Introduction
The etiology of chronic pancreatitis (CP) is most
commonly related to alcohol abuse, the incidence rate for clinical
cases increased significantly from 2.94/100,000 persons between
1977–1986 to 4.35/100,000 persons between 1997–2006 (1). CP is characterized by exocrine and
endocrine pancreatic insufficiency, persistent or recurrent
inflammation, fibrosis and macrophage infiltration (2). The main clinical symptom of CP is
abdominal pain (3). The specific
pathogenesis of CP is not clear, leading to insufficient diagnosis
and treatment. At present, the treatment of CP is limited to
symptomatic treatment rather than treatment based on the etiology
and pathogenesis of the disease (4). In some cases, partial or total
resection of the pancreas is an effective surgical treatment for
CP-related abdominal pain if other treatments are ineffective
(5,6). Due to the chronicity and constant
inflammation of CP, it is necessary to seek a treatment plan that
is highly effective and presents a low risk to patients. Therefore,
mesenchymal stem cell therapy has the potential to be an effective
means of treatment.
Mesenchymal stem cells are considered to be
pluripotent cells, which are present in adult bone marrow, the
umbilical cord, endodontic pulp and other organs (7). They have the potential to
differentiate into mesenchymal tissue lineages, including bone, fat
and muscle (8,9). Mesenchymal stem cells have been used
to treat pancreatic endocrine dysfunction in type 1 diabetes and
have considerable efficacy (10,11).
Mesenchymal stem cells can inhibit the activation of T lymphocytes
(12), and the proliferation of B
lymphocytes (13) and natural
killer cells (14). They also have
immunomodulatory functions that provide a promising therapeutic
strategy to regulate immune responses in immune-mediated diseases
(15).
There are a number of possible sources of
mesenchymal cells, but those derived from adipose tissue are
convenient and abundant (16).
Studies have shown that the transplantation of adipose-derived
mesenchymal stem cells (ASCs) markedly improves revascularization
and tissue perfusion in limb ischemia (17). Various studies have demonstrated
that ASCs have a treatment effect for severe acute pancreatitis
(AP) (18), type 1 diabetes
(19,20) and experimental colitis (21) in animal models. ASCs are currently
being tested in clinical trials for the treatment of
transsphincteric cryptoglandular fistulas (22), Crohn's-related rectovaginal fistula
(23), refractory rheumatoid
arthritis (24), severe
osteoarthritis of the knee (25),
systemic sclerosis (26) and other
diseases (27). Continuous
regional arterial infusion with low-molecular-weight heparin
exhibits strong therapeutic effects in the case of severe AP with a
high level of safety (28). In the
present study, the therapeutic effects of ASCs were studied in a
rat dibutyltin dichloride (DBTC)-induced CP model via inferior vena
cava and left gastric artery injection. It was found that ASCs
could delay the progression of CP by suppressing the PI3K/AKT/mTOR
pathway.
Materials and methods
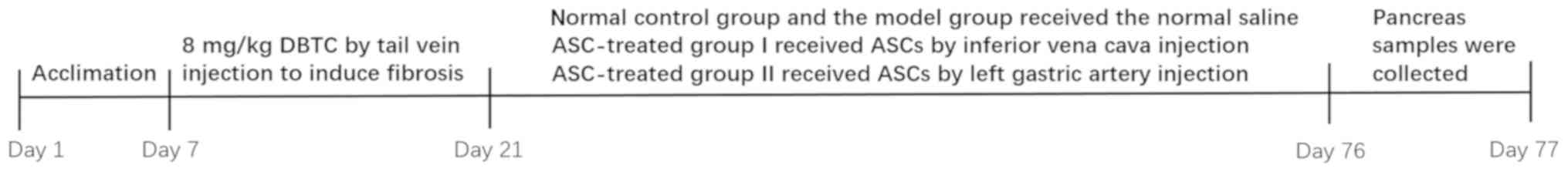
Animals and treatment
A total of 24 adult male Sprague-Dawley (SD) rats
weighing approximately 280 g were obtained from the animal center
at Wenzhou Medical University. All animal work was approved by the
Animal Ethics Committee of Wenzhou Medical University. The rats
were kept in an environment with a comfortable humidity and were
given no less than ten hours of light each day at 28–30°C. The
animals were allowed free access to food and water and were
acclimated to the environment for one week before the experiment
began. CP was induced by a single 8 mg/kg intravenous
administration of DBTC (Schering AG) and ASCs were then introduced
via different routes of administration. Lastly, the pancreatic
tissue was removed for further study. The experiment schedule is
shown in Fig. 1. The rats were
randomly divided into four groups with six rats per group: Control
group (rats received normal saline); DBTC-induced CP model group
(CP was induced in the rats via DBTC injection through the tail
vein); ASC-treated group I (after DBTC-induced CP, the rats were
anesthetized via an intraperitoneal injection of 5% chloral
hydrate, 300 mg/kg, and received 2,000,000 cells/kg ASCs via
inferior vena cava injection); and ASC-treated group II (after
DBTC-induced CP, the rats were anesthetized via an intraperitoneal
injection of 5% chloral hydrate, 300 mg/kg, and received 2,000,000
cells/kg ASCs by left gastric artery injection). All the rats,
except for the control, were given 10% ethanol per day for 10 weeks
after the DBTC injection to induce pancreatic fibrosis; the rats in
the control group were given normal drinking water. In the third
week, the rats in the ASC-treated group I received 2,000,000
cells/kg ASCs by inferior vena cava injection, and the rats in the
ASC-treated groups II received 2,000,000 cells/kg ASCs by left
gastric artery injection. The rats in the DBTC-induced CP model
group and the control group received the equivalent volume of
normal saline by intravenous injection. At the end of the
experiment, all animals were euthanized by intraperitoneal
injection of pentobarbital sodium (200 mg/kg). Finally, pancreatic
tissue samples were collected and stored at −80°C for further
examination.
Cell culture
SD rat ASCs were purchased from Cyagen Biosciences,
Inc., and cultured in OriCell™ Adipose-Derived Mesenchymal Stem
Cell Growth Medium (Cyagen Biosciences, Inc.). Cells were incubated
at 37°C in an atmosphere containing 5% CO2 and passaged
using 0.25% trypsin-EDTA solution before the treatment began.
Histological features of pancreatic
tissue
Pancreatic tissue samples were placed on
standardized 1×1 cm pieces of paper. They were fixed in 10%
paraformaldehyde overnight at 4°C, embedded in paraffin and
sectioned into 6-µm-thick slices. The slices were then stained
using Sirius red stain (staining: Sirius red dye for 1 h; and Mayer
hematoxylin for 15 min at 25°C). The sections were then observed
under a light microscope (Nikon Corporation) to determine
pancreatic pathological changes.
Immunohistochemistry assays
Pancreatic tissue samples were fixed in 10%
paraformaldehyde overnight at 4°C, embedded in paraffin and
sectioned into 4-µm-thick slices. The slices were then incubated in
an oven overnight at 55–65°C. After 30 min of deparaffinization in
xylene, the slices were rehydrated in a graded ethanol series. The
slices were then incubated in citrate buffer for 5 min at 25°C and
treated in a microwave oven for 15 min for antigen repair at
65–75°C.
The sections were washed with 3%
H2O2 and blocked with 10% goat serum (OriGene
Technologies, Inc.) for 60 min at 37°C. The samples were incubated
with the primary antibody against collagen type I (1:1,000; cat.
no. 66761-1-Ig; ProteinTech Group, Inc.) and collagen type III
(1:1,000; cat. no. 22734-1-AP; ProteinTech Group, Inc.) overnight
at 4°C. Species-specific secondary antibody (1:200; A0277; Beyotime
Institute of Biotechnology) was added to the pancreatic tissue
sections for 60 min at 37°C. Finally, the pancreatic tissue
sections were stained with diaminobenzidine for 10 min at 25°C, and
the cell nuclei were stained with hematoxylin for 3 min at 25°C.
After sealing the sections with neutral resin, they were examined
under a light microscope.
Western blot analysis
The pancreatic tissues were incubated for 60 min in
a mixture of radioimmunoprecipitation assay buffer (Beyotime
Institute of Biotechnology), phosphatase inhibitor (Roche
Diagnostics GmbH) and phenylmethylsulfonyl fluoride (Beyotime
Institute of Biotechnology) at a ratio of 100:10:1, which was used
to extract proteins from the pancreatic tissue. The tissue lysate
was then centrifuged at 12,000 × g for 20 min at 4°C, and the
supernatant was collected. The total protein concentration was
determined by a BCA protein kit (Beyotime Institute of
Biotechnology). The mixture of protein samples and gel-loading
buffer was boiled for 5 min and then stored overnight at 4°C.
Protein samples (16 µl) were isolated by SDS-PAGE (10%) and then
transferred to PVDF membranes (EMD Millipore). Membranes were
blocked with 5% skimmed milk powder for 2 h at 25°C. The blots were
incubated with primary antibodies at 4°C overnight, followed by
incubation with a horseradish peroxidase-conjugated goat
anti-rabbit IgG antibody (1:10,000; BioSharp, Technology Inc.) at
room temperature for 1 h. Primary antibodies to the following
proteins were used: Collagen type I (1:1,000; cat. no. 66761-1-Ig;
ProteinTech Group, Inc.), Collagen type III (1:1,000; cat. no.
22734-1-AP; ProteinTech Group, Inc.), tumor necrosis factor-α
(TNF-α; 1:1,000; cat. no. ab6671; Abcam), PI3K (1:1,000; cat. no.
4249S; Cell Signaling Technology, Inc.), phosphorylated (p)-PI3K
(1:1,000; cat. no. 4228S; Cell Signaling Technology, Inc.), AKT
(1:1,000; cat. no. 4691T; Cell Signaling Technology, Inc.), p-AKT
(1:1,000; cat. no. 4060S; Cell Signaling Technology, Inc.), mTOR
(1:1,000; cat. no. 2983S; Cell Signaling Technology, Inc.), p-mTOR
(1:1,000; cat. no. 5536S; Cell Signaling Technology, Inc.), BAX
(1:1,000; 2772S; Cell Signaling Technology, Inc.), BCl-2 (1:1,000;
cat. no. ab59348; Abcam), caspase-3 (1:1,000; cat. no. 9662S; Cell
Signaling Technology, Inc.) and GAPDH (1:1,000; cat. no. 5174S;
Cell Signaling Technology, Inc.). Finally, protein bands were
visualized by an enhanced chemiluminescence detection system
(VisionWorks 8.20; Analytik Jena US LLC).
Statistical analysis
Data are presented as mean ± SD and analyzed using
one-way ANOVA followed by Tukey's post hoc test. Statistical
significance was determined as P<0.05. The data were obtained
from independent experiments conducted three times.
Results
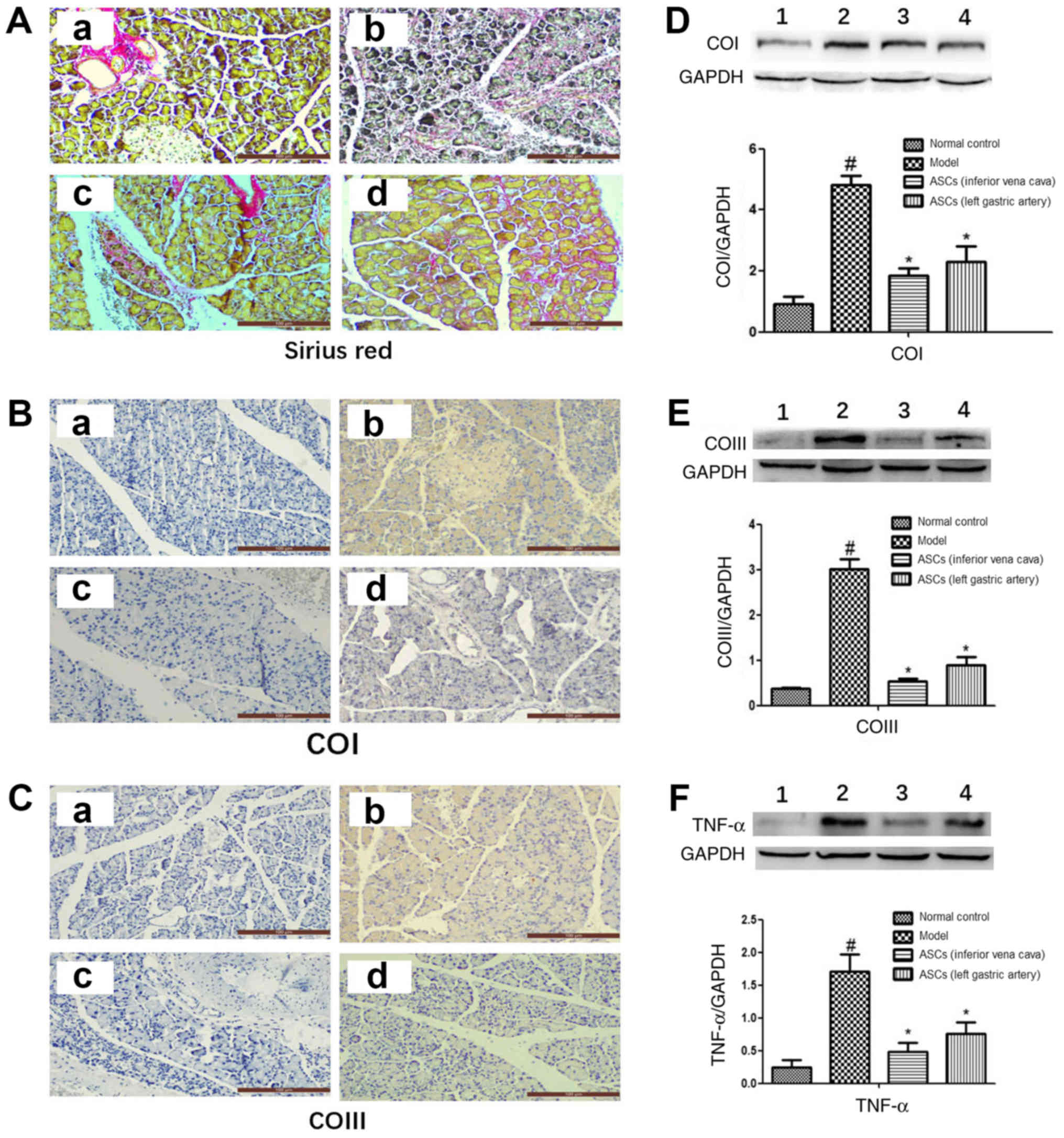
ASC treatment ameliorates pancreatic
fibrosis and alleviates collagen accumulation
The level of pancreatic fibrosis and collagen
accumulation was visualized by Sirius Red staining. Rats from the
control group showed a standard histological structure with
pancreatic acinar cells closely arranged around the islets. Samples
from the DBTC-induced CP model group showed significant fibrous
connective tissue hyperplasia, acinar cell atrophy and necrosis.
However, ASC treatment markedly improved pancreatic morphology and
architecture. There was no accumulation of collagen in the healthy
pancreatic cells, but there was an accumulation of collagen in the
wall of the healthy blood vessels (Fig. 2A-a). In the DBTC-induced CP model
group, pancreatic cells were surrounded by collagen, and the normal
structure of the pancreatic tissue was destroyed (Fig. 2A-b). However, ASC treatment
markedly decreased collagen accumulation and damage in pancreatic
tissues of DBTC-induced CP (Fig. 2A-c
and A-d). Moreover, it was found that ASC treatment markedly
decreased the expression levels of collagen type I, collagen type
III and TNF-α in pancreatic tissues of DBTC-induced CP (Fig. 2B-F). However, there was no
statistical difference in the expression level of collagen type I,
collagen type III and TNF-α between the ASC-treated group I and the
ASC-treated group II. Overall, these findings demonstrated that
ASCs could preserve pancreatic structure and inhibit collagen
accumulation and pancreatic fibrogenesis, regardless of the site of
injection (inferior vena cava or left gastric artery).
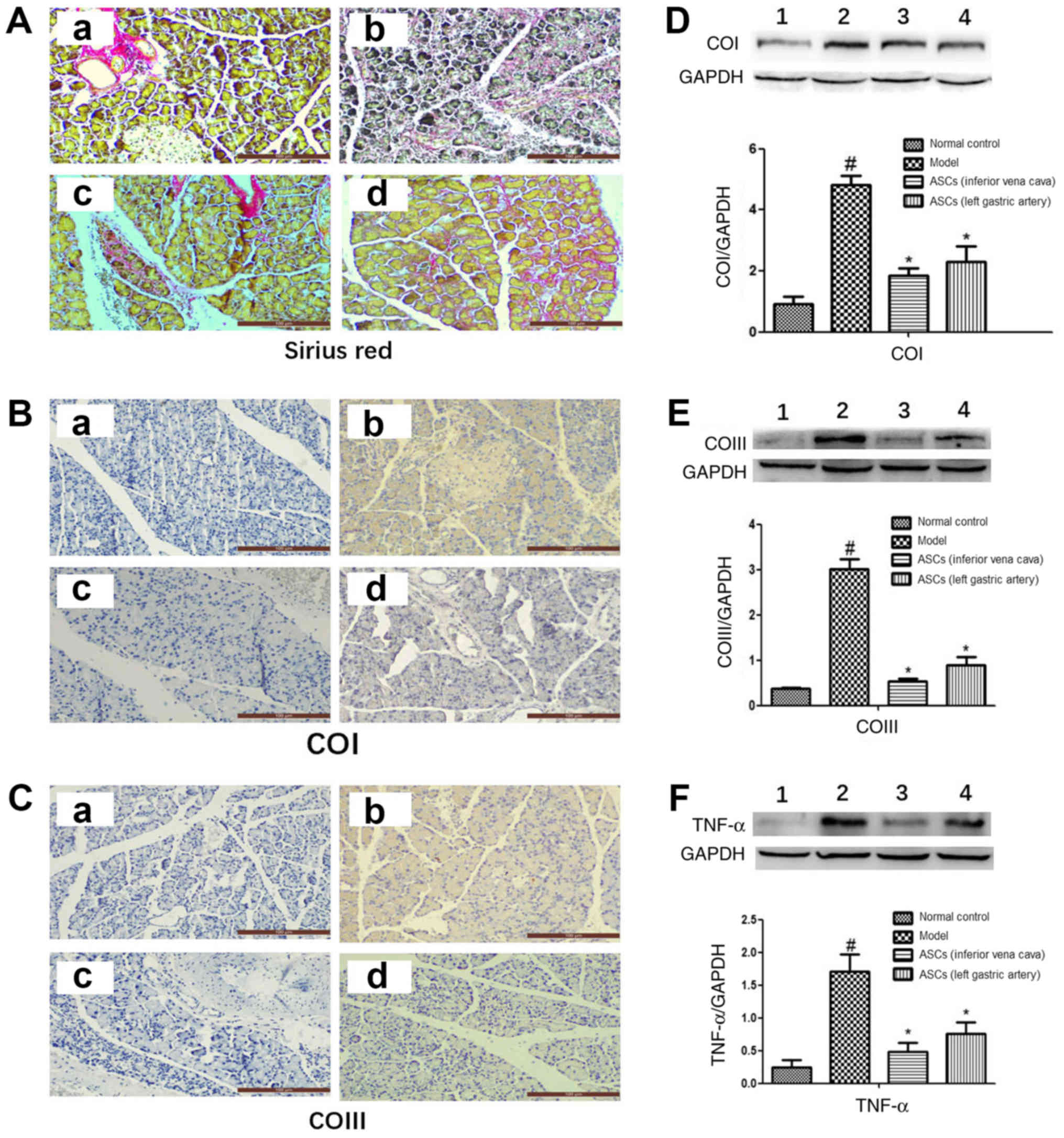 | Figure 2.ASCs reduce pancreatic tissue
collagen accumulation in DBTC-induced pancreatic fibrosis. (A)
Pancreatic collagen was observed by Sirius Red staining
(magnification, ×200). Using immunohistochemical staining
(magnification, ×200) the expression of (B) COI and (C) COIII was
detected. Images represent: a, the control; b, the DBTC-induced
chronic pancreatitis model; c, the ASC-treated group I; and d, the
ASC-treated group II. Using western blotting the expression of (D)
COI, (E) COIII and (F) TNF-α were detected. Bands represent: 1, the
control; 2, the DBTC-induced chronic pancreatitis model; 3, the
ASC-treated group I; and 4, the ASC-treated group II. Data are
presented as mean ± SEM (n=3). #P<0.05 vs. Control
group; *P<0.05 vs. DBTC-induced chronic pancreatitis model
group. ASC, adipose-derived mesenchymal stem cell; DBTC, dibutyltin
dichloride; COI, collagen type I; COIII, collagen type III; TNF-α,
tumor necrosis factor-α. |
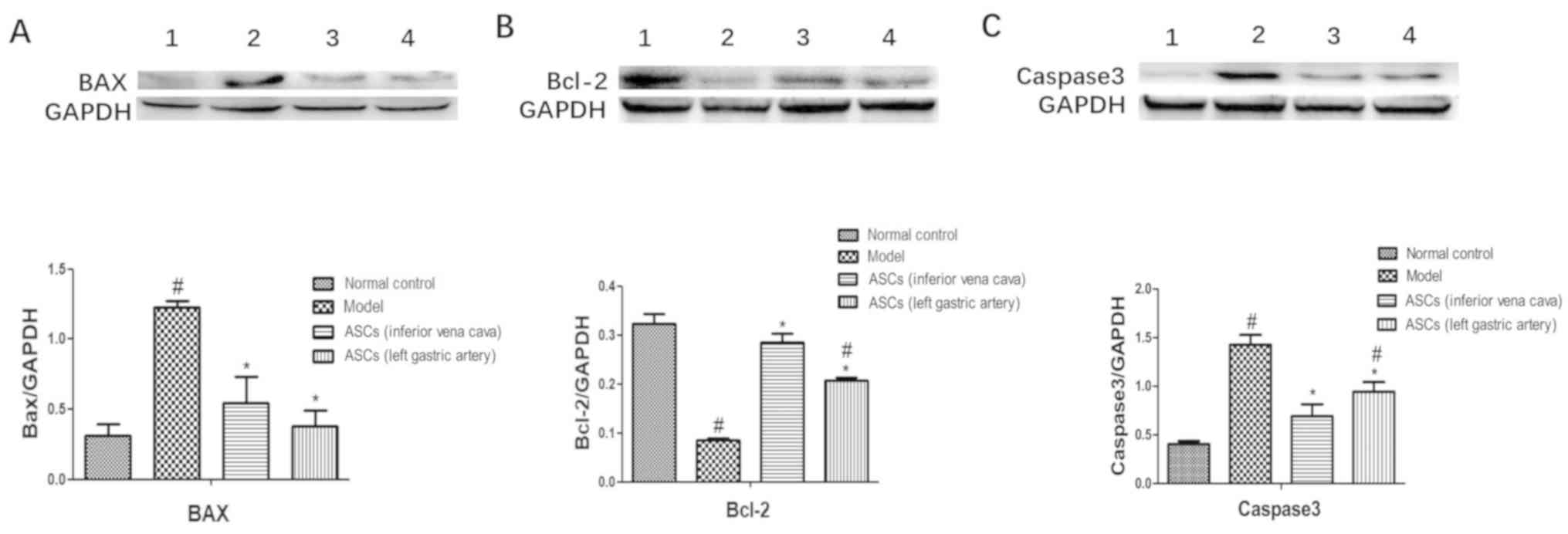
ASCs decrease DBTC-induced pancreatic
cell apoptosis
In this study, the expression levels of
apoptosis-related proteins of the pancreatic tissues were examined
using western blotting. The apoptosis-related proteins include BAX,
Bcl-2 and caspase-3. As shown in Fig.
3, ASC treatment markedly increased the expression level of the
anti-apoptotic protein Bcl-2. ASC treatment also significantly
decreased the expression levels of the pro-apoptotic protein BAX.
The expression levels of caspase-3 were significantly increased in
the CP model group. After ASC treatment, the expression level of
caspase-3 was markedly decreased. However, there was no statistical
difference in the expression of BAX, Bcl-2 and caspase-3 between
ASC-treated group I and ASC-treated group II. These results
demonstrated that ASCs could reduce DBTC-induced pancreatic cell
apoptosis regardless of the site of injection (inferior vena cava
or left gastric artery).
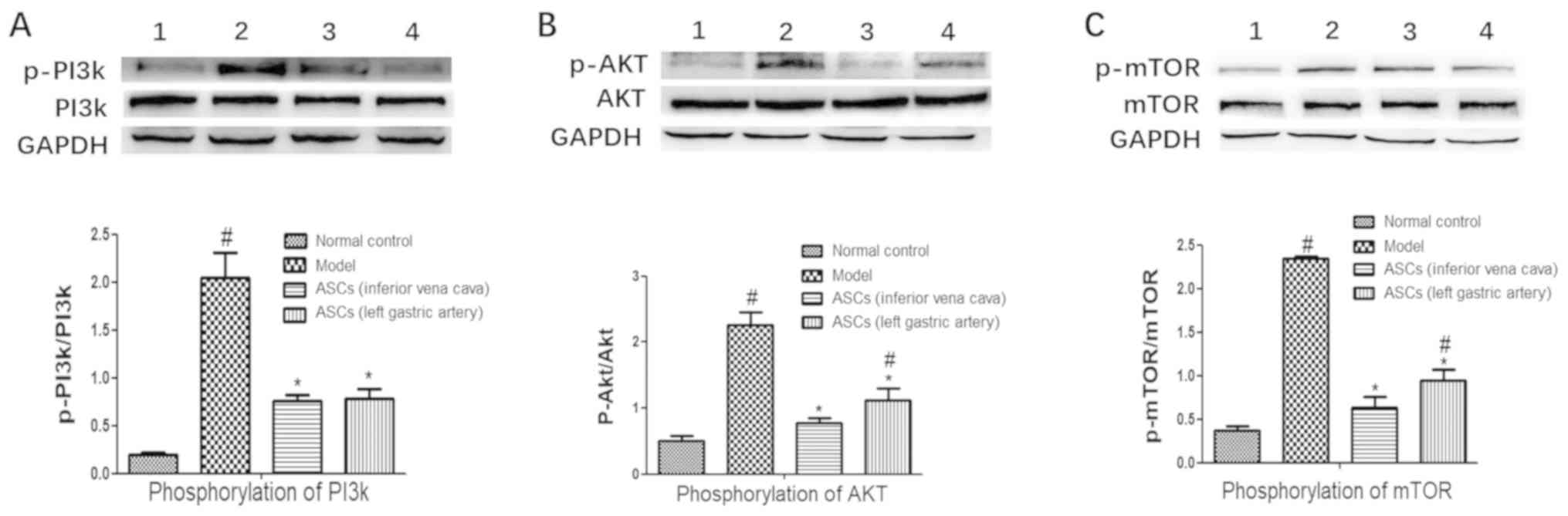
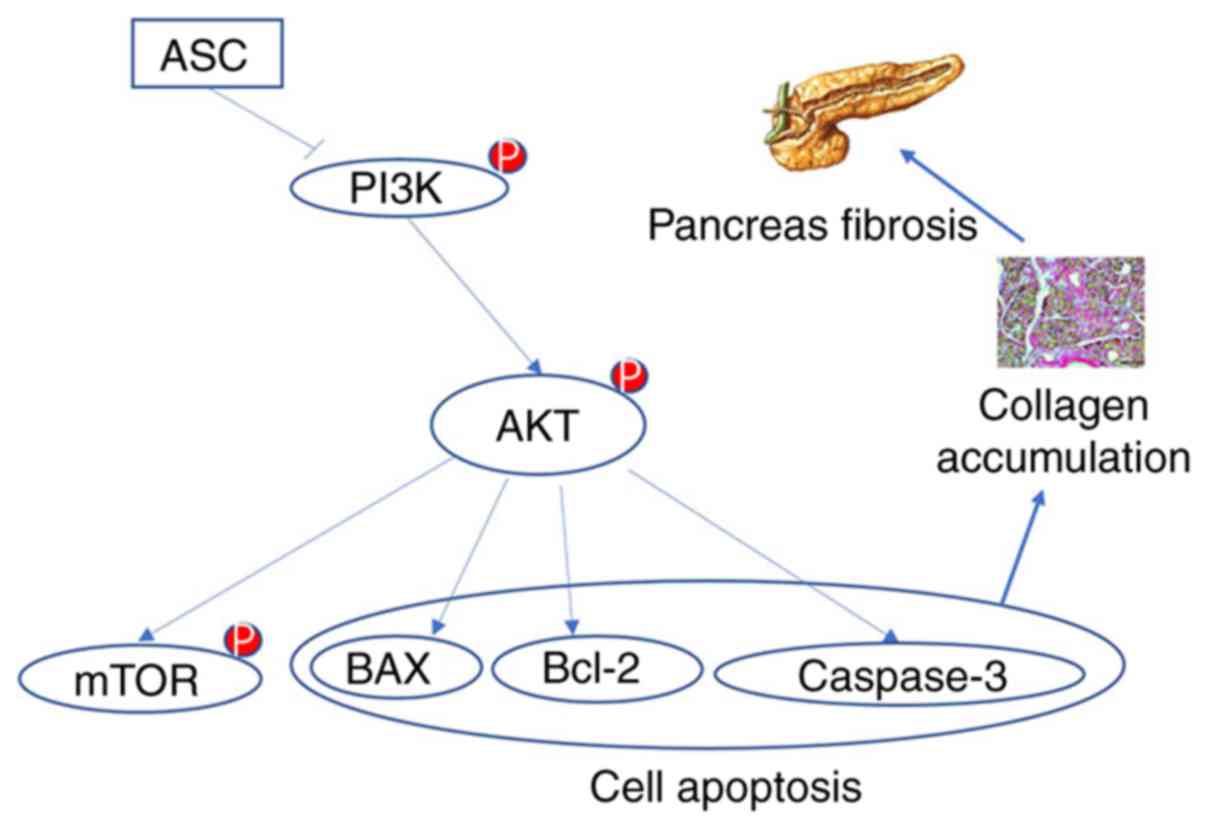
ASCs suppress the PI3K/AKT/mTOR
pathway in DBTC-induced CP
To explore whether there is a link between
pancreatic fibrosis and the PI3K/AKT/mTOR pathway, the
PI3K/AKT/mTOR pathway in pancreatic tissue was analyzed. The
expressions of p-PI3K, p-AKT and p-mTOR were markedly increased in
the DBTC-induced CP model group. However, ASC treatment
significantly decreased the expression levels of the p-PI3K, p-AKT
and p-mTOR compared to the DBTC-induced CP model group (Fig. 4A-C). There was no statistical
difference in the expression levels of the p-PI3K, p-AKT and p-mTOR
between the ASC-treated groups I and II. These results demonstrated
that the ASCs suppressed activation of the PI3K/AKT/mTOR pathway
(Fig. 4).
Discussion
CP is characterized by inflammation and persistent
pancreatic damage with collagen accumulation that ultimately leads
to pancreatic fibrosis (29,30).
Hepatocyte damage and fibrosis have a close relationship with
hepatic stellate cell activation (31). Stellate cells that resemble hepatic
stellate cells and have similar functions were also found in the
pancreas (32). Pancreatic tissue
damage and inflammation in CP that release cytokines can lead to
the activation of pancreatic stellate cells (PSCs), which
ultimately leads to pancreatic fibrosis (33). ASCs were able to suppress PSC
activation and proliferation, as well as inducing their apoptosis
(34). ASCs could have a potential
protective effect for pancreatic tissue damage and pancreatic
fibrosis. At present, the underlying mechanism of how ASCs
alleviate pancreatic fibrosis remains unclear. In the present
study, CP was induced by a single intravenous administration of
DBTC. The DBTC treatment caused severe injury and fibrosis of the
pancreatic tissue, and ASCs treatment reduced the degree of
pancreatic fibrosis and damage. These results indicated that ASCs
are able to alleviate DBTC-induced pancreatic damage.
Collagen type I and III are overexpressed in
pancreatic fibrosis, and numerous studies have found that specific
signaling molecules, such as Sma- and Mad-related proteins,
mitogen-activated protein kinases, and peroxisome
proliferator-activated receptor g participate in the synthesis of
proteins of the extracellular matrix. Activation of these pathways
leads to collagen accumulation and accelerates fibrotic progression
(35–37). TNF-α is a monokine that displays
pro-inflammatory properties. It is produced in the pancreas in the
early stages of AP and is detected in high amounts in both blood
and pancreatic tissue (38). TNF-α
also occurs in the early stages of CP, and its expression has been
observed in acinar cells, as well as in inflamed cells (39). Studies have revealed that TNF-α is
also important in the development of CP by affecting PSCs (40). In a healthy pancreas, collagen type
IX dominates, while type I is mainly produced in response to TNF-α
(41). In the present study, it
was also found that DBTC injection leads to collagen accumulation
in the pancreatic tissues, as shown by Sirius Red staining, and ASC
treatment could markedly reduce collagen accumulation in the
pancreatic tissues of DBTC-induced CP. Moreover, ASC treatment
notably suppressed the expressions of TNF-α, collagen type I and
collagen type III in pancreatic tissue. These results indicated
that ASCs decrease the accumulation of collagen in pancreatic
tissue and reduce the degree of pancreatic fibrosis.
The caspase family is a group of structurally
related cysteine proteases in the cytosol that is closely related
to cell proliferation, differentiation and migration (42). Caspases are divided into apoptotic
and pro-inflammatory types, depending on their involvement in these
cellular responses (43). Caspases
also play a key role in the regulation of pancreatic acinar cell
death (44). Caspase 3 is the
prototype of the protein family and has an important role in the
mechanism of apoptosis (45).
Bcl-2 is an antiapoptotic protein that regulates mitochondrial
pathways to led to antiapoptotic effects (46), and its expression is increased
during the activation of PSC (47). Moreover, Bcl-2 inhibitors
potentiate acinar cell necrosis in the in vitro model of
pancreatitis (48). The expression
of BAX is increased during apoptosis of pancreatic acinar cells
during induction AP (49). In the
present study, ASC treatment markedly improved the expression
levels of Bcl-2 and significantly suppressed the expression levels
of BAX and caspase-3. These results demonstrated that the
therapeutic effect of ASCs inhibit DBTC-induced pancreatic fibrosis
and reduce pancreatic cell apoptosis.
The PI3K/AKT/mTOR pathway is over-activated in
pancreatic neuroendocrine tumor pathogenesis (50–55),
breast cancer brain metastases (56) and colorectal cancer (57). The PI3K/AKT/mTOR signaling pathway
is closely related to cell proliferation, differentiation,
apoptosis, exercise, metabolism and autophagy (58,59).
The inhibition of this pathway contributes to the treatment of
cancer patients, suggesting that it can be used as a target for the
treatment of certain cancers (60). Previous studies indicated that
saikosaponin d prevents pancreatic fibrosis by reducing the
autophagy of PSCs via the PI3K/AKT/mTOR pathway (61). In the present study, ASC treatment
significantly decreased the phosphorylation of PI3K, AKT and mTOR
in pancreatic tissue, suggesting that ASCs can successfully
suppress the PI3K/AKT/mTOR pathway to reduce the degree of fibrosis
in pancreatic tissue.
As discussed, pancreatic fibrosis is associated with
the activation of PSCs; however, it is still unknown whether the
ASC treatment of DBTC-induced CP suppresses the activation of PSCs
by inhibiting the PI3K/AKT/mTOR pathway. This needs further
verification. The present study demonstrated the potential use of
mesenchymal stem cell therapy in the clinical treatment of CP. In
clinical practice, AP can be treated by regional arterial infusion
of drugs, with improved results compared with intravenous treatment
(62,63). Therefore, this study explored
whether different approaches to CP could have an impact on the
outcome of the treatment. It was shown that there was no
statistically significant difference between the two treatment
groups. The next step is to investigate whether ASCs can inhibit
the activation of PSCs in vitro and its possible mechanism.
In conclusion, this study demonstrated that ASCs alleviated
DBTC-induced pancreatic fibrosis in rats by regulating the
PI3K/AKT/mTOR pathway (Fig. 5).
These findings may provide a new strategy for the treatment of
CP.
Acknowledgements
Not applicable.
Funding
This study was supported by grants from The National
Natural Science of China (grant no. 81770630), Natural Science
Foundation of Zhejiang Province (grant no. LY16H030013) and Wenzhou
Municipal Science and Technology Bureau (grant no. Y20150062).
Availability of data and materials
The data used to support the findings of this study
are available from the corresponding author upon request.
Authors' contributions
XX carried out the experiment and wrote the article.
HY participated in the experiment and made substantial
contributions to the conception and design of the experiments. LS
was involved in the article writing and interpretation of data. CZ,
YS and ZZ contributed to the analysis and interpretation of data.
CW and BC contributed to the design of the study. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
Animal Experiment Ethics Number of Experimental
Animal Center of Wenzhou Medical University (policy no.
wydw2019-0971).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Yadav D, Timmons L, Benson JT, Dierkhising
RA and Chari ST: Incidence, prevalence, and survival of chronic
pancreatitis: A population-based study. Am J Gastroenterol.
106:2192–2199. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lankisch PG: Natural course of chronic
pancreatitis. Pancreatology. 1:3–14. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
DiMagno MJ and Dimagno EP: Chronic
pancreatitis. Curr Opin Gastroenterol. 22:487–497. 2006.PubMed/NCBI
|
|
4
|
Andrén-Sandberg A, Hoem D and Gislason H:
Pain management in chronic pancreatitis. Eur J Gastroenterol
Hepatol. 14:957–970. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Argo JL, Contreras JL, Wesley MM and
Christein JD: Pancreatic resection with islet cell autotransplant
for the treatment of severe chronic pancreatitis. Am Surg.
74:530–536. 2008.PubMed/NCBI
|
|
6
|
Dixon J, DeLegge M, Morgan KA and Adams
DB: Impact of total pancreatectomy with islet cell transplant on
chronic pancreatitis management at a disease-based center. Am Surg.
74:735–738. 2008.PubMed/NCBI
|
|
7
|
da Silva Meirelles L, Chagastelles PC and
Nardi NB: Mesenchymal stem cells reside in virtually all post-natal
organs and tissues. J Cell Sci. 119:2204–2213. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pittenger MF, Mackay AM, Beck SC, Jaiswal
RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S and
Marshak DR: Multilineage potential of adult human mesenchymal stem
cells. Science. 284:143–147. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jiang Y, Jahagirdar BN, Reinhardt RL,
Schwartz RE, Keene CD, Ortiz-Gonzalez XR, Reyes M, Lenvik T, Lund
T, Blackstad M, et al: Pluripotency of mesenchymal stem cells
derived from adult marrow. Nature. 418:41–49. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
D'Addio F, Valderrama Vasquez A, Ben Nasr
M, Franek E, Zhu D, Li L, Ning G, Snarski E and Fiorina P:
Autologous nonmyeloablative hematopoietic stem cell transplantation
in new-onset type 1 diabetes: A multicenter analysis. Diabetes.
63:3041–3046. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Frumento D, Ben Nasr M, El Essawy B,
D'Addio F, Zuccotti GV and Fiorina P: Immunotherapy for type 1
diabetes. J Endocrinol Invest. 40:803–814. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Krampera M, Glennie S, Dyson J, Scott D,
Laylor R, Simpson E and Dazzi F: Bone marrow mesenchymal stem cells
inhibit the response of naive and memory antigen-specific T cells
to their cognate peptide. Blood. 101:3722–3729. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Corcione A, Benvenuto F, Ferretti E,
Giunti D, Cappiello V, Cazzanti F, Risso M, Gualandi F, Mancardi
GL, Pistoia V and Uccelli A: Human mesenchymal stem cells modulate
B-cell functions. Blood. 107:367–372. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sotiropoulou PA, Perez SA, Gritzapis AD,
Baxevanis CN and Papamichail M: Interactions between human
mesenchymal stem cells and natural killer cells. Stem Cells.
24:74–85. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Nauta AJ and Fibbe WE: Immunomodulatory
properties of mesenchymal stromal cells. Blood. 110:3499–3506.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Jurgens WJ, Oedayrajsingh-Varma MJ, Helder
MN, Zandiehdoulabi B, Schouten TE, Kuik DJ, Ritt MJ and van
Milligen FJ: Effect of tissue-harvesting site on yield of stem
cells derived from adipose tissue: Implications for cell-based
therapies. Cell Tissue Res. 332:415–426. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Bura A, Planat-Benard V, Bourin P,
Silvestre JS, Gross F, Grolleau JL, Saint-Lebese B, Peyrafitte JA,
Fleury S, Gadelorge M, et al: Phase I trial: The use of autologous
cultured adipose-derived stroma/stem cells to treat patients with
non-revascularizable critical limb ischemia. Cytotherapy.
16:245–257. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kim HW, Song WJ, Li Q, Han SM, Jeon KO,
Park SC, Ryu MO, Chae HK, Kyeong K and Youn HY: Canine adipose
tissue-derived mesenchymal stem cells ameliorate severe acute
pancreatitis by regulating T cells in rats. J Vet Sci. 17:539–548.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kang HM, Kim J, Park S, Kim J, Kim H, Kim
KS, Lee EJ, Seo SI, Kang SG, Lee JE and Lim H: Insulin-secreting
cells from human eyelid-derived stem cells alleviate type I
diabetes in immunocompetent mice. Stem Cells. 27:1999–2008. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Bassi ÊJ, Moraes-Vieira PM, Moreira-Sá CS,
Almeida DC, Vieira LM, Cunha CS, Hiyane MI, Basso AS, Pacheco-Silva
A and Câmara NO: Immune regulatory properties of allogeneic
adipose-derived mesenchymal stem cells in the treatment of
experimental autoimmune diabetes. Diabetes. 61:2534–2545. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Lopez-Santalla M, Mancheño-Corvo P,
Escolano A, Menta R, DelaRosa O, Abad JL, Büscher D, Redondo JM,
Bueren JA, Dalemans W, et al: Biodistribution and efficacy of human
adipose-derived mesenchymal stem cells following intranodal
administration in experimental colitis. Front Immunol. 8:6382017.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Dozois EJ, Lightner AL, Mathis KL, Chua
HK, Kelley SR, Fletcher JG, Dietz AB, Friton JJ, Butler GW and
Faubion WA: Early results of a phase I trial using an
adipose-derived mesenchymal stem cell-coated fistula plug for the
treatment of transsphincteric cryptoglandular fistulas. Dis Colon
Rectum. 62:615–622. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sanz-Baro R, García-Arranz M, Guadalajara
H, de la Quintana P, Herreros MD and García-Olmo D: First-in-human
case study: Pregnancy in women with crohn's perianal fistula
treated with adipose-derived stem cells: A safety study. Stem Cells
Transl Med. 4:598–602. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Álvaro-Gracia JM, Jover JA, García-Vicuña
R, Carreño L, Alonso A, Marsal S, Blanco F, Martínez-Taboada VM,
Taylor P, Martín-Martín C, et al: Intravenous administration of
expanded allogeneic adipose-derived mesenchymal stem cells in
refractory rheumatoid arthritis (Cx611): Results of a multicentre,
dose escalation, randomised, single-blind, placebo-controlled phase
Ib/IIa clinical trial. Ann Rheum Dis. 76:196–202. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Pers YM, Rackwitz L, Ferreira R, Pullig O,
Delfour C, Barry F, Sensebe L, Casteilla L, Fleury S, Bourin P, et
al: Adipose mesenchymal stromal cell-based therapy for severe
osteoarthritis of the knee: A phase I dose-escalation trial. Stem
Cells Transl Med. 5:847–856. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Guillaume-Jugnot P, Daumas A, Magalon J,
Jouve E, Nguyen PS, Truillet R, Mallet S, Casanova D, Giraudo L,
Veran J, et al: Autologous adipose-derived stromal vascular
fraction in patients with systemic sclerosis: 12-month follow-up.
Rheumatology (Oxford). 55:301–306. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Díez-Tejedor E, Gutiérrez-Fernández M,
Martínez-Sánchez P, Rodríguez-Frutos B, Ruiz-Ares G, Lara ML and
Gimeno BF: Reparative therapy for acute ischemic stroke with
allogeneic mesenchymal stem cells from adipose tissue: A safety
assessment: A phase II randomized, double-blind,
placebo-controlled, single-center, pilot clinical trial. J Stroke
Cerebrovasc Dis. 23:2694–2700. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ke L, Ni HB, Tong ZH, Li WQ, Li N and Li
JS: Efficacy of continuous regional arterial infusion with
low-molecular-weight heparin for severe acute pancreatitis in a
porcine model. Shock. 41:443–448. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Sarles H: Etiopathogenesis and definition
of chronic pancreatitis. Dig Dis Sci. 31 (9 Suppl):91S–107S. 1986.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Witt H, Apte MV, Keim V and Wilson JS:
Chronic pancreatitis: Challenges and advances in pathogenesis,
genetics, diagnosis, and therapy. Gastroenterology. 132:1557–1573.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Friedman SL: Hepatic stellate cells:
Protean, multifunctional, and enigmatic cells of the liver. Physiol
Rev. 88:125–172. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Omary MB, Lugea A, Lowe AW and Pandol SJ:
The pancreatic stellate cell: A star on the rise in pancreatic
diseases. J Clin Invest. 117:50–59. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Xu M, Wang G, Zhou H, Cai J, Li P, Zhou M,
Lu Y, Jiang X, Huang H, Zhang Y and Gong A: TGF-β1-miR-200a-PTEN
induces epithelial-mesenchymal transition and fibrosis of
pancreatic stellate cells. Mol Cell Biochem. 43:1161–1168.
2017.
|
|
34
|
Yu FX, Su LF, Dai CL, Wang Y, Teng YY, Fu
JH, Zhang QY and Tang YH: Inhibition of pancreatic stellate cell
activity by adipose-derived stem cells. Hepatobiliary Pancreat Dis
Int. 14:215–221. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Zhang SK, Tsui NC, Li DH, Yao GW and Wang
YN: Expression of transforming growth factor beta1/Sma- and
Mad-related proteins in rat with chronic pancreatitis induced by
dibutyltin dichloride. Pancreas. 39:252–253. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Schwer CI, Mutschler M, Stoll P, Goebel U,
Humar M, Hoetzel A and Schmidt R: Carbon monoxide releasing
molecule-2 inhibits pancreatic stellate cell proliferation by
activating p38 mitogen-activated protein kinase/heme oxygenase-1
signaling. Mol Pharmacol. 77:660–669. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Fortunato F, Berger I, Gross ML, Rieger P,
Buechler MW and Werner J: Immune-compromised state in the rat
pancreas after chronic alcohol exposure: The role of peroxisome
proliferator-activated receptor gamma. J Pathol. 213:441–452. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Mayer J, Rau B, Gansauge F and Beger HG:
Inflammatory mediators in human acute pancreatitis: Clinical and
pathophysiological implications. Gut. 47:546–552. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Xie MJ, Motoo Y, Su SB and Sawabu N:
Expression of tumor necrosis factor-alpha, interleukin-6, and
interferon-gamma in spontaneous chronic pancreatitis in the WBN/Kob
rat. Pancreas. 22:400–408. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Mews P, Phillips P, Fahmy R, Korsten M,
Pirola R, Wilson J and Apte M: Pancreatic stellate cells respond to
inflammatory cytokines: Potential role in chronic pancreatitis.
Gut. 50:535–541. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Poudel B, Ki HH, Lee YM and Kim DK:
Collagen I-induced dendritic cells activation is regulated by
TNF-αlpha production through down-regulation of IRF4. J Biosci.
40:71–78. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Li J and Yuan J: Caspases in apoptosis and
beyond. Oncogene. 27:6194–6206. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Man SM and Kanneganti TD: Converging roles
of caspases in inflammasome activation, cell death and innate
immunity. Nat Rev Immunol. 16:7–21. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Mareninova OA, Sung KF, Hong P, Lugea A,
Pandol SJ, Gukovsky I and Gukovskaya AS: Cell death in
pancreatitis: Caspases protect from necrotizing pancreatitis. J
Biol Chem. 281:3370–3381. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Pop C and Salvesen GS: Human caspases:
Activation, specificity, and regulation. J Biol Chem.
284:21777–21781. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Leist M and Jäättelä M: Four deaths and a
funeral: From caspases to alternative mechanisms. Nat Rev Mol Cell
Biol. 2:589–598. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Shen J, Wan R, Hu G, Yang L, Xiong J, Wang
F, Shen J, He S, Guo X, Ni J, et al: miR-15b and miR-16 induce the
apoptosis of rat activated pancreatic stellate cells by targeting
Bcl-2 in vitro. Pancreatology. 12:91–99. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Sung KF, Odinokova IV, Mareninova OA,
Rakonczay Z Jr, Hegyi P, Pandol SJ, Gukovsky I and Gukovskaya AS:
Prosurvival Bcl-2 proteins stabilize pancreatic mitochondria and
protect against necrosis in experimental pancreatitis. Exp Cell
Res. 315:1975–1989. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Gomez G, Lee HM, He Q, Englander EW,
Uchida T and Greeley GH Jr: Acute pancreatitis signals activation
of apoptosis-associated and survival genes in mice. Exp Biol Med
(Maywood). 226:692–700. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Djukom C, Porro LJ, Mrazek A, Townsend CM
Jr, Hellmich MR and Chao C: Dual inhibition of PI3K and mTOR
signaling pathways decreases human pancreatic neuroendocrine tumor
metastatic progression. Pancreas. 43:88–92. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Briest F and Grabowski P:
PI3K-AKT-mTOR-signaling and beyond: The complex network in
gastroenteropancreatic neuroendocrine neoplasms. Theranostics.
4:336–365. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
François RA, Maeng K, Nawab A, Kaye FJ,
Hochwald SN and Zajac-Kaye M: Targeting focal adhesion kinase and
resistance to mTOR inhibition in pancreatic neuroendocrine tumors.
J Natl Cancer Inst. 107(pii): djv1232015. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Falletta S, Partelli S, Rubini C, Nann D,
Doria A, Marinoni I, Polenta V, Di Pasquale C, Degli Uberti E,
Perren A, et al: mTOR inhibitors response and mTOR pathway in
pancreatic neuroendocrine tumors. Endocr Relat Cancer. 23:883–891.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Vandamme T, Beyens M, de Beeck KO, Dogan
F, van Koetsveld PM, Pauwels P, Mortier G, Vangestel C, de Herder
W, Van Camp G, et al: Long-term acquired everolimus resistance in
pancreatic neuroendocrine tumours can be overcome with novel
PI3K-AKT-mTOR inhibitors. Br J Cancer. 114:650–658. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Zitzmann K, De Toni EN, Brand S, Göke B,
Meinecke J, Spöttl G, Meyer HH and Auernhammer CJ: The novel mTOR
inhibitor RAD001 (everolimus) induces antiproliferative effects in
human pancreatic neuroendocrine tumor cells. Neuroendocrinology.
85:54–60. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Adamo B, Deal AM, Burrows E, Geradts J,
Hamilton E, Blackwell KL, Livasy C, Fritchie K, Prat A, Harrell JC,
et al: Phosphatidylinositol 3-kinase pathway activation in breast
cancer brain metastases. Breast Cancer Res. 13:R1252011. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Johnson SM, Gulhati P, Rampy BA, Han Y,
Rychahou PG, Doan HQ, Weiss HL and Evers BM: Novel expression
patterns of PI3K/Akt/mTOR signaling pathway components in
colorectal cancer. J Am Coll Surg. 210:767–778. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
LoRusso PM: Inhibition of the
PI3K/AKT/mTOR pathway in solid tumors. J Clin Oncol. 34:3803–3815.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Rodon J, Dienstmann R, Serra V and
Tabernero J: Development of PI3K inhibitors: Lessons learned from
early clinical trials. Nat Rev Clin Oncol. 10:143–153. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Engelman JA: Targeting PI3K signalling in
cancer: Opportunities, challenges and limitations. Nat Rev Cancer.
9:550–562. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Cui LH, Li CX, Zhuo YZ, Yang L, Cui NQ and
Zhang SK: Saikosaponin d ameliorates pancreatic fibrosis by
inhibiting autophagy of pancreatic stellate cells via PI3K/Akt/mTOR
pathway. Chem Biol Interact. 300:18–26. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Hirota M, Shimosegawa T, Kitamura K,
Takeda K, Takeyama Y, Mayumi T, Ito T, Takenaka M, Iwasaki E,
Sawano H, et al: Continuous regional arterial infusion versus
intravenous administration of the protease inhibitor nafamostat
mesilate for predicted severe acute pancreatitis: A multicenter,
randomized, open-label, phase 2 trial. J Gastroenterol. Nov
22–2019.(Epub ahead of print).
|
|
63
|
Yong FJ, Mao XY, Deng LH, Zhang MM and Xia
Q: Continuous regional arterial infusion for the treatment of
severe acute pancreatitis: A meta-analysis. Hepatobiliary Pancreat
Dis Int. 14:10–17. 2015. View Article : Google Scholar : PubMed/NCBI
|