Introduction
Type 2 diabetes mellitus (T2DM) is a chronic,
systemic metabolic disease related to a variety of genetic and
environmental factors (1).
Glycolipid metabolism disorder is a consequence of T2DM (2). Normally, glycolipid metabolism is
maintained in a stable state to provide energy, but disorders of
glycolipid metabolism play a primary role in obesity and can
increase the risk of various diseases, such as T2DM and vascular
endothelial dysfunction, which are closely related to
cardiovascular diseases (3).
Additionally, endothelial dysfunction can accelerate the
pathological process of atherosclerosis, hypertension, T2DM and
cerebrovascular disease (4).
Lipoprotein levels are also disturbed or complicated by glycolipid
metabolism disorders, accompanied by a reduction in high-density
lipoprotein (HDL) levels and an increase in total cholesterol (TC),
triglyceride (TG) and low-density lipoprotein (LDL) levels
(5). Glycolipid metabolism
disorders lead to insulin resistance and hyperlipidemia in T2DM
mice (2). Hyperlipidemia is
classified as one of the major risk factors leading to
cardiovascular disease (6). In
recent years, the impact of proinsulin C-peptide has been
highlighted in the development of vascular disease. It plays an
important role in both type 1 DM and T2DM (7). A study among T2DM patients has shown
that with the progression of diabetic retinopathy, there are lower
levels of fasting and 2 h postprandial C-peptide compared with
healthy individuals (8). T2DM may
progress to a late stage due to pancreatic β-cell demise and
C-peptide deficiency (9).
Cluster of differentiation (CD)36, a member of the
scavenger receptor B (SRB) family, is the key transcription factor
responsible for fatty acid synthesis, lipid uptake and catabolism,
and is expressed predominantly by vascular cells (10). CD36 has increasingly been
considered as a possible biomarker for obesity, metabolic syndrome
and T2DM (11). CD36 protein
serves a role in lipid metabolism and insulin resistance, and the
expression of CD36 is inducible in obesity (12). Studies in CD36-deficient humans and
spontaneously hypertensive rats suggested that CD36 is responsible
for hyperlipidemia and insulin resistance (13,14).
Inhibition of vascular endothelial cell-specific CD36 directly
contributes to a reduction in lipid levels that correlates with
improvement in the lipid markers LDL-r and TG (15,16).
CD36 not only has been implicated in mediating lipid
internalization, but also can bind modified forms of LDL r and
increase excessive cholesterol accumulation in macrophages
(17). CD36 is the main cause of
atherosclerotic plaque formation induced by vascular lipid
deposition (18). However, the
mechanism whereby CD36 controls glycolipid metabolism associated
with T2DM remains to be elucidated.
Sterol regulatory element binding protein 2
(SREBP-2) is a main regulator that controls cholesterol
biosynthesis gene expression (19). CD36 can regulate SREBP-2 expression
and subsequently stimulate the transcription of various lipogenic
genes (20). It has been reported
that the SREBP cleavage-activating protein (SCAP)/SREBP2/LDL-r
pathway plays a crucial role in regulating lipid droplets in
numerous diseases (21). This
pathway regulates the transduction of a number of factors related
to insulin sensitivity and glycolipid metabolism (21). Lipid accumulation can be due to the
upregulation of SREBP2, its target gene LDL-r and its regulatory
gene scavenger receptor A(SRA), the subtype SRA1 (22) was examined in the present
study.
Epigallocatechin-3-gallate (EGCG) is a major
polyphenol found in green tea. Preclinical studies in animals, and
studies in cell line models and humans have reported the beneficial
effects of EGCG (23) on
obesity-related parameters, including decreases in body weight
(24–26), adipose mass (24), food intake (27) and total lipid, TC and TG levels in
the liver and plasma, and improvement of glucose homeostasis
(24,25,28).
Treatment of C57BL/6J mice with 0.32% dietary EGCG for 16 weeks has
been shown to reduce body weight gain and markers of T2DM induced
by a high-fat diet (HFD) (24).
EGCG reduces the reactive oxygen species content of the serum of
obese KK-ay mice, as well as that of 3T3-L1 adipose cells, whilst
also decreasing glucose levels and increasing glucose tolerance in
animals (29). Research has shown
beneficial effects of the anti-lipid deposition activity of EGCG,
and indicated that it may affect SREBP and CD36 in blood vessels
(30). Chen et al (31), found that EGCG reduced oxidized LDL
(ox-LDL) levels, decreased SRA expression (but not that of CD36),
and suppressed ox-LDL uptake and foam cell formation in human
macrophages in a dose-dependent manner. Furthermore, there are
other mechanisms involved in the effects of EGCG on endothelial
dysfunction. This includes prevention of oxidative injury in
cultured endothelial cell lines via the downregulation of
intercellular adhesion molecule 1 expression and 4-hydroxynonenal
accumulation, and restoration of nitrite/nitrate levels and nitric
oxide synthase 3 activity. EGCG can also protect endothelial cells
via the downregulation of transforming growth factor-β and the
Bax/Bcl-2/caspase 3 signaling pathway in the progression of
diabetic nephropathy in rats (32,33).
Therefore, the present study investigated the role
of EGCG in regulating a macrovascular glycolipid metabolic disorder
in T2DM, and the results may provide improved understanding of T2DM
and its mechanisms.
Materials and methods
Animals
A total of 67 C57BL6/J mice (male; 18–22 g; 4 weeks
old) were purchased from Beijing Vital River Laboratory Animal
Technology Co., Ltd. The mice were raised under controlled
temperature (23±1°C) and humidity (50±5%) conditions with a 12 h
light/dark cycle. The animals were allowed free access to drinking
water and food. The animals were acclimated to the housing
conditions for 7 days before the experiments. The health and
behavior of each group of mice were observed daily. All experiments
were approved by the Ethics Review Committee for Animal
Experimentation of the Institute of Clinical Pharmacology, Kunming
Medical University.
Materials
The levels of TC (cat. no. CS0005; Sigma-Aldrich;
Merck KGaA), TG (cat. no. MAK266; Sigma-Aldrich; Merck KGaA) and
LDL-r (cat. no. RAB0707; Sigma-Aldrich; Merck KGaA) were measured
using ELISA kits. An Oil Red O staining kit (cat. no. ab150678;
Abcam) was also employed. The primary antibodies were anti-β-actin
(cat. no. ab8227; 1:4,000; Abcam), anti-SRA1 (1:500; cat. no.
sc-166139; Santa Cruz Biotechnology, Inc.), anti-CD36 (1:3,500;
cat. no. ab133625; Abcam), anti-SREBP2 (1:3,000; cat. no. ab30682;
Abcam) and anti-LDL-r (1:4,000; cat. no. ab52818; Abcam). The
secondary antibodies used were Goat IgG horseradish peroxidase
(HRP)-conjugated antibody (1:2,000; cat. no. HAF017; R&D
Systems, Inc.) and Rabbit IgG HRP-conjugated antibody (1:2,000;
cat. no. HAF008; R&D Systems, Inc.).
Drugs
EGCG, a white powder with >95% purity, was
provided by the School of Pharmaceutical Sciences and Yunnan Key
Laboratory of Pharmacology for Natural Products, Kunming Medical
University. Pravastatin was obtained as a white power with >97%
purity from Sigma-Aldrich; Merck KGaA (cat. no. P4498).
Experimental design
Diabetes was induced in 4-week-old male C57BL/6J
mice as described previously (12). Male mice were fed a HFD containing
22% fat, 48% carbohydrates and 20% protein blended with standard
laboratory chow consisting of 5% fat, 53% carbohydrates and 23%
protein for 4 weeks. After the period of dietary manipulation,
animals were deprived of food for 12 h, and then the mice were
injected intraperitoneally with a low dose of streptozotocin (STZ;
45 mg/kg; cat. no. 572201; Sigma-Aldrich; Merck KGaA), which was
dissolved in 50 nm Na citrate buffer (pH 4.5). Thereafter, the
animals had free access to water and standard food (34,35).
After 72 h of STZ administration, fasting blood sugar and insulin
levels were measured with a reagent kit (cat. no. P006-1-1; Nanjing
Jiancheng Bioengineering Institute Co., Ltd.). Mice were deprived
for food for 6 h, and then fasting blood glucose levels were
assessed, blood was drawn from the tail and body weight was
measured weekly. Mice with fasting blood glucose ≥16.7 mmol/l were
considered diabetic (36). The
diabetic mice were randomly divided into 5 groups (n=12/group): A
diabetic model group, a pravastatin group (40 mg/kg body weight
administered daily) and 3 EGCG groups. A total of 20 mice had
succumbed to STZ toxicity during modeling (37) so they were euthanized after
reaching a humane endpoint, leaving only 8 in each diabetic model
group. This level of mortality was accounted for in the ethical
approval granted for this study. The health and behavior of each
group of mice were observed daily.
EGCG was suspended in a 0.5% sodium carboxymethyl
cellulose (CMC-Na) solution. Normal mice (n=7) and mice in the
diabetic model groups (n=8/group) received CMC-Na. EGCG-treated
diabetic mice received EGCG at 50, 100, or 200 mg/kg/day. All
substances were given by oral gavage once daily for 6 weeks. Mouse
weights were measured every 3 days. The duration of the animal
experiment was 10 weeks. The longer the diabetic model mice were
kept, the clearer their symptoms were (poor mental state,
inactivity, reduced activity capacity, dull hair, eating more and
urinating more), and the more evident their distress. The setting
of the sampling time point was based on the relevant literature of
EGCG (38,39), and according to our previous
preliminary experiments (data not shown), in order to ensure that
the effects of EGCG could be evaluated while minimizing the
distress of the experimental mice. All the procedures of the
experiments in the present study were designed to reduce the
suffering of experimental animals as much as possible in order to
guarantee the stability of experimental results. At the end of the
experiments, the animals were anesthetized with 1% sodium
pentobarbital (50 mg/kg) via intraperitoneal injection. Blood was
collected from the inferior vena cava into heparinized syringes,
followed by centrifugation (1,300 × g, 20 min, 4°C). The serum was
collected and stored in a deep freezer before analysis. Blood was
taken from the inferior vena cava under anesthesia, and the hearts
stopped beating and the mice succumbed after the blood was
collected. The total volume of blood obtained from each mouse was
0.6±0.2 ml/mouse. After the blood was collected, each mouse
experienced a 4–6% reduction in body weight. Additionally,
respiratory arrest and cardiac arrest were monitored for 30 min to
assess animal mortality. The abdominal aortas from each group were
also obtained. All samples were kept at −80°C for mRNA, protein and
oil red O staining analysis.
Insulin tolerance test (ITT)
After 10 weeks of EGCG treatment, mice underwent an
oral ITT (40). Mice were deprived
of food for 4 h, and the ITT was performed after intraperitoneal
injection of insulin (0.75 UI/kg). Blood glucose concentrations
were measured at 0 min, and then at 15, 30, 60, 90 and 120 min
after insulin injection using a portable Contour®
glucose monitor (Bayer AG) and test strips. The concentration of
insulin C-peptide in blood serum at 120 min was measured using a
mouse insulin C-peptide radioimmunoassay kit (cat. no. DIC P00;
R&D Systems, Inc.), according to the manufacturers
protocols.
Serum biochemical analysis
Serum was obtained from blood samples by
centrifugation (1,350 × g, 4°C, 10 min) and stored at 80°C. Serum
TG, TC and LDL-r levels were investigated with commercial assay
kits and an automated Mindray BS-200 biochemistry analyzer
instrument (Mindray Bio-Medical Electronics Co,. Ltd.).
Reverse transcription-quantitative
(RT-q)PCR
Total RNA was extracted from the tissue of each
abdominal aorta using TRIzol® (Thermo Fisher Scientific,
Inc.). cDNA was synthesized from RevertAid First Strand cDNA
Synthesis kit (cat. no. K1621; Thermo Fisher Scientific, Inc.)
according to the manufacturers instructions. RT-qPCR was performed
using SYBR Green PCR master mix (Applied Biosystems; Thermo Fisher
Scientific, Inc.). Thermocycling conditions included, initial
denaturation, 95°C for 10 min; followed by 40 cycles of 95°C for 5
sec and 60°C for 35 sec. The following primer sequences: CD36
forward, 5 CTGCTGTTCTTTGCCACGTC-3 and reverse, 5
CTGCTGTTCTTTGCCACGTC-3; SRA1 forward, 5 CCCCAGGTTCTTCACTACGCC-3 and
reverse, 5 TCCTTATCCTGGGAGCCCTT-3; SREBP2 forward, 5
AGCATACCGCAAGGTGTTCC-3 and reverse, 5 CCAGGTGTCTACTTCTCCGTGT-3;
LDL-r forward, 5 CAGCGTATCTGTGGCTGACA-3 and reverse, 5
AGTGTCGACTTCTCTAGGCT-3; β-actin forward, 5 GGCTGTGCTATCCCTGTACG-3
and reverse, 5 TTGATCTTCATTGTGCTGGGTG-3. Expression was analyzed
with the 2−∆∆Cq method (41) and gene expression was presented as
expression relative to that of the reference gene β-actin.
Oil red O staining
Fresh-frozen optimal cutting temperature
compound-embedded tissue sections were stained after 8-µm slices
were obtained on a cryostat. The slides were placed in propylene
glycol for 2 min and then incubated in oil red O solution for 6 min
at room temperature. A mixture of 85% propylene glycol in distilled
water was prepared, and the tissue sections were incubated in this
mixture for 1 min at room temperature. The slides were rinsed in 2
changes of distilled water and then thoroughly rinsed in tap water
at room temperature. For oil red O quantification, the slides were
dried, and 250 µl of isopropanol was added, followed by incubation
for 3 min at room temperature; the eluted solution was read at 510
nm using a Varioskan LUX multimode microplate reader (Thermo Fisher
Scientific, Inc.).
Western blot analysis
Protein from all frozen abdominal aorta samples was
extracted with 1 ml of RIPA buffer (150 mM sodium chloride 1.0%
NP40 or Triton X-100 Tris, pH 8.0). Protease and phosphatase
inhibitor cocktails (cat. no. 78439; Thermo Fisher Scientific,
Inc.) were added to the homogenization buffer. The concentration of
protein in the supernatant of each sample was determined by using a
Pierce™ Bradford assay kit (cat. no. 23200; Thermo Fisher
Scientific, Inc.). The protein was then loaded using loading dye
(40 µg protein/well) and separated in 8–12% SDS-PAGE gels. PVDF
membranes were blocked with 0.5% BSA (cat. no. 17879-45-7;
Guidechem), washed and incubated with the primary antibodies
(1:1,000) described in the Materials section at 4°C overnight. The
membranes were then blotted with the corresponding secondary
antibody (1:2,000; cat. nos. HAF017 and HAF008; R&D Systems,
Inc.) at room temperature for 1 h, and antigen-antibody
interactions were detected by using Pierce ECL reagents (Thermo
Fisher Scientific, Inc.) and quantified using a C-DiGit blot
scanner (LI-COR Biosciences) and in-built Image Studio DiGit
software (Flow max 2.82). Protein expression was presented as
expression relative to that of the reference protein β-actin.
Statistical analysis
Statistical analyses were performed using GraphPad
Prism version 5.0 (GraphPad Software, Inc.) and P<0.05 was
considered to indicate a statistically significant difference.
Students t-test was used to compare the two groups. One-way ANOVA
followed by Tukeys post hoc test or repeated measures ANOVA was
used to determine the significance of the differences between
groups. The data are presented as the means ± standard error of the
means unless otherwise stated.
Results
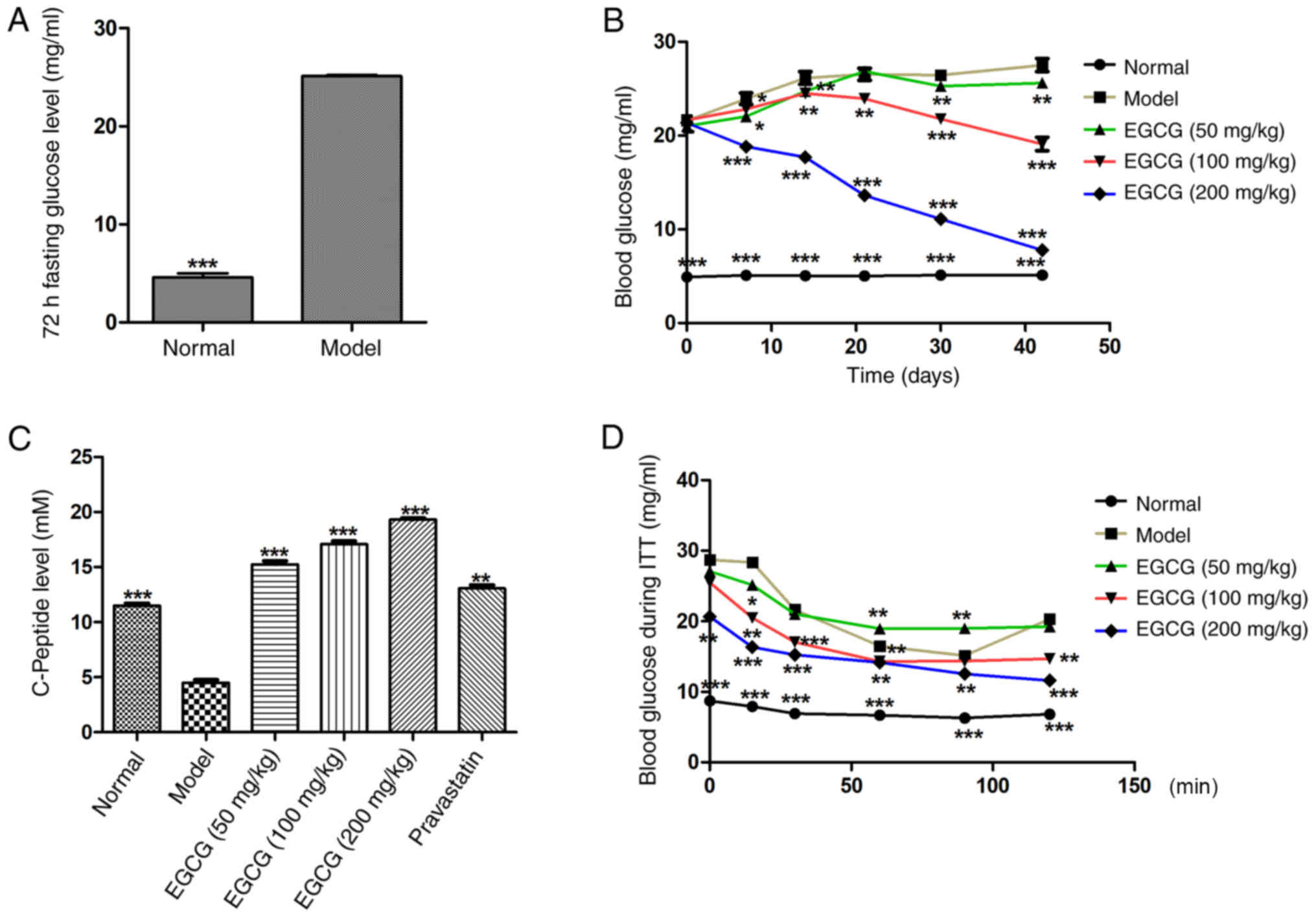
EGCG increases insulin sensitivity and
decreases blood sugar levels in T2DM mice
To investigate whether EGCG reversed insulin
resistance and blood sugar in T2DM mice, EGCG was administered to
T2DM mice for 6 weeks; fasting blood glucose was measured and ITTs
were performed. It was found that 72 h fasting blood glucose
(normal 5.12±0.29 mg/ml vs. model 25.01±1.22 mg/ml; P<0.001;
Fig. 1A) was significantly
increased in the model group after treatment with EGCG for 6 weeks.
Blood glucose in the EGCG (200 mg/kg) group was significantly lower
than in the model group at each tested time point (P<0.01; Fig
1B), and the decrease occurred in a dose-dependent manner [glucose
in the model group (26.17±1.53 mg/ml) vs. the EGCG (200 mg/kg)
group (7.76±1.09 mg/ml)]. The results demonstrated that EGCG could
decrease glucose levels in T2DM mice in a dose-dependent manner
(Fig. 1B).
The response to extrinsic insulin in
the mice was investigated by an ITT
The results demonstrated that C-peptide levels in
the EGCG group were significantly higher than in the model group at
the 120-min time point (P<0.001; Fig. 1C), and this increase occurred in a
dose-dependent manner. The blood glucose levels at the 120 min
after insulin injection in the EGCG (100 and 200 mg/kg) group were
significantly lower than in the model group (P<0.001; Fig. 1D). The results demonstrated that
EGCG could decrease insulin resistance and ameliorate insulin
sensitivity in T2DM mice.
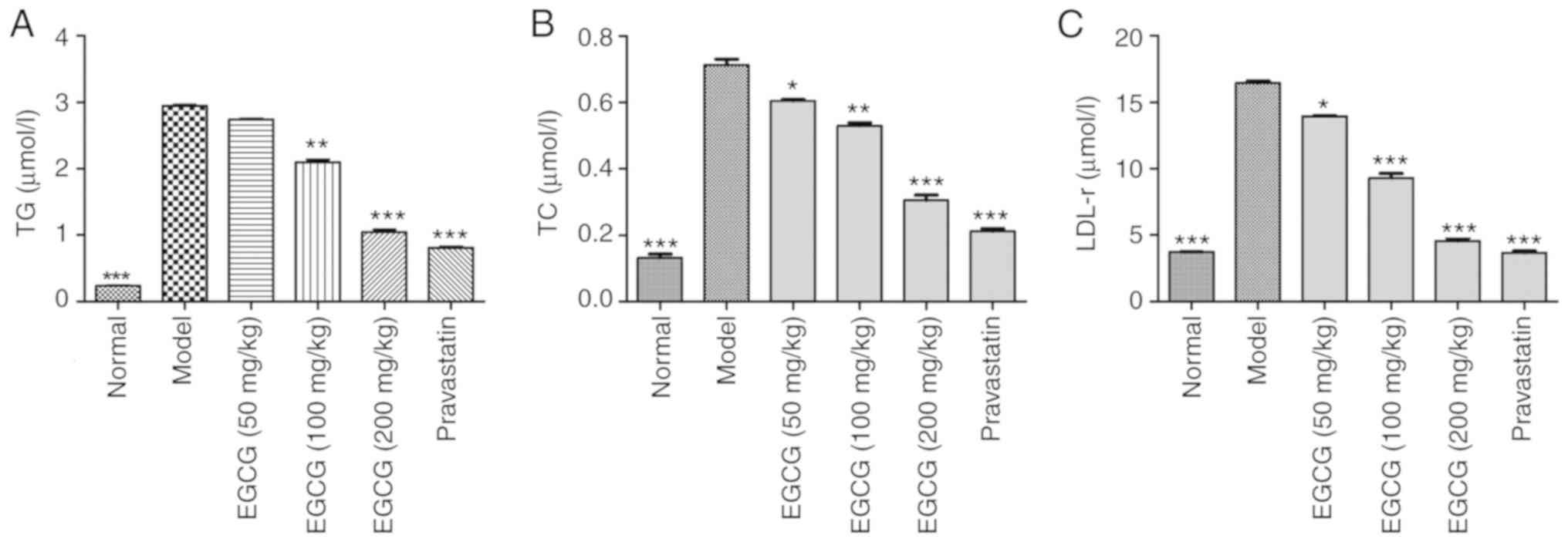
EGCG decreases the contents of TG, TC
and LDL-r in T2DM mice
STZ-induced diabetic mice exhibited significantly
increased blood serum levels of TG, TC and LDL r compared with
normal mice (P<0.001). EGCG (100, 200 mg/kg) decreased serum
levels of TG, TC and LDL-r, as did pravastatin (P<0.05; Fig. 2A-C).
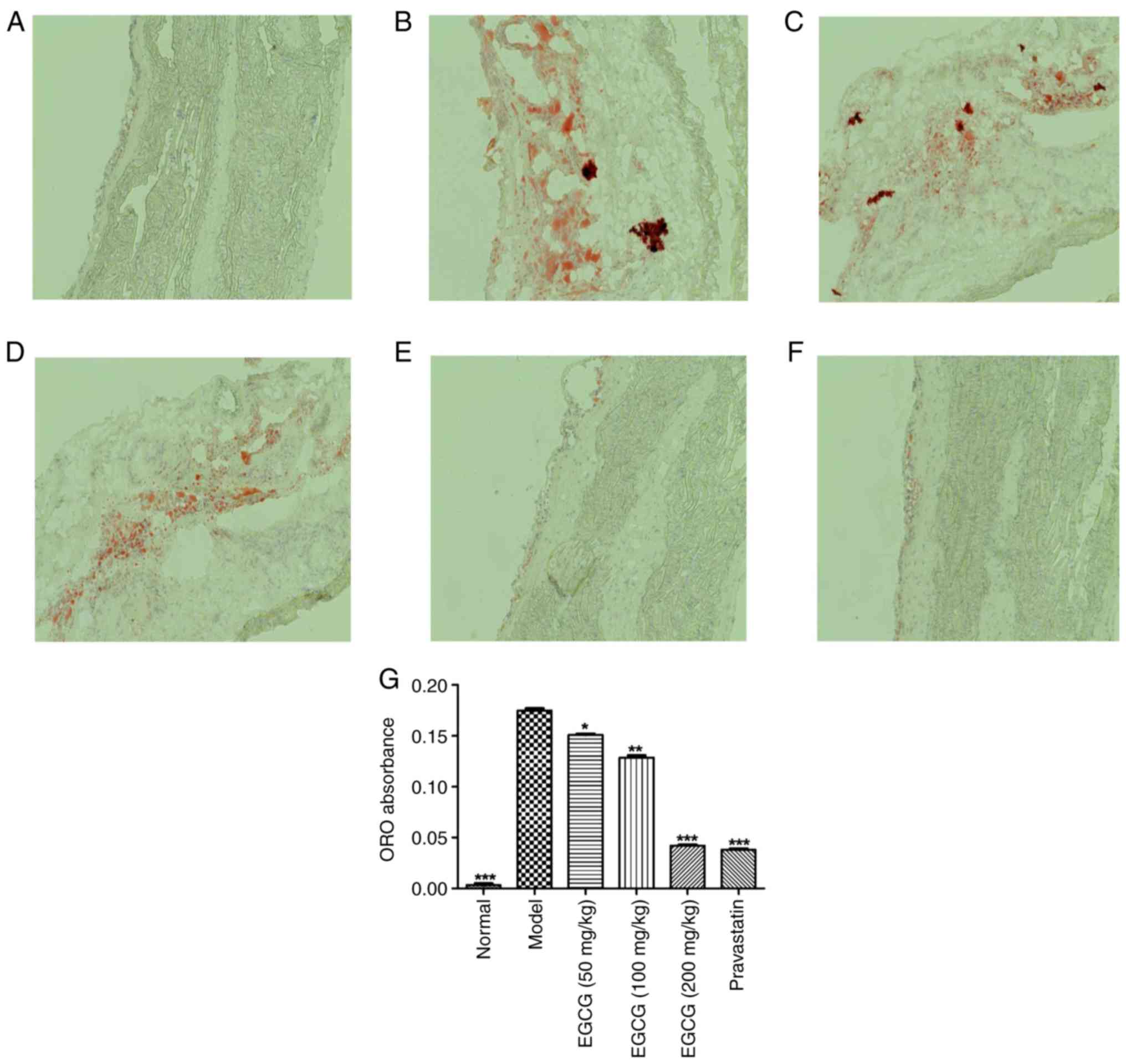
EGCG controls lipid deposition in the
blood vessels of T2DM mice
The effects of EGCG on lipid deposition in blood
vessels were investigated, as shown in Fig. 3. The lipid droplets in the blood
vessels of the model group were irregular and larger, and they were
significantly greater in number than those observed in the normal
group (P<0.001). EGCG (200 mg/kg) decreased the number of lipid
droplets to a similar extent as pravastatin (P>0.05).
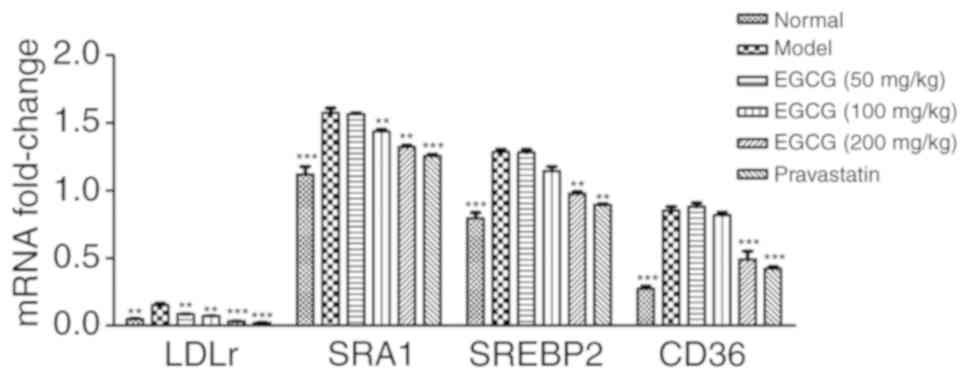
EGCG reduces the gene expression of
SRA1, CD36, SREBP2 and LDL-r in the blood vessels of T2DM mice
All mRNA products of all tested genes were within
normal values (Cq=16-30). The levels of the loading control and
β-actin were constant in all tested samples. Significant increases
in the relative mRNA expression of SRA1, CD36, SREBP2 and LDL-r
were observed in the blood vessel samples obtained from STZ-induced
mice compared with the normal mice. However, the EGCG group
exhibited reduced gene expression of SRA1, CD36, SREBP2 and LDL r
in blood vessels compared with the model group (P<0.01 or
P<0.001; Fig. 4).
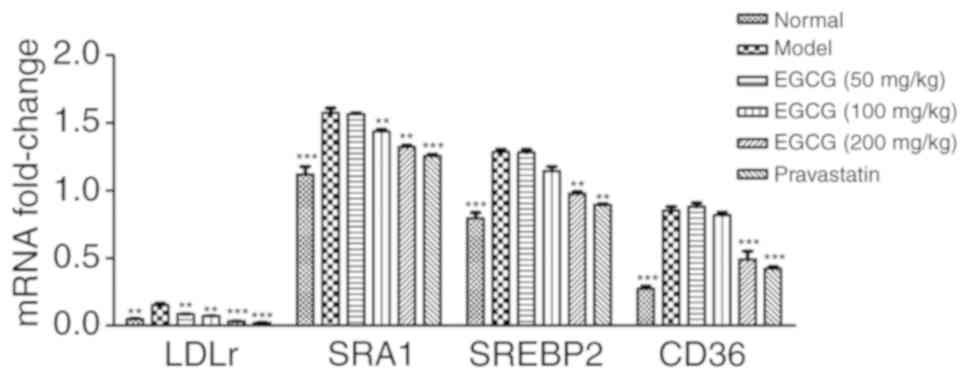 | Figure 4.Relative mRNA expression of SRA1,
SREBP2, LDL-r and CD36 in the blood vessels of STZ-induced treated
mice. Significant increases in mRNA relative expression of SRA1 and
CD36, SREBP2 and LDL-r were observed in the blood vessels from
STZ-induced treated mice, compared with the normal mice. However,
EGCG (100 mg/kg, 200 mg/kg) was able to reduce the gene expression
of SRA1 and CD36, SREBP2 and LDL-r in blood vessels. Comparisons
were assessed with one-way ANOVA followed by Tukey's post hoc test.
**P<0.01, ***P<0.001 vs. model group. SRA, scavenger receptor
A; CD, cluster of differentiation; SREBP2, sterol regulatory
element binding protein 2; LDL-r, low-density lipoprotein receptor;
STZ, streptozotocin; EGCG, epigallocatechin-3-gallate. |
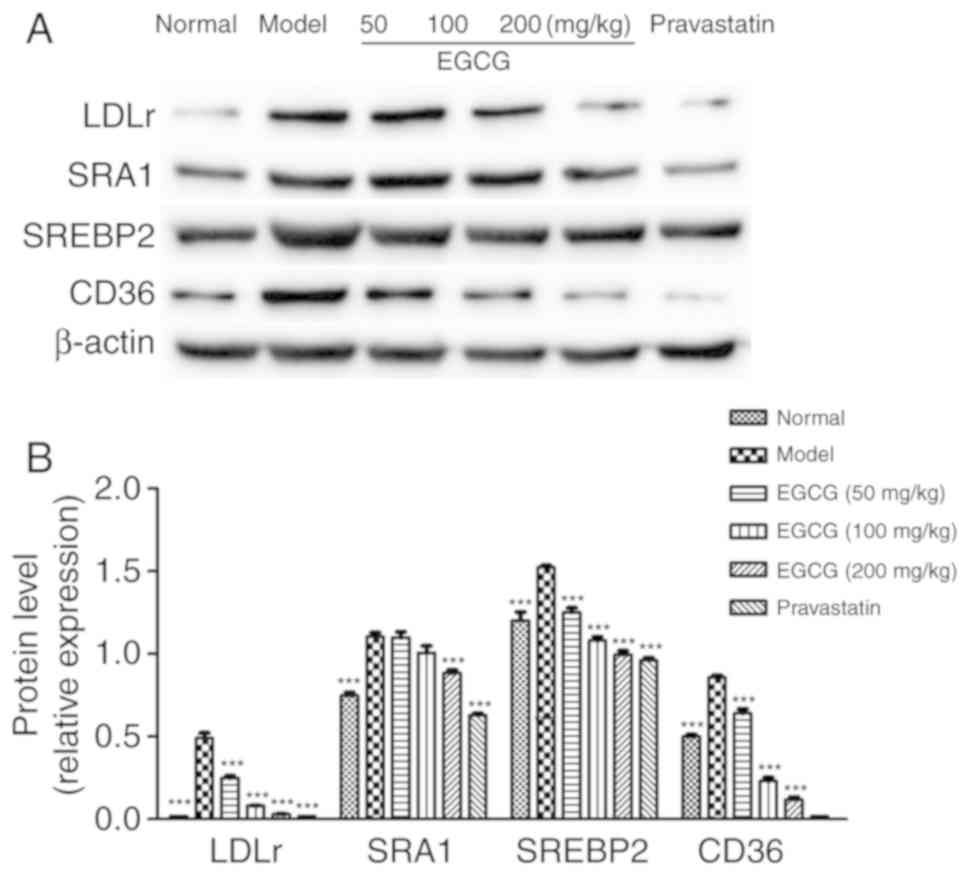
EGCG inhibits the expression of SRA1,
CD36, SREBP2, and LDL-r in diabetic mice
As shown in Fig. 5,
the protein levels of SRA1, SREBP2 and LDL-r were increased in the
diabetic mice compared with the normal group (P<0.001). EGCG
reduced the expression of SRA1 (P<0.05), CD36 (P<0.001),
SREBP2 (P<0.001) and LDL-r (P<0.001) in a dose-dependent
manner; EGCG downregulated the levels of SREBP2 and CD36 in a
similar manner to pravastatin (P>0.05).
Discussion
Lipid metabolic dysfunction is associated with the
development and progression of high-mortality diseases, including
T2DM, as well as the subsequent associated cardiovascular and
cerebrovascular pathologies (42).
Lipoprotein levels are also disturbed or complicated by lipid
metabolism disorders, accompanied by a reduction in HDL levels, and
an increase in TC, TG and LDL-r levels (43). The present study identified that
the levels of TC, TG and LDL were increased in HFD and STZ-induced
T2DM mice. The serum TC, TG and LDL levels of the T2DM group were
significantly higher compared with the normal group, showing that a
hyperlipidemia T2DM mouse model had been successfully established.
A previous clinical trial revealed that the serum levels of TG and
LDL-r are significantly higher in T2DM patients with vascular
lesions compared with T2DM patients without such complications
(44). The HFD and STZ-induced
diabetic mice also demonstrated dyslipidemia, as evidenced by
elevated levels of TC, LDL-r and TG, with a concomitant decrease in
HDL, as observed in human T2DM (45), which was consistent with the
findings of the present study. Additionally, decreased expression
of LDL-r and TG can reduce lipid accumulation in vascular lesions
(46). To observe this effect,
lipid deposition in the vascular endothelium was measured by oil
red O staining, and it was found that the lipid droplets in the
blood vessels of the T2DM group were irregular and larger compared
with those observed in the normal group.
The present study observed increased levels of TG
and LDL-r in the serum of HFD/STZ-induced T2DM mice, as well as
large amounts of lipid droplets deposited in vascular endothelial
cells. The model mice treated with HFD/STZ had the same genetic
background as the normal mice. This model involved the combination
of HFD feeding to induce hyperlipidemia, hyperinsulinemia and
glucose intolerance, and subsequent treatment with STZ (47–49),
which resulted in a reduction in the number of functional β-cells.
HFD/STZ-induced mice are designed to mimic the pathology of T2DM
but on a shorter time scale than in humans. As pravastatin is not
soluble in water, a suspension was made in 0.5% CMC-Na. In order to
achieve solvent consistency, 0.5% CMC-Na was also used to dissolve
the EGCG. CMC-Na is recognized as a solvent without any effect in
pharmacological research.
In recent years, drugs used for the treatment of
patients with T2DM, such as rosiglitazone and metformin, have been
found to induce various side effects; in addition, they are unable
to prevent angiopathy (50). Due
to the lack of effective and applicable pharmacological treatments
for T2DM with hyperlipidemia and related vascular lesion
dysfunctions, an increasing number of researchers are now studying
traditional medicines. The investigation of the therapeutic
functions of traditional medicinal herbs in T2DM presents promising
potential.
TC, TG and LDL-r are the main markers of T2DM with
angiopathy; a previous study indicated that they directly increase
the risk of hyperlipidemia (51).
To investigate the protective mechanisms of EGCG, the expression of
TC, TG and LDL-r in serum was tested. The results demonstrated that
compared with the T2DM group, the EGCG treatment (200 mg/kg) group
exhibited marked reductions in serum TC, TG and LDL levels.
C-peptide is not affected by exogenous insulin, nor is it degraded
by the liver (52). It can
directly reflect the secretion of endogenous insulin and the
function of islet β-cells (52).
The ITT results of the present study demonstrated that EGCG (100
and 200 mg/kg) reduced blood glucose levels and promoted C-peptide
levels. These results indicated that EGCG ameliorated the degree of
fatty degeneration in vascular endothelial cells and modulated the
expression levels of lipid metabolism genes in a dose-dependent
manner.
To further confirm the protective mechanism of EGCG
against vascular endothelial cell injury caused by lipid metabolism
disorder in HFD and STZ-induced T2DM mice, gene and protein
expression levels in vascular endothelial cells were detected. It
was found that EGCG downregulated the expression of CD36 in a
dose-dependent manner. CD36 has been found to act as a scavenger
receptor for ox-LDL and as a cellular transporter of long-chain
fatty acids (53), and it is
expressed on diverse cell types, including adipocytes, cardiac and
skeletal myocytes, retinal pigment epithelial cells, platelets,
mononuclear phagocytes and the microvascular endothelium (54). In addition, a CD36 inhibitor can be
used to lower lipid levels and reduce cholesterol accumulation
in vivo (55).
Yang et al (56), identified enriched genes through
Gene Ontology enrichment analyses. These genes were mainly related
to biological processes such as steroid metabolism and lipid
metabolism; their results indicated that CD36, SCAP, SREBP2 and
LDL-r gene expression in the arterial endothelium may be a target
of the lipid-reducing action of EGCG, which is consistent with the
results of the present study. CD36 is a type of SRB, and scavenger
receptor genes are closely related to lipid deposition in vascular
endothelial cells and hyperlipidemia. The present study identified
that the expression of CD36 was higher in the model group compared
with the normal group at the mRNA level and the protein level, and
that CD36 upregulated the expression of SREBP2 in the T2DM group.
The oil red O staining revealed that the lipid droplets in the
blood vessels of mice in the EGCG groups were fewer in number and
smaller compared with the model group, particularly in the 200
mg/kg group. In addition, EGCG inhibited the expression of CD36,
downregulated the expression of SREBP2 and decreased LDL-r
levels.
At present, EGCG is widely used in research. A
number of trials of patients with clinical tumors have proved that
EGCG is safe and reliable, and oral administration is the main
method of drug administration. For example, no adverse reactions
were found following 1-year oral EGCG (300 mg/day) in patients with
highly differentiated prostate cancer (57). In the study on the safety of EGCG
supplementation in postmenopausal women at high risk for breast
cancer, only a few subjects who took 1,315 mg/day of green tea
extract (with an EGCG content of 843 mg) experienced mild,
transient adverse reactions (58).
The adverse reactions of EGCG were found to be mild in the dose
expansion test of patients with estrogen receptor-negative breast
cancer, and the main adverse reactions included nausea, heartburn,
abdominal pain, headache, dizziness and myalgia (59). In stage III non-small cell lung
cancer treated with radiation and chemotherapy, and patients with
breast cancer with neoadjuvant radiotherapy, giving EGCG was
reported to be safe, and EGCG prevented radiation and chemotherapy
injury, playing a positive role in promoting tissue repair
(60,61). These clinical trials of EGCG have
shown its low toxicity and wide margin of safety.
Overall, the present study demonstrated that CD36 is
a treatment target of EGCG in T2DM mice. EGCG downregulated glucose
levels and upregulated C-peptide levels in T2DM mice, which may be
associated with the protection of β-cell in the pancreas. In
addition, EGCG ameliorates lipid metabolism disorders, perhaps by
regulating the SREBP2/SCAP/LDL-r pathway, which is an effective way
to control serum cholesterol synthesis levels. It was hypothesized
that EGCG could regulate lipid metabolism in T2DM mice through
CD36/SRA1/SREBP2/LDL-r pathways, and then reduce blood lipid
deposition. Together, the results of the present work suggested
that EGCG might be a promising natural hypoglycemic product for the
prevention and treatment of lipid regulation disorders and the
protection of vascular endothelial cells from lipid injury.
Acknowledgements
Not applicable.
Funding
The present study was supported by grants from
Yunnan Applied Basic Research Projects-Joint Special Project [grant
no. 2018FE001(−210)] and Yunnan Provincial Education Department
Project (grant nos. 2017ZDX157 and 2020J0151).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors contributions
ZR and HY conceived and designed the study. ZR, ZY,
YL and RZ performed the experiments. ZY, YL, RZ and HY analyzed the
data. ZR, ZY and HY wrote the manuscript. ZR and HY reviewed and
edited the manuscript. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The animal experiments were approved by the Animals
Ethics Committee of Kunming Medical University and the Guide for
the Care and Use of Laboratory Animals.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Tanaka S, Tanaka S, Iimuro S, Yamashita H,
Katayama S, Ohashi Y, Akanuma Y, Yamada N and Sone H; Japan
Diabetes Complications Study Group, : Cohort profile: The Japan
diabetes complications study: a long-term follow-up of a randomised
lifestyle intervention study of type 2 diabetes. Int J Epidemiol.
43:1054–1062. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Perry RJ, Samuel VT, Petersen KF and
Shulman GI; RJ P, : The role of hepatic lipids in hepatic insulin
resistance and type 2 diabetes. Nature. 510:84–91. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Turner RC, Millns H, Neil HA, Stratton IM,
Manley SE, Matthews DR and Holman RR: Risk factors for coronary
artery disease in non-insulin dependent diabetes mellitus: United
Kingdom Prospective Diabetes Study (UKPDS: 23). BMJ. 316:823–828.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Shin NR, Lee JC, Lee HY, Kim MS, Whon TW,
Lee MS and Bae JW: An increase in the Akkermansia spp. population
induced by metformin treatment improves glucose homeostasis in
diet-induced obese mice. Gut. 63:727–735. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Torimoto K, Okada Y and Tanaka Y: Type 2
diabetes and vascular endothelial dysfunction. J UOEH. 40:65–75.
2018.(In Japanese). View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Smith SA: Peroxisome
proliferator-activated receptors and the regulation of mammalian
lipid metabolism. Biochem Soc Trans. 30:1086–1090. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wang L, Lin P, Ma A, Zheng H, Wang K, Li
W, Wang C, Zhao R, Liang K, Liu F, et al: C-Peptide is
independently associated with an increased risk of coronary artery
disease in T2DM subjects: A cross-sectional study. PLoS One.
10:e01271122015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Cai X, Han X, Zhang S, Luo Y, Chen Y and
Ji L: Age at diagnosis and C-peptide level are associated with
diabetic retinopathy in Chinese. PLoS One. 9:e911742014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Massi-Benedetti M and Orsini-Federici M:
Treatment of type 2 diabetes with combined therapy: what are the
pros and cons? Diabetes Care. 31:S131–135. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Febbraio M, Hajjar DP and Silverstein RL:
CD36: A class B scavenger receptor involved in angiogenesis,
atherosclerosis, inflammation, and lipid metabolism. J Clin Invest.
108:785–791. 2001. View
Article : Google Scholar : PubMed/NCBI
|
|
11
|
Susztak K, Ciccone E, McCue P, Sharma K
and Böttinger EP: Multiple metabolic hits converge on CD36 as novel
mediator of tubular epithelial apoptosis in diabetic nephropathy.
PLoS Med. 2:e452005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gautam S, Pirabu L, Agrawal CG and
Banerjee M: CD36 gene variants and their association with type 2
diabetes in an Indian population. Diabetes Technol Ther.
15:680–687. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pravenec M, Landa V, Zidek V, Musilova A,
Kren V, Kazdova L, Aitman TJ, Glazier AM, Ibrahimi A, Abumrad NA,
et al: Transgenic rescue of defective Cd36 ameliorates insulin
resistance in spontaneously hypertensive rats. Nat Genet.
27:156–158. 2001. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Miyaoka K, Kuwasako T, Hirano K, Nozaki S,
Yamashita S and Matsuzawa Y: CD36 deficiency associated with
insulin resistance. Lancet. 357:686–687. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Febbraio M, Abumrad NA, Hajjar DP, Sharma
K, Cheng W, Pearce SF and Silverstein RL: A null mutation in murine
CD36 reveals an important role in fatty acid and lipoprotein
metabolism. J Biol Chem. 274:19055–19062. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Martin CA, Longman E, Wooding C, Hoosdally
SJ, Ali S, Aitman TJ, Gutmann DAP, Freemont PS, Byrne B and Linton
KJ: Cd36, a class B scavenger receptor, functions as a monomer to
bind acetylated and oxidized low-density lipoproteins. Protein Sci.
16:2531–2541. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Park YM: CD36, a scavenger receptor
implicated in atherosclerosis. Exp Mol Med. 46:e992014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Trent CM, Yu S, Hu Y, Skoller N, Huggins
LA, Homma S and Goldberg IJ: Lipoprotein lipase activity is
required for cardiac lipid droplet production. J Lipid Res.
55:645–658. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Moslehi A and Hamidi-zad Z: Role of SREBPs
in liver diseases: A mini-review. J Clin Transl Hepatol.
28:332–338. 2018.
|
|
20
|
Qi Q, Liang L, Doria A, Hu FB and Qi L:
Genetic predisposition to dyslipidemia and type 2 diabetes risk in
two prospective cohorts. Diabetes. 61:745–752. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Lee EJ, Oh H, Kang BG, Kang MK, Kim DY,
Kim YH, Lee JY, Ji JG, Lim SS and Kang YH: Lipid-lowering effects
of medium-chain triglyceride-enriched coconut oil in combination
with licorice extracts in experimental hyperlipidemic mice. J Agric
Food Chem. 66:10447–10457. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Mysliwiec P, Choromanska B, Winnicka MM,
Kaminski K, Mysliwiec H, Dadan J, Supruniuk E and Chabowski A:
Interleukin-6 deficiency modifies the effect of high fat diet on
myocardial expression of fatty acid transporters and myocardial
lipids. J Physiol Pharmacol. 69:692018.
|
|
23
|
Yoon JY, Kwon HH, Min SU, Thiboutot DM and
Suh DH: Epigallocatechin-3-gallate improves acne in humans by
modulating intracellular molecular targets and inhibiting P. acnes.
J Invest Dermatol. 133:429–440. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Song X, Du J, Zhao W and Guo Z:
Epigallocatechin-3-gallate(EGCG): Mechanisms and the combined
applications. Comb Chem High Throughput Screen.
doi:10.2174/1386207321666171218115850.
|
|
25
|
Xiao J, Ho CT, Liong EC, Nanji AA, Leung
TM, Lau TY, Fung ML and Tipoe GL: Epigallocatechin gallate
attenuates fibrosis, oxidative stress, and inflammation in
non-alcoholic fatty liver disease rat model through TGF/SMAD, PI3
K/Akt/FoxO1, and NF-kappa B pathways. Eur J Nutr. 53:187–199. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Annaba F, Kumar P, Dudeja AK, Saksena S,
Gill RK and Alrefai WA: Green tea catechin EGCG inhibits ileal
apical sodium bile acid transporter ASBT. Am J Physiol Gastrointest
Liver Physiol. 298:G467–G473. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhou P, Yu JF, Zhao CG, Sui FX, Teng X and
Wu YB: Therapeutic potential of EGCG on acute renal damage in a rat
model of obstructive nephropathy. Mol Med Rep. 7:1096–1102. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Farabegoli F, Papi A and Orlandi M:
(−)-Epigallocatechin-3-gallate down-regulates EGFR, MMP-2, MMP-9
and EMMPRIN and inhibits the invasion of MCF-7 tamoxifen-resistant
cells. Biosci Rep. 31:99–108. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Yan J, Zhao Y, Suo S, Liu Y and Zhao B:
Green tea catechins ameliorate adipose insulin resistance by
improving oxidative stress. Free Radic Biol Med. 52:1648–1657.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Baselga-Escudero L, Blade C, Ribas-Latre
A, Casanova E, Suárez M, Torres JL, Salvadó MJ, Arola L and
Arola-Arnal A: Resveratrol and EGCG bind directly and distinctively
to miR-33a and miR-122 and modulate divergently their levels in
hepatic cells. Nucleic Acids Res. 42:882–892. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Chen SJ, Kao YH, Jing L, Chuang YP, Wu WL,
Liu ST, Huang SM, Lai JH, Ho LJ, Tsai MC, et al:
Epigallocatechin-3-gallate reduces scavenger receptor A expression
and foam cell formation in human macrophages. J Agric Food Chem.
65:3141–3150. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chang HH, Chien CY, Chen KH, Huang SC and
Chien CT: Catechins blunt the effects of oxLDL and its primary
metabolite phosphatidylcholine hydroperoxide on endothelial
dysfunction through inhibition of oxidative stress and restoration
of eNOS in rats. Kidney Blood Press Res. 42:919–932. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Mohan T, Velusamy P, Chakrapani LN,
Srinivasan AK, Singh A, Johnson T and Periandavan K: Impact of EGCG
supplementation on the progression of diabetic nephropathy in rats:
An insight into fibrosis and apoptosis. J Agric Food Chem.
65:8028–8036. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Zhang M, Lv XY, Li J, Xu ZG and Chen L:
The characterization of high-fat diet and multiple low-dose
streptozotocin induced type 2 diabetes rat model. J Diabetes Res.
2008:7040452008.
|
|
35
|
Qian C, Zhu C, Yu W, Jiang X and Zhang F:
High-fat diet/low-dose streptozotocin-induced type 2 diabetes in
rats impacts osteogenesis and wnt signaling in bone marrow stromal
cells. PLoS One. 10:e01363902015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Algandaby MM, Alghamdi HA, Ashour OM,
Abdel-Naim AB, Ghareib SA, Abdel-Sattar EA and Hajar AS: Mechanisms
of the antihyperglycemic activity of Retama raetam in
streptozotocin-induced diabetic rats. Food Chem Toxicol.
48:2448–2453. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Estil·les E, Téllez N, Nacher M and
Montanya E: A model for human islet transplantation to
immunodeficient streptozotocin-induced diabetic mice. Cell
Transplant. 27:1684–1691. 2018. View Article : Google Scholar :
|
|
38
|
Grove KA, Sae-tan S, Kennett MJ and
Lambert JD: (−)-Epigallocatechin-3-gallate inhibits pancreatic
lipase and reduces body weight gain in high fat-fed obese mice.
Obesity (Silver Spring). 20:2311–2313. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Uchiyama Y, Suzuki T, Mochizuki K and Goda
T: Dietary supplementation with a low dose of
(−)-epigallocatechin-3-gallate reduces pro-inflammatory responses
in peripheral leukocytes of non-obese type 2 diabetic GK rats. J
Nutr Sci Vitaminol (Tokyo). 59:541–547. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Zhang YY, Li C, Yao GF, Du LJ, Liu Y,
Zheng XJ, Yan S, Sun JY, Liu Y, Liu MZ, et al: Deletion of
macrophage mineralocorticoid receptor protects hepatic steatosis
and insulin resistance through ERα/HGF/Met pathway. Diabetes.
66:1535–1547. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Δ Δ C(T)) Method. Methods. 25:402–408. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Parhofer KG: The treatment of disorders of
lipid metabolism. Dtsch Arztebl Int. 113:261–268. 2016.PubMed/NCBI
|
|
43
|
Luo J, Yang H and Song BL: Mechanisms and
regulation of cholesterol homeostasis. Nat Rev Mol Cell Biol.
doi:10.1038/s41580-019-0190-7.
|
|
44
|
Ruiz-Ojeda FJ, Anguita-Ruiz A, Rupérez AI,
Gomez-Llorente C, Olza J, Vázquez-Cobela R, Gil-Campos M, Bueno G,
Leis R, Cañete R, et al: Effects of X-chromosome tenomodulin
genetic variants on obesity in a childrens cohort and implications
of the gene in adipocyte metabolism. Sci Rep. 9:39792019.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Ahangari N, Ghayour Mobarhan M, Sahebkar A
and Pasdar A: Molecular aspects of hypercholesterolemia treatment:
Current perspectives and hopes. Ann Med. 50:303–311. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Hammad RH, El-Madbouly AA, Kotb HG and
Zarad MS: Frequency of circulating B1a and B2 B-cell subsets in
Egyptian patients with type 2 diabetes mellitus. Egypt J Immunol.
25:71–80. 2018.PubMed/NCBI
|
|
47
|
Rajesh M, Mukhopadhyay P, Bátkai S, Patel
V, Saito K, Matsumoto S, Kashiwaya Y, Horváth B, Mukhopadhyay B,
Becker L, et al: Cannabidiol attenuates cardiac dysfunction,
oxidative stress, fibrosis, and inflammatory and cell death
signaling pathways in diabetic cardiomyopathy. J Am Coll Cardiol.
56:2115–2125. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Zhang Z, Wang S, Zhou S, Yan X, Wang Y,
Chen J, Mellen N, Kong M, Gu J, Tan Y, et al: Sulforaphane prevents
the development of cardiomyopathy in type 2 diabetic mice probably
by reversing oxidative stress-induced inhibition of LKB1/AMPK
pathway. J Mol Cell Cardiol. 77:42–52. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Kurlawalla-Martinez C, Stiles B, Wang Y,
Devaskar SU, Kahn BB and Wu H: Insulin hypersensitivity and
resistance to streptozotocin-induced diabetes in mice lacking PTEN
in adipose tissue. Mol Cell Biol. 25:2498–2510. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Su N, Zhao N, Wang G, Wang L, Zhang Y, Li
R, Liu Y, Yang X, Li C and Hou M: The effects of adiponectin and
adiponectin receptor 1 levels on macrovascular complications among
patients with type 2 diabetes mellitus. Cell Physiol Biochem.
52:225–231. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Wang J, He K, Yang C, Lin X, Zhang X, Wang
Y, Liu G and Xian X: Dietary cholesterol is highly associated with
severity of hyperlipidemia and atherosclerotic lesions in
heterozygous LDLR-deficient hamsters. Int J Mol Sci. 20:202019.
|
|
52
|
Walcher D, Marx N, D W and N M: Advanced
glycation end products and C-peptide-modulators in diabetic
vasculopathy and atherogenesis. Semin Immunopathol. 31:103–111.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Chien KL, Hsu HC, Liu PH, Lin HJ and Chen
MF: Common sequence variants in CD36 gene and the levels of
triglyceride and high-density lipoprotein cholesterol among ethnic
Chinese in Taiwan. Lipids Health Dis. 11:1742012. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Maréchal L Maximilien Laviolette M,
Rodrigue-Way A, Sow B, Brochu M, Caron V and Tremblay A: The
CD36-PPARγ pathway in metabolic disorders. Int J Mol Sci.
19:15292018. View Article : Google Scholar :
|
|
55
|
Farook VS, Puppala S, Schneider J, Fowler
SP, Chittoor G, Dyer TD, Allayee H, Cole SA, Arya R, Black MH, et
al: Metabolic syndrome is linked to chromosome 7q21 and associated
with genetic variants in CD36 and GNAT3 in Mexican Americans.
Obesity (Silver Spring). 20:2083–2092. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Yang D, Hu C, Deng X, Bai Y, Cao H, Guo J
and Su Z: Therapeutic effect of chitooligosaccharide tablets on
lipids in high-fat diets induced hyperlipidemic rats. Molecules.
24:242019.
|
|
57
|
Kumar NB, Pow-Sang J, Spiess PE, Park J,
Salup R, Williams CR, Parnes H and Schell MJ: Randomized,
placebo-controlled trial evaluating the safety of one-year
administration of green tea catechins. Oncotarget. 7:70794–70802.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Dostal AM, Samavat H, Bedell S, Torkelson
C, Wang R, Swenson K, Le C, Wu AH, Ursin G, Yuan J-M and Kurzer MS:
The safety of green tea extract supplementation in postmenopausal
women at risk for breast cancer: Results of the Minnesota green tea
trial. Food Chem Toxicol. 83:26–35. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Crew KD, Brown P, Greenlee H, Bevers TB,
Arun B, Hudis C, McArthur HL, Chang J, Rimawi M, Vornik L, et al:
Phase IB randomized, double-blinded, placebo-controlled, dose
escalation study of polyphenon E in women with hormone
receptor-negative breast cancer. Cancer Prev Res (Phila).
5:1144–1154. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Zhu W, Jia L, Chen G, Zhao H, Sun X, Meng
X, Zhao X, Xing L, Yu J and Zheng M: Epigallocatechin-3-gallate
ameliorates radiation-induced acute skin damage in breast cancer
patients undergoing adjuvant radiotherapy. Oncotarget.
7:48607–48613. 2016.PubMed/NCBI
|
|
61
|
Zhao H, Zhu W, Xie P, Li H, Zhang X, Sun
X, Yu J and Xing L: A phase I study of concurrent chemotherapy and
thoracic radiotherapy with oral epigallocatechin-3-gallate
protection in patients with locally advanced stage III
non-small-cell lung cancer. Radiother Oncol. 110:132–136. 2014.
View Article : Google Scholar : PubMed/NCBI
|