Introduction
Ovarian cancer exhibits high rates of mortality
compared with other gynecological malignances (1). Investigations into the pathogenesis
of ovarian cancer have reported that diagnosis occurs within the
later stages of pathogenesis, which has been associated with lower
overall survival rates (2,3). Previous studies have reported that
ovarian cancer metastasizes throughout the peritoneal cavity and
numerous organs may be affected during the pathogenesis of ovarian
cancer (4,5). At present, the incidence rate of
ovarian cancer is increasing; omental metastases have been observed
in 80% of patients with severe ovarian cancer (6). Without effective treatment, cases of
ovarian cancer may progress to mortality. Therefore, effective
treatment may improve the prognosis of ovarian cancer (7,8).
Paclitaxel (PTX) is a tricyclic diterpene compound
that may be delivered from poly-(DL-lactic-co-glycolic) acid or
pegylated liposomal (PL) foams for controlled release in
postoperative chemotherapy against glioblastoma multiforme
(9). PTX exhibits anticancer
properties in patients with epithelial ovarian cancer (10). In addition, PTX reveals therapeutic
effects in the treatment of human cancers, including ovarian,
breast, lung, colorectal, melanoma, head and neck cancer, lymphoma
and brain tumors (11–13). Furthermore, antiangiogenic therapy
vs. dose-dense PTX therapy for the frontline treatment of
epithelial ovarian cancer has been reviewed in phase III randomized
clinical trials (14). Notably,
the development and evaluation of the novel tocopheryl methoxy poly
(ethylene glycol)-block-(lactic-co-glycolic acid) copolymer
nanoparticles significantly enhance the therapeutic effects of PTX
for the treatment of ovarian cancer (15).
In the present study, the efficacy of PL-PTX was
investigated within ovarian cancer cells and a tumor-bearing mouse
model. Treatment with PL-PTX inhibited the growth and
aggressiveness of ovarian cancer cells, and significantly induced
ovarian cancer cell apoptosis in vitro and in vivo.
Additionally, the apoptotic signaling pathways mediated by PL-PTX
within ovarian cancer cells were investigated.
Materials and methods
Ethics statement
The present study was conducted with the
recommendations in the guide for the Care and Use of Laboratory
Animals and was approved by the ethics committee of The Second
Hospital of Tianjin Medical University, Tianjin, China (approval
no. 20151105DGB). All animal protocols were conducted and
maintained in accordance with the National Institutes of Health and
approved by the ethics committee of Animal Experiments Defence
Research of the Second Hospital of Tianjin Medical University
(Tianjin, China; Approval validity: Oct 2015 to Oct 2017).
Cell culture
CAOV-3 cells were obtained from the American Type
Culture Collection (Manassas, VA, USA). All cells were cultured in
Dulbecco's modified Eagle's medium (Thermo Fisher Scientific, Inc.,
Waltham, MA, USA) supplemented with 10% fetal bovine serum (Thermo
Fisher Scientific, Inc.). All cells were cultured in a 37°C
humidified atmosphere containing 5% CO2.
MTT assay
CAOV-3 cells (1×103 cells/well) were
incubated with PTX (5, 10 and 15 mg/ml) or PL-PTX (5, 10 and 15
mg/ml) in 96-well plates for 24, 48 and 72 h at 37°C in triplicate
for each condition, with PBS serving as a control. Following
incubation, 20 µl MTT (5 mg/ml) in PBS was added to each well and
the plate was further incubated for 4 h. The majority of the medium
was removed and 100 µl dimethyl sulfoxide was added into the wells
to solubilize the crystals. Optical density was measured with an
ELISA reader (Bio-Rad Laboratories, Inc., Hercules, CA, USA) at a
wavelength of 570 nm.
Cells invasion and migration
assays
CAOV-3 cells (1×105 cells/well) were
cultured at 37°C in an environment containing 5% CO2
until 90% confluence was attained. CAOV-3 cells were then incubated
with PTX (10 mg/ml), PL-PTX (10 mg/ml) or extracellular
signal-regulated kinase (ERK) inhibitor (cat. no. ab142271; Abcam,
Cambridge, UK) treatment for 48 h at 37°C. For the invasion assay,
1×105 CAOV-3 cells were suspended in 500 µl serum-free
RPMI (Thermo Fisher Scientific, Inc.) and 500 µl RPMI with 5% FBS
(Thermo Fisher Scientific, Inc.) was ploaced in the lower chamber
for 48 h at 37°C. The cells were plated in the upper chambers of BD
BioCoat Matrigel Invasion Chambers (BD Biosciences, Franklin Lakes,
NJ, USA) according to the manufacturer's protocol. Cotton swabs
were used to remove cells and to plate cells. To investigate
migration, CAOV-3 cells (1×106) were cultured in RPMI
medium in the upper chamber and RPMI medium with 5% FBS (Thermo
Fisher Scientific, Inc.) in the lower chamber. Cells were then
plated in a control insert chamber (BD Biosciences) for 48 h at
37°C. Cells were stained using 0.1% crystal violet dye
(Sigma-Aldrich; Merck KGaA) for 30 min at 37°C. Tumor cell
migration and invasion were observed in ≥3 randomly-selected
stained-fields per membrane under a light microscope (BX51; Olympus
Corporation, Tokyo, Japan).
Western blot analysis
CAOV-3 cells were then incubated with PTX (10
mg/ml), PL-PTX (10 mg/ml) or ERK inhibitor (cat. no. ab142271;
Abcam) for 48 h at 37°C. Cells were collected and lysed in
radioimmunoprecipitation assay buffer (M-PER reagent for cells and
T-PER reagent for tissues; Thermo Fisher Scientific, Inc.) followed
by homogenization at 4°C for 10 min. Protein concentration was
measured with a bicinchoninic acid protein assay kit (Thermo Fisher
Scientific, Inc.). A total of 20 µg protein was electrophoresed via
12.5% SDS-PAGE and subsequently transferred to nitrocellulose
membranes. Prior to incubation with primary antibodies at 4°C
overnight, membranes were incubated with blocking buffer (5% milk)
for 2 h at 37°C. The primary antibodies used were against:
Caspase-9 (1:1,200; ab32539), ERK (1:1,000; ab54230) and
phosphorylayed (p)ERK 1/2 (phospho-Thr202/Tyr204; 1:1,000;
ab214362), caspase-3 (1:1,200; ab2171), protein kinase B (AKT;
1:1,000; ab8805), p-AKT (phosphor-S473; 1:1,000; ab8932) and
β-actin (1:500; ab8226; all Abcam) for 12 h at 4°C. Horseradish
peroxidase-conjugated anti-rabbit immunoglobulin G (IgG; Bio-Rad
Laboratories, Inc.) was applied to membranes at a 1:5,000 dilution
for 2 h at 37°C and detected using an enhanced chemiluminescence
substrate ECL Select™ (Roche Diagnostics, Basel, Switzerland). The
density of the protein bands was analyzed by Quantity One software
version 4.62 (Bio-Rad Laboratories, Inc.).
Apoptosis assay
CAOV-3 cells (5×106) were then incubated
with PTX (10 mg/ml), PL-PTX (10 mg/ml) or and or ERK inhibitor
(ERKIR; IR7936) and/or anti-TNFα (1:1,000; cat. no. ab6671; 2
mg/ml; both Abcam) treatment for 48 h at 37°C. Following
trypsinization, cells were washed in cold PBS and adjusted to
1×106 cells/ml using PBS 3 times at room temperature;
CAOV-3 cells were labeled with Annexin V-fluorescein isothiocyanate
(V-FITC) and propidium iodide (Annexin V-FITC kit, BD Biosciences)
for 2 h at 37°C, according to the manufacturer's protocol, and
analyzed with a FACScan flow cytometer (BD Biosciences) using BD
FACSChorus™ intuitively designed software version 1.2 (BD
Biosciences).
Animal studies
Specific pathogen-free male Balb/c mice (n=90; 8
weeks old; 32–35 g body weight) were purchased from the Shanghai
Laboratory Animal Center Co., Ltd. (Shanghai, China). All mice were
housed separately and maintained in a 12 h light/dark cycle with
23±1°C with a relative and humidity of 50±5%. All mice had free
access to food and water. Nude mice were subcutaneously injected
with CAOV-3 cells (1×105) into the right forelimb under
aseptic conditions. All mice were housed in a
temperature-controlled facility at 23±1°C with free access to food
and water. Mice were randomly divided into three groups (n=30 per
group) and received a treatment of 10 mg/kg PTX, 10 mg/kg PL-PTX or
PBS by intravenous injection. Treatments were initiated on day 3
following tumor implantation (diameter: 5–6 mm) and continued 10
times daily for a total of 20 days. Tumor volumes were calculated
once every 3 days according to the formula: V=0.5xa2xb,
where a: Short diameter and b: Long diameter of tumor as measured
with a Vernier caliper.
Immunohistochemistry
Tumors from xenograft mice, extracted as previously
described (16), were fixed by
using 10% formaldehyde for 4 h at 37°C and embedded in paraffin
(4-µm thick sections). Antigen retrieval was performed using a
microwave to heat the sections (standard microwave settings; 20s)
and graded series of ethanol, followed by blocking of endogenous
peroxidase activity with 3% hydrogen peroxide for 10 min at room
temperature. Tumor sections were incubated with 5% BSA
(Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) for 2 h at 37°C and
then incubated with rabbit anti-mouse primary antibodies caspase-9
(1:1,200; ab32539) or caspase-3 (1:1,200; ab2171; both Abcam) for
12 h at 4°C. Tumor tissues were washed with PBS three times and
incubated with biotinylated secondary antibodies anti-rabbit IgG
(1:2,000; Pierce; Thermo Fisher Scientific, Inc.) for 2 h at 37°C.
Biotin-peroxidase signals were detected using 0.5 mg/ml
3′3′-diaminobenzidine (DAB)/0.003% H2O2
(Dako; Agilent Technologies, Inc. Santa Clara, CA, USA) as a
substrate. Results were recorded using a laser confocal microscope
(BX51; Olympus Corporation).
Terminal deoxynucleotidyl
transferase-mediated dUTP nick end labeling (TUNEL) assay
Apoptotic cells (5×106) of tumor
specimens were fixed using 4% formaldehyd for 30 min at 37°C and
analyzed using a TUNEL assay (DeadEnd™ Colorimetric TUNEL System;
Promega Corporation, Madison, WI, USA) according to the
manufacturer's protocol. Tumor sections were incubated with the
reaction mixture (terminal deoxynucleotidyl transferase,
equilibration buffer and biotinylated nucleotide mix) for 1 h at
37°C. Subsequently, streptavidin- and DAB-bound biotin was
quantified and counterstained with hemalum (1%; Merck KGaA,
Darmstadt, Germany) and aquatex (Merck KGaA) for 1 h at 37°C. Tumor
sections were washed with PBS three times for 5 min at room
temperature. DNA fragmentation was analyzed in 3 randomly selected
fields of 4-µm tumor sections using light microscope
(magnification, ×40).
Statistical analysis
Each experiment was performed at least three times.
All data are expressed as the mean ± standard deviation of
triplicate dependent experiments and analyzed by using one-way
analysis of variance followed by a Tukey test. All data were
analyzed using SPSS software, version 19.0 (IBM Corp. Armonk, NY,
USA), GraphPad Prism 5.0 (GraphPad Software, Inc., La Jolla, CA,
USA) and Microsoft Excel (Microsoft Corporation, Redmond, WA USA).
P<0.05 and was considered to indicate a statistically
significant difference.
Results
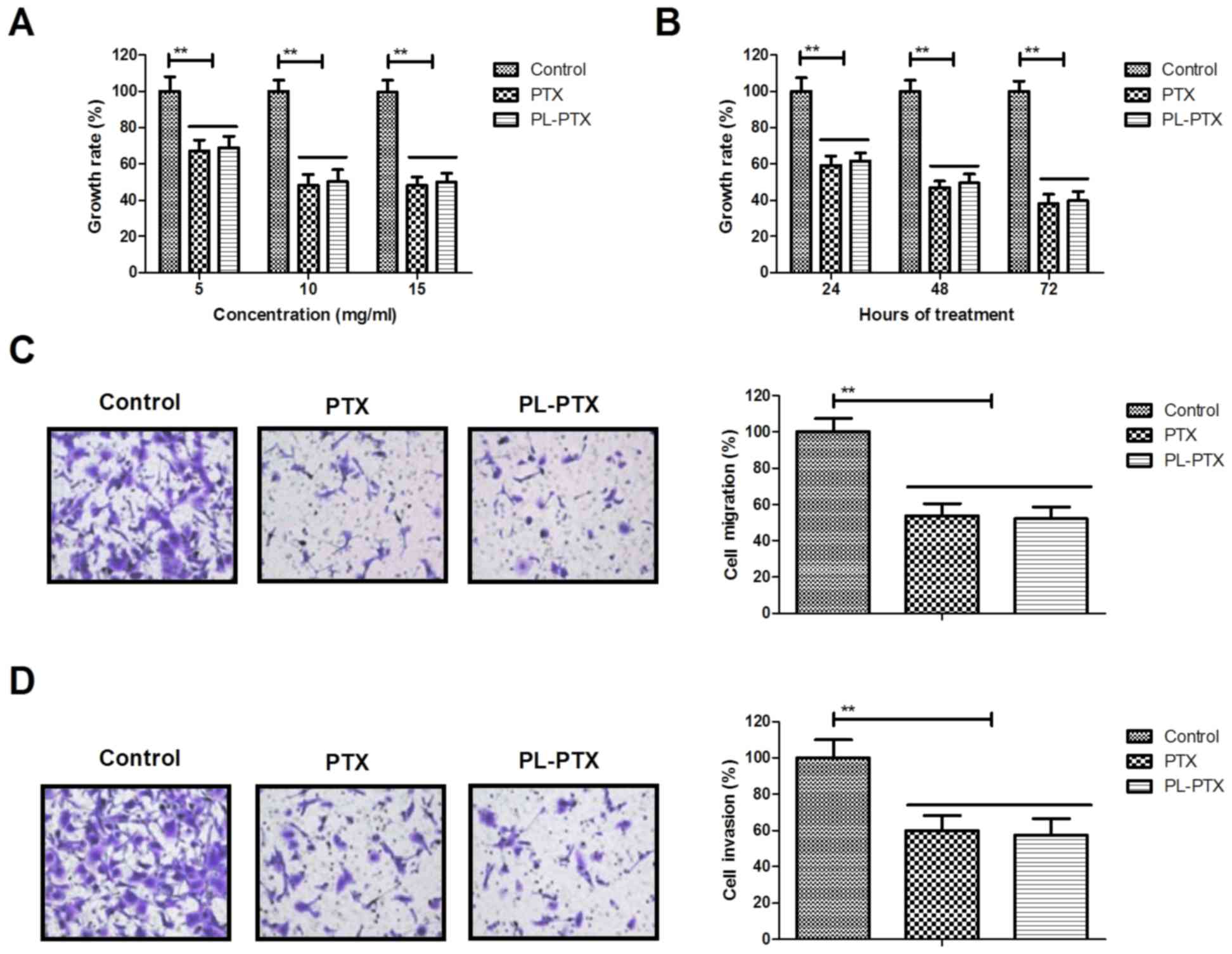
PL-PTX treatment inhibits the growth
and aggressiveness of ovarian cancer cells
The inhibitory effects of PL-PTX on the growth and
aggressiveness of ovarian cancer cells were studied in
vitro. PL-PTX and PTX treatment significantly inhibited ovarian
cancer cell growth (Fig. 1A). In
addition, PL-PTX and PTX inhibited growth of ovarian cancer cells
in time-dependent manner (Fig.
1B). Treatments of 10 mg/ml PL-PTX or PTX significantly
inhibited migration and invasiveness of ovarian cancer cells
(Fig. 1C and D). The results of
the present study indicated that PL-PTX significantly inhibited the
growth and aggressiveness of ovarian cancer cells.
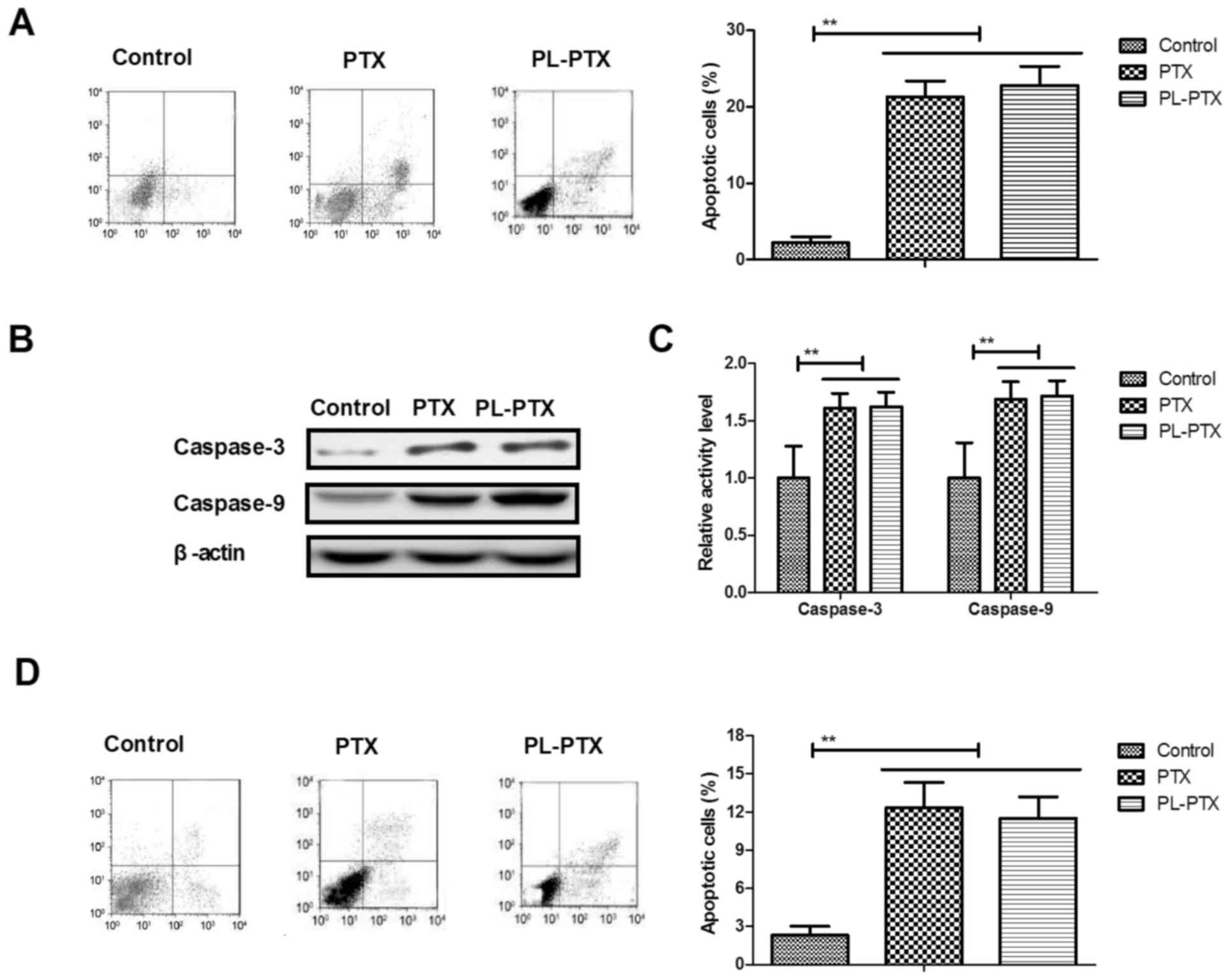
PL-PTX promotes apoptosis of ovarian
cancer cells via the caspase-dependent signaling pathway
As presented in Fig.
2A, the apoptotic ability of CAOV-3 cells was promoted by
PL-PTX. Significantly increased caspase-3 and caspase-9 activities
were detected within PL-PTX-treated CAOV-3 cells (Fig. 2B). PL-PTX treatment increased
caspase-3 and caspase-9 protein expression levels in CAOV-3 cells
(Fig. 2C). These results
demonstrated that PTX- and PL-PTX induced apoptosis of CAOV-3 cells
(Fig. 2D). The results of the
present study suggested that PL-PTX promoted ovarian cancer cell
apoptosis via the caspase-dependent signaling pathway.
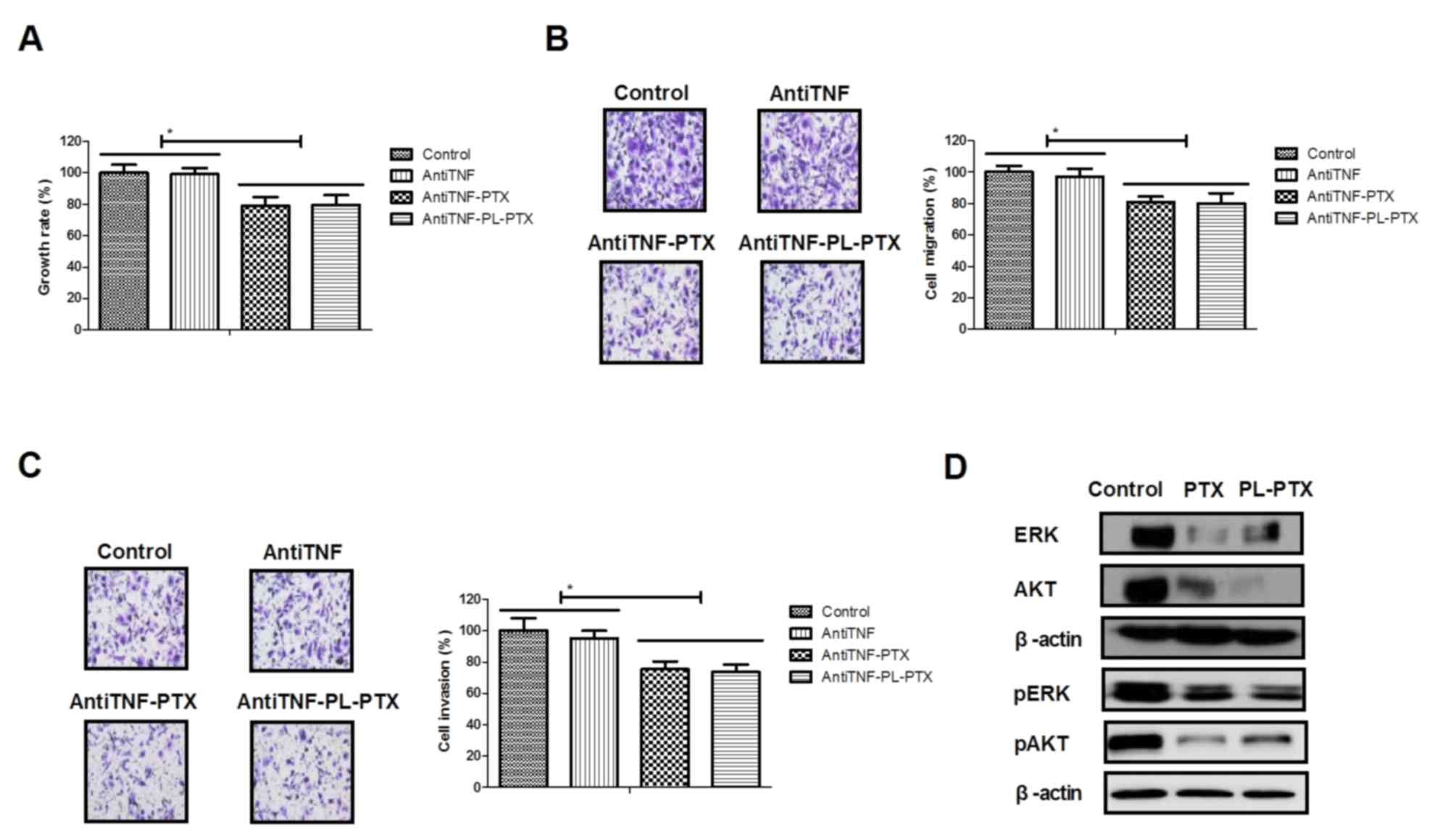
PL-PTX is associated with ovarian
cancer cell apoptosis via tumor necrosis factor (TNF)-induced the
ERK/AKT signaling pathway
TNF has been reported to promote tumor cell
apoptosis (17,18); the effects of TNF on PL-PTX-induced
apoptosis were investigated in the present study. Employment of
AntiTNF, an anti-TNF neutralizing antibody, partially reduced PTX-
and PL-PTX-inhibited growth and aggressiveness of CAOV-3 cells
(Fig. 3A-C). The results of the
present study demonstrated that PL-PTX treatment led to a reduction
in ERK and AKT expression and phosphorylation levels; however,
anti-TNF inhibited the effects exhibited by PL-PTX (Fig. 3D and E). Additionally, inhibition
of the TNF significantly reduced PTX- and PL-PTX-induced CAOV-3
cell apoptosis (Fig. 3F). These
results suggested that PL-PTX may be associated with ovarian cancer
metastasis, which is mediated by the TNF-induced inhibition of the
ERK/AKT signaling pathway.
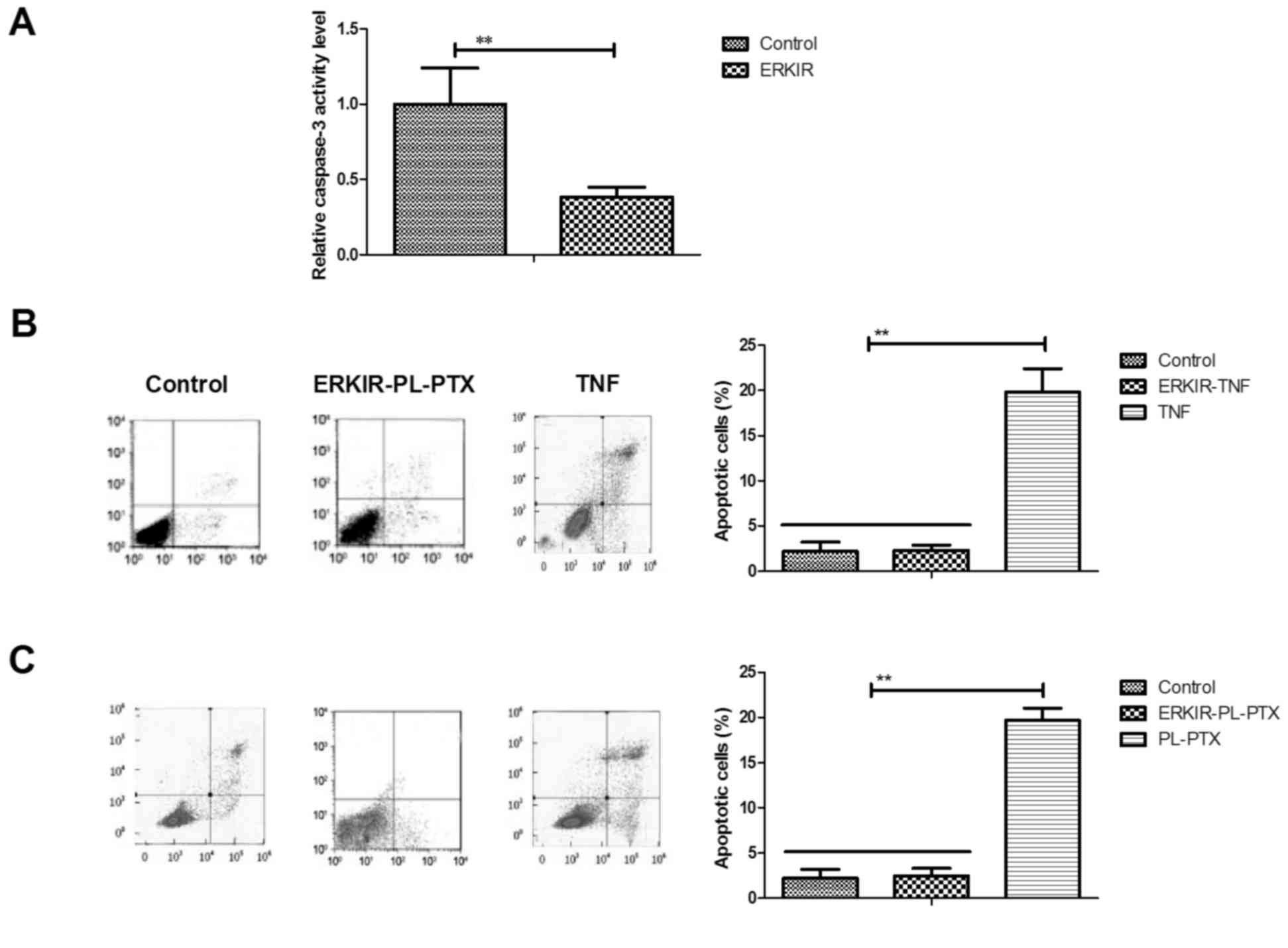
ERK/AKT signaling pathway is involved
in the activation of the TNF/caspase-3 cascade within ovarian
cancer cells
Associations between ERK/AKT and the caspase-3
cascade within CAOV-3 cells were analyzed in the present study. The
inhibition of ERK/AKT activity using ERKIR decreased the expression
levels of caspase-3 within CAOV-3 cells compared with in cells
control group (Fig. 4A). ERKIR
inhibited TNF-induced apoptosis of CAOV-3 cells compared with cells
of the control group (Fig. 4B).
PL-PTX-induced CAOV-3 cell apoptosis was also inhibited by an ERK
inhibitor (Fig. 4C). The results
of the present study suggested that the ERK/AKT signaling pathway
may be involved in the activation of the TNF/caspase-3 cascade
within ovarian cancer cells.
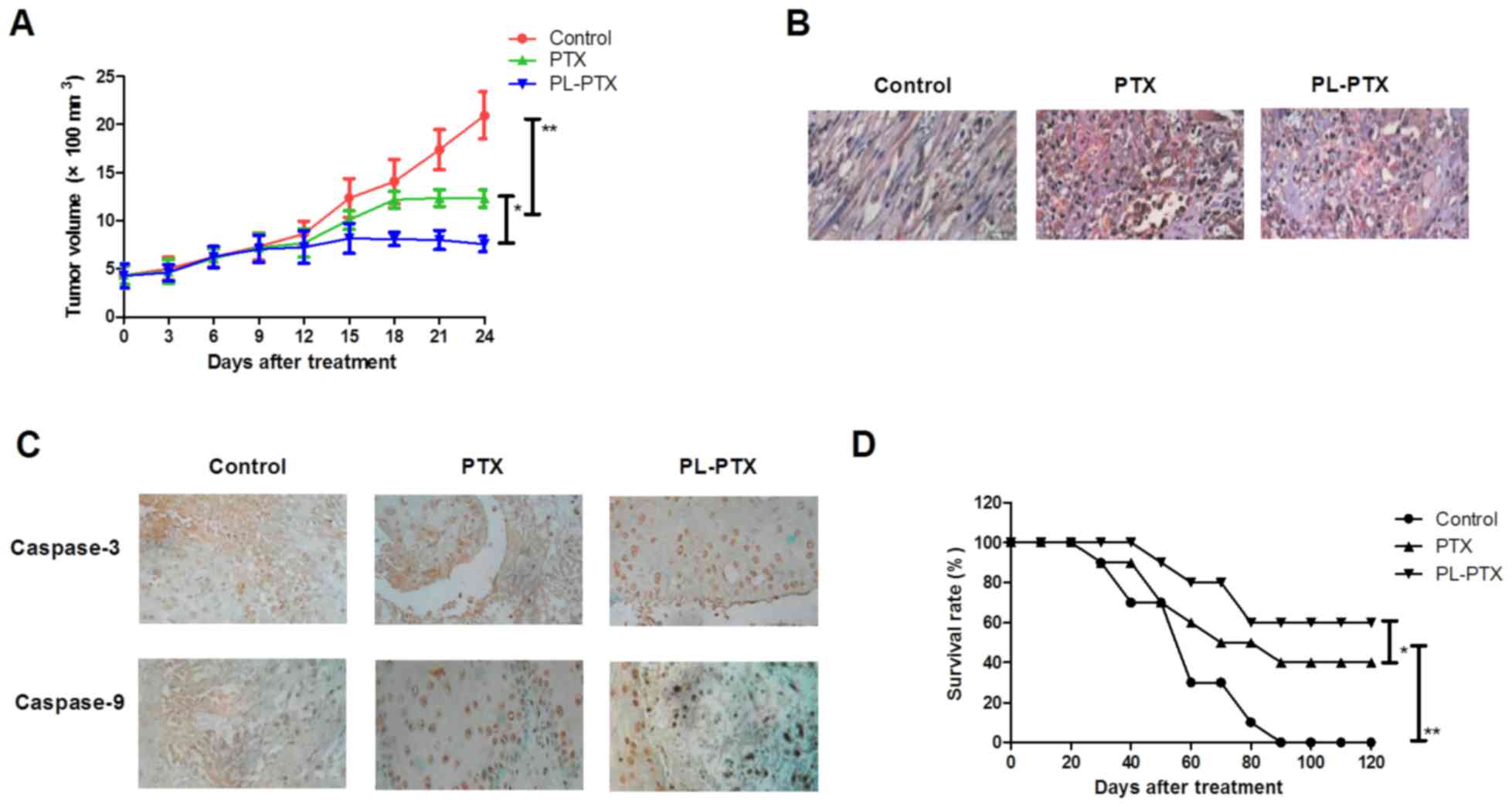
PL-PTX treatment suppresses in vivo
growth of ovarian cancer cells within a tumor mouse model
CAOV-3-bearing mouse model was established and
received treatment of PL-PTX (10 mg/kg), PTX (10 mg/kg) or PBS once
a day. In vivo analyses revealed that PL-PTX and PTX
treatments significantly inhibited the growth of ovarian cancer
cells compared with cells of the PBS groups in a 20 day observation
(Fig. 5A). TUNEL analysis revealed
that PL-PTX treatment significantly promoted tumor cell apoptosis
compared with in cells of the PTX and PBS group (Fig. 5B). Caspase-3 and caspase-9
expression levels were upregulated in response to PL-PTX and PTX
treatments (Fig. 5C). In addition,
prolonged survival was observed within the PL-PTX treated group
compared with in the PTX and PBS treated groups (Fig. 5D).
Discussion
Ovarian cancer has been associated with poor
prognosis despite the administration of maximal multimodal therapy
(19). Patients with advanced
ovarian cancer are frequently diagnosed with metastatic cancer
(20,21). It has previously been demonstrated
that PTX exerts anticancer properties on human malignancies by
inducing apoptosis and inhibiting tumor cell growth and
proliferation (22–24). A systematic review indicated that
PL-PTX is more efficient compared with PTX in inhibiting growth and
tumor metastasis of advanced, recurrent or refractory types of
ovarian cancer (25). In the
present study, the efficacy of PL-PTX within ovarian cancer cells
was analyzed in vitro and in vivo; PL-PTX treatment
was associated with the suppression of growth, migration and
invasiveness, and promotion of apoptosis of ovarian cancer
cells.
The tolerance of weekly metronomic PTX and
carboplatin have been regarded as neoadjuvant chemotherapies for
patients with advanced ovarian cancer; the efficacy of weekly vs.
every-3-week administration of PTX has been compared in patients
with ovarian cancer (26,27). Compared with PTX, PL-PTX exhibits
increased efficiency against the growth and aggressiveness of
ovarian cancer cells. Perkins et al (28) demonstrated that PTX upregulates the
protein expression levels of apoptotic peptidase activating
factor-1, caspase-9, and BH3-interating domain death agonist during
the mitochondrial events of apoptosis. The results of the present
study indicated that PL-PTX treatment upregulated caspase-3
expression levels within ovarian cancer cells; a previous study
reported that PTX treatment induces apoptosis of anaplastic thyroid
cancer cells via caspase-3 activation (29). The findings of the present study
suggested that PL-PTX treatment promoted ovarian cancer cell
apoptosis via a caspase-dependent signaling pathway.
Previously, recombinant TNF-α has been demonstrated
to be beneficial in patients with epithelial ovarian cancer
receiving PTX and cisplatinum (30). In the present study, PL-PTX
treatment was associated with the suppression of ovarian cancer via
activation of the TNF-caspase-3 cascade within ovarian cancer
cells. Suyama et al (31)
reported that ERK activation and retinoblastoma protein
phosphorylation may serve as markers of PTX sensitivity of lung
adenocarcinoma cells. In addition, previous studies have
demonstrated PTX-induced apoptosis of human gastric cancer cells
via inhibition of the ERK/AKT signaling pathway (32). In the present study, PTX induced
ovarian cancer cell apoptosis via the induction of the TNF-mediated
downregulation of ERK/AKT signaling pathway; a previous study
proposed the association of the ERK/AKT signaling activation with
cancer cell-resistance to PTX treatment (33). Additionally, a previous report
demonstrated that upregulation of caspase-3 expression levels
inhibits lung cancer metastasis and migration in a
protease-independent manner via the downregulation of the ERK
signaling pathway (34). The
present study suggested that the ERK/AKT signaling pathway is
involved in the activation of the TNF/caspase-3 cascade via PL-PTX
within ovarian cancer cells.
In conclusion, analysis of the potential mechanism
of PL-PTX-induced apoptosis within ovarian cancer cells revealed
that PL-PTX may serve as an efficient anticancer drug in the
treatment of ovarian cancer. In addition, the data of the present
study demonstrated the potent apoptotic and anti-metastatic roles
exhibited by PL-PTX in the treatment of ovarian cancer. Therefore,
PL-PTX is more efficient compared with PTX in inhibiting tumor
growth in vivo by mediating the ERK/AKT signaling inhibited
by TNF.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The analyzed data sets generated during the study
are available from the corresponding author on reasonable
request.
Authors' contributions
ZQ performed experiments. LY designed this study. YX
and FW analyzed all data in the present study.
Ethics approval and consent to
participate
The present study was conducted with the
recommendations in the guide for the Care and Use of Laboratory
Animals and was approved by the ethics committee of The Second
Hospital of Tianjin Medical University, Tianjin, China (approval
no. 20151105DGB).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Tempfer CB, El Fizazi N, Ergonenc H and
Solass W: Metastasis of ovarian cancer to the breast: A report of
two cases and a review of the literature. Oncol Lett. 11:4008–4012.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Shakeel S, Elit L, Akhtar-Danesh N,
Schneider L and Finley C: Care delivery patterns, processes, and
outcomes for primary ovarian cancer surgery: A Population-based
review using a national administrative database. J Obstet Gynaecol
Can. 39:25–33. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yamamoto A, Miyasaka Y, Furuya K, Watanabe
H, Maruyama M, Nakada H, Takano A, Hada M, Nakagomi H, Omata M and
Oyama T: Pseudo-Meigs' syndrome due to ovarian metastases from
colon cancer: A case report and review of the literature. Surg Case
Rep. 2:1122016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pimentel C, Becquet M, Lavoue V, Henno S,
Leveque J and Ouldamer L: Ovarian metastases from breast cancer: A
series of 28 cases. Anticancer Res. 36:4195–4200. 2016.PubMed/NCBI
|
|
5
|
Lago V, Minig L and Fotopoulou C:
Incidence of lymph node metastases in apparent Early-stage
low-grade epithelial ovarian cancer: A comprehensive review. Int J
Gynecol Cancer. 26:1407–1414. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Raave R, de Vries RB, Massuger LF, van
Kuppevelt TH and Daamen WF: Drug delivery systems for ovarian
cancer treatment: A systematic review and meta-analysis of animal
studies. PeerJ. 3:e14892015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Munhoz RR, Pereira AA, Sasse AD, Hoff PM,
Traina TA, Hudis CA and Marques RJ: Gonadotropin-releasing hormone
agonists for ovarian function preservation in premenopausal women
undergoing chemotherapy for Early-stage breast cancer: A systematic
review and Meta-analysis. JAMA Oncol. 2:65–73. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Bian C, Yao K, Li L, Yi T and Zhao X:
Primary debulking surgery vs. neoadjuvant chemotherapy followed by
interval debulking surgery for patients with advanced ovarian
cancer. Arch Gynecol Obstet. 293:163–168. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ong BY, Ranganath SH, Lee LY, Lu F, Lee
HS, Sahinidis NV and Wang CH: Paclitaxel delivery from PLGA foams
for controlled release in post-surgical chemotherapy against
glioblastoma multiforme. Biomaterials. 30:3189–3196. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ansaloni L, Coccolini F, Morosi L,
Ballerini A, Ceresoli M, Grosso G, Bertoli P, Busci LM, Lotti M,
Cambria F, et al: Pharmacokinetics of concomitant cisplatin and
paclitaxel administered by hyperthermic intraperitoneal
chemotherapy to patients with peritoneal carcinomatosis from
epithelial ovarian cancer. Br J Cancer. 112:306–312. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Karmakar S, Banik NL and Ray SK:
Combination of all-trans retinoic acid and paclitaxel-induced
differentiation and apoptosis in human glioblastoma U87MG
xenografts in nude mice. Cancer. 112:596–607. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nikanjam M, Gibbs AR, Hunt CA, Budinger TF
and Forte TM: Synthetic nano-LDL with paclitaxel oleate as a
targeted drug delivery vehicle for glioblastoma multiforme. J
Control Release. 124:163–171. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Merighi S, Benini A, Mirandola P, Gessi S,
Varani K, Leung E, Maclennan S, Baraldi PG and Borea PA: Hypoxia
inhibits paclitaxel-induced apoptosis through adenosine-mediated
phosphorylation of bad in glioblastoma cells. Mol Pharmacol.
72:162–172. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Slaughter KN, Moore KN and Mannel RS:
Anti-angiogenic therapy versus dose-dense paclitaxel therapy for
frontline treatment of epithelial ovarian cancer: Review of phase
III randomized clinical trials. Curr Oncol Rep. 16:4122014.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lv W, Cheng L and Li B: Development and
evaluation of a novel TPGS-mediated paclitaxel-loaded PLGA-mPEG
nanoparticle for the treatment of ovarian cancer. Chem Pharm Bull
(Tokyo). 63:68–74. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lai J, Cai Q, Biel MA, Wang C, Hu X, Wang
S and Lin J: Id1 and NF-kB promote the generation of CD133+ and
BMI-1+ keratinocytes and the growth of xenograft tumors in mice.
Int J Oncol. 44:1481–1489. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Griffith TS, Anderson RD, Davidson BL,
Williams RD and Ratliff TL: Adenoviral-mediated transfer of the
TNF-related apoptosis-inducing ligand/Apo-2 ligand gene induces
tumor cell apoptosis. J Immunol. 165:2886–2894. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sato T, Yamauchi N, Sasaki H, Takahashi M,
Okamoto T, Sakamaki S, Watanabe N and Niitsu Y: An
apoptosis-inducing gene therapy for pancreatic cancer with a
combination of 55-kDa tumor necrosis factor (TNF) receptor gene
transfection and mutein TNF administration. Cancer Res.
58:1677–1683. 1998.PubMed/NCBI
|
|
19
|
Yang XJ, Zheng FY, Xu YS and Ou RY:
Ovarian cancer initially presenting with isolated ipsilateral
superficial inguinal lymph node metastasis: A case study and review
of the literature. J Ovarian Res. 7:202014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Debniak T, Gromowski T, Scott RJ, Gronwald
J, Huzarski T, Byrski T, Kurzawski G, Dymerska D, Górski B,
Paszkowska-Szczur K, et al: Management of ovarian and endometrial
cancers in women belonging to HNPCC carrier families: Review of the
literature and results of cancer risk assessment in Polish HNPCC
families. Hered Cancer Clin Pract. 13:32015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ebell MH, Culp M, Lastinger K and Dasigi
T: A systematic review of the bimanual examination as a test for
ovarian cancer. Am J Prev Med. 48:350–356. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Han X, Chen J, Jiang M, Zhang N, Na K, Luo
C, Zhang R, Sun M, Lin G, Zhang R, et al: Paclitaxel-paclitaxel
prodrug nanoassembly as a versatile nanoplatform for combinational
cancer therapy. ACS Appl Mater Interfaces. 8:33506–33513. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Fukuchi M, Mochiki E, Ishiguro T, Ogura T,
Sobajima J, Kumagai Y, Ishibashi K and Ishida H: Efficacy of
Nab-paclitaxel as Second-line chemotherapy for unresectable or
recurrent gastric cancer. Anticancer Res. 36:6699–6703. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhang T, Luo J, Fu Y, Li H, Ding R, Gong T
and Zhang Z: Novel oral administrated paclitaxel micelles with
enhanced bioavailability and antitumor efficacy for resistant
breast cancer. Colloids Surf B Biointerfaces. 150:89–97. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Edwards SJ, Barton S, Thurgar E and Trevor
N: Topotecan, pegylated liposomal doxorubicin hydrochloride,
paclitaxel, trabectedin and gemcitabine for advanced recurrent or
refractory ovarian cancer: A systematic review and economic
evaluation. Health Technol Assess. 19:1–480. 2015. View Article : Google Scholar
|
|
26
|
Narod SA: Weekly vs. every-3-week
paclitaxel for ovarian cancer. N Engl J Med. 374:26022016.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Dessai SB, Chakraborty S, Babu TV, Nayanar
S, Bhattacharjee A, Jones J, Balasubramanian S and Patil VM:
Tolerance of weekly metronomic paclitaxel and carboplatin as
neoadjuvant chemotherapy in advanced ovarian cancer patients who
are unlikely to tolerate 3 weekly paclitaxel and carboplatin. South
Asian J Cancer. 5:63–66. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Perkins CL, Fang G, Kim CN and Bhalla KN:
The role of Apaf-1, caspase-9, and bid proteins in etoposide- or
paclitaxel-induced mitochondrial events during apoptosis. Cancer
Res. 60:1645–1653. 2000.PubMed/NCBI
|
|
29
|
Pan J, Xu G and Yeung SC: Cytochrome c
release is upstream to activation of caspase-9, caspase-8, and
caspase-3 in the enhanced apoptosis of anaplastic thyroid cancer
cells induced by manumycin and paclitaxel. J Clin Endocrinol Metab.
86:4731–4740. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Oktem M, Dilek TU, Guner H and Tiras MB:
The effect of recombinant GM-CSF on IL-6 and TNF-alpha levels in
epithelial ovarian cancer patients who received paclitaxel and
cisplatinum: Preliminary results. Eur J Gynaecol Oncol. 25:478–480.
2004.PubMed/NCBI
|
|
31
|
Suyama H, Igishi T, Sano H, Matsumoto S,
Shigeoka Y, Nakanishi H, Endo M, Burioka N, Hitsuda Y and Shimizu
E: ERK activation and subsequent RB phosphorylation are important
determinants of the sensitivity to paclitaxel in lung
adenocarcinoma cells. Int J Oncol. 24:1499–1504. 2004.PubMed/NCBI
|
|
32
|
Atjanasuppat K, Lirdprapamongkol K,
Jantaree P and Svasti J: Non-adherent culture induces paclitaxel
resistance in H460 lung cancer cells via ERK-mediated up-regulation
of βIVa-tubulin. Biochem Biophys Res Commun. 466:493–498. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Wu G, Qin XQ, Guo JJ, Li TY and Chen JH:
AKT/ERK activation is associated with gastric cancer cell
resistance to paclitaxel. Int J Clin Exp Pathol. 7:1449–1458.
2014.PubMed/NCBI
|
|
34
|
Cheng YJ, Lee CH, Lin YP, Huang JY, Su CC,
Chang WT and Yang BC: Caspase-3 enhances lung metastasis and cell
migration in a protease-independent mechanism through the ERK
pathway. Int J Cancer. 123:1278–1285. 2008. View Article : Google Scholar : PubMed/NCBI
|