Introduction
Diabetes mellitus is a disease associated with
numerous complications (1).
Hyperglycemia affects patients with diabetes by damaging macro- and
microvessels, thus resulting in retinopathy, neuropathy and
nephropathy, and cardiovascular, cerebrovascular and other serious
complications (2,3). Although multiple mechanisms cause
diabetic complications, growing evidence has suggested that
immoderate aggregation of advanced glycation end products (AGEs)
may be a causative factor (4).
Excessive AGEs activate and interact with the receptor for AGEs
(RAGE), leading to the activation of inflammatory factors (5,6).
FPS-ZM1 is a specific and high-affinity inhibitor of RAGE (7). Numerous studies have reported that
FPS-ZM1 exerts an anti-inflammatory effect on various cells, and on
human periodontal ligament fibroblasts and human gingival
fibroblasts (8–10). These findings suggested a promising
application of FPS-ZM1 in preventing periodontal diseases. However,
further studies are required to explore its application and
importance in the medical field.
It has been reported that expression of RAGE is high
in gingival fibroblasts, periodontal ligament fibroblasts and
periodontal ligament stem cells in a high glucose (HG) environment
(11). Under HG conditions,
various inflammatory factors, including but not limited to IL-1β,
high mobility group box-1, IL-6, intercellular adhesion molecule-1
and TNF-α, can be activated through the combination of RAGE and
AGEs (12,13). These inflammatory cytokines have
been demonstrated to cause inflammation in periodontal tissues,
including the alveolar bone and surrounding soft tissues (14,15).
As observed previously, IL-6, IL-1β and TNF-α largely accumulate in
the periodontal tissues of patients with diabetes (16). Bone marrow mesenchymal stem cells
(BMSCs) are present in the alveolar bone and possess
multi-directional differentiation potential; these cells have an
essential role in bone formation (17). It has previously been reported that
the release of inflammatory cytokines promotes the proliferation of
BMSCs in a HG environment, thus suggesting its application in the
pathological process of periodontal diseases (18). Therefore, this study aimed to
assess how HG activates inflammatory cytokines in BMSCs.
Several intracellular signaling pathways involved in
the activation of inflammatory cytokines are currently being
studied. Notably, to the best of our knowledge, the
infection-associated proinflammatory function of NF-κB is the most
widely studied (19). The
thioredoxin-interacting protein (TXNIP)/nucleotide-binding
oligomerization domain-like receptor protein 3 (NLRP3) inflammasome
pathway has been reported to be associated with diabetes-associated
inflammation (20). The NLRP3
inflammasome has been well studied and is comprised of three
components: NLRP3 protein, apoptosis-related speck-like protein
containing CARD (ASC) and caspase-1 (21). The NLRP3 inflammasome can detect
danger signals, known as danger-associated molecular patterns
(22). NLRP3 agonists can activate
caspase-1, which in turn releases the proinflammatory cytokines
IL-18 and IL-1β (23,24). The role of the NLRP3 inflammasome
has been demonstrated in the pathogenic process of various diseases
including, but not limited to, Alzheimer's disease, osteoarthritis
and type 2 diabetes (25–27).
However, few studies have described the mechanism
through which the NLRP3 inflammasome is activated. Functionally,
TXNIP dissociates from thioredoxin (TRX), combines directly with
NLRP3 and activates it (28). In
addition, recent studies have demonstrated that TXNIP is
upregulated in diabetes-related inflammation (20,29).
In patients with diabetes, hyperglycemia has been suggested to
stimulate the expression of TXNIP (30). Therefore, it may be hypothesized
that HG activates the NLRP3 inflammasome by promoting TXNIP
expression.
The aim of the present study was to assess the
expression of RAGE in BMSCs under HG stimulation, and to
investigate the expression of related inflammatory cytokines and
the potential molecular mechanisms in response to a RAGE-specific
inhibitor. Consequently, the feasibility of using RAGE as a target
for drug therapy to prevent periodontal inflammation and promote
the healing process of bone tissue injury in patients with diabetes
was considered.
Materials and methods
Cell culture
BeNa Culture Collection; Beijing Beina Chunglian
Biotechnology Research Institute provided the rat BMSCs. Cells were
cultured under normal glucose (NG; 5 mM) or HG (25 mM) conditions
in DMEM (HyClone; Cytiva) supplemented with 10% FBS (Gibco; Thermo
Fisher Scientific, Inc.) and 1% penicillin-streptomycin solution
(Beyotime Institute of Biotechnology). Cells were cultured in a
humidified atmosphere containing 5% CO2 at 37°C. Through
the cell viability assay, an optimal concentration of FPS-ZM1 (500
nM; Beyotime Institute of Biotechnology) was selected to treat the
cells, with or without HG stimulation for 48 h. The TXNIP inhibitor
resveratrol (Res; 50 µmol/l; Beyotime Institute of Biotechnology)
was used to inhibit the TXNIP/NLRP3 pathway. Cells were stimulated
with Res for 2 h at 37°C in the dark and were then incubated under
HG conditions for 48 h. BMSCs were cultured to 4–7 generations for
subsequent experiments.
Cell viability assay
Cell viability was determined using the Cell
Counting Kit (CCK)-8 assay (Dojindo Molecular Technologies, Inc.).
Firstly, cells were seeded in a 96-well plate at a density of
5×103 cells/well. The cells were grown to ~90%
confluence and were then co-cultured with various concentrations of
FPS-ZM1 (0, 250, 500 or 750 nM) and HG (25 mM) at 37°C.
Subsequently, the viability of the cultured cells was detected
after 24, 48 or 72 h. The original medium was removed and 100 µl
serum-free DMEM containing 10 µl CCK-8 solution was added to each
well. Cells were subsequently incubated for 2 h at 37°C with 5%
CO2. Finally, a Varioskan Flash microplate reader
(Thermo Fisher Scientific, Inc.) was used to detect the absorbance
value at 450 nm. The mean absorbance values of the control group
obtained from the three different time-points were set as 100%.
Experiments were conducted three times.
RNA isolation and reverse
transcription-quantitative PCR (RT-qPCR)
The expression of specific genes (NLRP3, ASC,
caspase-1, TXNIP and TRX) were quantitatively assessed by RT-qPCR.
RNA was isolated from cultured BMSCs using TRIzol®
reagent (Invitrogen; Thermo Fisher Scientific, Inc.). Subsequently,
RT of total RNA into cDNA was conducted using the Prime Script RT
reagent kit (Takara Bio, Inc.), according to the manufacturer's
protocol. SYBR FAST qPCR Master Mix (Kapa Biosystems; Roche
Diagnostics) and a CFX-Connect 96 RT-qPCR system (Bio-Rad
Laboratories, Inc.) were used to carry out the amplification of
target genes. The PCR protocol was as follows: 95°C for 3 min,
followed by 40 cycles at 95°C for 5 sec and 56°C for 10 sec, and a
final extension step at 72°C for 25 sec. The mRNA levels of the
specific genes were normalized to β-actin and expressed as a ratio
to the internal reference. The primer sequences used for PCR are
listed in Table I. The relative
mRNA expression levels were calculated using the 2−ΔΔCq
method and are presented as calculated values (31).
 | Table I.Primer sequences used for reverse
transcription-quantitative PCR. |
Table I.
Primer sequences used for reverse
transcription-quantitative PCR.
| Gene | Primer sequence
(5′-3′) |
|---|
| NLRP3 |
F-CATCTTAGTCCTGCCAA |
|
|
R-CAACAGACGCTACACCC |
| ASC |
F-AGCATCCAGCAAACCA |
|
|
R-GGACCCCATAGACCTCA |
| Caspase-1 |
F-TTGAAGAGCAGAAAGCA |
|
|
R-CAGTAGGAAACTCCGAAG |
| TXNIP |
F-CAAGGTAAGTGTGCCG |
|
|
R-GATTCTGTGAAGGTGATGA |
| TRX |
F-CCAACCTTTTGACCCTTT |
|
|
R-CCCTTCTTTCATTCCCTC |
| β-actin |
F-TAGGAGCCAGGGCAGTA |
|
|
R-CGTTGACATCCGTAAAGAC |
ELISA
Cell supernatants were obtained by centrifugation
(1,000 × g; room temperature; 10 min) after treatment at 48 h and
stored at −80°C for follow-up experiments. Activation of
inflammatory factors was quantified using rat IL-1β (cat. no.
RLB00), TNF-α (cat. no. RTA00) and IL-6 (cat. no. R6000B) ELISA
kits (all R&D Systems, Inc.), according to the manufacturer's
protocols. Experiments were carried out three times.
Protein isolation and western blot
analysis
The expression levels of specific proteins (NLRP3,
ASC, caspase-1, TXNIP, TRX and RAGE) were detected by western
blotting. Proteins were extracted from cultured BMSCs using RIPA
buffer (Thermo Fisher Scientific, Inc.) at 4°C and total protein
was boiled at 95°C for 10 min and centrifuged at room temperature
at 12,000 × g for 10 min. The bicinchoninic acid protein assay kit
(Beijing Solarbio Science & Technology, Co., Ltd.) was used for
protein quantification. Protein samples (20 µg) were separated by
12% SDS-PAGE (Sigma-Aldrich; Merck KGaA) and were blotted onto
polyvinylidene fluoride membranes (EMD Millipore). The membranes
were then blocked in 5% skim milk in PBS-0.05% Tween-20 at room
temperature for 1 h. The membranes were then incubated with primary
antibodies against RAGE (rabbit; 1:1,000; cat. no. PAB32996), NLRP3
(rabbit; 1:2,000; cat. no. PAB37930), ASC (rabbit; 1:1,000; cat.
no. PAB30696), caspase-1 (rabbit; 1:1,000; cat. no. PAB36756),
TXNIP (rabbit; 1:1,000; cat. no. PAB43948), TRX (rabbit; 1:1,000;
cat. no. PAB32168) and β-actin (rabbit; 1:1,000; cat. no. PAB36265)
(all Bioswamp) at 4°C overnight. β-actin was used as the loading
control. Subsequently, membranes were incubated with horseradish
peroxidase-conjugated goat anti-rabbit antibodies (1:20,000; cat.
no. SAB43714; Bioswamp) for 1 h at room temperature. An enhanced
chemiluminescence kit (Analytik Jena AG) was used to measure
reactivity, and the target bands were detected, and protein
expression was semi-quantified using TANON GIS 4.2 software (Tanon
Science & Technology Co., Ltd.). The detected protein
expression levels were normalized to those of β-actin.
Statistical analysis
All data obtained from three experimental repeats
are presented as the mean ± standard deviation, and statistical
analyses were conducted using SPSS 19.0 software (IBM Corp.).
One-way analysis of variance was used for multiple group
comparisons, and Tukey's post hoc test was used for intergroup
comparisons. P<0.05 was considered to indicate a statistically
significant difference.
Results
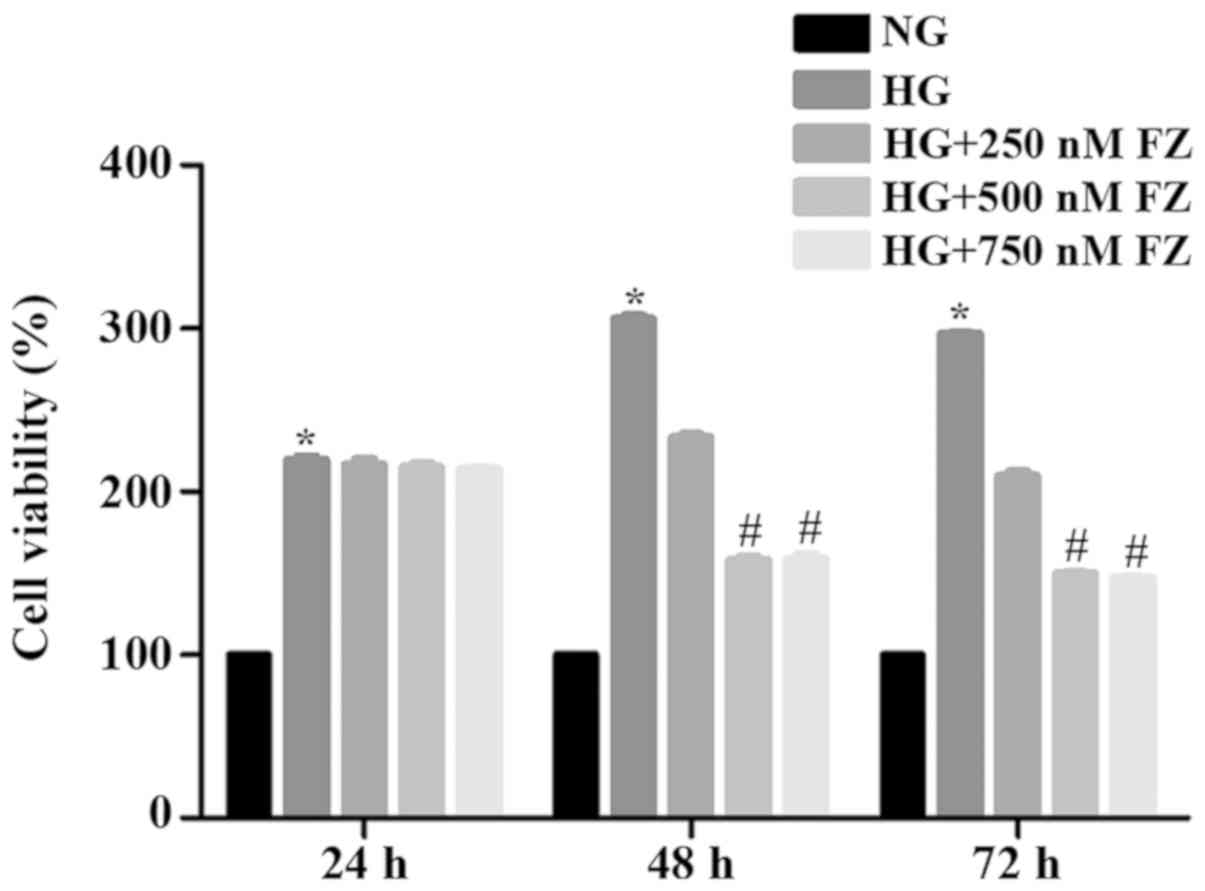
FPS-ZM1 inhibits HG-induced cell
viability
To verify suitable time-points and the optimal
concentration of FPS-ZM1 for follow-up experiments, BMSCs were
treated with FPS-ZM1 (0, 250, 500 and 750 nM) for 24, 48 and 72 h.
Alterations in BMSC viability are presented in Fig. 1. Compared with in the NG group, HG
stimulation significantly enhanced the viability of BMSCs at all
selected time points (P<0.05). Notably, no significant
alterations in BMSC viability were detected following treatment
with 250, 500 or 750 nM FPS-ZM1 for 24 h. Conversely, treatment
with 500 and 750 nM FPS-ZM1 for 48 or 72 h significantly alleviated
HG-induced cell viability compared with the HG group (P<0.05).
No significant differences in viability were observed between cells
treated with 500 or 750 nM FPS-ZM1 for 48 and 72 h (P>0.05).
These results indicated that HG may promote the viability of BMSCs
at 48 h, but this effect may gradually decrease as the culture time
increases.
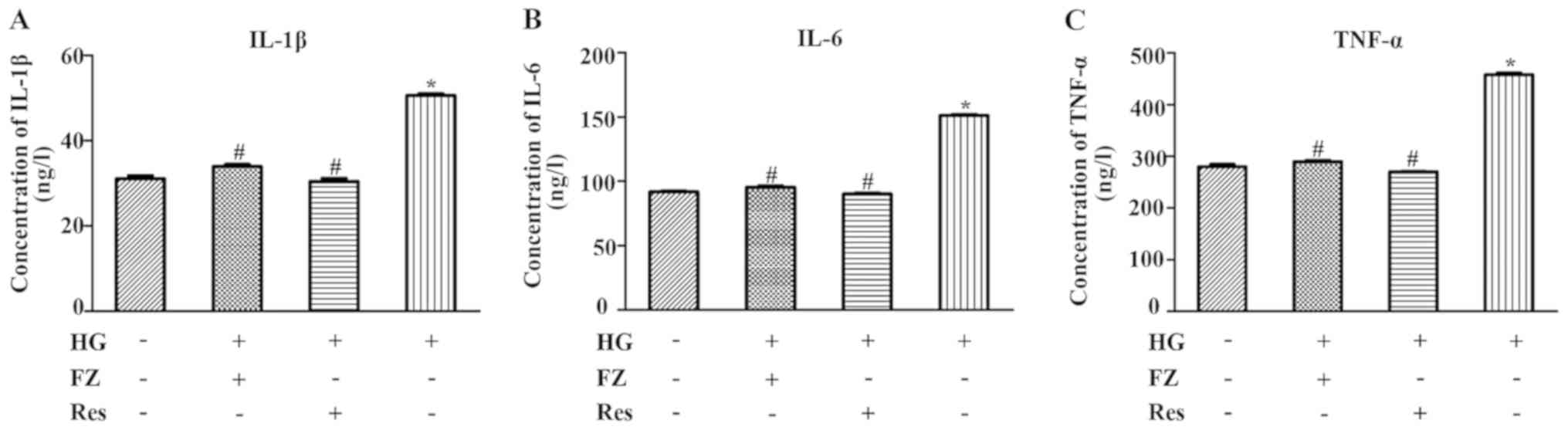
FPS-ZM1 alleviates HG-induced
inflammatory factor activation in BMSCs
ELISA kits were used to detect the levels of IL-6,
TNF-α and IL-1β in BMSCs under different treatments. The impact of
FPS-ZM1 on HG-induced intracellular inflammation was also assessed.
As presented in Fig. 2, the
concentrations of TNF-α, IL-1β and IL-6 were elevated under HG
conditions compared with in the NG group (P<0.05). However,
FPS-ZM1 significantly reduced the effects of HG on inflammatory
marker levels (P<0.05). Similarly, the concentrations of TNF-α,
IL-1β and IL-6 were decreased in BMSCs after pretreatment with Res
(P<0.05).
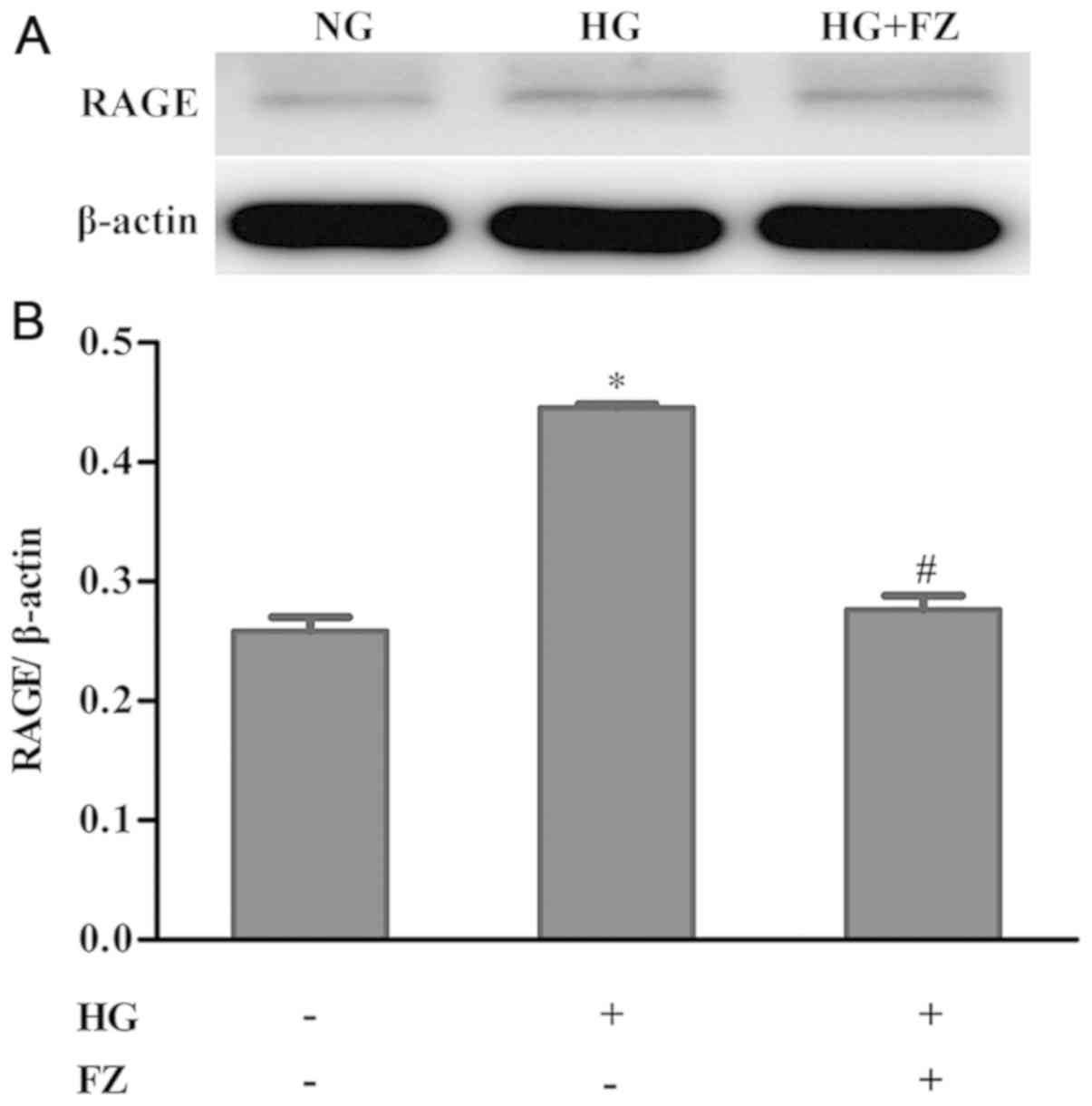
FPS-ZM1 inhibits RAGE expression in
HG-induced BMSCs
To explore the impact of FPS-ZM1 on RAGE expression
in BMSCs under HG conditions, western blotting was used to assess
the protein expression of RAGE. RAGE expression was increased in
BMSCs under HG conditions, whereas treatment with FPS-ZM1 inhibited
the increase in RAGE expression in HG-induced BMSCs (P<0.05)
(Fig. 3).
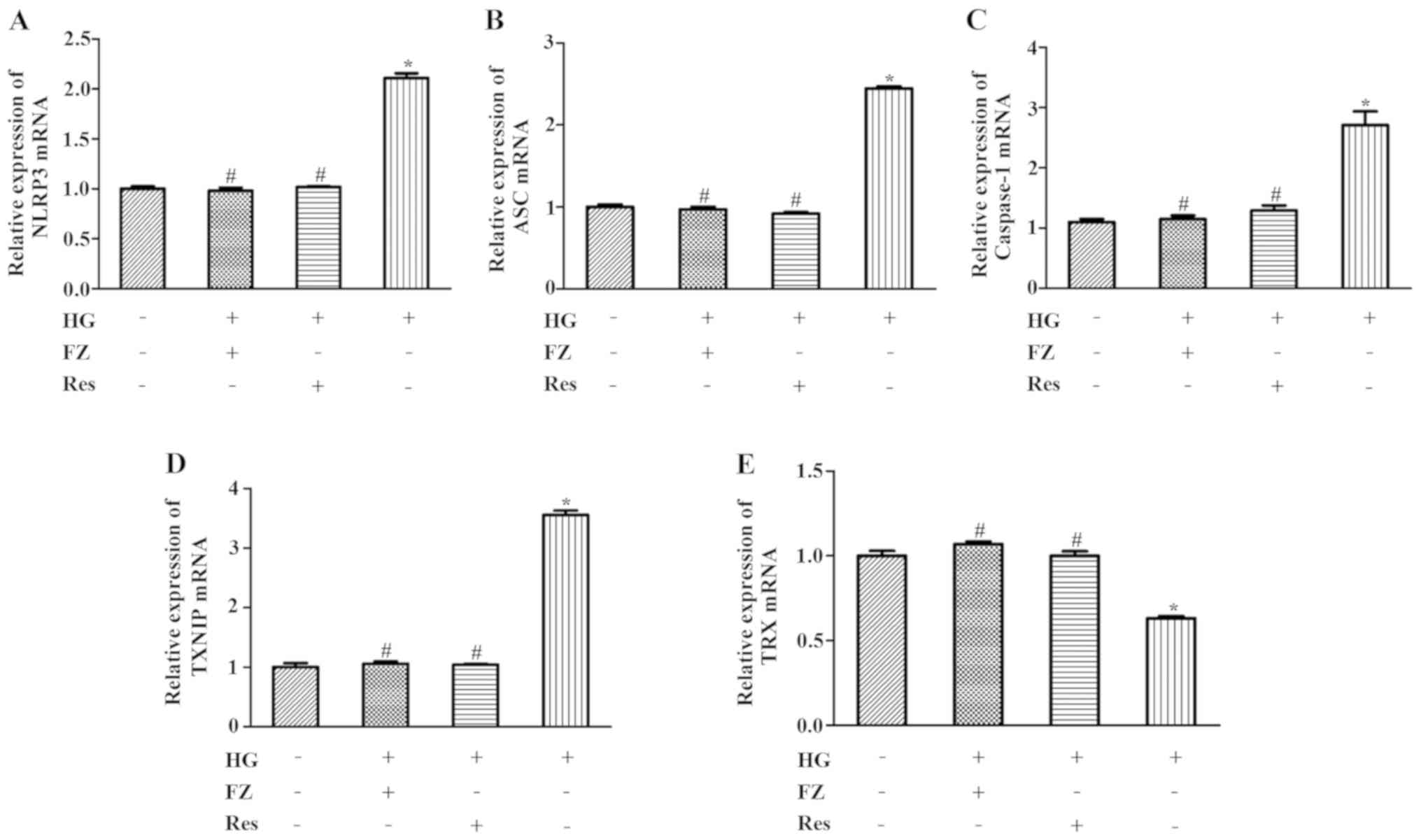
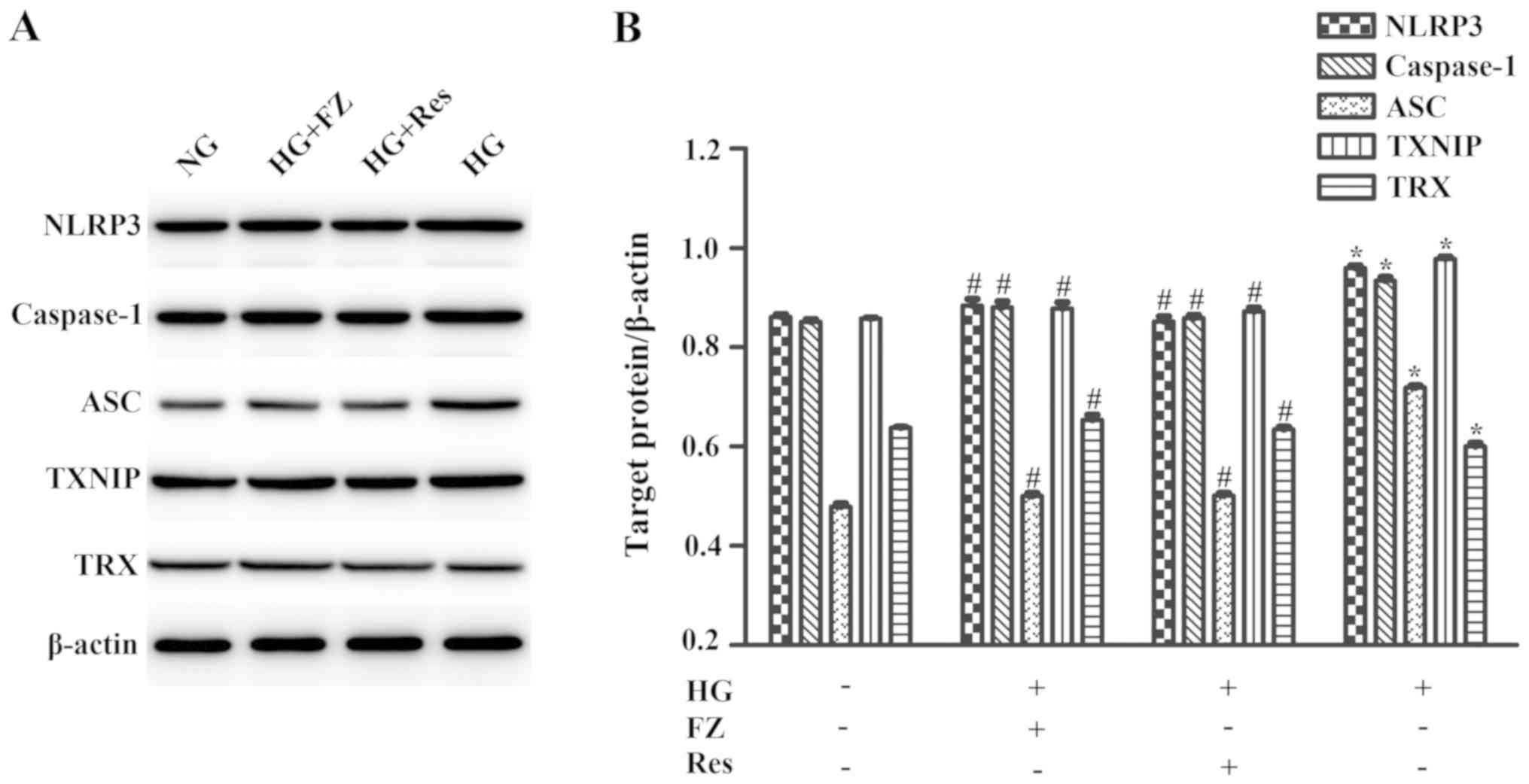
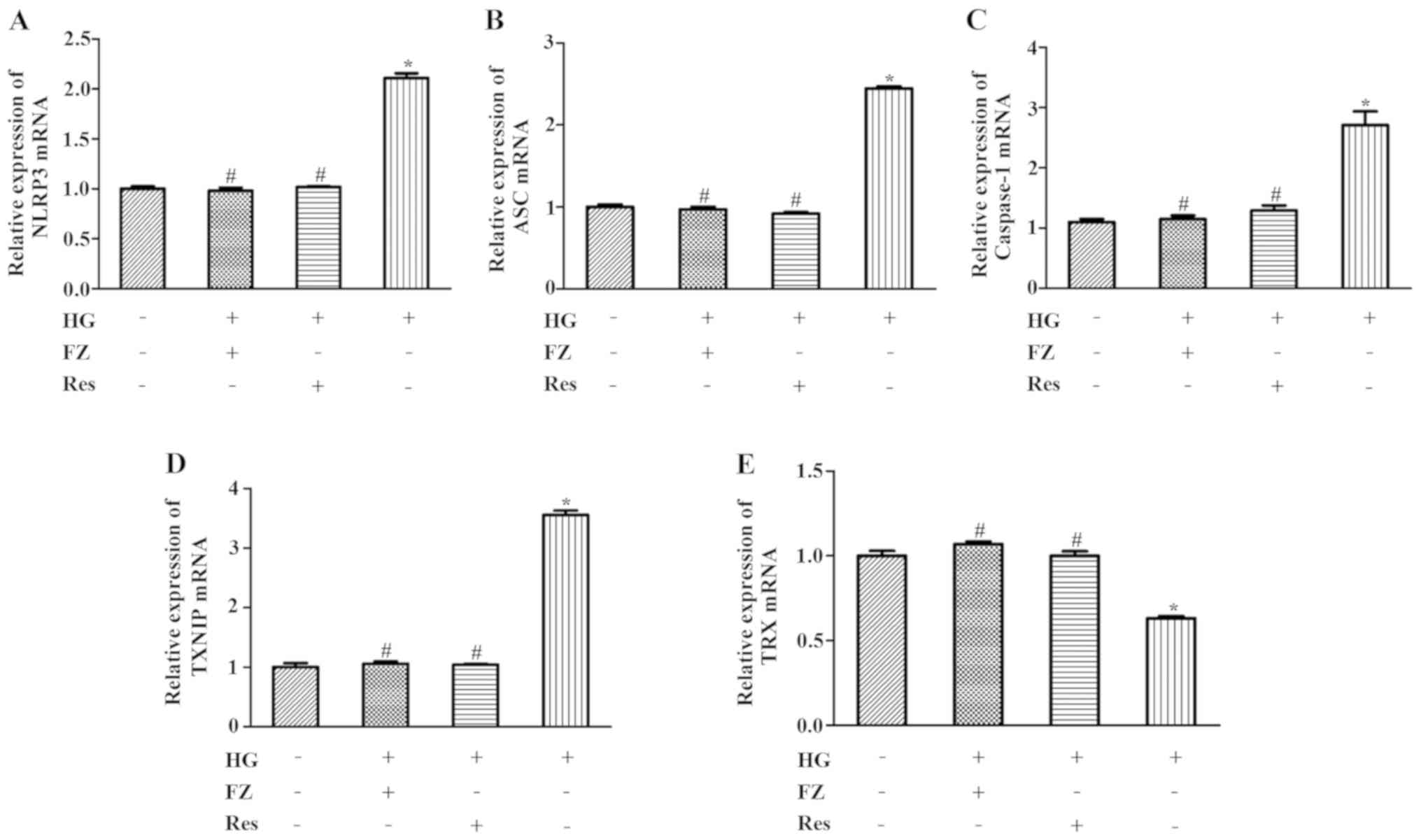
FPS-ZM1 inhibits HG-induced
TXNIP/NLRP3 inflammasome activation
The present study aimed to determine whether FPS-ZM1
inhibited inflammation through the TXNIP/TRX/NLRP3 inflammasome
signaling pathway. As presented in Fig. 4, the mRNA expression of TXNIP,
NLRP3, ASC and caspase-1 were increased, whereas TRX expression
levels were decreased in HG-induced cells (P<0.05). Treatment
with FPS-ZM1 or pretreatment with Res reduced the expression of
TXNIP, caspase-1, NLRP3 and ASC, and enhanced TRX expression
(P<0.05). Similar results were determined by western blotting;
TXNIP, NLRP3, ASC and caspase-1 levels were increased, whereas TRX
expression was decreased in HG-induced BMSCs (P<0.05). However,
these effects were significantly reversed by FPS-ZM1 or Res
(P<0.05) (Fig. 5). These
results indicated that FPS-ZM1 may inhibit TXNIP/NLRP3 activation
under a HG environment.
 | Figure 4.Effects of FZ on the mRNA expression
levels of ASC, TXNIP, NLRP3, caspase-1 and TRX. Reverse
transcription-quantitative PCR was performed after cells were
pretreated with Res for 2 h or co-cultured with FZ and HG for 48 h.
(A) NLRP3, (B) ASC, (C) caspase-1, (D) TXNIP and (E) TRX mRNA
expression. Data are presented as the mean ± standard deviation.
*P<0.05 vs. the normal glucose group; #P<0.05 vs.
the HG group. FZ, FPS-ZM1; ASC, apoptosis-related speck-like
protein containing CARD; TXNIP, thioredoxin-interacting protein;
NLRP3, nucleotide-binding oligomerization domain-like receptor
protein 3; TRX, thioredoxin; HG, high glucose; Res,
resveratrol. |
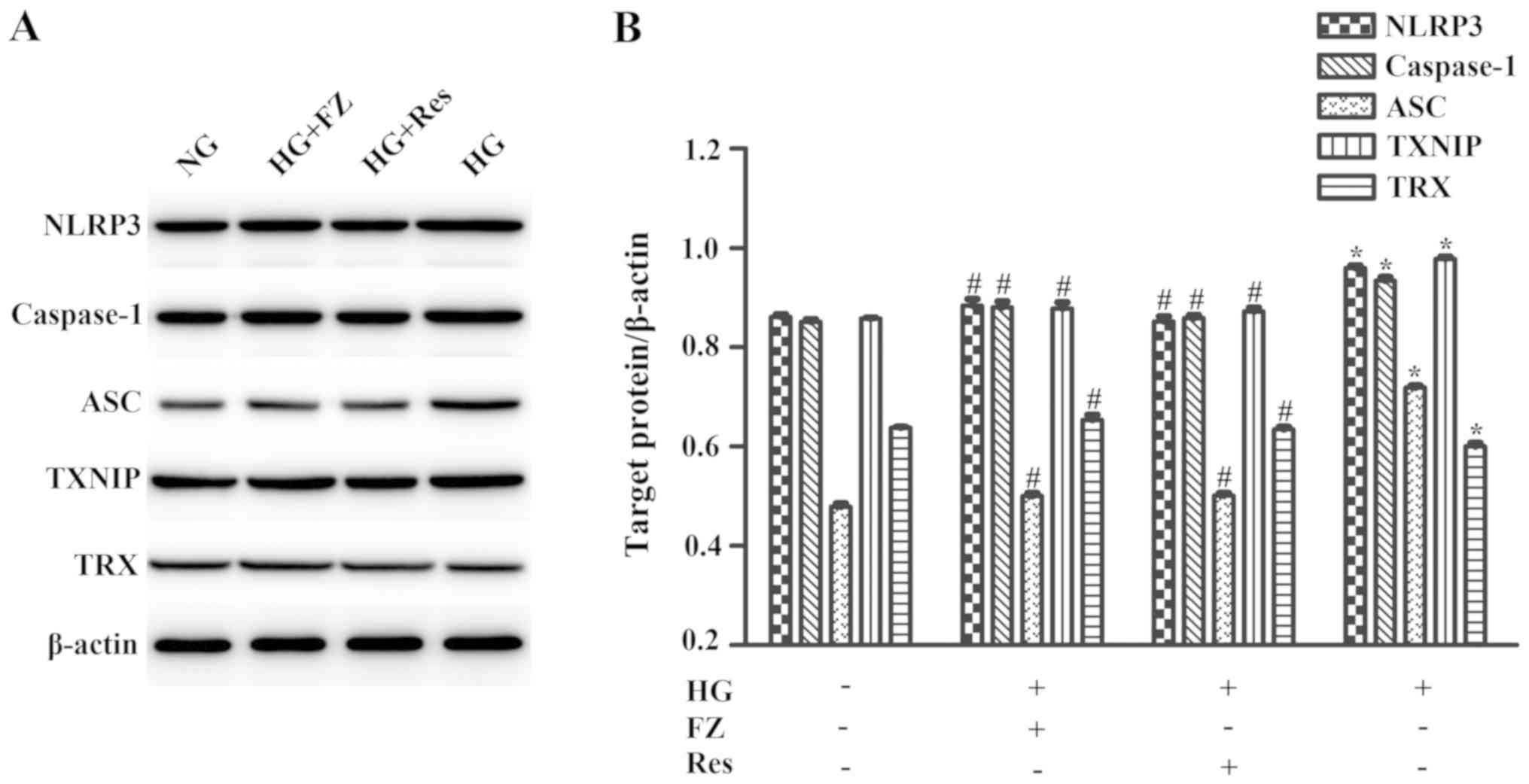 | Figure 5.Effect of FZ on target protein
expression levels, including ASC, TXNIP, NLRP3, caspase-1 and TRX.
Western blot analysis was performed after cells were pretreated
with Res for 2 h or co-cultured with FPS-ZM1 and HG for 48 h.
β-actin was used as a loading control. (A) Protein expression
levels of NLRP3, caspase-1, ASC, TXNIP and TRX were measured by
western blotting. (B) NLRP3/β-actin, caspase-1/β-actin,
ASC/β-actin, TXNIP/β-actin and TRX/β-actin ratios were calculated
to perform densitometric analysis of band intensity. Data are
presented as the mean ± standard deviation. *P<0.05 vs. the NG
group. #P<0.05 vs. the HG group. FZ, FPS-ZM1; ASC,
apoptosis-related speck-like protein containing CARD; TXNIP,
thioredoxin-interacting protein; NLRP3, nucleotide-binding
oligomerization domain-like receptor protein 3; TRX, thioredoxin;
NG, normal glucose; HG, high glucose; Res, resveratrol. |
Discussion
AGEs have been reported to aggregate within the oral
periodontal tissues of patients with diabetes, contributing to the
inflammatory process in the surrounding soft and hard tissues
(32,33). Inflammation may be enhanced when
AGEs bind to RAGE, thus resulting in upregulation of various
proinflammatory factors (34).
IL-1β is considered the most important cytokine, which serves a
crucial role in the inflammatory process (35). IL-6 is a proinflammatory cytokine
that is closely related to periodontitis and rheumatoid arthritis
(36). TNF-α promotes T cells by
secreting various activated cytokines, which are closely associated
with autoimmune diseases, inflammation and diabetes (37).
RAGE is highly expressed in numerous cell types in
periodontal tissues under HG stimulation, including BMSCs (18,38).
It is well known that BMSCs are characterized by multidirectional
differentiation and low immunity, and the potential
immune-regulating effect of BMSCs has garnered increasing
attention. BMSCs are functional and pivotal cells that repair
damaged tissues and organs, including bone tissue, cartilage and
joint injury (39). However, the
differentiation of BMSCs into osteoblasts, lipoblasts or
chondroblasts can be inhibited by inflammation, thus affecting the
tissue repair process (40). BMSC
inflammation has been reported to respond to HG; a previous study
revealed that BMSCs isolated from diabetic rats exhibited stronger
expression of NF-κB and IL-18 compared with normal rats (41). The present study assessed the
inflammatory response of BMSCs induced by HG in vitro.
Subsequently, the effects of FPS-ZM1 on regulating HG-induced
inflammation and the underlying potential mechanism were
determined.
In the present study, the effects of HG were
detected on RAGE expression in BMSCs; the results indicated that HG
exposure stimulated the increased expression of RAGE in BMSCs.
However, FPS-ZM1, a RAGE-specific inhibitor, reversed the enhanced
expression of RAGE induced by HG. In addition, the effects of
various concentrations of FPS-ZM1 (0, 250, 500 and 750 nM) for
different durations on BMSCs were examined. The viability of BMSCs
was enhanced under HG conditions. Conversely, FPS-ZM1 alleviated
HG-induced viability. The present study identified significant
differences between the NG group and the HG-treated groups
regardless of treatment duration. Cell viability of the HG group
was significantly increased compared with NG group, and peaked at
48 h; however, the cell viability began to decrease from 72 h,
which might be due to time-dependent HG aggravation of oxidative
stress in BMSCs (42,43). It has been reported that AGE
expression can significantly inhibit the viability of cells, such
as fibroblasts, in a time-dependent manner (44). AGEs may destroy stability of the
internal environment by enhancing intracellular oxidative stress,
thus inhibiting cell viability (45).
The present study assessed the effects of FPS-ZM1 on
HG-stimulated inflammation in BMSCs. It was previously observed
that HG conditions promoted inflammatory factors and inflammatory
cytokines, such as TNF-α, IL-1β and IL-6, in periodontal tissues
(46,47). The present study on BMSCs presented
similar findings; TNF-α, IL-1β and IL-6 expression was enhanced
after HG stimulation, whereas these effects were inhibited by
FPS-ZM1. FPS-ZM1 exerted a protective effect against HG conditions
in vitro; however, the mechanism underlying the
anti-inflammatory effects of FPS-ZM1 has yet to be determined.
The present study indicated that the TXNIP/NLRP3
pathway may serve a role as the intracellular transduction pathway
underlying the regulatory effects of FPS-ZM1 on HG-induced
inflammation. The NLRP3 inflammasome is a protein complex that
regulates inflammation and cell death (48). Previous studies have reported that
NLRP3 can be overexpressed in epithelial cells or fibroblasts by
glucose, oxidative stress and other types of stimulation, and it
has been suggested to affect diabetes-related periodontal diseases
(49,50). TXNIP has been recognized as an
early mediator associated with diabetic inflammation (51). TXNIP binds to TRX and inhibits its
activity; therefore, TXNIP is also called the TRX-binding protein
(52). Hyperglycemia may
upregulate TXNIP by directly activating the NLRP3 inflammasome,
followed by an enhancement of inflammation-activated factors
(53). In the present study,
FPS-ZM1 downregulated HG-induced expression of TXNIP and NLRP3.
Furthermore, the downregulation of TRX expression stimulated by HG
was reversed by FPS-ZM1. These findings confirmed the role of the
TXNIP/NLRP3 inflammasome signaling pathway in the regulatory
effects of FPS-ZM1 on HG-induced BMSC. This pathway was also
inactivated by Res.
A previous study reported that Res significantly
inhibited the activity of the TXNIP/NLRP3 inflammasome pathway to
achieve the pharmacological effect of inhibiting inflammation
(54). In the present study,
pretreatment with Res disrupted the activity of the TXNIP/NLRP3
inflammasome pathway. Furthermore, Res downregulated HG-induced
expression of TNF-α, IL-1β and IL-6. These findings further support
the hypothesis that the TXNIP/NLRP3 inflammasome signaling pathway
is involved in HG-stimulated inflammation. Therefore, inhibition of
the TXNIP/NLRP3 inflammasome signaling pathway may be considered
one of the mechanisms underlying the anti-inflammatory effects of
FPS-ZM1.
The present study also revealed that although the
mRNA and protein expression levels of inflammation-associated
molecules, such as NLRP3, caspase-1, ASC and TXNIP, were higher in
the HG group than in the NG group, there was a marked difference
between mRNA and protein expression levels. There exists a linear
correlation between mRNA and protein expression, and the change
ratio should be the same; however, the results of other
experimental studies have demonstrated that the linear correlation
is not very high (55,56). This phenomenon has been reported by
numerous studies and may be explained as follows: Gene expression
is regulated in numerous ways, not just by transcriptional
regulation (e.g., histone modification, DNA methylation and
transcription factor regulation), but also by post-transcriptional
alterations, such as microRNA targeting, RNA-binding proteins or
RNA modification (57–59). In addition, various factors,
including mRNA degradation, protein degradation and protein folding
may lead to differences between mRNA and protein expression levels
(60,61). How the reasons for the differences
observed between the mRNA and protein expression remain unknown and
should be further investigated in the future.
In conclusion, the regulatory effects of FPS-ZM1 on
HG-induced inflammation and NLRP3 accumulation in BMSCs were
investigated. HG stimulated RAGE expression in BMSCs and mediated a
series of inflammatory responses, whereas treatment with FPS-ZM1, a
RAGE-specific inhibitor, protected BMSCs by exerting
anti-inflammatory effects, specifically reducing HG-induced cell
viability, inflammatory factor production and TXNIP/NLRP3
inflammasome signaling pathway activation. In addition,
inactivation of the TXNIP/NLRP3 inflammasome by Res exhibited
similar effects as FPS-ZM1, which indicated that the molecular
mechanism underlying the anti-inflammatory effect of FPS-ZM1 may be
associated with the TXNIP/NLRP3 inflammasome signaling pathway.
Based on the anti-inflammatory effects, the results of the present
study provided a novel therapeutic approach and target drug therapy
for patients with diabetes with accelerated occurrence and
development of periodontal diseases. Nonetheless, these studies
were limited to in vitro experiments on BMSCs. Further
studies regarding the role of FPS-ZM1 on peri-implantitis or
periodontal tissues in animal models are required, as the human
microenvironment is more complicated, and an assessment of the
response in vivo is necessary.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Luzhou-school
Union (grant no. 2016LZXNYD-J20).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
MJ and LG mainly contributed to experimental
conception and design. MJ, XW and PW performed the experiments and
collected the data. MJ, WP and BZ conducted the statistical
analysis. MJ wrote the original draft. XW, PW and LG revised the
completed draft. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Shi Y and Hu FB: The global implications
of diabetes and cancer. Lancet. 383:3255–1948. 2014. View Article : Google Scholar
|
|
2
|
Yamamoto Y and Yamamoto H: RAGE-Mediated
Inflammation, type 2 diabetes, and diabetic vascular complication.
Front Endocrinol (Lausanne). 4:1052013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Rübsam A, Parikh S and Fort PE: Role of
Inflammation in diabetic retinopathy. Int J Mol Sci. 19:9422018.
View Article : Google Scholar
|
|
4
|
Yuan Y, Sun H and Sun Z: Advanced
glycation end products (AGEs) increase renal lipid accumulation: A
pathogenic factor of diabetic nephropathy (DN). Lipids Health Dis.
16:1262017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Shi L, Yu X, Yang H and Wu X: Advanced
glycation end products induce human corneal epithelial cells
apoptosis through generation of reactive oxygen species and
activation of JNK and p38 MAPK pathways. PLoS One. 8:e667812013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Meloche J, Paulin R, Roy M, Agharazii M
and Bonnet S: Activation of RAGE/STAT3 axis by advanced glycation
endproducts in vascular remodeling diseases. Circulation. 122
(Suppl 21):S159692010.
|
|
7
|
Sanajou D, Haghjo AG, Argani H and Aslani
S: AGE-RAGE axis blockade in diabetic nephropathy: Current status
and future directions. Eur J Pharmacol. 833:158–164. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sanajou D, Ghorbani Haghjo A, Argani H,
Roshangar L, Rashtchizadeh N, Ahmad SNS, Ashrafi-Jigheh Z and
Bahrambeigi S: Reduction of renal tubular injury with a RAGE
inhibitor FPS-ZM1, valsartan and their combination in
streptozotocin-induced diabetes in the rat. Eur J Pharmacol.
842:40–48. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhan D, Guo L and Zheng L: Inhibition of
the receptor for advanced glycation promotes proliferation and
repair of human periodontal ligament fibroblasts in response to
high glucose via the NF-kappa B signaling pathway. Arch Oral Biol.
87:86–93. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Huang J, Xiong T, Zhang Z, Tan Y and Guo
L: Inhibition of the receptor for advanced glycation inhibits
lipopolysaccharide-mediated High mobility group protein B1 and
Interleukin-6 synthesis in human gingival fibroblasts through the
NF-κB signaling pathway. Arch Oral Biol. 105:81–87. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Graves DT, Ding Z and Yang Y: The impact
of diabetes on periodontal diseases. Periodontol. 82:214–224. 2020.
View Article : Google Scholar
|
|
12
|
Almajwal AM, Alam I, Abulmeaty M, Razak S,
Pawelec G and Alam W: Intake of dietary advanced glycation end
products influences inflammatory markers, Immune phenotypes, and
antiradical capacity of healthy elderly in a little-studied
population. Food Sci Nutr. 8:1046–1057. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yao D, Wang S, Wang M and Lu W:
Renoprotection of dapagliflozin in human renal proximal tubular
cells via the inhibition of the high mobility group box 1receptor
for advanced glycation end productsnuclear factor-κB signaling
pathway. Mol Med Rep. 18:3625–3630. 2018.PubMed/NCBI
|
|
14
|
Chang PC, Chien LY, Yeo JF, Wang YP, Chung
MC, Chong LY, Kuo MY, Chen CH, Chiang HC, Ng BN, et al: Progression
of periodontal destruction and the roles of advanced glycation end
products in experimental diabetes. J Periodontol. 84:379–388. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bartold PM and Van Dyke TE: Periodontitis:
A host-mediated disruption of microbial homeostasis. Unlearning
learned concepts. Periodontol. 62:203–217. 2013. View Article : Google Scholar
|
|
16
|
Al-Sowygh ZH, Ghani SMA, Sergis K, Vohra F
and Akram Z: Peri-implant conditions and levels of advanced
glycation end products among patients with different glycemic
control. Clin Implant Dent Relat Res. 20:345–351. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Dey D, Jingar P, Agrawal S, Shrivastava V,
Bhattacharya A, Manhas J, Garg B, Ansari MT, Mridha AR, Sreenivas
V, et al: Symphytum officinale augments osteogenesis in human bone
marrow-derived mesenchymal stem cells in vitro as they
differentiate into osteoblasts. J Ethnopharmacol. 248:1123292020.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dhanasekaran M, Indumathi S, Rajkumar JS
and Sudarsanam D: Effect of high glucose on extensive culturing of
mesenchymal stem cells derived from subcutaneous fat, omentum fat
and bone marrow. Cell Biochem Funct. 31:20–29. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Nonaka K, Kajiura Y, Bando M, Sakamoto E,
Inagaki Y, Lew JH, Naruishi K, Ikuta T, Yoshida K, Kobayashi T, et
al: Advanced glycation end-products increase IL-6 and ICAM-1
expression via RAGE, MAPK and NF-κB pathways in human gingival
fibroblasts. J Periodontal Res. 53:334–344. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Thielen L and Shalev A: Diabetes
pathogenic mechanisms and potential new therapies based upon a
novel target called TXNIP. Curr Opin Endocrinol Diabetes Obes.
25:75–80. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gouravani M, Khalili N, Razi S,
Keshavarz-Fathi M, Khalili N and Rezaei N: The NLRP3 inflammasome:
A therapeutic target for inflammation-associated cancers. Expert
Rev Clin Immunol. 16:175–187. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Feng H, Gu J, Gou F, Huang W, Gao C, Chen
G, Long Y, Zhou X, Yang M, Liu S, et al: High Glucose and
lipopolysaccharide prime NLRP3 inflammasome via ROS/TXNIP pathway
in mesangial cells. J Diabetes Res. 2016:1–11. 2016. View Article : Google Scholar
|
|
23
|
An N, Gao Y, Si Z, Zhang H, Wang L, Tian
C, Yuan M, Yang X, Li X, Shang H, et al: Regulatory mechanisms of
the NLRP3 inflammasome, a novel immune-inflammatory marker in
cardiovascular diseases. Front Immunol. 10:15922019. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Matsui T, Nakamura N, Ojima A, Nishino Y
and Yamagishi SI: Sulforaphane reduces advanced glycation end
products (AGEs)-induced inflammation in endothelial cells and rat
aorta. Nutr Metab Cardiovasc Dis. 26:797–807. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Saresella M, La Rosa F, Piancone F, Zoppis
M, Marventano I, Calabrese E, Rainone V, Nemni R, Mancuso R and
Clerici M: The NLRP3 and NLRP1 inflammasomes are activated in
Alzheimers disease. Mol Neurodegener. 11:232016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zhao LR, Xing RL, Wang PM, Zhang NS, Yin
SJ, Li XC and Zhang L: NLRP1 and NLRP3
inflammasomes mediate LPS/ATP-induced pyroptosis in knee
osteoarthritis. Mol Med Rep. 17:5463–5469. 2018.PubMed/NCBI
|
|
27
|
Wen H, Gris D, Lei Y, Jha S, Zhang L,
Huang MT, Brickey WJ and Ting JP: Fatty acid-induced NLRP3-ASC
inflammasome activation interferes with insulin signaling. Nat
Immunol. 12:408–415. 2011. View
Article : Google Scholar : PubMed/NCBI
|
|
28
|
Bharti V, Tan H, Zhou H and Wang JF: Txnip
mediates glucocorticoid-activated NLRP3 inflammatory signaling in
mouse microglia. Neurochem Int. 131:1045642019. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Omar DF, Kamal MM, El-Hefnawy MH and
El-Mesallamy HO: Serum Vitamin D and its upregulated protein,
thioredoxin interacting protein, are associated with beta-cell
dysfunction in adult patients with type 1 and type 2 diabetes. Can
J Diabetes. 42:588–594. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Gateva AT, Assyov YS, Velikova T and
Kamenov ZA: Higher levels of thioredoxin interacting protein
(TXNIP) in patients with prediabetes compared to obese
normoglycemic subjects. Diabetes Metabolic Syndrome. 13:734–737.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chiu HC, Fu MM, Yang TS, Fu E, Chiang CY,
Tu HP, Chin YT, Lin FG and Shih KC: Effect of high glucose,
Porphyromonas gingivalis lipopolysaccharide and advanced glycation
endproducts on production of interleukin-6/-8 by gingival
fibroblasts. J Periodontal Res. 52:268–276. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Lalla E, Lamster IB, Stern DM and Schmidt
AM: Receptor for advanced glycation end products, inflammation, and
accelerated periodontal disease in diabetes: Mechanisms and
insights into therapeutic modalities. Ann Periodontol. 6:113–118.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Daniele G, Guardado Mendoza R, Winnier D,
Fiorentino TV, Pengou Z, Cornell J, Andreozzi F, Jenkinson C,
Cersosimo E, Federici M, et al: The inflammatory status score
including IL-6, TNF-α, osteopontin, fractalkine, MCP-1 and
adiponectin underlies whole-body insulin resistance and
hyperglycemia in type 2 diabetes mellitus. Acta Diabetol.
51:123–131. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Han Y, Xu X, Tang C, Gao P, Chen X, Xiong
X, Yang M, Yang S, Zhu X, Yuan S, et al: Reactive oxygen species
promote tubular injury in diabetic nephropathy: The role of the
mitochondrial ros-txnip-nlrp3 biological axis. Redox Biol.
16:32–46. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Taylor JJ, Preshaw PM and Lalla E: A
review of the evidence for pathogenic mechanisms that may link
periodontitis and diabetes. J Clin Periodontol. 40 (4
Suppl):S113–S134. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Akdis M, Aab A, Altunbulakli C, Azkur K,
Costa RA, Crameri R, Duan S, Eiwegger T, Eljaszewicz A, Ferstl R,
et al: Interleukins (from IL-1 to IL-38), interferons, transforming
growth factor β, and TNF-α: Receptors, functions, and roles in
diseases. J Allergy Clin Immunol. 138:984–1010. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Zheng DH, Han ZQ, Wang XX, Ma D and Zhang
J: Erythropoietin attenuates high glucose-induced oxidative stress
and inhibition of osteogenic differentiation in periodontal
ligament stem cell (PDLSCs). Chem Biol Interact. 305:40–47. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Kang K, Chuai JB, Xie BD, Li JZ, Qu H, Wu
H, Fang SH, Cui JJ, Xiu LL, Han JC, et al: Mesenchymal stromal
cells from patients with cyanotic congenital heart disease are
optimal candidate for cardiac tissue engineering. Biomaterials.
230:1195742020. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Dong H, Wang Z, Chen Y and Li Y:
Protective effects of bone Marrow-derived mesenchymal stem cells on
insulin secretion and inflammation in the treatment of severe acute
pancreatitis in rats. Transplant Proc. 52:333–344. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Li H, Zhou HL, Guo F, Wang Q and Li W: The
effects of 25-hydroxyvitamin D3 on the activation of
NLRP3 inflammasome and inflammatory response of bone marrow
mesenchymal stem cells from the diabetic rats. J Pract Stomatol.
34:11–15. 2018.
|
|
42
|
Liao F, Liu Y, Liu HH, Hu J, Zhao S and
Yang SM: Effect of Angelica sinensis polysaccharide on the
osteogenic differentiation of bone marrow mesenchymal stem cells of
rats with high glucose levels. Hua Xi Kou Qiang Yi Xue Za Zhi.
37:193–199. 2019.(In Chinese). PubMed/NCBI
|
|
43
|
Li H, Wang D, Chen Y and Yang M:
β-Caryophyllene inhibits high glucose-induced oxidative stress,
inflammation and extracellular matrix accumulation in mesangial
cells. Int Immunopharmacol. 84:1065562020. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Soydas T, Yaprak Sarac E, Cinar S, Dogan
S, Solakoglu S, Tuncdemir M and Kanigur Sultuybek G: The protective
effects of metformin in an in vitro model of aging 3T3 fibroblast
under the high glucose conditions. J Physiol Biochem. 74:273–281.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Wu J, Lu K, Zhu M, Xie X, Ding Y, Shao X,
Chen Y, Liu J, Xu M, Xu Y, et al: miR-485 suppresses inflammation
and proliferation of mesangial cells in an in vitro model of
diabetic nephropathy by targeting NOX5. Biochem Biophys Res Commun.
521:984–990. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Wang Z, Maruyama K, Sakisaka Y, Suzuki S,
Tada H, Suto M, Saito M, Yamada S and Nemoto E: Cyclic stretch
force induces periodontal ligament cells to secrete exosomes that
suppress IL-1β production through the inhibition of the NF-κB
signaling pathway in macrophages. Front Immunol. 10:13102019.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Yang L, Wu L, Zhang X, Hu Y, Fan Y and Ma
J: 1,25(OH)2D3/VDR attenuates high glucoseinduced
epithelialmesenchymal transition in human peritoneal mesothelial
cells via the TGFβ/Smad3 pathway. Mol Med Rep. 15:2273–2279. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Dong F, Dong S, Liang Y, Wang K, Qin Y and
Zhao X: miR-20b inhibits the senescence of human umbilical vein
endothelial cells through regulating the Wnt/β-catenin pathway via
the TXNIP/NLRP3 axis. Int J Mol Med. 45:847–857. 2020.PubMed/NCBI
|
|
49
|
Lu WL, Song DZ, Yue JL, Wang TT, Zhou XD,
Zhang P, Zhang L and Huang DM: NLRP3 inflammasome may regulate
inflammatory response of human periodontal ligament fibroblasts in
an apoptosis-associated speck-like protein containing a CARD
(ASC)-dependent manner. Int Endod J. 50:967–975. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Bui FQ, Johnson L, Roberts J, Hung SC, Lee
J, Atanasova KR, Huang PR, Yilmaz Ö and Ojcius DM: Fusobacterium
nucleatum infection of gingival epithelial cells leads to NLRP3
inflammasome-dependent secretion of IL-1β and the danger signals
ASC and HMGB1. Cell Microbiol. 18:970–981. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Szpigel A, Hainault I, Carlier A,
Venteclef N, Batto AF, Hajduch E, Bernard C, Ktorza A, Gautier JF,
Ferré P, et al: Lipid environment induces ER stress, TXNIP
expression and inflammation in immune cells of individuals with
type 2 diabetes. Diabetologia. 61:399–412. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Lu L, Lu Q, Chen W, Li J, Li C and Zheng
Z: Vitamin D3 Protects against diabetic retinopathy by
inhibiting high-glucose-induced activation of the ROS/TXNIP/NLRP3
inflammasome pathway. J Diabetes Res. 2018:81935232018. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Yi X, Zhang L, Lu W, Tan X, Yue J, Wang P,
Xu W, Ye L and Huang D: The effect of NLRP inflammasome on the
regulation of AGEs-induced inflammatory response in human
periodontal ligament cells. J Periodontal Res. 54:681–689. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Bedarida T, Baron S, Vibert F, Ayer A,
Henrion D, Thioulouse E, Marchiol C, Beaudeux JL, Cottart CH and
Nivet-Antoine V: Resveratrol decreases TXNIP mRNA and protein
nuclear expressions with an arterial function improvement in old
mice. J Gerontol A Biol Sci Med Sci. 71:720–729. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Choe D, Palsson B and Cho BK: STATR: A
simple analysis pipeline of Ribo-Seq in bacteria. J Microbiol.
58:217–226. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Jeong Y, Kim JN, Kim MW, Bucca G, Cho S,
Yoon YJ, Kim BG, Roe JH, Kim SC, Smith CP, et al: The dynamic
transcriptional and translational landscape of the model antibiotic
producer Streptomyces coelicolor. Nat Commun. 7:116052016.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Liu Y, Beyer A and Aebersold R: On the
dependency of cellular protein levels on mRNA abundance. Cell.
165:535–550. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Koussounadis A, Langdon SP, Um IH,
Harrison DJ and Smith VA: Relationship between differentially
expressed mRNA and mRNA-protein correlations in a xenograft model
system. Sci Rep. 5:107752015. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Schwanhäusser B, Busse D, Li N, Dittmar G,
Schuchhardt J, Wolf J, Chen W and Selbach M: Global quantification
of mammalian gene expression control. Nature. 473:337–342. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Surkova S, Sokolkova A, Kozlov K, Nuzhdin
SV and Samsonova M: Quantitative analysis reveals genotype- and
domain-specific differences between mRNA and protein expression of
segmentation genes in Drosophila. Dev Biol. 448:48–58. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Wu X, Zhao W, Cui Q and Zhou Y:
Computational screening of potential regulators for mRNA-protein
expression level discrepancy. Biochem Biophys Res Commun.
523:196–201. 2020. View Article : Google Scholar : PubMed/NCBI
|