.75±0.50 |
| Control (n=8) | 1.25±0.89 | 0.63±0.52 | 0.25±0.46 | 2.13±1.46 |
| IR (n=8) | 2.00±1.07a | 1.88±0.64b | 1.88±0.84b | 5.75±2.12b |
 | Table IIPlasma activity of ALT. |
Table II
Plasma activity of ALT.
| Group | n | Plasma ALT
(U/l) |
|---|
| Control | 10 | 27.56±4.41 |
| Sham | 5 | 24.61±2.40 |
| IR | 10 |
198.25±44.56a |
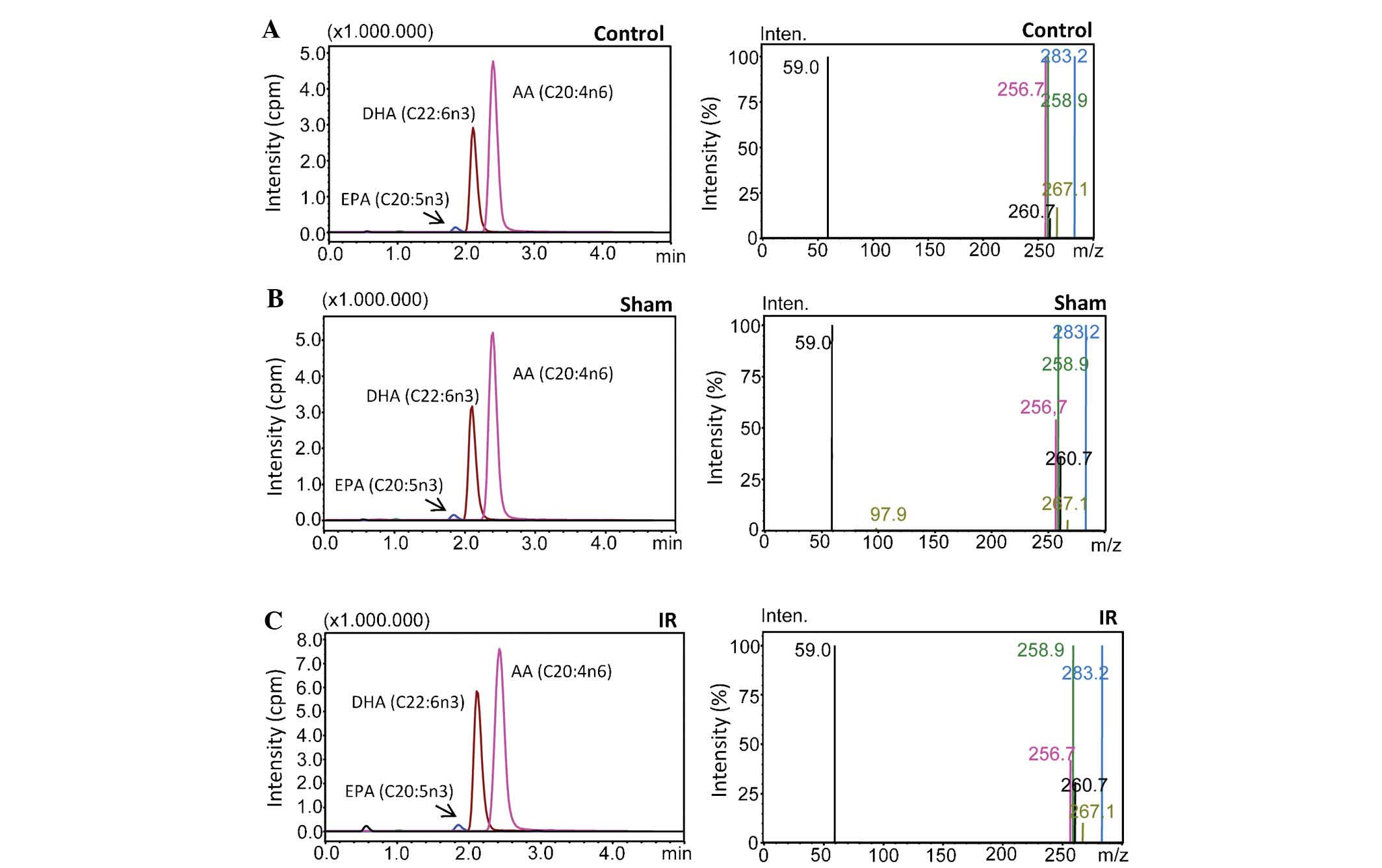
ESI-MS spectra
The precursor and product m/z values for analyzed
PUFAs were as follows: DGLA (C20:3n6), precursor m/z: 304.80,
product m/z: 59.00 and 260.70; AA (C20:4n6), precursor m/z: 303.10,
product m/z: 59.00 and 258.90; EPA (C20:5n3), precursor m/z:
301.10, product m/z: 59.10 and 256.70; DHA (C22:6n3), precursor
m/z: 327.10, product m/z: 59.10 and 283.20; AA-d8, precursor m/z:
311.10, product m/z: 59.10 97.90 and 267.10. Fig. 2A–C shows representative negative
ion mode spectra of a control, sham and IR tissue sample,
respectively. As shown in Fig. 2
(left-hand panel), the retention time of EPA (C20:5n-3), DHA
(C22:6n-3) and AA (C20:4n-6) was 1.869, 2.131 and 2.391 min,
respectively. The right-hand panel of Fig. 2 shows tandem mass spectra obtained
by collision-induced dissociation of precursor ions. The m/z values
of the product ions corresponded to endogenous C20:5n3, C20:4n6,
C20:3n6 and C22:6n3. The deuterium-labeled internal standard fatty
acid peaks are indicated at m/z 97.9 and 267.1.
Levels of PUFAs are increased following
IR-induced liver injury
Levels of PUFAs were determined by integration of
the chromatograms from LC-MS/MS analysis. Levels of PUFAs in the
control, sham and IR groups are listed in Table III. Endogenous tissue levels of
DGLA, AA, EPA and DHA were significantly increased following IR
injury when compared to those in the control and sham groups. No
significant differences in the AA/DHA and AA/EPA ratios was
observed among the experimental groups.
 | Table IIIAnalysis of polyunsaturated fatty
acids in liver tissue. |
Table III
Analysis of polyunsaturated fatty
acids in liver tissue.
| Parameter | Control (n=10) | Sham (n=5) | IR (n=10) |
|---|
| DGLA (C20:3n6) | 2.95±1.56 | 4.98±1.94 | 7.86±2.41a |
| AA (C20:4n6) | 29.36±12.73 | 38.26±17.72 | 62.16±17.68a |
| EPA (C20:5n3) | 0.86±0.53 | 0.80±0.13 | 2.27±0.87a |
| DHA (C22:6n3) | 10.02±4.82 | 10.67±2.39 | 20.43±7.63a |
| AA/DHA | 3.01±0.76 | 3.53±1.14 | 3.26±1.06 |
| AA/EPA | 39.07±12.83 | 29.39±7.86 | 26.32±2.57 |
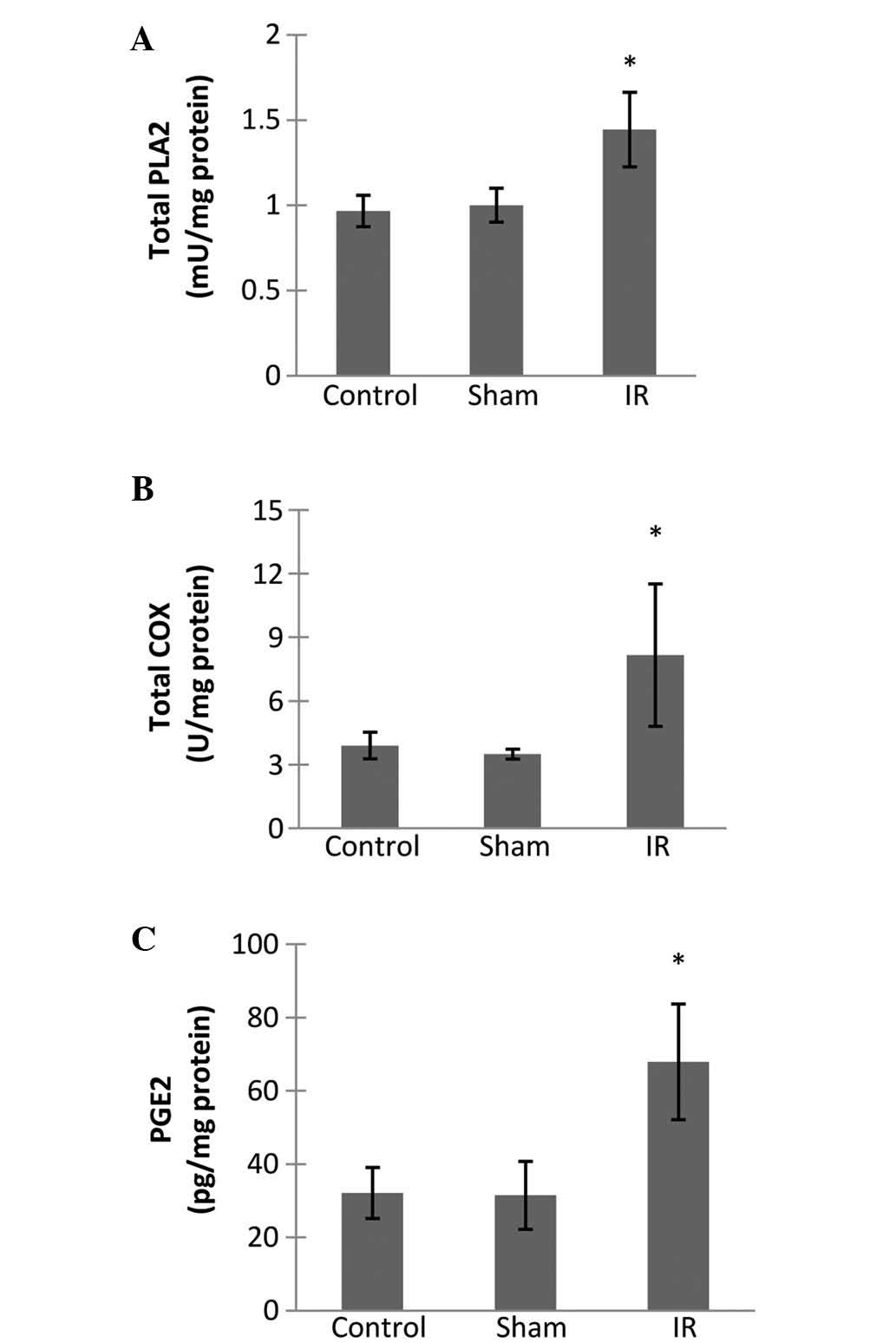
Total PLA2 activity is increased in liver
tissue following IR-induced injury
Total PLA2 activity measured in IR tissue
homogenates (n=10) was significantly higher compared to that in the
control (n=10) and sham (n=5) groups with values of 1.44±0.22 vs.
0.97±0.09 and 1.00±0.10 mU/mg protein, respectively (Fig. 3A). No significant difference was
observed between control and sham groups.
Total COX activity is increased in the
liver following IR-induced injury
Total COX activity in IR tissue homogenates (n=10)
was significantly higher compared to that in the control (n=10) and
sham (n=5) groups with levels of 8.16±3.36 vs. 3.90±0.63 and
3.49±0.23 U/mg protein, respectively (Fig. 3B). No significant difference was
observed between control and sham groups.
PGE2 content in the liver is increased
following IR
The PGE2 content in the liver is shown in Fig. 3C. PGE2 measured in IR samples
(67.91±15.81 pg/mg protein) was significantly higher compared to
that in the control (32.12±6.96 pg/mg protein) and sham (31.47±9.28
pg/mg protein) groups. No significant difference was observed
between control and sham groups.
Discussion
The present study investigated changes of endogenous
PUFA levels following liver IR injury in rats without n-3 or n-6
dietary supplementation. To the best of our knowledge, the present
study was the first to measure endogenous DGLA (C20:3n-6), AA
(C20:4n-6), DHA (C22:6n-3) and EPA (C20:5n-3) levels following
liver IR injury via optimized multiple reaction monitoring using
LC-MS/MS.
Clamping of the hepatic artery and portal vein
(Pringle manoeuvre) is often employed to reduce excessive blood
loss during liver resection (20).
This procedure unavoidably leads to warm IR injury. In the present
study, vessels supplying the median and left lateral hepatic lobes
were clamped for 60 min and subsequent re-perfusion for 60 min via
removal of the microvascular clip. Serum ALT activity was
significantly increased in this model of warm liver IR. The
increase in serum activity of ALT is a specific marker of liver
damage (21) and thus confirms the
presence of hepatic injury in the animal model used herein.
Considering that ALT activity in the liver is significantly greater
than that in serum, a small amount of enzyme released from tissue
can cause a significant increase in circulating plasma levels of
the enzyme. Histopathological evaluation of liver sections
confirmed the presence of liver IR injury and was in agreement with
biochemical findings of increased serum activity of ALT. As stated
above, the total histopathological score of liver IR injury was
obtained by summation of all scores for intracellular edema,
congestion and necrosis. Histopathological evaluation revealed that
intracellular edema, congestion and necrosis in IR-injured livers
were greater than those in the control and sham groups; these
results are reflected in the total score which was significantly
higher in livers that underwent IR.
Liver AA (C20:4n-6), DGLA (C20:3n-6), EPA (C20:5n-3)
and DHA (C22:6n-3) were significantly increased following IR injury
compared to those in the control and sham groups. No significant
difference was observed in the AA/DHA and AA/EPA ratio between the
IR injury group and the control and sham groups. Competition
between n-6 and n-3 fatty acids occurs in the production of
eicosanoids by stereospe-cific lipid-oxidizing enzymes COX and
lipoxygenase (22). Eicosanoids,
derived mainly from AA (C20:4n-6), are key mediators and regulators
of inflammation. These include prostaglandins (PGs), thromboxanes
(TXs) and leukotrienes (LTs) (9).
Elevated liver AA (C20:4n-6) levels may thus be a source of
pro-aggregatory substances in liver IR injury (23). In this context, it is important to
note that decreased levels of prostacyclin and increased levels of
TXs and LTs are associated with abnormalities in the ratio of
vasodilator to vasoconstrictor mediators in liver IR injury
(24).
Eicosapentaenoic acid (C20:5n3) is a precursor of
eicosanoids with a less marked inflammatory effect. Lipoxins,
resolvins and protectins generated from EPA (C20:5n3) and DHA
(C22:6n3) display potent anti-inflammatory properties and are
recognized in the resolution of inflammation (10). Hence, increased EPA and DHA levels
indicate more precursors for the synthesis of anti-inflammatory
eicosanoids.
Previous studies have demonstrated a marked release
of prostanoids from hepatic tissue after liver transplantation
(25). Increased eicosanoid
synthesis is shown to be regulated at the level of key enzymes
(26). The present study has
addressed changes of the local availability of these enzymes after
warm liver IR injury. It was observed that total PLA2 activity
measured in IR tissue homogenates was significantly higher compared
to that in the control and sham groups. Accumulating evidence has
revealed that PLA2 has an important role in IR injury (27,28).
In fact, the PLA2 inhibitor LY329722 was shown to attenuate hepatic
IR injury caused by 2-h total hepatic vascular exclusion in dogs
(28). PLA2 degrades cell membrane
phospholipids and has an important role in the synthesis of
pro-inflammatory lipid mediators, including AA (C20:4n-6) and
cytokines, during IR injury after liver transplantation (28). PLA2 comprises a large group of
enzymes that include secretory PLA2 (sPLA2), cytosolic PLA2 and
calcium-independent PLA2 families (29). These enzymes hydrolyze the
phospholipid bond at the sn-2 position. Cytosolic PLA2 and
calcium-independent PLA2 are localized inside the cell and are
involved in the breakdown of intracellular membranes, whereas sPLA2
is secreted during inflammatory events (30). PLA2 accelerates the breakdown of
membrane phospholipids in the liver and other organs under warm
ischemia and releases free fatty acids including AA (C20:4n-6) and
lysophospholipids (31). Increased
total PLA2 activity observed in the experimental model of the
present study may therefore explain increased levels of measured
PUFAs in liver tissues. Free fatty acids released via the action of
PLA2 are metabolized into PGs, TXs, LTs and platelet-activating
factor (32). These lipid
derivatives have pro-inflammatory and vasoconstrictive effects and
contribute to post-ischemic organ dysfunction.
The activity of COX, the initial enzyme of
prostaglandin synthesis, was also measured in liver tissue
following IR injury. COX is the rate-limiting enzyme in the
production of prostanoids from arachidonic acid. Studies have shown
that the COX/prostanoid pathway is activated in hepatic diseases
and liver stress reactions, including alcoholic liver disease
(33), liver fibrogenesis
(34), viral hepatitis C (35) and IR injury of the liver (36), causing liver damage manifested as
inflammation, necrosis and fatty liver. In agreement with previous
studies, the results of the present study revealed a significantly
increased activity of COX following IR-induced injury of the liver
compared to that in the control and sham groups, suggesting that
the formation of prostanoids via the COX/prostanoid pathway also
has a role in the observed tissue damage.
The present study reported significantly increased
liver PGE2 levels following IR in agreement with previous studies
(25). Arachidonic acid is a
precursor of PGE2 synthesis and production of PGs are formed by
stereospecific lipid-oxidizing enzymes. PGE2, produced during
inflammatory responses, mediates a variety of innate and adaptive
immune responses through four receptor sub-types (37). Each receptor functions via a
distinct signaling cascade and has a unique role in a variety of
disease conditions (37). In the
liver, endogenous PGE2 is produced mainly by activated Kupffer
cells during hepatic injury (38).
Previous studies have demonstrated that endogenous as well as
exogenous PGE2 is protective against liver injury caused by IR
(39). This effect may be due to
increased inhibition of platelet aggregation, liver perfusion or
direct cytoprotection by PGE2 (40). PGE2 has also been suggested to
restore liver damage through the regulation of cytokine cascades
(38).
In conclusion, the present study revealed that
IR-induced liver injury significantly increased the concentration
of AA (C20:4n-6), DGLA (C20:3n-6), EPA (C20:5n-3) and DHA
(C22:6n-3) in liver tissue specimens and had no effect on the
hepatic AA/DHA and AA/EPA ratios. The observed increase of
endogenous PUFA levels in the liver following IR injury was
accompanied by increased activity of the key enzymes PLA2 and COX,
which are involved in the production of prostanoids. The results of
the present study therefore suggested that increased hydrolysis of
fatty acids via PLA2 triggers the activity of COX and leads to
increased PGE2 levels. Future studies evaluating agents which block
the formation of eicosanoids derived from n-6 PUFAs may facilitate
the development and application of treatment strategies in liver
injury following IR.
Acknowledgments
This study was supported by a grant from The
Scientific and Technological Research Council of Turkey (TUBITAK;
grant no. SBAG-113S999) and a grant from the Akdeniz University
Research Foundation (grant no. 2014.02.0122.015).
References
|
1
|
Hasselgren PO: Prevention and treatment of
ischemia of the liver. Surg Gynecol Obstet. 164:187–196.
1987.PubMed/NCBI
|
|
2
|
Lemasters JJ and Thurman RG: Reperfusion
injury after liver preservation for transplantation. Annu Rev
Pharmacol Toxicol. 37:327–338. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Olthoff KM: Can reperfusion injury of the
liver be prevented? Trying to improve on a good thing. Pediatr
Transplant. 5:390–393. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Dogan S and Aslan M: Hepatic
ischemia-reperfusion injury and therapeutic strategies to alleviate
cellular damage. Hepatol Res. 41:103–117. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Colletti LM, Kunkel SL, Walz A, Burdick
MD, Kunkel RG, Wilke CA and Strieter RM: The role of cytokine
networks in the local liver injury following hepatic
ischemia/reperfusion in the rat. Hepatology. 23:506–514. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Jaeschke H, Farhood A and Smith CW:
Neutrophils contribute to ischemia/reperfusion injury in rat liver
in vivo. FASEB J. 4:3355–3359. 1990.PubMed/NCBI
|
|
7
|
Bates EJ, Ferrante A, Smithers L, Poulos A
and Robinson BS: Effect of fatty acid structure on neutrophil
adhesion, degranulation and damage to endothelial cells.
Atherosclerosis. 116:247–259. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
De Caterina R, Liao JK and Libby P: Fatty
acid modulation of endothelial activation. Am J Clin Nutr. 71(1
Suppl): 213S–223S. 2000.PubMed/NCBI
|
|
9
|
Wall R, Ross RP, Fitzgerald GF and Stanton
C: Fatty acids from fish: The anti-inflammatory potential of
long-chain omega-3 fatty acids. Nutr Rev. 68:280–289. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Serhan CN, Chiang N and Van Dyke TE:
Resolving inflammation: Dual anti-inflammatory and pro-resolution
lipid mediators. Nat Rev Immunol. 8:349–361. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Marsman HA, Heger M, Kloek JJ, Nienhuis
SL, ten Kate FJ and van Gulik TM: Omega-3 fatty acids reduce
hepatic steatosis and consequently attenuate ischemia-reperfusion
injury following partial hepatectomy in rats. Dig Liver Dis.
43:984–990. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Coelho AM, Machado MC, Takahashi HK,
Sampietre SN, Stefano JT, Leite AZ, Curi R and D'Albuquerque LA:
Ischemic preconditioning-like effect of polyunsaturated fatty
acid-rich diet on hepatic ischemia/reperfusion injury. J
Gastrointest Surg. 15:1679–1688. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zúñiga J, Cancino M, Medina F, Varela P,
Vargas R, Tapia G, Videla LA and Fernández V: N-3 PUFA
supplementation triggers PPAR-α activation and PPAR-α/NF-κB
interaction: Anti-inflammatory implications in liver
ischemia-reperfusion injury. PLoS One. 6:e285022011. View Article : Google Scholar
|
|
14
|
Zhu XH, Wu YF, Qiu YD, Jiang CP and Ding
YT: Liver-protecting effects of omega-3 fish oil lipid emulsion in
liver transplantation. World J Gastroenterol. 18:6141–6147. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Dogan S, Ozlem Elpek G, Kirimlioglu Konuk
E, Demir N and Aslan M: Measurement of intracellular biomolecular
oxidation in liver ischemia-reperfusion injury via immuno-spin
trapping. Free Radic Biol Med. 53:406–414. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Curek GD, Cort A, Yucel G, Demir N, Ozturk
S, Elpek GO, Savas B and Aslan M: Effect of astaxanthin on
hepatocellular injury following ischemia/reperfusion. Toxicology.
267:147–513. 2010. View Article : Google Scholar
|
|
17
|
Yilmaz S, Ates E, Tokyol C, Pehlivan T,
Erkasap S and Koken T: The protective effect of erythropoietin on
ischaemia/reperfusion injury of liver. HPB (Oxford). 6:169–173.
2004. View Article : Google Scholar
|
|
18
|
Aslan M, Aslan I, Özcan F, Eryılmaz R,
Ensari CO and Bilecik T: A pilot study investigating early
postoperative changes of plasma polyunsaturated fatty acids after
laparoscopic sleeve gastrectomy. Lipids Health Dis. 13:622014.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Aslan M, Özcan F, Aslan I and Yücel G:
LC-MS/MS analysis of plasma polyunsaturated fatty acids in type 2
diabetic patients after insulin analog initiation therapy. In:
Lipids Health Dis. 12. pp. 1692013
|
|
20
|
van Gulik TM, de Graaf W, Dinant S, Busch
OR and Gouma DJ: Vascular occlusion techniques during liver
resection. Dig Surg. 24:274–281. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ozer J, Ratner M, Shaw M, Bailey W and
Schomaker S: The current state of serum biomarkers of
hepatotoxicity. Toxicology. 245:194–205. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Calder PC: Polyunsaturated fatty acids,
inflammation and immunity. Lipids. 36:1007–1024. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Setty BN, Dampier CD and Stuart MJ:
Arachidonic acid metabolites are involved in mediating red blood
cell adherence to endothelium. J Lab Clin Med. 125:608–617.
1995.PubMed/NCBI
|
|
24
|
Besse T, Gustin T, Claeys N, Schroeyers P
and Lambotte L: Effect of PGI2 and thromboxane antagonist on liver
ischemic injury. Eur Surg Res. 21:213–217. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Post S, Goerig M, Otto G, Manner M,
Senninger N, Kommerell B and Herfarth C: Prostanoid release in
experimental liver transplantation. Transplantation. 49:490–494.
1990. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Post S, Goerig M, Otto G, Manner M, Foltis
C, Hofmann W and Herfarth C: Rapid increase in the activity of
enzymes of eicosanoid synthesis in hepatic and extrahepatic tissues
after experimental liver transplantation. Transplantation.
51:1058–1065. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Koike K, Yamamoto Y, Hori Y and Ono T:
Group IIA phospholipase A2 mediates lung injury in intestinal
ischemia-reperfusion. Ann Surg. 232:90–97. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ogata K, Jin MB, Taniguchi M, Suzuki T,
Shimamura T, Kitagawa N, Magata S, Fukai M, Ishikawa H, Ono T, et
al: Attenuation of ischemia and reperfusion injury of canine livers
by inhibition of type II phospholipase A2 with LY329722.
Transplantation. 71:1040–1046. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Murakami M and Kudo I: Phospholipase A2. J
Biochem. 131:285–292. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Menschikowski M, Hagelgans A and Siegert
G: Secretory phospholipase A2 of group IIA: Is it an offensive or a
defensive player during atherosclerosis and other inflammatory
diseases? Prostaglandins Other Lipid Mediat. 79:1–33. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Dan P, Nitzan DW, Dagan A, Ginsburg I and
Yedgar S: H2O2 renders cells accessible to
lysis by exogenous phospholipase A2: A novel mechanism for cell
damage in inflammatory processes. FEBS Lett. 383:75–78. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Murakami M, Nakatani Y, Atsumi G, Inoue K
and Kudo I: Regulatory functions of phospholipase A2. Crit Rev
Immunol. 17:225–283. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Nanji AA, Miao L, Thomas P, Rahemtulla A,
Khwaja S, Zhao S, Peters D, Tahan SR and Dannenberg AJ: Enhanced
cyclo-oxygenase-2 gene expression in alcoholic liver disease in the
rat. Gastroenterology. 112:943–951. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Planagumà A, Clària J, Miquel R,
López-Parra M, Titos E, Masferrer JL, Arroyo V and Rodés J: The
selective cyclooxy-genase-2 inhibitor SC-236 reduces liver fibrosis
by mechanisms involving non-parenchymal cell apoptosis and
PPARgamma activation. FASEB J. 19:1120–1122. 2005.
|
|
35
|
Waris G and Siddiqui A: Hepatitis C virus
stimulates the expression of cyclooxygenase-2 via oxidative stress:
Role of pros-taglandin E2 in RNA replication. J Virol.
79:9725–9734. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Kim SH and Lee SM: Expression of hepatic
vascular stress genes following ischemia/reperfusion and subsequent
endotoxemia. Arch Pharm Res. 27:769–775. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Breyer RM, Bagdassarian CK, Myers SA and
Breyer MD: Prostanoid receptors: Subtypes and signaling. Annu Rev
Pharmacol Toxicol. 41:661–690. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Wanner GA, Müller P, Ertel W, Busch CJ,
Menger MD and Messmer K: Differential effect of cyclooxygenase
metabolites on proinflammatory cytokine release by Kupffer cells
after liver ischemia and reperfusion. Am J Surg. 175:146–151. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Arai M, Peng XX, Currin RT, Thurman RG and
Lemasters JJ: Protection of sinusoidal endothelial cells against
storage/reperfusion injury by prostaglandin E2 derived from Kupffer
cells. Transplantation. 68:440–445. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Masaki N, Ohta Y, Shirataki H, Ogata I,
Hayashi S, Yamada S, Hirata K, Nagoshi S, Mochida S, Tomiya T, et
al: Hepatocyte membrane stabilization by prostaglandins E1 and E2:
Favorable effects on rat liver injury. Gastroenterology.
102:572–576. 1992.PubMed/NCBI
|