Introduction
Liver injury induced by hepatic ischemia/reperfusion
(IR) is a major cause of hepatic failure following various forms of
circulatory shock, severe trauma, liver resection, orthotropic
liver transplantation or other surgical procedures where blood
supply to the liver is temporarily blocked (1). The mechanism of IR injury of the
liver is complicated and interactive. During the phase of IR,
hepatocyte damage occurs through lipid peroxidation, release of
reactive oxygen species, activation of signal transduction cascades
and production of various inflammatory mediators (2). Subsequently, cell death programs are
activated, including apoptosis, autophagy-associated cell death and
necrosis (3).
Several strategies, such as ischemic
preconditioning, remote ischemic preconditioning or pharmacological
preconditioning, that may protect the liver during IR injury have
been investigated (4). Among these
strategies, mild hypothermia has received increasing attention. The
modern clinical use of hypothermia was initiated in 1950 by Bigelow
et al (5) when the
neuroprotective effects were demonstrated during cardiac surgery.
For many years, therapeutic hypothermia has been applied to improve
the survival rate and neurological outcome of patients following
cardiac arrest. The beneficial effects of therapeutic hypothermia
include conservation of hepatic metabolism, and reduction in the
inflammatory response and apoptosis during ischemia (6,7).
However, there is a lack of consensus on the most appropriate
target temperature. Experimental studies (8,9) in
recent years have suggested that mild hypothermia (32–34°C) exert
more effective protection against warm IR injury of the liver.
Previous studies have focused on the investigation of therapeutic
hypothermia at 32–34°C. However, in selective cases the application
of mild hypothermia pretreatment may outweigh the risks, whereas
fewer studies were conducted on it and the mechanisms by which mild
hypothermia pretreatment protects liver against I/R injury are not
fully understood.
Previous studies (10,11)
demonstrate that the phosphatidylinositol-3-kinase (PI3K)/protein
kinase B (AKT) pathway has an important role in protection against
hepatic IR injury in rats. Activated AKT inhibits apoptosis by
phosphorylating a large number of downstream proteins (12). Several genetic and biochemical
studies have reported that the forkhead box O (FOXO) family is a
key downstream target of the PI3K/AKT pathway (13,14).
FOXO3a is a member of the FOXO family of transcription factors and
is expressed in the liver, pancreas, spleen, brain and other
tissues (15). FOXO3a induces
expression of target genes involved in crucial cellular processes,
including oxidative stress, glucose metabolism, inflammation
response and apoptosis (16).
There are multiple mechanisms that post-translationally regulate
transcriptional activity of FOXO3a transcription factors (17). Notably, phospho (p)-AKT regulates
phosphorylation of FOXO3a, which increases translocation of
p-FOXO3a from the nucleus to the cytosol, inhibiting the
transcriptional activity of FOXO3a. In turn, dephosphorylation of
FOXO3a increases its nuclear activity, which enhances target gene
expression (16). However, the
majority of previous studies assessed p-AKT alone without focusing
on its substrates, such as FOXO3a. The activation of FOXO3a may
have an important role in IR injury.
Based on the above reports, it is well established
that mild hypothermia possesses potent anti-apoptosis activity and
inhibits the inflammatory response. The aim of the present study
was to determine whether the use of mild hypothermia pretreatment
protects the liver, reducing ischemia-reperfusion injury.
Furthermore, whether the activation of PI3K/AKT/FOXO3a pathways
contributed to the induction of liver protection in this type of
pretreatment via anti-apoptosis and inhibited the inflammatory
response were investigated.
Materials and methods
Animals
Male Sprague-Dawley rats (n=48; 3 months old; weight
250–280 g) were purchased from Hubei Provincial Center for Disease
Control and Prevention (Wuhan, China), and then housed in the
animal center of Zhongnan Hospital of Wuhan University (Wuhan,
China). Rats were housed at 22±2°C with a 12-h light/dark cycle,
60±5% humidity and given food and water ad libitum. They were
allowed to adapt to the environment for 3 days prior to the
experiment. All the rats were randomly divided into 6 groups, each
group had 8 rats: i) Normal (N) group; ii) mild hypothermic
pretreatment (MH) group; iii) sham (S) group; iv) normothermic
pretreatment + IR (NH + IR) group; v) mild hypothermic pretreatment
+ IR (MH + IR) group; vi) Ly294002 + mild hypothermic pretreatment
+ IR (Ly + MH + IR) group. All animals were fasted 12 h before the
experiment, with free access to water. All experimental procedures
were approved by the Ethics Review Committee of Zhongnan Hospital
of Wuhan University and every effort was taken to minimize pain and
discomfort of rats.
Model for liver IR
The rats in the MH, MH + IR, and Ly + MH + IR groups
were cooled until their rectal temperatures were reduced to
32.2±0.5°C. Mild hypothermia pretreatment was maintained for 2 h by
maintaining the rat with an icebox and a heat lamp. The rectal
temperatures of the rats in the N, S, and N + IR groups were also
maintained at 37±0.5°C for 2 h.
Pre-treatment with PI3K inhibitor (Ly294002; 1.5
mg/kg) and vehicle [10% dimethyl sulfoxide (DMSO) and 90% PBS. was
given intraperitoneally (i.p.) 30 min prior to the mild hypothermic
pretreatment in the Ly + MH + IR group. The other rats in the S, NH
+ IR, and MH + IR groups were injected with an equivalent volume of
vehicle (10% DMSO and 90% PBS).
The rats were anesthetized with chloral hydrate (40
mg/kg, i.p.) during surgery. Then a midline incision was made to
expose the liver and free the perhepatic ligament, injected 100
IU/kg heparin for systemic anti-coagulation through a penile vein.
The artery and portal venous blood supply to the left/middle liver
lobes were blocked with an atraumatic clip for 60 min. The abdomen
was closed temporarily until re-opened, and the clamp was removed
to induce reperfusion. The rectal temperature of the rat was
maintained at 37±0.5°C in the entire surgical procedure. After 6 h
of reperfusion, the rats were reanesthetized and sacrificed to
collect hepatic tissues and blood samples immediately. The sham
group rats underwent the same surgical procedure without vascular
occlusion. The N group and MH group did not receive surgery.
Serum alanine aminotransferase ALT
levels
Serum sALT level, an indicator of hepatocellular
injury, was measured in blood samples using an automated chemical
analyzer.
Liver histology
Ringer (0–4°C, heparinized, 20 ml) was used to flush
the blood from the liver via the abdominal aorta, then fixed in 10%
formalin and embedded in paraffin. Paraffin sections were cut into
5 µm and stained with hematoxylin and eosin (H&E) according to
standard protocols (18). Stained
tissue slices were observed with a bright field microscope by a
pathologist. The severity of liver IR injury was graded blindly
using the criteria of Suzuki et al (19) on a scale from 0–4.
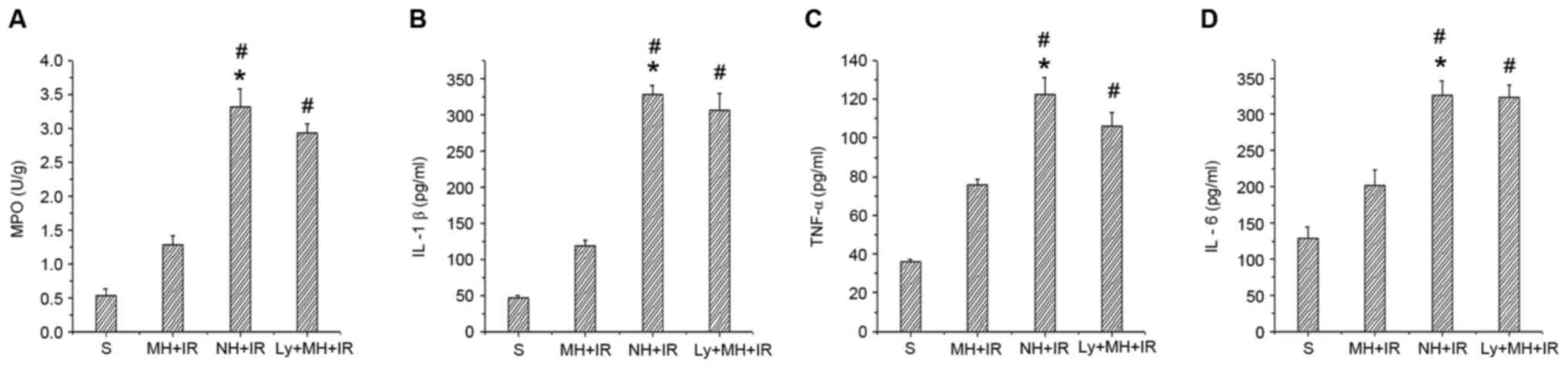
Myeloperoxidase (MPO) assay
The presence of MPO was used as an index of
neutrophil accumulation in the liver and was obtained from Nanjin
Jianchen Biotechnology, (Nanjin, China; http://www.njjcbio.com). MPO activity was measured
according to the manufacturer's protocols.
Serum cytokines
Interleukin-1β (IL-1β) and tumor necrosis factor-α
(TNF-α) and IL-6 were quantified from serum by ELISA and were
obtained from Cloud-Clone Corp. (Katy, TX, USA).
Terminal deoxynucleotidyl transferase
(TdT) dUTP nick-end labelling (TUNEL) detection
Sections were permeabilized in xylene, dehydrated in
graded ethanol series to water, incubation with 3% hydrogen
peroxide for 30 min, then treated with proteinase K (5 mg/ml) for 5
min at room temperature. Subsequently, the sections were applied
with TdT reaction buffer (Roche Diagnostics GmbH, Mannheim,
Germany) for 1 h at 37°C. Following washing in PBS, the sections
were incubated with converter-peroxidase and detected with
diaminobenzidine.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Total RNA was obtained from liver tissue with TRIzol
reagent (Invitrogen; Thermo Fisher Scientific, Inc., Waltham, MA,
USA) according to the manufacturer's protocols, and cDNA for
RT-qPCR was synthesized using oligo d(T) and a Superscript III RT
kit (Thermo Fisher Scientific, Inc.). qPCR was conducted using a
Quantitative SYBR-Green RT-PCR kit (Takara Bio, Inc., Otsu, Japan)
and an Applied Biosystems 7500 system (Thermo Fisher Scientific,
Inc.). All reactions were conducted in a 20 µl reaction volume in
triplicate. The relative expression levels for a target gene were
normalized to β-actin. Specificity was verified by melting curve
analysis and agarose gel electrophoresis. FOXO3a, nuclear factor
(NF)-κB and β-actin were obtained from Wuhan GuGe Biotechnology,
(Wuhan China). Primers were as follows: FOXO3a sense,
5′-AACAGTACCGTGTTCGGACC-3′ and anti-sense,
5′-AGTGTCTGGTTGCCGTAGTG-3′; NF-κB sense,
5′-GCTCCTTTTCTCAAGCCGATGT-3′ and anti-sense,
5′-CGTAGGTCCTTTTGCGTTTTTC-3′; and β-actin sense,
5′-GTTACAGGAAGTCCCTCACCC-3′ and anti-sense,
5′-CAGACCTGGGCCATTCAGAAA-3′. Data were analyzed using the
comparative Cq (2−∆∆Cq) (20).
Western blotting
Total protein was obtained from liver tissue with a
triple detergent RIPA buffer (Solarbio, Wuhan, China) containing a
protease inhibitor cocktail and nuclear protein was obtained from
liver tissue with nuclear and cytoplasmic protein extraction kit
(Beyotime Institute of Biotechnology, Beijing, China) according to
the manufacturer's protocols. Approximately 40 µg of proteins were
separated by 10% SDS-PAGE and transferred onto polyvinylidene
membranes. Membranes were blocked with 5% skimmed milk in PBS at
room temperature for 2 h and then incubated with the corresponding
primary antibodies: p-AKT (ser473; ab81283; 1:1,000), p-FOXO3a
(ser253; ab47285; 1:1,000), FOXO3a (ab109629; 1:1,000), NF-κB
(ab16502; 1:1,000), Bcl-2 associated X apoptosis regulator (Bax;
ab32503; 1:1,000), Bcl-2 apoptosis regulator (Bcl-2; ab59348;
1:1,000; all from Abcam, Cambridge, UK), p-NF-κB inhibitor α (IKBα;
ser32; 2859; 1:1,000; Cellular Technology Ltd., Cleveland, OH, USA)
at 4°C overnight. Membranes were then washed with Tris-buffered
saline-Tween repeatedly and incubated with secondary antibodies
(SE132; 1:3,000; Beijing Solarbio Science and Technology Co., Ltd.,
Beijing, China) at room temperature for 45 min. Enhanced
chemiluminescence (Wuhan Sanying Biotechnology, Wuhan, China) was
used to visualize the immunoreactive bands. Signal intensities of
all protein bands were assessed by the Quantity One software
version 4.62 (Bio-Rad Laboratories, Inc., Hercules, CA, USA).
Anti-rat β-actin (K006153P; 1:3,000; Wuhan GuGe Biotechnology,
Wuhan, China) and TATA-box binding protein (22006–1-AP, 1:3,000;
Wuhan Sanying Biotechnology) were used as internal controls.
Statistical analysis
All data are expressed as the mean ± standard
deviation (n=8/group). Comparison between two groups were performed
using Student's t-test, while the differences among ≥3 groups were
analyzed by one-way analysis of variance for post hoc multiple
comparisons. P<0.05 was considered to indicate a statistically
significant difference.
Results
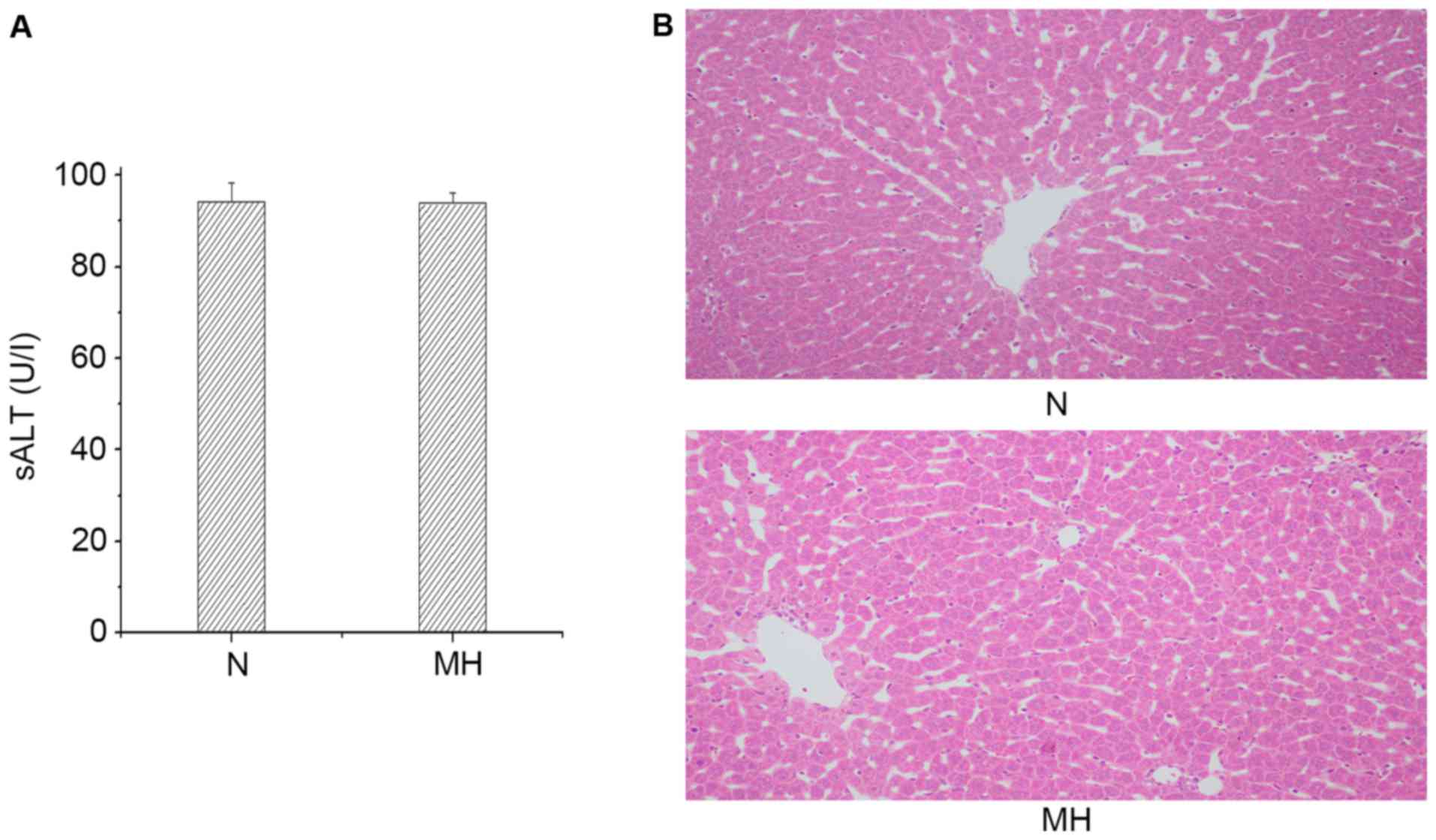
Mild hypothermia pretreatment does not
damage hepatocellular function
The hepatocellular function was analyzed in rat
livers subjected to mild hypothermia pretreatment without any
operation. As presented in Fig.
1A, there was no difference in the sALT level between the N and
MH group (94.23±4.18 vs. 93.85±2.38 IU/l). These data were
supported by H&E staining (Fig.
1B). The MH group and N group did not exhibit sinusoidal
congestion, vacuolization or necrosis. These data indicated that
only giving mild hypothermia pretreatment would not damage
hepatocellular function, thus, the effects of mild hypothermia
pretreatment only were not examined further.
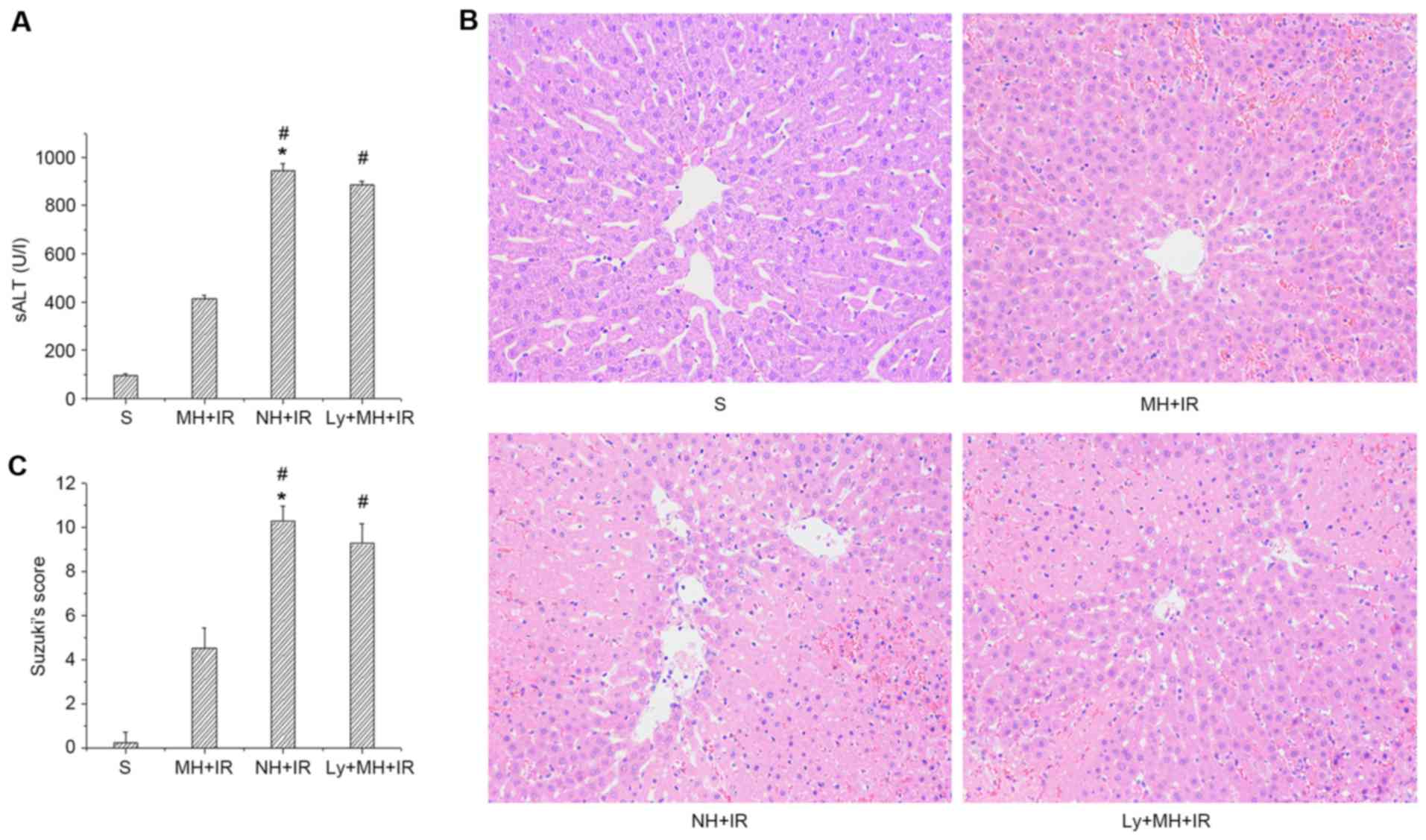
Mild hypothermia pretreatment protects
the liver against IRI
The hepatocellular function was analyzed in rat
livers subjected to 60 min of warm ischemia followed by 6 h
reperfusion. As presented in Fig.
2A, sALT levels in the MH + IR group was decreased compared
with the NH + IR group (414.65±12.74 vs. 943.52±32.3 IU/l). These
data were supported by Suzuki's histological grading of liver IRI
(Fig. 2B and C). Indeed, mild
hypothermia pretreatment resulted in minimal liver sinusoidal
congestion, vacuolization and necrosis (score, 4.5±0.93; Fig. 2B and C). By contrast, untreated
livers (NH + IR) exhibited severe edema and extensive
hepatocellular necrosis (score, 10.25±0.7; Fig. 2B and C). However, the protective
effect of mild hypothermia pretreatment was blocked when rats were
pre-treated with Ly294002 (885.2±14.51 IU/l, Fig. 2A; and score, 9.25±0.89, Fig. 2B and C).
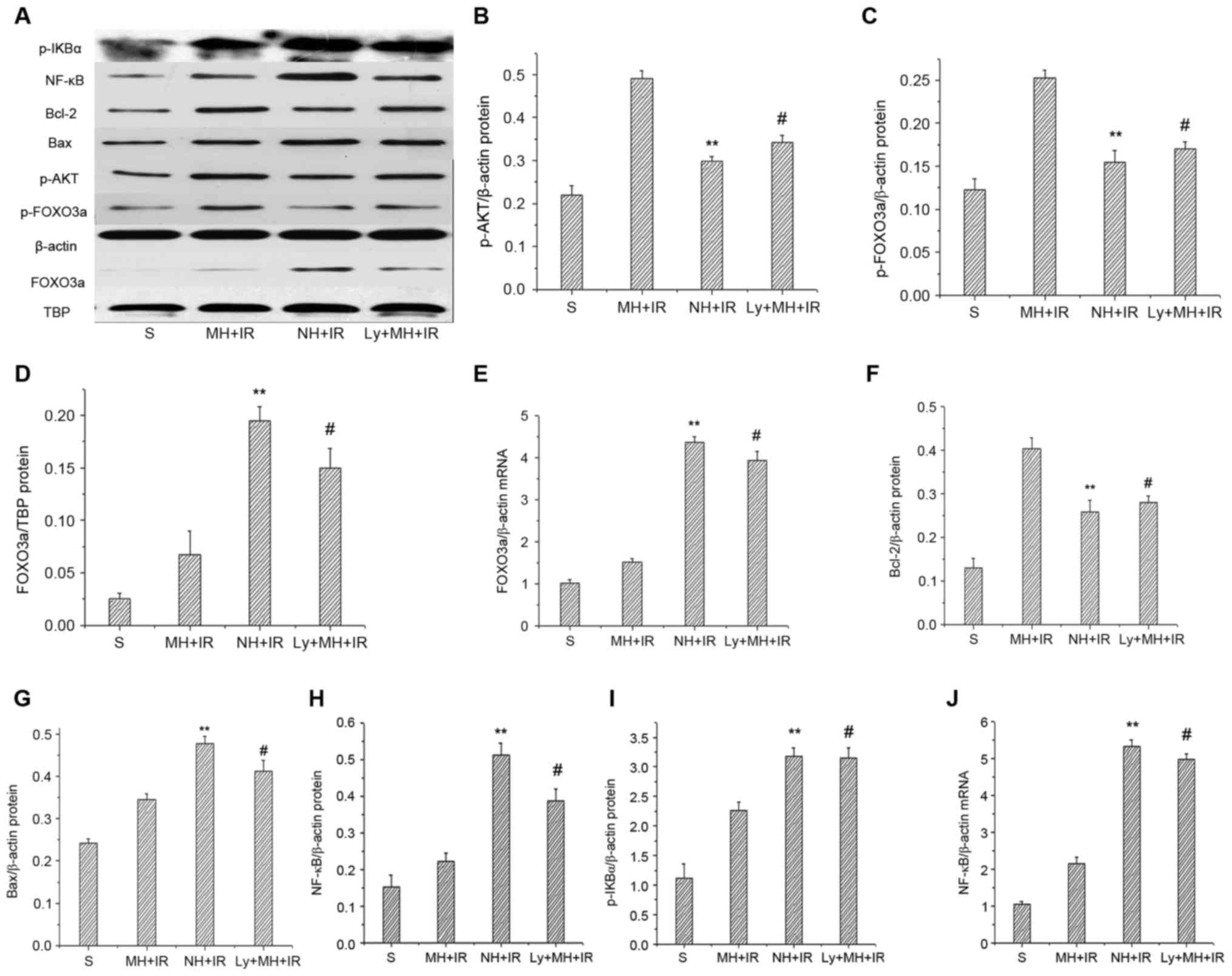
Mild hypothermia pretreatment
activates PI3K/AKT/FOXO3a signaling in liver IRI
To further investigate the role of PI3K/AKT/FOXO3a
signaling in liver IRI protection by mild hypothermia pretreatment,
the expression levels of FOXO3a mRNA and p-AKT, p-FOXO3a and
nuclear FOXO3a protein were determined. When compared with the NH +
IR group and Ly + MH + IR, mild hypothermia pretreatment increased
p-AKT and p-FOXO3a protein (Fig.
3A-C). Notably, the mRNA and nuclear FOXO3a protein expression
were significantly reduced in the MH+IR group compared with the NH
+ IR group and Ly + MH + IR group (Fig. 3A, D and E).
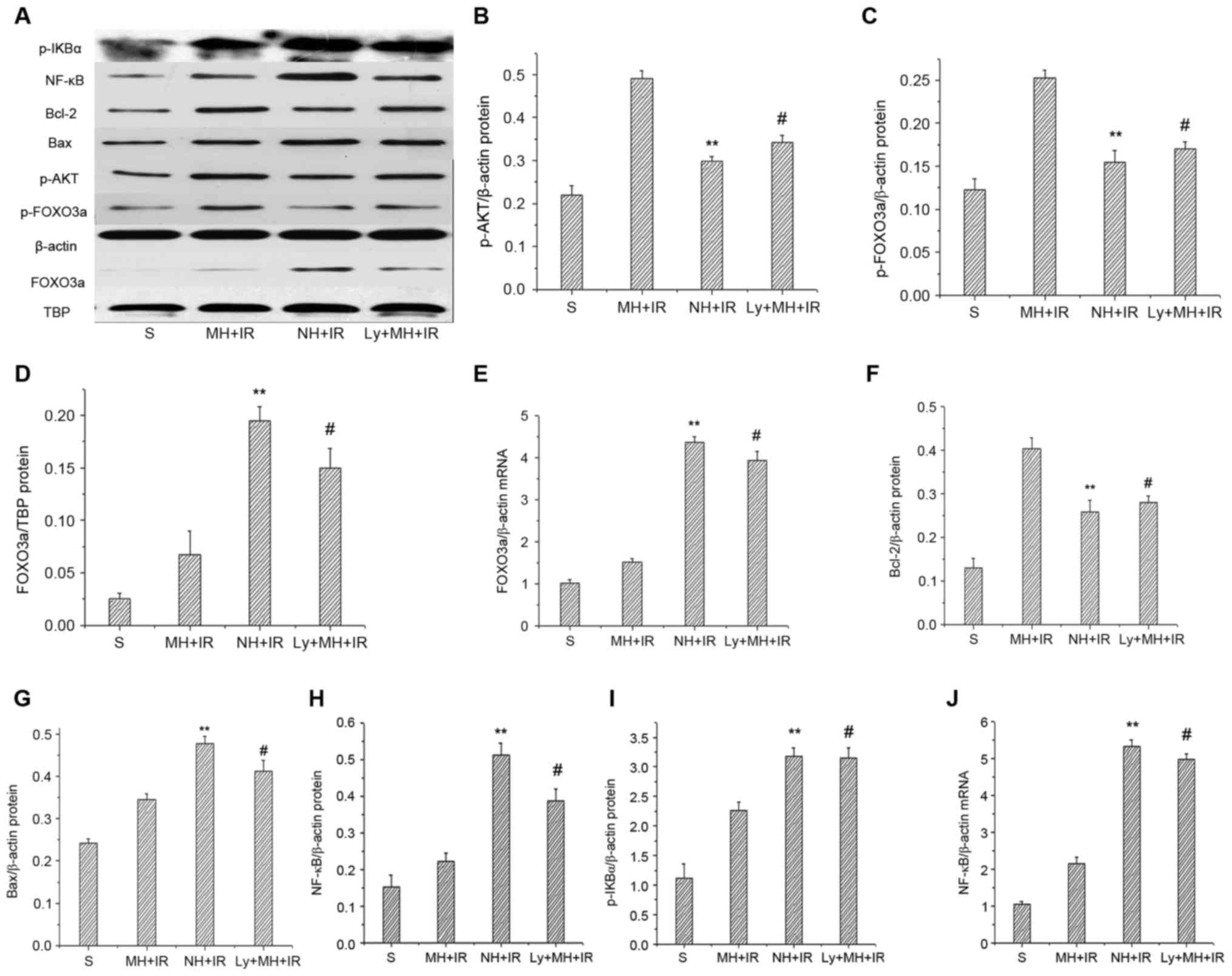 | Figure 3.Mild hypothermia pretreatment
activates phosphatidylinositol-3-kinase/AKT/FOXO3a signaling in
liver IR injury. (A) Western blot analysis of p-AKT, p-FOXO3a,
Bcl-2, Bax, p-IKBα and NF-κB; with β-actin as an internal control.
Western blot analysis of nuclear FOXO3a and TBP served as an
internal control. Band density of (B) p-AKT, (C) p-FOXO3a, (D)
FOXO3a were measured, and p-AKT and p-FOXO3a were normalized to
that of β-actin, FOXO3a was normalized to TBP. (E) RT-qPCR used to
detect mRNA coding for FOXO3a. Data were normalized to β-actin gene
expression. (F) Bcl-2, (G) Bax, (H) NF-κB and (I) p-IKBα were
measured and normalized to that of β-actin. (J) RT-qPCR used to
detect mRNA coding for NF-κB. Data were normalized to β-actin gene
expression. Values are expressed as the mean ± standard deviation
(n=8/group). **P<0.05 NH + IR group vs. MH + IR group,
#P<0.05 Ly + MH + IR group vs. MH + IR group. p-,
phospho; IKBα, NF-κB inhibitor α; Bcl-2, Bcl-2 apoptosis regulator;
Bax, Bcl-2 associated X apoptosis regulator; AKT, protein kinase B;
FOXO3a, forkhead box O 3a; TBP, TATA-box binding protein; S, sham;
MH, mild hypothermia pretreatment; IR, ischemia/reperfusion; NH,
normothermic pretreatment; Ly, Ly294002. |
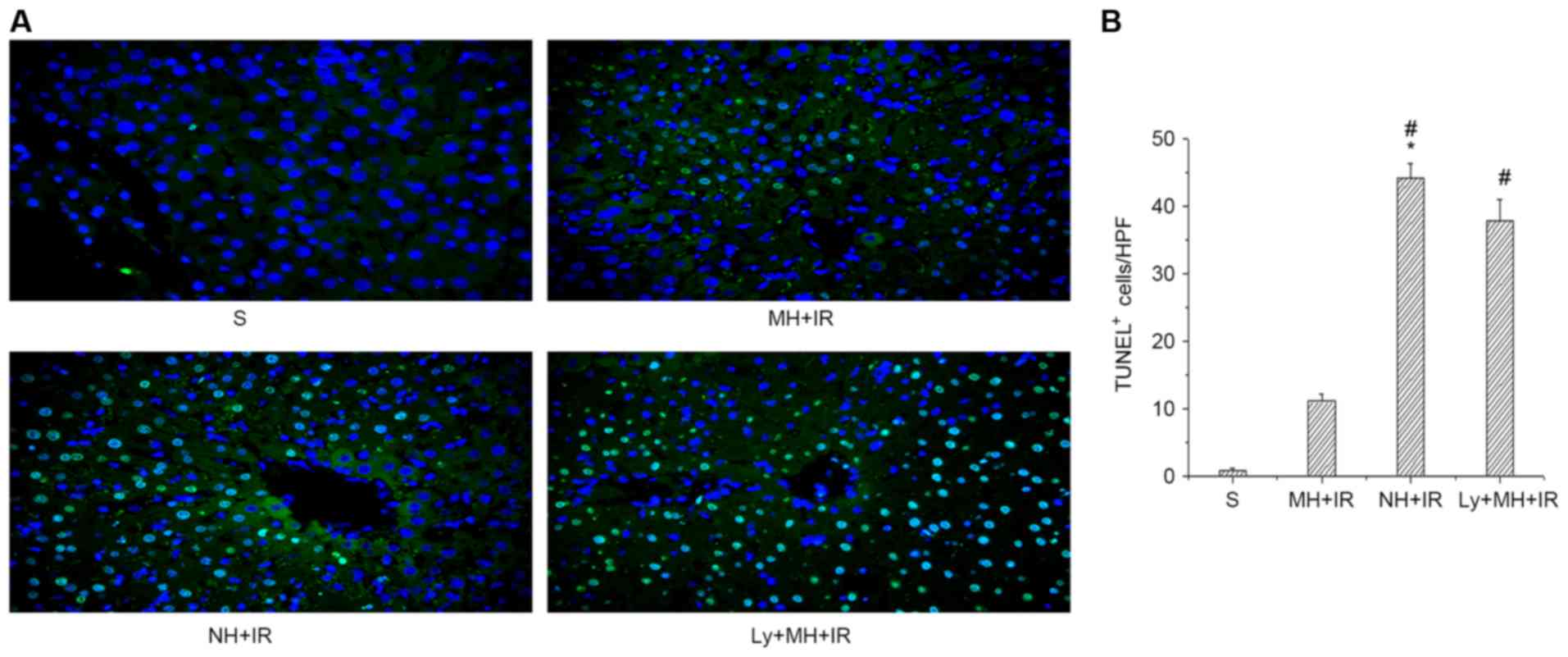
Mild hypothermia pretreatment promotes
anti-apoptotic function and reduces hepatocellular apoptosis in
liver IR injury
In order to study the protective effect of mild
hypothermia pretreatment against cell death induced by IR, the
expression of anti-apoptotic (Bcl-2) and pro-apoptotic (Bax)
proteins was determined. Indeed, the Bcl-2 protein expression was
MH + IR group markedly increased in the ischemic liver compared
with the NH + IR or Ly + MH + IR group (Fig. 3A and F). Furthermore, the
expression of Bax was lower in the MH + IR group compared with the
NH + IR or Ly + MH + IR group (Fig. 3A
and G). Hepatocellular apoptosis was also determined using
TUNEL staining. Mild hypothermia pretreatment decreased the number
of TUNEL-positive cells compared with NH + IR group or Ly + MH + IR
(Fig. 4A and B).
Mild hypothermia pretreatment inhibits
the release of proinflammatory mediators in liver IRI
IR activates a redox sensitive transcription factor
NF-κB and the activation of NF-κB induces the expression of
proinflammatory mediators. Whether mild hypothermia pretreatment
contributed to inhibit this was investigated. As presented in
Fig. 3A and I, when compared with
the NH + IR and Ly + MH + IR groups, mild hypothermia pretreatment
reduced p-IKBα protein, and decreased protein and mRNA expression
of NF-κB (Fig. 3A, H and J). The
MPO assay reflecting liver neutrophil activity (U/g) was reduced in
the MH + IR compared with the NH + IR group or Ly + MH + IR group
(Fig. 5A). Similar changes were
obtained for the effects of mild hypothermia pretreatment on IL-1β,
TNF-α and IL-6 (Fig. 5B-D).
Discussion
Organ damage by IR is associated with high morbidity
and mortality. Accordingly, it is necessary to formulate treatment
strategies for curing this disease. This has initiated numerous
attempts to improve tissue protection against IR injury of the
liver e.g., through ischemic preconditioning, pharmacological
agents, hypothermia and so on. Mild hypothermia has achieved good
results in animal models of brain ischemic injury (21). In addition to improvements in brain
ischemic injury, artificial hypothermia can significantly reduce
ischemic damage of other organs, including the liver, kidney and
myocardium (22,23). Four large-scale prospective
randomized controlled trials reported that mild hypothermia
improved neural function in patients with cardiac arrest caused by
ventricular fibrillation. The majority of previous studies
(8,9,24)
have focused on investigation of therapeutic hypothermia (32–34°C).
However, in selective cases the application of mild hypothermia
pretreatment may outweigh the risks, whereas fewer studies have
been conducted using this method. The current in vivo study
demonstrated that mild hypothermia pretreatment ameliorated liver
IR and improved hepatocellular function, as evidenced by its
ability to reduce sALT levels, histological liver damage,
neutrophil activity and pro-inflammatory cytokine expression. A
specific PI3K inhibitor (Ly294002) blocked the protective effect of
mild hypothermia on liver IR. The present findings demonstrate a
novel molecular protective mechanism of mild hypothermia
pretreatment in rat livers subjected to 60 min warm ischemia and 6
h reperfusion via activation of the PI3K/AKT/FOXO3a signaling
network.
FOXO3a is a member of the family of forkhead
transcription factors, which have emerged to be critical regulators
of gene expression, and to control oxidative stress and apoptosis
in various cell types, and are regulated via phosphorylation by
p-AKT (16). Without growth factor
stimulation, FOXO3a is located in the nucleus and functions as a
transcription factor. Once the PI3K signaling cascade is activated,
FOXO3a is phosphorylated by p-AKT, reducing its DNA-binding
capacity and exports p-FOXO3a from the nucleus to the cytoplasm,
where it is degraded following ubiquitination (25). Previous studies (26,27)
have reported that PI3K/AKT pro-survival signaling is essential in
heart and brain ischemic injury. IR causes inactivation of AKT,
thereby decreasing phosphorylation of FOXO3a. However, once FOXO3a
is phosphorylated, it is translocated into the cytoplasm, which
downregulates the expression of pro-apoptosis molecules, such as
Bax, and upregulates anti-apoptotic protein Bcl-2 (28,29).
The results of the current study demonstrated that IR insult
downregulated the expression of p-AKT, whereas mild hypothermia
pretreatment would block it. When compared with the NH + IR and Ly
+ MH + IR groups, mild hypothermia pretreatment increased p-AKT
protein. The latter phosphorylated FOXO3a increased, resulting in
the reduction of its DNA-binding capacity and export of p-FOXO3a
from the nucleus to the cytoplasm, and decreased nucleus FOXO3a
protein and mRNA, subsequently the expression of anti-apoptotic
Bcl-2 was increased and pro-apoptotic Bax protein was deceased.
There data was further confirmed by a TUNEL assay, which
demonstrated that the number of apoptotic cells was increased in
the NH + IR group compared with the MH+IR group ischemic liver
samples. By contrast, ablation of PI3K/AKT signaling with Ly294002
depressed p-AKT, p-FOXO3a and Bcl-2; yet enhanced nuclear FOXO3a
and Bax, and the number of apoptotic cells compared with the MH +
IR group. Thus, mild hypothermia pretreatment-mediated
PI3K/AKT/FOXO3a signaling is essential to protect hepatocytes
against IR-induced apoptotic.
FOXO3a signaling is known to induce proinflammatory
cytokine gene expression, and it can regulate innate immune
functions in respiratory epithelial cells (30). It is possible that mild hypothermia
pretreatment attenuated inflammation response following IR injury
via PI3K/AKT/FOXO3a signaling. Initially, liver IR triggers
macrophage activation and neutrophil recruitment leading to aseptic
inflammation (31). MPO assay is a
measure of liver neutrophil activity. The results of the present
study demonstrated that liver IR injury leads to increased MPO
activity, whereas mild hypothermia pretreatment suppress MPO
activity. However, blocking the effects of mild hypothermia with
Ly294002 reversed the process. NF-κB is a ubiquitous inducible
transcription factor, which induces target gene expression and
promotes inflammatory responses (32). Numerous studies (33,34)
have reported strong evidence that NF-κB has a crucial role in
tissue inflammatory responses during the pathogenesis of IR. NF-κB
knockout mice developed less ischemia damage following permanent
focal insult (35). Increasing
FOXO transcriptional activity enhances TNF-α and IL-1β production,
whereas activation of NF-κB increases FOXO binding to the TNF-α and
IL-1β promoters, indicating NF-κB regulation of FOXO-mediated
regulation of proinflammatory cytokines (36). In the current study, mild
hypothermia pretreatment inhibited FOXO3a transcriptional activity,
and ischemia resulted in increased p-IKBα, which reduced the level
of NF-κB and thus blocked activation of the NF-κB pathway that may
attenuate inflammation though the regulation of proinflammatory
cytokines (such as TNF-α, IL-1β and IL-6). Furthermore, blocking
PI3K/AKT with Ly294002 led to increased NF-κB transcription and
TNF-α, IL-1β and IL-6 release, with similar results to the NH + IR
group. The results demonstrated that inactivation of FOXO3a by mild
hypothermia pretreatment can attenuate inflammation by regulation
NF-κB activation and proinflammatory cytokine release.
In conclusion, the present study provided evidence
that in vivo mild hypothermia pretreatment provides an
efficient tool to protect the liver by inhibiting the degree of
apoptosis and inflammation injury in the IR, leading to improved
hepatic function, which may be due to activation of the
PI3K/AKT/FOXO3a pathway. The study provides a rationale for novel
therapeutic approaches for the management of hepatic injury
triggered by IR. However, further studies are necessary to
investigate the long-term effect of mild hypothermia pretreatment
in liver IR injury. Subsequent clinical research needs to validate
this conclusion.
Acknowledgements
This study was supported by National Natural Science
Foundation of China (grant no. U1403222).
References
|
1
|
Selzner N, Rudiger H, Graf R and Clavien
PA: Protective strategies against ischemic injury of the liver.
Gastroenterology. 125:917–936. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Eltzschig HK and Eckle T: Ischemia and
reperfusion-from mechanism to translation. Nat Med. 17:1391–1401.
2011. View
Article : Google Scholar : PubMed/NCBI
|
|
3
|
Duarte S, Hamada T, Kuriyama N, Busuttil
RW and Coito AJ: TIMP-1 deficiency leads to lethal partial hepatic
ischemia and reperfusion injury. Hepatology. 56:1074–1085. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jaeschke H and Woolbright BL: Current
strategies to minimize hepatic ischemia-reperfusion injury by
tageting reactive oxygen species. Transplant Rev (Orlando).
26:103–114. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bigelow WG, Callaghan JC and Hopps JA:
General hypothermia for experimental intracardiac surgery. Ann
Surg. 132:531–537. 1950. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Miao YF, Wu H, Yang SF, Dai J, Qiu YM, Tao
ZY and Zhang XH: 5′-adenosine monophosphate-induced hypothermia
attenuates brain ischemia/reperfusion injury in a rat model by
inhibiting the inflammatory response. Mediators Inflamm.
2015:5207452015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kida K, Shirozu K, Yu B, Mandeville JB,
Bloch KD and Ichinose F: Beneficial effects of nitric oxide on
outcomes after cardiac arrest and cardiopulmonary resuscitation in
hypothermia-treated mice. Anesthesiology. 120:880–889. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Behrends M, Hirose R, Serkova NJ, Coatney
JL, Bedolli M, Yardi J, Park YH and Niemann CU: Mild hypothermia
reduces the inflammatory response and hepatic ischemia/reperfusion
injury in rats. Liver Int. 26:734–741. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Niemann CU, Choi S, Behrends M, Hirose R,
Noh J, Coatney JL, Roberts JP, Serkova NJ and Maher JJ: Mild
hypothermia protects obese rats from fulminant hepatic necrosis
induced by ischemia-reperfusion. Surgery. 140:404–412. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhang R, Zhang L, Manaenko A, Ye Z, Liu W
and Sun X: Helium preconditioning protects mouse liver against
ischemia and reperfusion injury through the PI3K/Akt pathway. J
Hepatol. 61:1048–1055. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Suo L, Kang K, Wang X, Cao Y, Zhao H, Sun
X, Tong L and Zhang F: Carvacrol alleviates ischemia reperfusion
injury by regulating the PI3K-Akt pathway in rats. PLoS One.
9:e1040432014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Uranga RM, Katz S and Salvador GA:
Enhanced phosphatidylinositol 3-kinase (PI3K)/Akt signaling has
pleiotropic targets in hippocampal neurons exposed to iron-induced
oxidative stress. J Biol Chem. 288:19773–19784. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Brunet A, Bonni A, Zigmond MJ, Lin MZ, Juo
P, Hu LS, Anderson MJ, Arden KC, Blenis J and Greenberg ME: AKT
promotes cells survival by phosphorylating and inhibiting a
forkhead transcription factor. Cell. 96:857–868. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lin K, Dorman JB, Rodan A and Kenyon C:
daf-16: An HNF-3/forkhead family member that can function to double
the life-span of Caenorhabditis elegans. Science. 278:1319–1322.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Furuyama T, Nakazawa T, Nakano I and Mori
N: Identification of the differential distribution patterns of
mRNAs and consensus binding sequences for mouse DAF-16 homologues.
Biochem J. 349:629–634. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Essers MA, de Vries-Smits LM, Barker N,
Polderman PE, Burgering BM and Korswagen HC: Functional interaction
between beta-catenin and FOXO in oxidative stress signaling.
Science. 308:1181–1184. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tzivion G, Dobson M and Ramakrishnan G:
FoxO transcription factors; Regulation by AKT and 14-3-3 proteins.
Biochim Biophys Acta. 1813:1938–1945. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Fischer AH, Jacobson KA, Rose J and Zeller
R: Hematoxylin and eosin staining of tissue and cell sections. CSH
Protoc. 2008:pdb.prot49862008.PubMed/NCBI
|
|
19
|
Suzuki S, Toledo-Pereyra LH, Rodriguez FJ
and Cejalvo D: Neutriphil infiltration as an important factor in
liver ishcemia and reperfusion injury. Modulating effects of FK506
and cyclosporine. Transplantation. 55:1265–1272. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Tang Y, Liu X, Zhao J, Tan X, Liu B, Zhang
G, Sun L, Han D, Chen H and Wang M: Hypothermia-induced ischemic
tolerance is associated with Drp1 inhibition in cerebral
ischemia-reperfusion injury of mice. Brain Res. 1646:73–83. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Niemann CU, Xu F, Choi S, Behrends M, Park
Y, Hirose R and Maher JJ: Short passive cooling protects rats
during hepatectomy by inducing heat shock proteins and limiting the
induction of pro-inflammatory cytokines. J Surg Res. 158:43–52.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Niemann CU, Feiner J, Swain S, Bunting S,
Friedman M, Crutchfield M, Broglio K, Hirose R, Roberts JP and
Malinoski D: Therapeutic hypothermia in deceased organ donors and
kidney-graft function. New Engl J Med. 373:405–414. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bernard SA, Gray TW, Buist MD, Jones BM,
Silvester W, Gutteridge G and Smith K: Treatment of comatose
survivors of out-of-hospital cardiac arrest with induced
hypothermia. New Engl J Med. 346:557–563. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ma J, Ding Y, Fang X, Wang R and Sun Z:
Protein kinase C-θ inhibits inducible regulatory T cell
differentiation via an AKT-Foxo1/3a-dependent pathway. J Immunol.
188:5337–5347. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Pei YH, Chen J, Xie L, Cai XM, Yang RH,
Wang X and Gong JB: Hydroxytyrosol protects against myocardial
ischemia/reperfusion injury through a PI3K/Akt-dependent mechanism.
Mediators Inflamm. 2016:12321032016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chen L, Wei X, Hou Y, Liu X, Li S, Sun B,
Liu X and Liu H: Tetramethylpyrazine analogue CXC195 protects
against cerebral ischemia/reperfusion-induced apoptosis through
PI3K/Akt/GSK3β pathway in rats. Neurochem Int. 66:27–32. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Huang C, Gu H, Zhang W, Herrmann JL and
Wang M: Testosterone-down-regulated Akt pathway during cardiac
ischemia/reperfusion: A mechanism involving BAD, Bcl-2 and FOXO3a.
J Surg Res. 164:e1–e11. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Luedde T, Kaplowitz N and Schwabe RF: Cell
death and cell death responses in liver disease: Mechanisms and
clinical relevance. Gastroenterology. 147:765–783.e4. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Seiler F, Hellberg J, Lepper PM,
Kamyschnikow A, Herr C, Bischoff M, Langer F, Schäfers HJ, Lammert
F, Menger MD, et al: FOXO transcription factors regulate innate
immune mechanisms in respiratory epithelial cells. J Immunol.
190:1603–1613. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Zhai Y, Busuttil RW and Kupiec-Weglinski
JW: Liver ischemia and reperfusion injury: New insights into
mechanisms of innate adaptive immune-mediated tissue inflammation.
Am J Transplant. 11:1563–1569. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Li Q and Verma IM: NF-kappaB regulation in
the immune system. Nat Rev Immunol. 2:725–734. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Yang JC, Lin MW, Rau CS, Jeng SF, Lu TH,
Wu YC, Chen YC, Tzeng SL, Wu CJ and Hsieh CH: Altered exosomal
protein expression in the serum of NF-κB knockout mice following
skeletal muscle ischemia-reperfusion injury. J Biomed Sci.
22:402015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Rao J, Qian X, Li G, Pan X, Zhang C, Zhang
F, Zhai Y, Wang X and Lu L: ATF3-mediated NRF2/HO-1 signaling
regulates TLR4 innate immune responses in mouse liver
ischemia/reperfusion injury. Am J Transplant. 15:76–87. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Nurmi A, Lindsberg PJ, Koistinaho M, Zhang
W, Juettler E, Karjalainen-Lindsberg ML, Weih F, Frank N,
Schwaninger M and Koistinaho J: Nuclear factor-kappaB contributes
to infarction after permanent focal ischemia. Stroke. 35:987–991.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Su D, Coudriet GM, Kim D Hyun, Lu Y,
Perdomo G, Qu S, Slusher S, Tse HM, Piganelli J, Giannoukakis N, et
al: FoxO1 links insulin resistance to proinflammatory cytokine
IL-1beta production in macrophages. Diabetes. 58:2624–2633. 2009.
View Article : Google Scholar : PubMed/NCBI
|