|
1
|
Xing ZW, Wang J, Ke H, et al: The
fabrication of novel nano-bubble ultrasound contrast agent for
potential tumor imaging. Nanotechnology. 21:1456072010. View Article : Google Scholar
|
|
2
|
Tran TD, Caruthers SD, Hughes M, et al:
Clinical applications of perfluorocarbon nanoparticles for
molecular imaging and targeted therapeutics. Int J Nanomedicine.
2:515–526. 2007.
|
|
3
|
Quaia E: Microbubble ultrasound contrast
agents: an update. Eur Radiol. 17:1995–2008. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sun C, Sboros V, Butler MB and Moran CM:
In vitro acoustic characterization of three phospholipid ultrasound
contrast agents from 12 to 43 MHz. Ultrasound Med Biol. 40:541–550.
2014. View Article : Google Scholar :
|
|
5
|
Pfister K, Kasprzak PM, Apfelbeck H, et
al: The significance of contrast-enhanced ultrasound in vascular
surgery. Zentralbl Chi. Dec 10–2013.(Epub ahead of print) (In
German).
|
|
6
|
Liu H, Jiang Y, Dai Q, et al: Peripheral
enhancement of breast cancers on contrast-enhanced ultrasound:
correlation with microvessel density and vascular endothelial
growth factor expression. Ultrasound Med Biol. 40:293–299. 2014.
View Article : Google Scholar
|
|
7
|
Malinova M: Preoperative sonovue contrast
color Doppler in patients with cervical cancer. Preliminary report.
Akush Ginekol (Sofiia). 52(Suppl 1): 11–16. 2013.In Bulgarian.
|
|
8
|
Hoffmann R, von Bardeleben S, Barletta G,
et al: Comparison of two- and three-dimensional unenhanced and
contrast-enhanced echocardiographies versus cineventriculography
versus cardiac magnetic resonance for determination of left
ventricular function. Am J Cardiol. 113:395–401. 2014. View Article : Google Scholar
|
|
9
|
Sartori S, Postorivo S, Vece FD, et al:
Contrast-enhanced ultrasonography in peripheral lung
consolidations: What's its actual role? World J Radiol. 5:372–380.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Saracco A, Szabó BK, Aspelin P, et al:
Contrast-enhanced ultrasound using real-time contrast harmonic
imaging in invasive breast cancer: comparison of enhancement
dynamics with three different doses of contrast agent. Acta Radiol.
Jan 20–2014.Epub ahead of print. PubMed/NCBI
|
|
11
|
Lisowska A, Knapp M, Tycinska A, et al:
Usefulness of automatic measurement of contrast flow intensity: an
innovative tool in contrast-enhanced ultrasound imaging of
atherosclerotic carotid plaque neovascularization. A pilot study.
Int Angiol. 33:50–57. 2014.PubMed/NCBI
|
|
12
|
Nagesha D, Laevsky GS, Lampton P, et al:
In vitro imaging of embryonic stem cells using multiphoton
luminescence of gold nanoparticles. Int J Nanomedicine. 2:813–819.
2007.
|
|
13
|
Threlfall G, Wu HJ, Li K, et al:
Quantitative guidelines for the prediction of ultrasound contrast
agent destruction during injection. Ultrasound Med Biol.
39:1838–1847. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
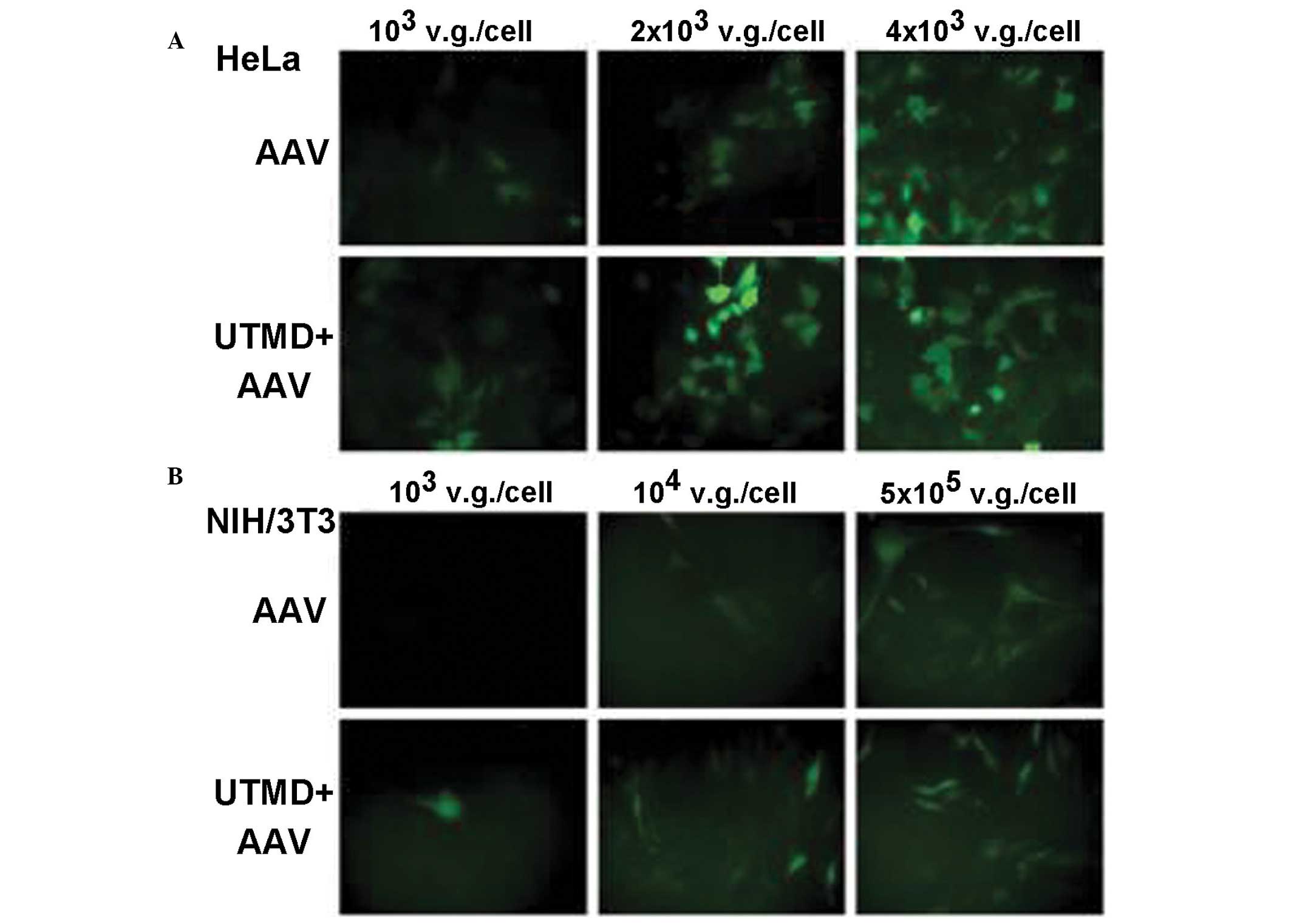
Chen ZY, Liang K, Lin Y and Yang F: Study
of the UTMD-based delivery system to induce cervical cancer cell
apoptosis and inhibit proliferation with shRNA targeting Survivin.
Int J Mol Sci. 14:1763–1777. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Li F, Jin L, Wang H, et al: The dual
effect of ultrasound-targeted microbubble destruction in mediating
recombinant adeno-associated virus delivery in renal cell
carcinoma: transfection enhancement and tumor inhibition. J Gene
Med. 16:28–39. 2014. View
Article : Google Scholar : PubMed/NCBI
|
|
16
|
Liu H, Chang S, Sun J, et al:
Ultrasound-mediated destruction of LHRHa-targeted and
paclitaxel-loaded lipid microbubbles induces proliferation
inhibition and apoptosis in ovarian cancer cells. Mol Pharm.
11:40–48. 2014. View Article : Google Scholar :
|
|
17
|
Pu C, Chang S, Sun J, et al:
Ultrasound-mediated destruction of LHRHa-targeted and
paclitaxel-loaded lipid microbubbles for the treatment of
intraperitoneal ovarian cancer xenografts. Mol Pharm. 11:49–58.
2014. View Article : Google Scholar :
|
|
18
|
Yan P, Chen KJ, Wu J, et al: The use of
MMP2 antibody-conjugated cationic microbubble to target the
ischemic myocardium, enhance Timp3 gene transfection and improve
cardiac function. Biomaterials. 35:1063–1073. 2014. View Article : Google Scholar
|
|
19
|
Deng Q, Chen JL, Zhou Q, et al: Ultrasound
microbubbles combined with the NFκB binding motif increase
transfection efficiency by enhancing the cytoplasmic and nuclear
import of plasmid DNA. Mol Med Rep. 8:1439–1445. 2013.PubMed/NCBI
|
|
20
|
Ling ZY, Shu SY, Zhong SG, et al:
Ultrasound targeted micro-bubble destruction promotes angiogenesis
and heart function by inducing myocardial microenvironment change.
Ultrasound Med Biol. 39:2001–2010. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hao YN, Luo WL, Wang D and Wang ZG:
Experimental research on treatment of injured facial nerves induced
by hepatocyte growth factor mediated by ultrasound-targeted
microbubble destruction. J Craniofac Surg. 24:421–424. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yang D, Gao YH, Tan KB, et al: Inhibition
of hepatic fibrosis with artificial microRNA using ultrasound and
cationic liposome-bearing microbubbles. Gene Ther. 20:1140–1148.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Prentice P, Cushierp A, Dholakiak, et al:
Membrane disruption by optically controlled microbubble
cavitiation. Nat Phys. 1:107–110. 2005. View Article : Google Scholar
|
|
24
|
Tachibana K, Uchida T, Ogawa K, et al:
Induction of cell-membrane porosity by ultrasound. Lancet.
353:14091999. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
van Wamel A, Kooiman K, Harteveld M, et
al: Vibrating micro-bubbles poking individual cells: drug transfer
into cells via sonoporation. J Control Release. 112:149–155. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Juffermans LJ, Dijkmans PA, Musters RJ, et
al: Transient permeabilization of cell membranes by
ultrasound-exposed microbubbles is related to formation of hydrogen
peroxide. Am J Physiol Heart Circ Physiol. 291:H1595–H1601. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Miller DL and Gies RA: The interaction of
ultrasonic heating and cavitation in vascular bioeffects on mouse
intestine. Ultrasound Med Biol. 24:123–128. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Schlicher RK, Radhakrishna H, Tolentino
TP, et al: Mechanism of intracellular delivery by acoustic
cavitation. Ultrasound Med Biol. 32:915–924. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Jin LF, Li F, Wang HP, et al: Ultrasound
targeted microbubble destruction stimulates cellular endocytosis in
facilitating adeno-associated virus delivery. Int J Mol Sci.
14:9737–9750. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Du J, Shi QS, Sun Y, et al: Enhanced
delivery of monomethoxypoly(ethylene
glycol)-poly(lactic-co-glycolic acid)-poly l-lysine nanoparticles
loading platelet-derived growth factor BB small interfering RNA by
ultrasound and/or micro-bubbles to rat retinal pigment epithelium
cells. J Gene Med. 13:312–323. 2011. View
Article : Google Scholar : PubMed/NCBI
|
|
31
|
Du J, Sun Y, Shi QS, et al: Biodegradable
nanoparticles of mPEG-PLGA-PLL triblock copolymers as novel
non-viral vectors for improving siRNA delivery and gene silencing.
Int J Mol Sci. 13:516–533. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Shi Q, Liu P, Sun Y, et al: siRNA delivery
mediated by copolymer nanoparticles, phospholipid stabilized
sulphur hexa-fluoride microbubbles and ultrasound. J Biomed
Nanotechnol. 10:436–444. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Jin L, Li F, Wang H, et al:
Ultrasound-targeted microbubble destruction enhances gene
transduction of adeno-associated virus in a less-permissive cell
type, NIH/3T3. Mol Med Rep. 8:320–326. 2013.PubMed/NCBI
|
|
34
|
Li HL, Zheng XZ, Wang HP, et al:
Ultrasound-targeted micro-bubble destruction enhances AAV-mediated
gene transfection in human RPE cells in vitro and rat retina in
vivo. Gene Ther. 16:1146–1153. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Zheng X, Du L, Wang H and Gu Q: A novel
approach to attenuate proliferative vitreoretinopathy using
ultrasound-targeted microbubble destruction and recombinant
adenoassociated virus-mediated RNA interference targeting
transforming growth factor-b2 and platelet-derived growth factor-B.
J Gene Med. 14:339–347. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
36
|
Li YH, Jin LF, Du LF, et al: Enhancing
HSP70-ShRNA transfection in 22RV1 prostate cancer cells by
combination of sonoporation, liposomes and HTERT/CMV chimeric
promoter. Int J Oncol. 43:151–158. 2013.PubMed/NCBI
|
|
37
|
Zhang Y, Ye C, Wang G, et al:
Kidney-targeted transplantation of mesenchymal stem cells by
ultrasound targeted microbubble destruction promotes kidney repair
in diabetic nephropathy rats. BioMed Res Int. 2013:5263672013.
View Article : Google Scholar
|
|
38
|
Li P, Gao Y, Zhang J, et al: Renal
interstitial permeability changes induced by microbubble enhanced
diagnostic ultrasound. J Drug Target. 21:507–514. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Jafari S, Diou O, Mamou J, Renault G, et
al: High-frequency (20 to 40 MHz) acoustic response of
liquid-filled nanocapsules. IEEE Trans Ultrason Ferroelectr Freq
Control. 61:5–15. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Hughes GA: Nanostructure-mediated drug
delivery. Nanomedicine. 1:22–30. 2005. View Article : Google Scholar
|
|
41
|
Lanza GM, Trousil RL, Wallace KD, et al:
In vitro characterization of a novel, tissue-targeted ultrasonic
contrast system with acoustic microscopy. J Acoust Soc Am.
104:3665–3672. 1998. View
Article : Google Scholar : PubMed/NCBI
|
|
42
|
Sciallero C, Paradossi G and Trucco A: A
preliminary in vitro assessment of polymer-shelled microbubbles in
contrast-enhanced ultrasound imaging. Ultrasonics. 52:456–464.
2012. View Article : Google Scholar
|
|
43
|
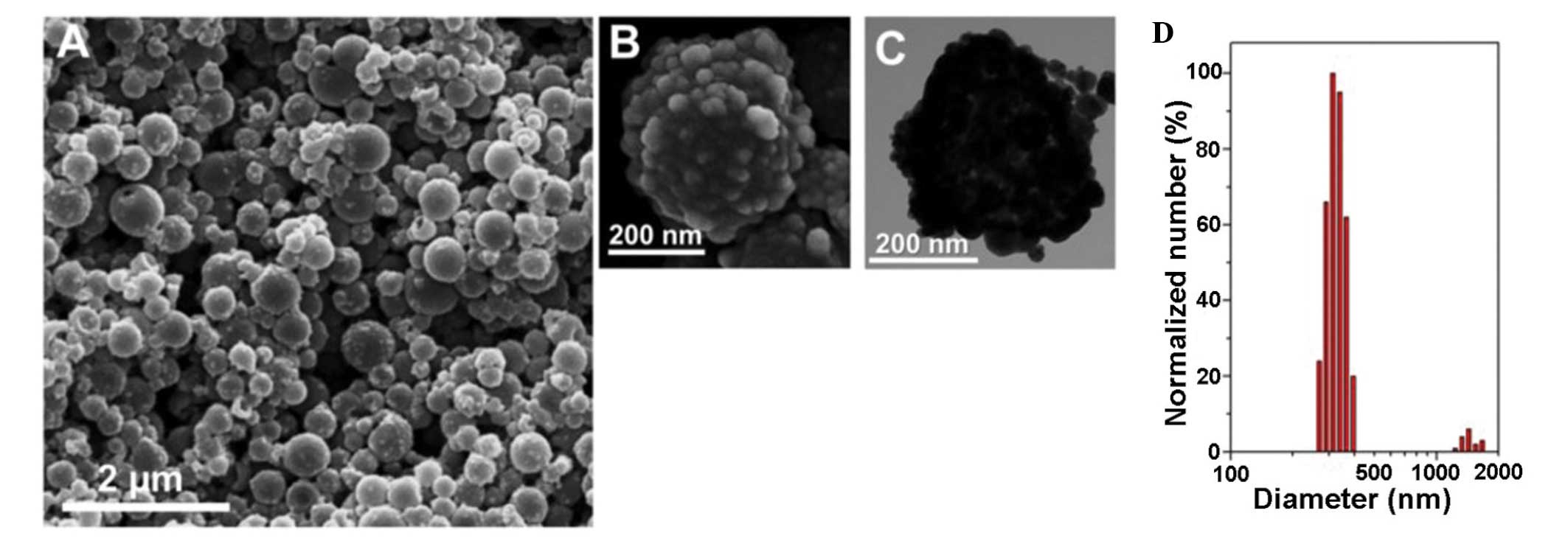
Nie L, Chen M, Sun X, et al: Palladium
nanosheets as highly stable and effective contrast agents for in
vivo photoacoustic molecular imaging. Nanoscale. 6:1271–1276. 2014.
View Article : Google Scholar
|
|
44
|
Trung, Tran TD, Caruthers SD, Hughes M, et
al: Clinical applications of perfluorocarbon nanoparticles for
molecular imaging and targeted therapeutics. Int J Nanomedicine.
2:515–526. 2007.
|
|
45
|
Milgroom A, Intrator M, Madhavan K, et al:
Mesoporous silica nanoparticles as a breast-cancer targeting
ultrasound contrast agent. Colloids Surf B Biointerfaces.
11:652–657. 2014. View Article : Google Scholar
|
|
46
|
Lin CA, Chuang WK, Huang ZY, et al: Rapid
transformation of protein-caged nanomaterials into microbubbles as
bimodal imaging agents. ACS Nano. 6:5111–5121. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Wilson KE, Wang TY and Willmann JK:
Acoustic and photo-acoustic molecular imaging of cancer. J Nucl
Med. 54:1851–1854. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Homan KA, Souza M, Truby R, et al: Silver
nanoplate contrast agents for in vivo molecular photoacoustic
imaging. ACS Nano. 6:641–650. 2012. View Article : Google Scholar
|
|
49
|
Ku G, Zhou M, Song S, et al: Copper
sulfide nanoparticles as a new class of photoacoustic contrast
agent for deep tissue imaging at 1064 nm. ACS Nano. 6:7489–7496.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Sciallero C and Trucco A: Ultrasound
assessment of polymer-shelled magnetic microbubbles used as dual
contrast agents. J Acoust Soc Am. 133:EL478–EL484. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Kim C, Qin R, Xu JS, Wang LV and Xu R:
Microbubbles and nanobubbles for photoacoustic and ultrasound
imaging. J Biomed Opt. 15:0105102010. View Article : Google Scholar
|
|
52
|
Xu JS, Huang J, Qin R, et al: Synthesizing
and binding dual-mode poly (lactic-co-glycolicacid) (PLGA)
nanobubbles for cancer targeting and imaging. Biomaterials.
31:1716–1722. 2010. View Article : Google Scholar
|
|
53
|
Mehrmohammadi M, Shin TH, Qu M, et al: In
vivo pulsed magneto-motive ultrasound imaging using
high-performance magnetoactive contrast nanoagents. Nanoscale.
5:11179–11186. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Nie L, Chen M, Sun X, et al: Palladium
nanosheets as highly stable and effective contrast agents for in
vivo photoacoustic molecular imaging. Nanoscale. 6:1271–1276. 2014.
View Article : Google Scholar
|
|
55
|
Park J, Park D, Shin U, et al: Synthesis
of laboratory ultrasound contrast agents. Molecules.
18:13078–13095. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Barnett BP, Ruiz-Cabello J, Hota P, et al:
Use of perfluorocarbon nanoparticles for non-invasive multimodal
cell tracking of human pancreatic islets. Contrast Media Mol
Imaging. 6:251–259. 2011.PubMed/NCBI
|
|
57
|
Anayama T, Nakajima T, Dunne M, et al: A
novel minimally invasive technique to create a rabbit VX2 lung
tumor model for nano-sized image contrast and interventional
studies. PLoS One. 8:e673552013. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Arifin DR, Kedziorek DA, Fu Y, et al:
Microencapsulated cell tracking. NMR Biomed. 26:850–859. 2013.
View Article : Google Scholar :
|
|
59
|
Cheng X, Li H, Chen Y, et al:
Ultrasound-triggered phase transition sensitive magnetic
fluorescent nanodroplets as a multimodal imaging contrast agent in
rat and mouse model. PLoS One. 8:e850032013. View Article : Google Scholar
|
|
60
|
Rapoport N, Gao Z and Kennedy A:
Multifunctional nanoparticles for combining ultrasonic tumor
imaging and targeted chemotherapy. J Natl Cancer Inst.
99:1095–1106. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
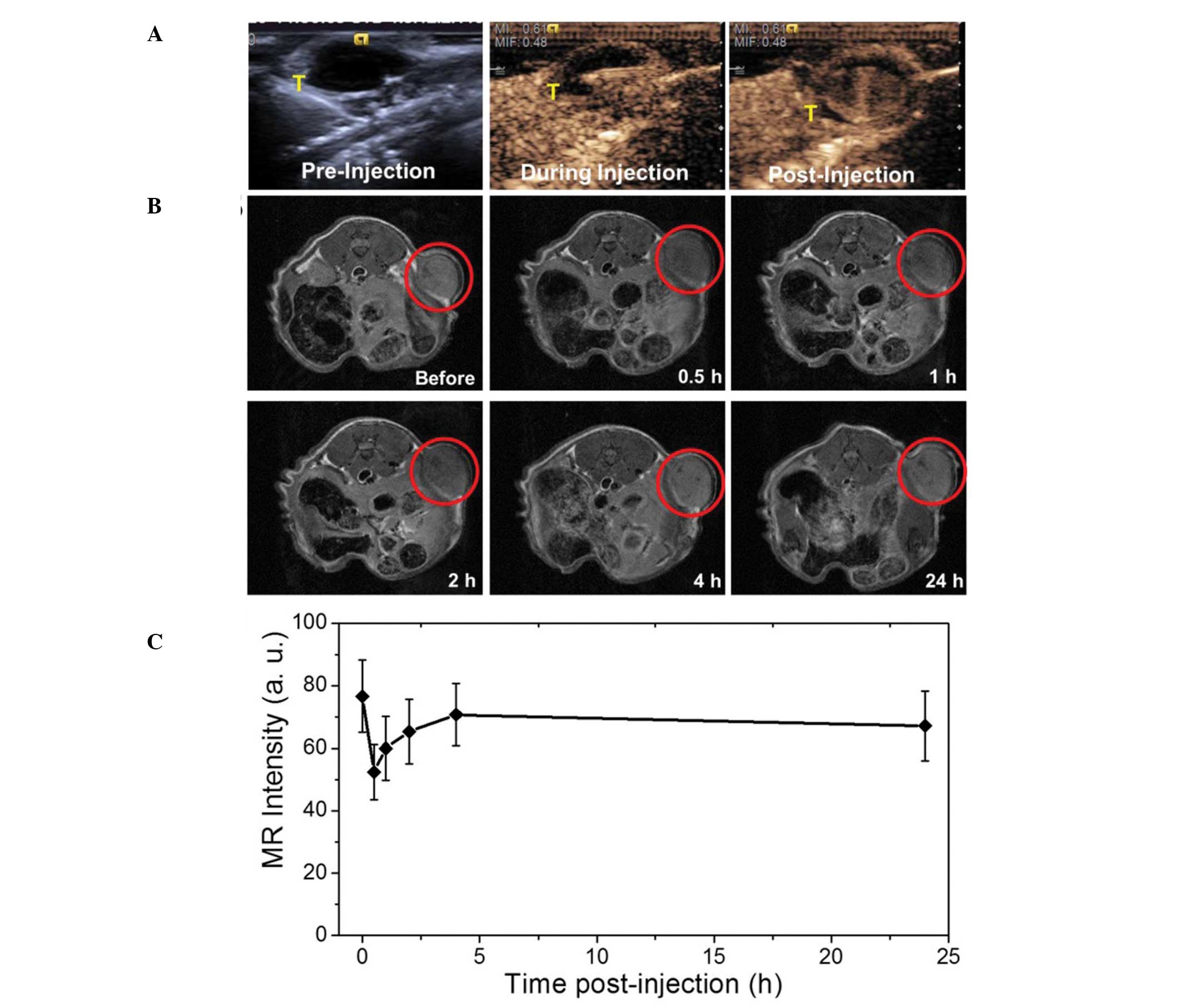
Ke H, Wang J, Dai Z, Jin Y, Qu E, Xing Z,
Guo C, Yue X and Liu J: Gold-nanoshelled microcapsules: A
theranostic agent for ultrasound contrast imaging and photothermal
therapy. Angew Chem Int Ed Engl. 50:3017–3021. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Ke H, Wang J, Tong S, et al: Gold
nanoshelled liquid perfluoro-carbon magnetic nanocapsules: a
nanotheranostic platform for bimodal ultrasound/magnetic resonance
imaging guided photo-thermal tumor ablation. Theranostics. 4:12–23.
2013. View Article : Google Scholar
|