Introduction
Heat stroke (HS) is a potentially fatal medical
condition, and its incidence and mortality rates are predicted to
increase due to global warming (1).
Between 2006 and 2010, ~3,000 HS-related deaths were reported in
the USA according to an epidemiological analysis (2). In 2003, ~30,000 HS-related deaths were
caused by a European heat wave event (3). Additionally, ~1,600 HS-related deaths
are reported in India annually (4).
A study estimated that HS-related deaths could increase to ~2.5
times the current rate (5).
HS is characterized by a core body temperature in
excess of 40°C, skin that feels hot and dry to the touch,
dysfunction of the central nervous system and occasionally multiple
organ dysfunction syndrome (MODS) (6–8). HS is
classified into exertional HS (EHS) and non-exertional HS (NEHS).
EHS primarily affects young individuals who perform physical
activities in high temperature and humid environments, such as
soldiers and athletes, whereas NEHS primarily affects elderly
individuals, or those with preexisting conditions such as diabetes
and heart disease (9). Regardless
of the type, HS affects the temperature regulation system of the
body, triggering damage to important body organs, such as the
lungs, liver, brain and kidneys (10–12);
this series of events may progress to MODS and induce death. The
most common complication of HS is acute kidney injury (AKI), which
can rapidly develop into acute renal failure (ARF), with a high
mortality (13,14).
Although advances in medical science have resulted
in the development of effective treatment/management strategies,
such as rapid cooling, blood purification to stabilize organ
functions and supportive therapies, the incidence and mortality
rates of severe HS have not decreased in previous decades (15–17). A
number of studies have identified certain biochemical markers as
prognostic factors for HS. For example, Ye et al (18) found that increased creatine kinase
and decreased blood platelet count are useful in assessing the
progression of HS, thereby enabling timely prediction of
complications. Zhao et al (19) reported that disseminated
intravascular coagulation (DIC) and AKI are the only two
significant prognostic factors for HS among all its complications,
including MODS, that predict increased HS-related mortality.
Another study demonstrated that AKI occurred during the early
stages of HS and lasted for a sustained period of time, before
progressing to ARF if left untreated (20). Moreover, a study also found that
occurrence of AKI has been associated with increased
myeloperoxidase, tumor necrosis factor-α and interleukin-6 levels
in the kidneys (21). A study on
CASQ1-knockout mice indicated that calsequestrin-1 could be
a novel candidate gene for malignant hyperthermia and EHS (22). Unfortunately, the identification of
all of these parameters associated with HS has resulted in only
limited improvements in the treatment of HS. Therefore,
understanding the potential mechanisms underlying HS is important
for improving the treatment of HS.
Several mechanisms involved in HS are currently
accepted. Systemic inflammation and MODS are reported to play key
roles in the pathophysiology of HS (23,24).
HS causes dysfunction of the intestinal barrier (25), leading to intercellular penetration
of harmful substances such as bacteria and endotoxins within the
gut lumen. The bacteria and endotoxins then seep into the
circulation, and cause inflammation and cytokine secretion, which
will eventually result in systemic inflammatory response syndrome
(SIRS) and MODS (26,27). Metabolomics profiling, an emerging
research methodology of systems biology, enables the comprehensive
and quantitative analysis of all metabolites in a biological sample
and the identification of their direct associations with biological
phenotypes, such as responses to a disease or a drug treatment or
intervention (28,29). In contrast to genomics and
proteomics, which focus on intermediate media, metabolomics
measures end products, which helps in accurate identification of
disease pathogenesis. HS increases glucose utilization, which
reduces the availability of the metabolic substrates required for
proper function of the brain, heart and muscles (30).
In the present study, a mouse model of HS was
constructed to examine whether the high-mobility group box 1
(HMGB1)/receptor for advanced glycosylation end products (RAGE)
pathway is activated in mouse kidneys. Metabolomics analysis was
performed to investigate the underlying mechanisms of HS. A total
of 136 differential metabolites were screened out and analyzed, and
several important signaling pathways that may play important roles
in HS development, including ‘biosynthesis of unsaturated fatty
acids’, were determined to be enriched.
Materials and methods
Animals
The present study was conducted on 20 8-week-old
male C57BL/6J mice (weight, 21–23 g; Beijing HFK Bioscience Co.,
Ltd.). The mice were housed in a specific pathogen-free and 40–50%
humidity environment at the animal laboratory of the Affiliated
Hospital of Southwest Medical University (free access to food and
water; 12-h light/12-h dark cycle; 24°C). All animal experiments
complied with the guidelines of the Animal Care and Use Committee
of the Southwest Medical University; the study protocol was
approved by the same committee.
Experimental design
The mice were randomly divided into control (no heat
exposure) and HS groups (heat exposure). The experimental design
was based on a previously described method (31–33).
After being subjected to 6 h of fasting, the HS group was housed in
a temperature-controlled environment at 41.0°C (relative humidity,
60%). An infrared thermometer (MC818A; Shenzhen MileSeey Technology
Co., Ltd.) was used to detect the shell temperature of the mice
every 15 min until the temperature reached 41°C. Electrodes were
then inserted into the rectum of each mouse to re-detect the
temperature. The onset of HS was defined as when the core
temperature exceeded 41°C (34). In
the experimental group, all mice were immediately withdrawn from
the heat environment and showered with cold water to rapidly
decrease their core temperature to 37.0°C. This temperature was
maintained by placing the mice in ambient conditions (26°C). In the
control group, the core temperature of the mice was maintained at
36°C using a folded heating pad, if needed. Control animals were
housed in the same temperature-controlled environment at the HS
group during the protocol. After model construction, two mice from
each group were selected for a micro-positron emission
tomography-computed tomography (micro-PET/CT) scan. All mice were
then anesthetized with 3% pentobarbital sodium (30 mg/kg) by
intraperitoneal injection and sacrificed via cervical dislocation.
Death was ascertained based on pupil dilation and an inability to
palpate the carotid pulse. Blood samples were then collected, and
the kidneys were dissected and fixed in 4% paraformaldehyde for 30
min at room temperature for follow-up examinations.
Plasma glucose and creatinine
levels
Before sacrificing the mice, peripheral plasma
glucose levels were measured with a blood glucose meter (Roche
Applied Science). The tails were removed to ensure that
18F-deoxyglucose (18FDG), which was injected
into the tail vein for micro-PET/CT, did not influence the
peripheral plasma glucose level measurements. Cardiac blood samples
were collected immediately after cervical dislocation.
Subsequently, peripheral and cardiac blood was centrifuged at 2,000
× g for 30 min at room temperature to isolate the plasma, which was
stored at −80°C. The obtained plasma was then transported to a
diagnostic laboratory for the measurement of creatinine levels
using an Indiko™ system (Thermo Fisher Scientific, Inc.).
Micro-PET/CT scanning
18FDG is a commonly used radionuclide
imaging agent that is actively absorbed by cells as an energy
substrate and indirectly reflects the energy metabolism of the
body. 18FDG (3.7 MBq/kg), obtained from an Eclipse HP/RD
accelerator (Siemens AG), was injected into the tail vein 20 min
before the scan. The radioisotope uptake of the tissues, which
reflects the status of the body's energy metabolism, was detected
using an Inveon™ micro-PET/CT system (Siemens AG). The test
parameters were set as follows: Resolution of transverse,
longitudinal and axial directions of the PET module, 1.5 mm;
collection timing window, 3.4 nsec; energy window, 350–650 keV; and
collection time, 10 min. The filtered back projection algorithm was
used for reconstruction. The images were analyzed using Inveon
image acquisition (IAW 1.5; Siemens AG). The PET value was set at
1.8–9.9, and the CT window width at 500–1000 HU.
H&E staining
Paraformaldehyde-fixed kidney tissues were
paraffin-embedded, cut into 4-µm sections, deparaffinized, and
serially rehydrated using xylene, an ethanol gradient series (100,
96, 80 and 70% ethanol) and finally H2O. Next, the
sections were stained with 10% hematoxylin for 5 min at room
temperature (Sigma-Aldrich; Merck KGaA), washed, stained with 1%
eosin (Sigma-Aldrich; Merck KGaA) supplemented with 0.2% glacial
acetic acid for 5 mins at room temperature, immediately washed
again, and dehydrated using an ethanol gradient (70, 80, 96 and
100%) and xylene. Finally, the sections were examined under an
inverted phase-contrast microscope (DMi1; Leica Microsystems GmbH).
The renal tubule injury score based on the Parller system was
calculated to analyze renal injury (35). A total of 10 renal tubules within 10
non-overlapping high magnification fields were randomly selected
for a total of 100 renal tubules, which were then evaluated to
determine the renal tubule injury score as follows: Normal
structure of the epithelial cells, 0 points; obvious renal tubule
expansion, loss of brush border, epithelial cell edema, vacuolar
degeneration, granular degeneration and/or nuclear deflation, 1
point; and foaming of the cell membrane, cell necrosis and/or
tubular appearance in the tubule lumen, 2 points. The sum of the
scores for all 100 tubules was used as the Parller score for each
animal.
Immunohistochemistry (IHC)
analysis
In brief, 4-µm paraffin-embedded sections were
deparaffinized, subjected to antigen retrieval using citrate buffer
(pH 6.0) at 95°C for 10 min and treated with 0.3%
H2O2 to block their endogenous peroxidase
activity at room temperature for 10 min. Next, the sections were
continuously treated with blocking reagent QuickBlock™ (cat. no.
P0260; Beyotime Institute of Biotechnology), then incubated with
the appropriate primary antibodies, such as apoptosis-inducing
factor mitochondria-associated 2 (Aifm2; 1:1,000; cat. no.
GXP20453; GenXspan) and HMGB1 (1:100; cat. no. ab227168; Abcam) at
4°C overnight, and then with the secondary antibody (1:5,000; cat.
no. TA130017 Biotinylated Goat anti rabbit; OriGene Technologies,
Inc.) for 1 h at room temperature. Peroxidase activity was
visualized using 3,3′-diaminobenzidine at room temperature for 5
min. The relative expression density and location of Aifm2 and
HMGB1 in the mouse kidney tissues were quantified at ×400
magnification per 30 fields, according to the Envision method
(36), by two pathologists blinded
to the experiment. The relative expression of proteins located
mainly in the cytoplasm was calculated using the relative mean
absorbance according to the Envision method. The relative
expression of proteins located mainly in the nucleus was determined
as the number of positive cells per 200 cells in a high-power field
(magnification, ×400). All IHC sections were examined with a
phase-contrast microscope. Image-Pro Plus 6 software (Media
Cybernetics, Inc.) was used for analysis.
Transmission electron microscopy
(TEM)
Dissected mouse kidneys were fixed in 2.5%
glutaraldehyde at 4°C overnight, washed three times with 0.1 M PBS
and stained with 1% osmium acid at 4°C for 3 h. The sections were
then washed 3 times with PBS, dehydrated in ethanol and
subsequently propylene oxide, embedded in Spurr resin at room
temperature overnight and finally polymerized at 70°C overnight.
The embedded sections were cut into 70-nm slices. Slides of these
slices were prepared and stained with lead citrate and uranium
dioxide acetate at 80°C for 15 min, and photographed under a
transmission electron microscope.
TUNEL assay
Sections (2–3 µm) of mouse kidney tissues were
incubated for 2 min with 0.1% Triton X-100 and washed using
ice-cold PBS. Cell apoptosis was assayed using TUNEL reagent for 60
min at 37°C (Roche Applied Science), according to the
manufacturer's protocols. Cells with yellow-stained nuclei were
defined as positive cells at 25°C for 10 min (Concentrated DAB
reagent kit; OriGene Technologies, Inc.). The positive cells in 200
randomly selected cells were counted using a phase-contrast
microscope (magnification, ×100; 10 fields of view).
Western blot analysis
The dissected kidney tissues were lysed and
sonicated (20 sec per 5 min) for 30 min on ice in
radioimmunoprecipitation assay buffer (Beyotime Institute of
Biotechnology) supplemented with a protease inhibitor and a
phosphatase inhibitor (Sigma-Aldrich; Merck KGaA) on an ice bath
for 30 min. The tissues were then centrifuged for 15 min at 13,000
× g and 4°C. The supernatant thus obtained was subjected to the
bicinchoninic acid assay for protein quantitation, and bovine serum
albumin (Beyotime Institute of Biotechnology,) was used as the
standard. In brief, 40 µg protein extracts were denatured,
separated via 10% SDS-PAGE, and transferred to Hybond®
polyvinylidene difluoride membranes. The membranes were washed and
blocked using 0.1% TBS-Tween buffer and 5% non-fat milk (BD
Biosciences) at room temperature for 2 h and subsequently probed
with RAGE (1:2,000; cat. no. ab3611; Abcam), HMGB1 (1:2,000; cat.
no. ab227168; Abcam) and β-actin (1:5,000; cat. no. ab8226; Abcam)
primary antibodies at 4°C overnight, and secondary antibodies for 1
h at room temperature [1:5,000; Biotinylated Goat anti rabbit IgG
(H + L); cat. no. ab6721; Abcam] Protein bands were evaluated using
enhanced chemiluminescence reagent (Bio-Rad Laboratories, Inc.) and
Biomax MR films (Kodak). Relative protein abundance of the
indicated proteins was determined using ChemiDoc XRS+ System/Image
Lab Software version 2.0 (Bio-Rad Laboratories, Inc.).
Liquid chromatography-mass
spectrometry (LC-MS) analysis
All chemicals and solvents used were of analytical
or high-performance liquid chromatography grade. Acetonitrile,
formic acid, methanol and water were acquired from CNW Technologies
GmbH, and 2-chloro-L-phenylalanine from Shanghai Hengchuang
Bio-technology Co., Ltd. Aliquots of the samples (30 mg) were
transferred to tubes containing two small steel balls. To each
tube, 400 µl extraction solvent with methanol water (4:1, v/v) and
20 µl internal standard (2-chloro-L-phenylalanine in methanol, 0.3
mg/ml) were added. The samples were frozen to −80°C for 2 min,
ground for 2 min at 60 Hz, ultrasonicated (frequency, 40 KHz;
capacity, 200 W) for 10 min in ice water bath, and frozen again to
−20°C for 20 min. The extract was centrifuged for 10 min at 15,624
× g in 4°C. Supernatants (200 µl) from each tube were collected
using crystal syringes, filtered using microfilters (pore size,
0.22 µm) and transferred to liquid chromatography vials. The vials
were stored at −80°C until LC-MS analysis.
An ACQUITY UPLC BEH C18 column (1.7 µm, 2.1×100 mm)
was employed in both positive and negative modes. The binary
gradient elution system consisted of (A) water (containing 0.1%
formic acid, v/v) and (B) acetonitrile (containing 0.1% formic
acid, v/v) and separation was achieved using the following
gradient: 0 min, 5% B; 2 min, 20% B; 4 min, 25% B; 9 min, 60% B; 14
min, 100% B; 18 min, 100% B; 18.1 min, 5% B and 19.5 min, 5% B. The
flow rate was 0.4 ml/min and the column temperature was 45°C. All
the samples were kept at 4°C during the analysis. The injection
volume was 5 µl. Data acquisition was performed in full scan mode
(m/z; ranges from 70–1,000 m/z) combined with IDA mode. Parameters
of mass spectrometry were as follows: Ion source temperature, 550°C
(+) and 550°C (−); ion spray voltage, 5,500 V (+) and 4,500 V (−);
curtain gas of 35 PSI; declustering potential, 100 V (+) and −100 V
(−); collision energy, 10 eV (+) and −10 eV (−); and interface
heater temperature, 550°C (+) and 600°C (−). For IDA analysis,
range of m/z was set as 25–1,000 m/z, the collision energy was 30
eV. The QCs were injected at regular intervals (every 10 samples)
throughout the analytical run to provide a set of data from which
repeatability can be assessed. Metabolic profiles were analyzed in
both the electrospray ionization-positive and electrospray
ionization-negative modes by using an AB SCIEX Triple TOF 5600
system (SCIEX) and an ACQUITY UHPLC system (Waters
Corporation).
Identification of differential
metabolites
The raw data obtained from LC-MS were analyzed using
Progenesis QI (v 2.3; Waters Corporation) for baseline filtering,
peak identification and alignment, normalization, integration and
retention time correction. Quantitative analysis was performed
using the Metlin metabolite database (metlin.scripps.edu), the Human Metabolome Database
(http://www.hmdb.ca/) and LIPID MAPS (http://www.lipidmaps.org/). The metabolic alterations
in each group were visualized using orthogonal partial least
squares discriminant analysis (OPLS-DA) and principal component
analysis (PCA). Differential metabolites were defined as
metabolites with variable influence on projection values >1.0
(obtained using the OPLS-DA model) and P<0.05 (obtained using a
two-tailed Student's t-test of normalized peak areas).
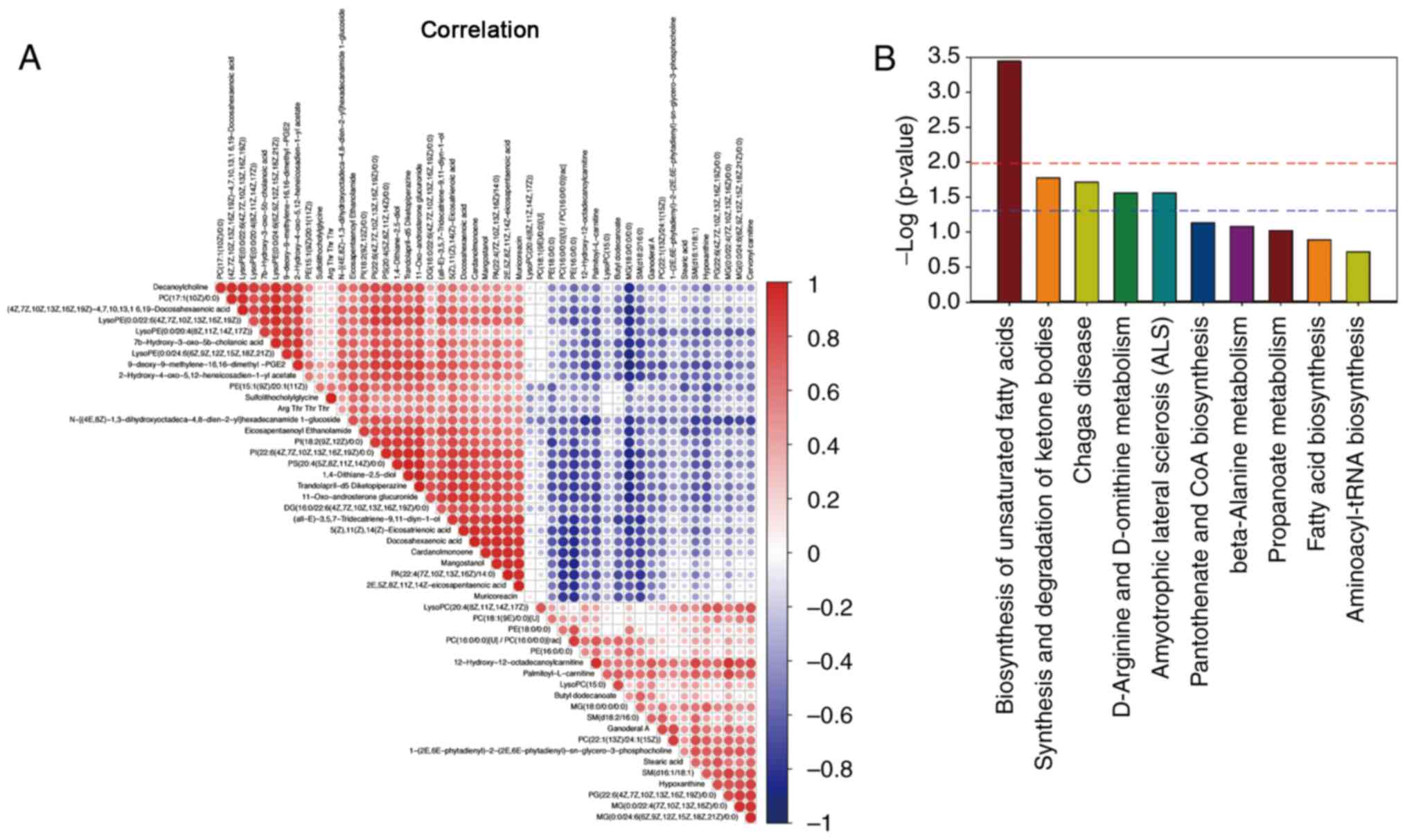
Pearson correlation coefficient analysis was used to
calculate the correlations among the differential metabolites.
Moreover, MBRole 2.0 (37) pathway
analysis of the differential metabolites was conducted using the
Kyoto Encyclopedia of Genes and Genomes (KEGG) database (38) to determine signaling pathways
associated with HS-related AKI.
Statistical analysis
All statistical analyses were performed using SPSS
v22.0 (IBM Corp.). Measurement data are expressed as the mean ± SD.
Between-group comparisons were performed using unpaired Student's
t-test. The heat map and volcano plot were performed and analyzed
using ‘pheatmap’ packages in R 3.53. P<0.05 was considered to
indicate a statistically significant difference.
Results
HS can induce SIRS
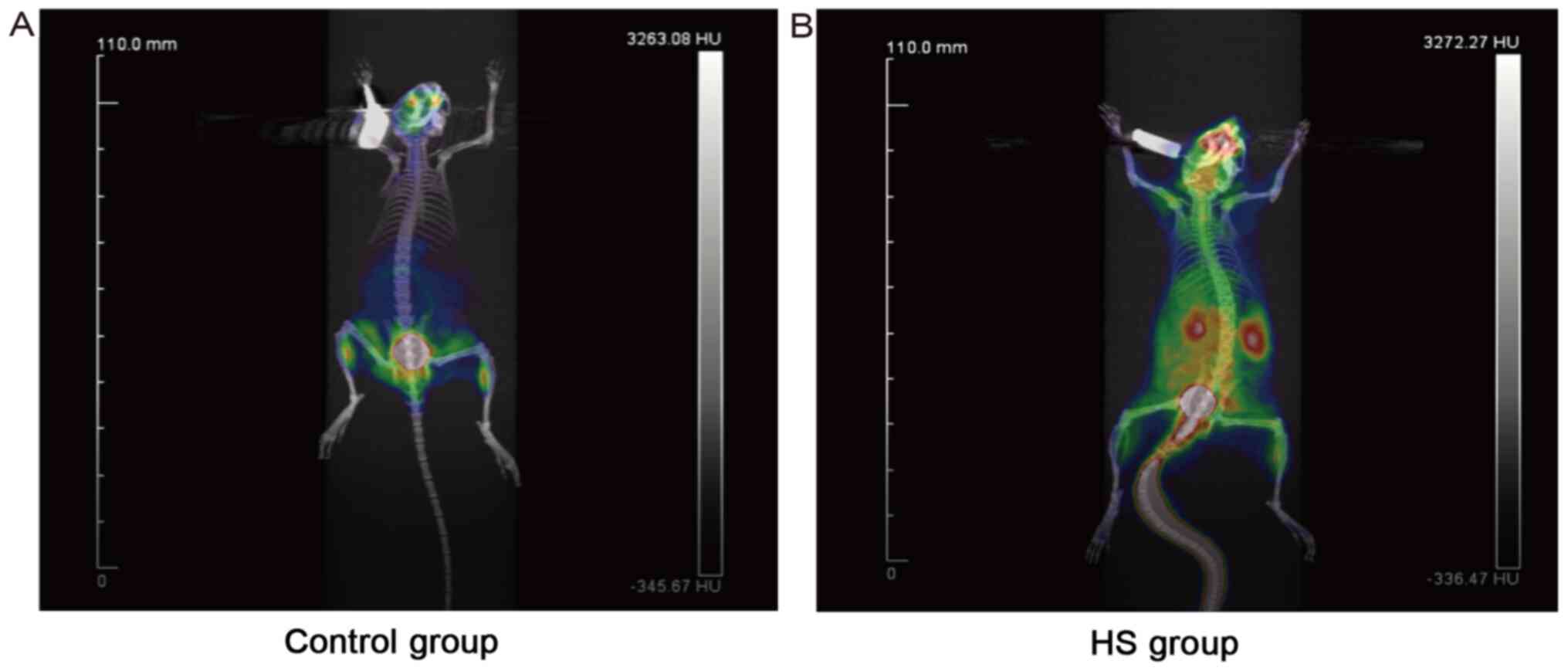
After inducing HS in mice, 18FDG was
injected into the tail vein of each of the 4 mice selected for the
measurement of changes in energy metabolism. As 18FDG is
a glucose analog that influences cell metabolism by inhibiting
glycolysis, peripheral plasma glucose levels were analyzed. The
results indicated that there were no significant differences in
plasma glucose concentrations between the control group (5.1 and
5.4 mM) and the HS group (5.2 and 5.5 mM; Table I). Micro-PET/CT showed that in the
control group, the uptake and dispersion of the radionuclide
imaging agent occurred only in the skeletal muscles and brain,
which are metabolically active organs (Fig. 1A). In the HS model, the intestine
was diversely metabolically activated, and the integrity of the
intestinal barrier may be disrupted, as indicated by the
accumulation of the imaging agent in the intestinal barrier, which
led to the release of bacteria and endotoxins into the circulation,
influencing the whole body. The radionuclide imaging agent had also
accumulated in the liver, brain, and kidneys, indicating the
presence of SIRS and MODS. Moreover, it was noted that in the HS
group, the kidneys were more active than the other organs (Fig. 1B).
 | Table I.Change in blood glucose and
creatinine levels in the study groups. |
Table I.
Change in blood glucose and
creatinine levels in the study groups.
| Group | Glucose,
mmol/l | Serum creatinine,
umol/l |
|---|
| Control | 5.26±1.63 | 11.47±3.91 |
| Heat stroke | 5.34±1.92 |
20.53±4.75a |
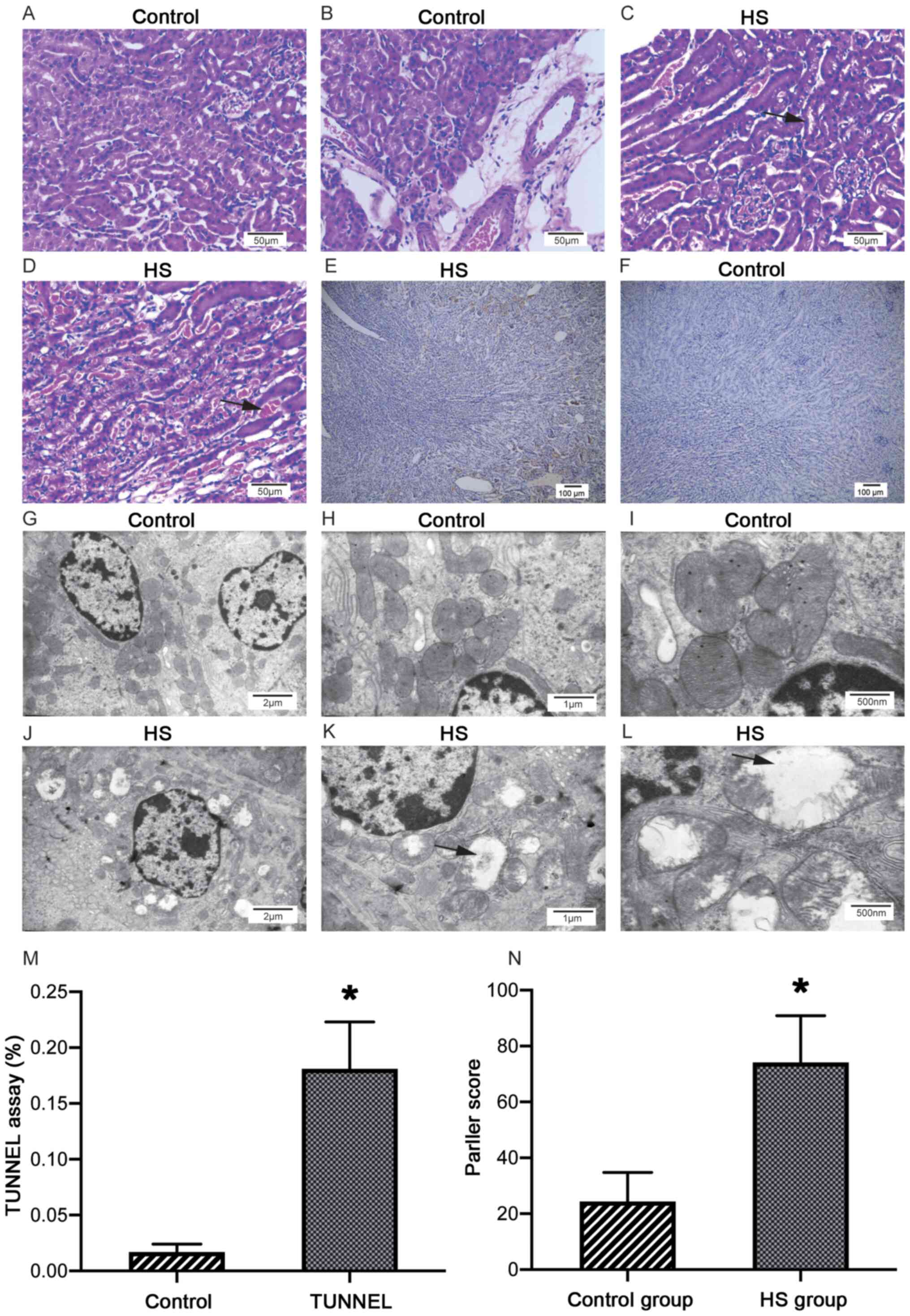
HS triggers AKI in mice
The plasma creatinine level was significantly
upregulated in the HS group compared with the control group
(P<0.05; Table I). In the HS
group, H&E staining revealed glomerular swelling, inflammatory
cell infiltration, vacuolar degeneration of endothelial cells and
red blood cells in renal tubules, which is a characteristic sign of
hyperemia and indicates a high risk of hemorrhage (Fig. 2C and D). All these changes were not
present in the control group (Fig. 2A
and B). The TUNEL assay revealed yellow-stained nuclei of
apoptotic cells primarily located in the renal tubule area in the
HS group. The number of apoptotic cells was significantly increased
in the HS group compared with in the control group (P<0.05;
Fig. 2E, F and M). Moreover, the
renal tubule injury score was significantly increased in the HS
group compared with in the control group (P<0.001; Fig. 2N). TEM revealed swollen mitochondria
with diminished inner ridges in the HS group (Fig. 2G-L). All of these changes indicated
HS-induced AKI.
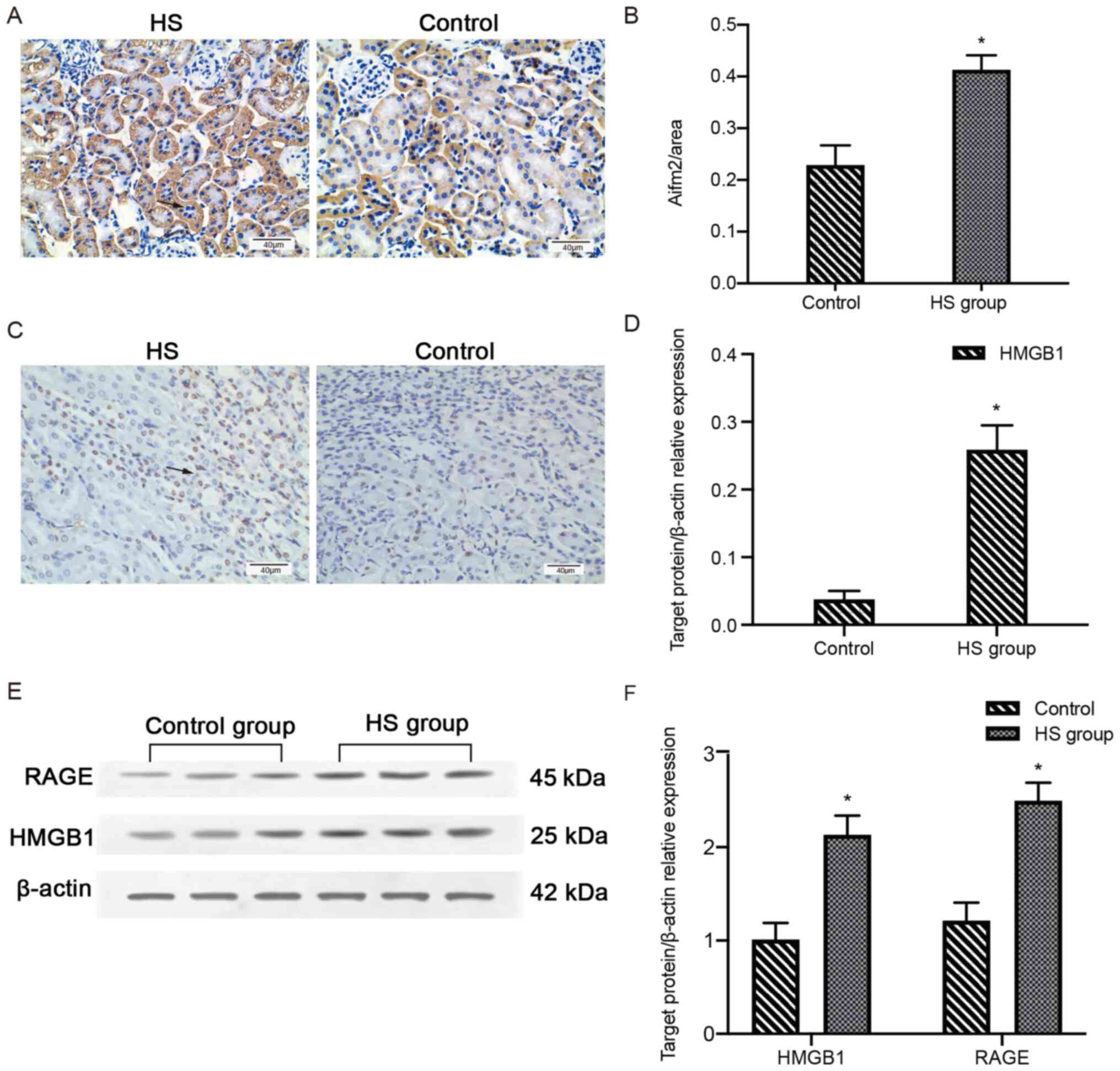
HS activates the HMGB1/RAGE
pathway
IHC staining revealed cytoplasmic expression of
Aifm2 in the kidney tissues in both groups, but the expression was
significantly increased in the HS group compared with in the
control group (P<0.05; Fig.
3A-B). HMGB1 was primarily expressed in the nuclei of the renal
tubule cells in both groups; however, HMGB1-positive cells were
abundant in the HS group and rarely observed in the control group
(P<0.05; Fig. 3C and D). Western
blot analysis revealed that the expression levels of HMGB1 and RAGE
were significantly elevated in the HS group compared with in the
control group (P<0.05; Fig. 3E and
F).
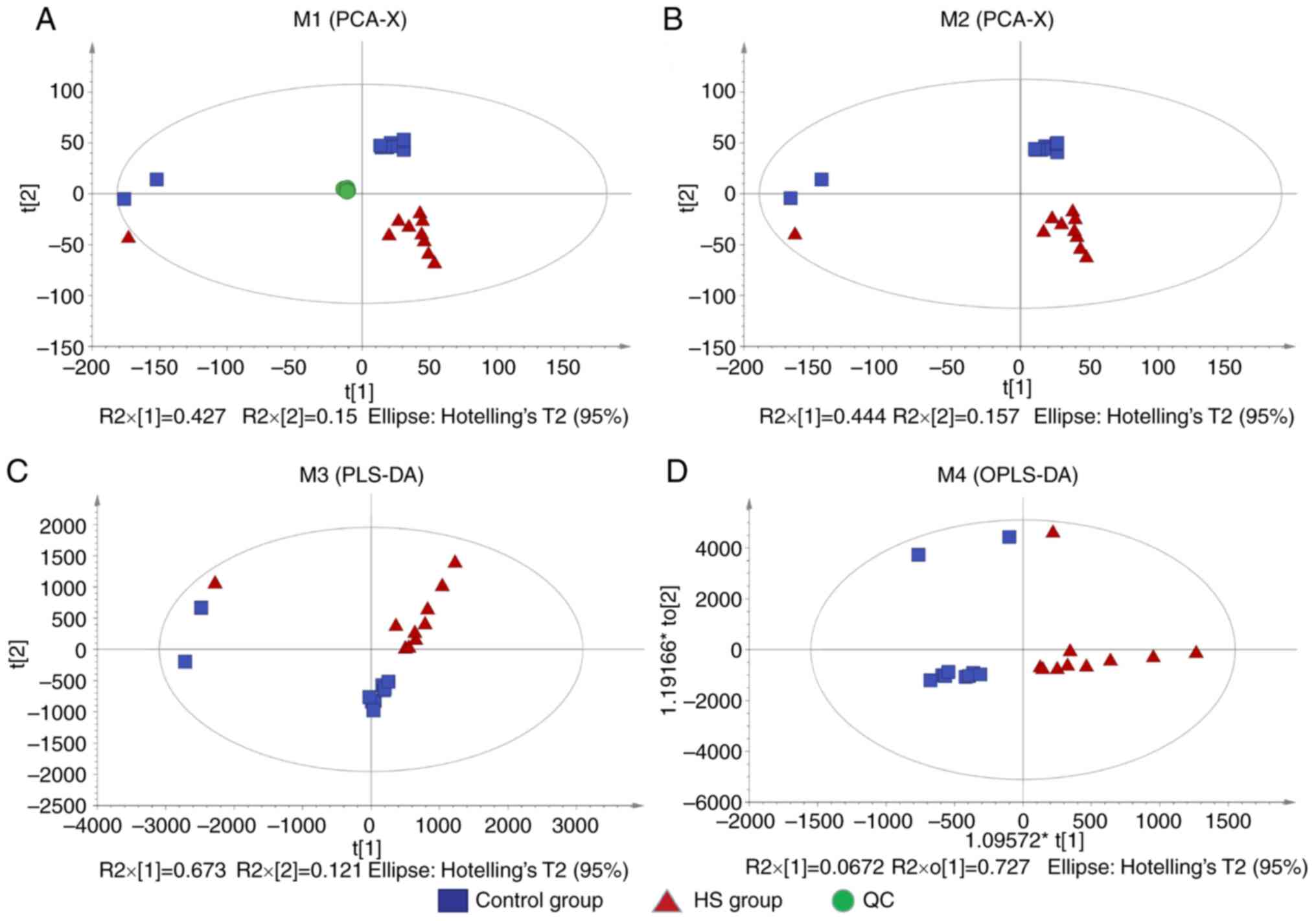
Metabolomic evaluation of HS
model
Intrinsic clustering and potential outliers were
detected using PCA. A plot of PC1 vs. PC2 scores (R2X=0.691,
Q2=0.528; Fig. 4A and B) showed
good separation between the control and HS groups, except for three
outliers. PLS-DA also showed good separation in the scatter plot
(R2X=0.794, R2Y=0.736, Q2=0.472; Fig.
4C). To minimize any potential effects of intergroup
variability and improve the between-group separation, the OPLS-DA
scores were plotted (Fig. 4D)
through LC-MS analysis of the kidney tissues, and a distinct
separation between the HS and control groups was found (R2X=0.794,
R2Y=0.736, Q2=0.006), which demonstrated a difference in kidney
metabolites between the two groups. The OPLS-DA model was selected
for the following experiment to examine variations in metabolite
profiles between the groups.
Identification of differential
metabolites and signaling pathways
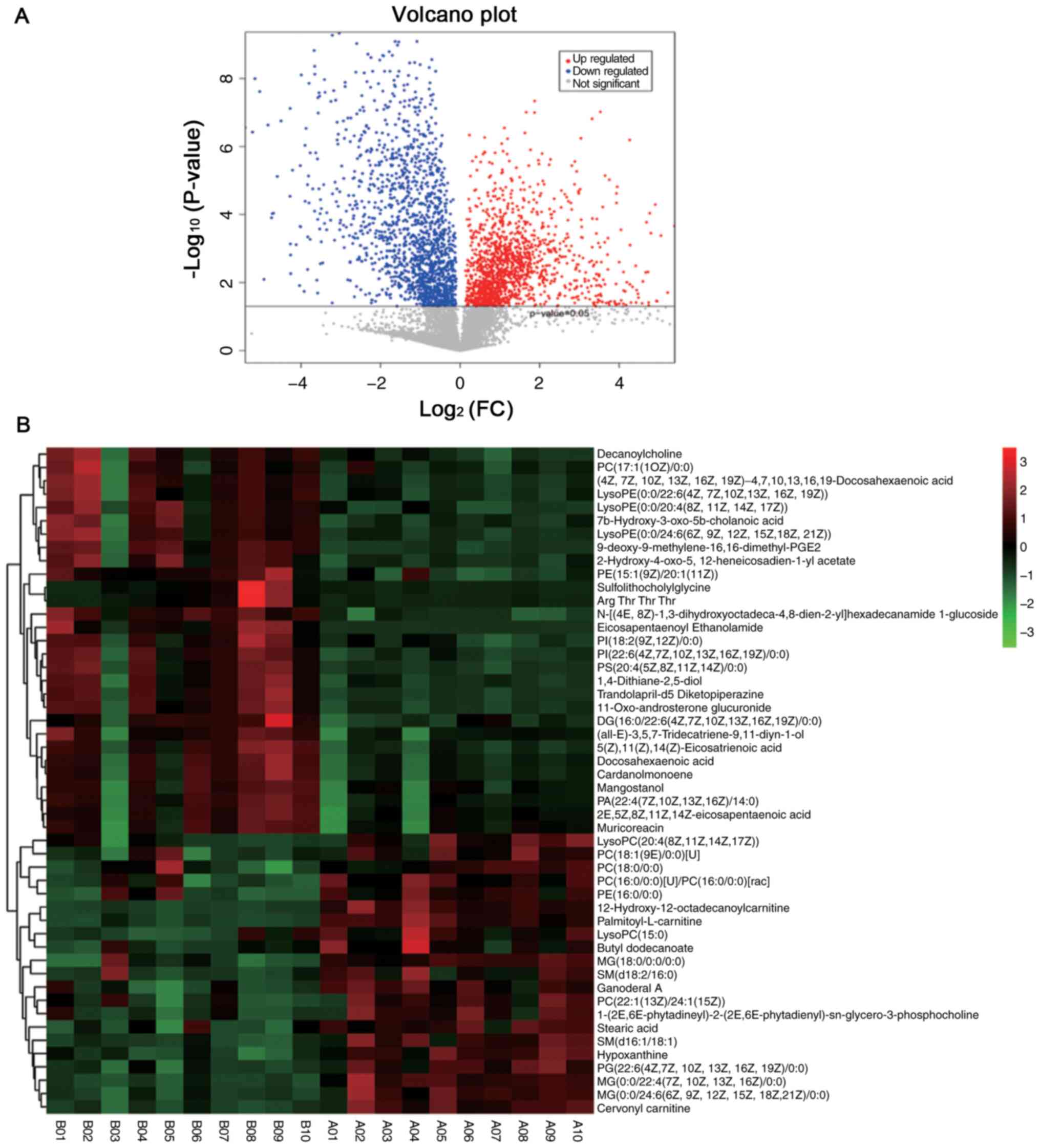
OPLS-DA models were used to identify differences in
metabolites between the control and HS groups. The HS-group cluster
was distant from the control-group cluster (Fig. 4). The results revealed that of the
136 metabolites that were differentially expressed in the HS and
control groups, 80 were upregulated and 56 were downregulated
(Fig. 5A and Table SI). The top 50 metabolites were
selected to construct a heat map, and it was found that the
differential metabolites were highly efficiently clustered in each
group (Fig. 5B). A majority of the
differential metabolites exhibited high correlation with other
different metabolites (Fig. 6A).
These results indicated that the screened-out metabolites may
cooperate with each other to induce AKI in response to HS. To
further investigate the mechanism of AKI in HS, enrichment analysis
was performed using the KEGG pathway database. The results revealed
that the ‘biosynthesis of unsaturated fatty acids’, ‘synthesis and
degradation of ketone bodies’, ‘Chagas disease’, ‘D-arginine and
D-ornithine metabolism’ and ‘amyotrophic lateral sclerosis (ALS)’
pathways were the only five signaling pathways significantly
enriched with differential metabolites (Fig. 6B). Adrenic acid, docosahexaenoic
acid (DHA), eicosapentaenoic acid (EPA), stearic acid, acetone and
L-arginine were the metabolites enriched in these signaling
pathways.
Discussion
Recently, an increasing number of studies (39–41)
focusing on high temperature-related diseases have been published,
primarily due to the continuously and rapidly increasing HS-related
morbidity and mortality rates (23). In addition to affecting the
temperature-regulation system, HS can cause several complications,
such as rhabdomyolysis, ARF, acute respiratory distress syndrome,
hepatic failure and DIC, all of which can eventually progress to
MODS, which commonly results in mortality for affected individuals
(42).
HS is considered to be to an SIRS-like disease that
is triggered by endotoxins, cytokines and other immune-regulatory
factors (43). Impaired integrity
of the intestinal barrier and increased intestinal permeability may
be the cause of these factors entering the circulation, as was
reported by a study, which revealed increased leakage of
lipopolysaccharides (LPS) and endotoxins into the circulation from
the gut during HS (44,45). Furthermore, another study found that
the use of anti-LPS antibodies can prevent this translocation
during HS (46). Translocation of
endotoxins and LPS induces the release of various cytokines and
HMGB1, a prototypic alarmin, which causes excessive activation of
leukocytes and endothelial cells, resulting in the development of
SIRS (47,48). Therefore, protecting the integrity
of the intestinal barrier appears to be important for preventing
HS. Furthermore, the combination of inflammatory factors and direct
cytotoxic effects of heat may cause injury to the vascular
endothelium, resulting in microthromboses (49). Certain authors have reported
significantly different expression of long non-coding RNAs and
their competing endogenous RNAs in exosomes secreted from human
umbilical vein endothelial cells in response to HS (50). Although these studies may identify
certain biomarkers involved in HS, the function and regulatory
mechanisms underlying the condition remain unexplored (50). In HS, microthrombosis-induced
platelet consumption and hyperthermia-induced platelet aggregation
both lead to a decreased platelet count (51). Although thrombocytopenia has been
associated with the development and prognosis of AKI in HS
(52), the precise mechanism
underlying AKI in HS remains unclear.
In the present study, a mouse model of HS was
established. Heat stress led to an increase in plasma creatinine
levels in the HS group compared with the control group. This
demonstrated that the renal function of heat-stressed mice was
impaired, and this deficiency in the HS mice may be comparable to
AKI. Micro-PET/CT scanning was used to visualize the uptake and
dispersion of 18FDG in mice. The tissue uptake of
18FDG is highly increased during states of inflammation
and hypercatabolism (53). Although
a glucose analog, 18FDG did not influence blood glucose
concentrations in the present study, indicating that it has no role
in mouse glucose metabolism. 18FDG accumulation was
noted in all organs, including the liver, intestine and kidneys, in
the HS group, which indicated that HS may induce SIRS in mice. It
was also found that 18FDG was primarily aggregated in
the kidneys, which is consistent with the increase observed in the
creatinine levels of the mice. Earlier studies have investigated
the pathogenesis of HS mainly in terms of systemic inflammation
(54) or nervous system protection
(55). The present study aimed to
acquire a deeper understanding of the mechanisms underlying
HS-induced AKI, which has been rarely studied and could provide
novel insight.
HMGB1, also known as alarmin, is a gene
transcription cofactor and a damage-associated molecular pattern
molecule that mediates proinflammatory effects by activating
multiple cell surface receptors, such as RAGE and Toll-like
receptors (56). This
proinflammatory role is relevant to the pathogenesis of several
kidney diseases, including AKI (57). HMGB1 is also considered to be
involved in the pathogenesis of HS, as increased serum HMGB1 levels
indicate poor prognosis in HS (48). Inhibiting the HMGB1/RAGE pathway may
aid in the treatment of AKI, although its role in HS-related AKI is
unclear (58). It was observed that
both HMGB1 and RAGE were significantly upregulated in the kidneys
of HS mice. Furthermore, both the TUNEL assay and TEM scanning
suggested that mitochondrial-dependent apoptosis had occurred in
the kidneys of HS mice, which was supported by the upregulation of
Aifm2, a gene involved in mitochondrial-dependent apoptosis
(59). As the HMGB1/RAGE pathway
may trigger mitochondria-related apoptosis in inflammatory states
(60), it is hypothesized that the
apparent increase in renal tubular epithelial cell apoptosis
observed in the present study was caused, at least partly, by the
HMGB1/RAGE pathway. However, pathological examination indicated
renal tubular hyperemia and edema, instead of apoptosis. A previous
study has reported the occurrence of severe pulmonary hemorrhage in
patients who died of HS; however, kidney injury due to HS was not
mentioned (61). Hence, it is
proposed that bleeding, rather than apoptosis, may be a
characteristic feature of HS-associated AKI. Moreover, HS-induced
SIRS and secondary hyperfibrinolysis may be other reasons for
hyperemia and edema in the kidneys, which were different from the
reported manifestations of common acute tubular necrosis (23). Dysregulation of the HMGB1/RAGE
pathway may be involved in this process (62), but the specific mechanism needs to
be elucidated.
In present study, metabolomics analysis of the
animal model was conducted to further explore the pathogenesis of
HS. Of the 136 differential metabolites, 80 metabolites were
upregulated and 56 were downregulated. The top 15 differential
metabolites were associated with fatty acid metabolism and other
associated metabolic pathways, which may induce early changes in
the kidneys during HS. Additionally, the correlation among a number
of the top 50 metabolites was strong, indicating their probable
interplay in inducing AKI in response to HS. Enrichment analysis of
all the differential metabolites was performed, and ‘biosynthesis
of unsaturated fatty acids’, ‘synthesis and degradation of ketone
bodies’, ‘Chagas disease’, ‘D-arginine and D-ornithine metabolism’
and ‘ALS’ were the only five significantly enriched signaling
pathways between the two groups. Adrenic acid, DHA and EPA, which
are involved in the ‘biosynthesis of unsaturated fatty acids’
pathway, were upregulated in the HS group. This may appear to be in
contrast to a previous study, which reported the synergistic
functioning of DHA and EPA to protect intestinal barrier integrity
in HS (63). However, these are, in
fact, two phases of a process. HS can damage the intestine barrier
to allow the seepage of unsaturated fatty acids, which are
important components of cell membranes, into the urinary system,
leading to an increase in their levels in the urinary system. As
DHA and EPA treatment prevents the disruption of the intestinal
barrier, fewer metabolites, such as unsaturated fatty acids, flow
into the circulation to initiate inflammatory processes, and the
damage caused by HS is limited. As reported previously, the
HMGB1/RAGE pathway may be a potential target for unsaturated fatty
acids or regulate the concentration of unsaturated fatty acids in
other diseases via various means (64,65).
At present, the relationship between the HMGB1/RAGE pathway and
unsaturated fatty acids remains unclear, and further studies are
required.
The present study has certain limitations. First,
for a more in-depth investigation of the mechanisms underlying
HS-related AKI, multiple observation time points should be used,
such as 15 and 30 min, and 1 and 2 h; this will be explored in
subsequent studies. Second, the correlations between metabolic
changes and alterations in signaling pathways should be verified
using gain-or-loss experiments. Third, as HS is a complex disease
that involves alterations in diverse signaling pathways,
therapeutic interventions targeting the HMGB1/RAGE pathway or
biosynthesis of unsaturated fatty acids could be added in future
studies into HS.
In summary, the present study suggested that
HS-associated AKI is the most common result of HS-induced SIRS, and
may be associated with the HMGB1/RAGE pathway. Furthermore, a
feedback loop between the HMGB1/RAGE pathway and the biosynthesis
of unsaturated fatty acids may contribute to the progression of
HS-related AKI. Therefore, it is of great importance to elucidate
the relationship between the HMGB1/RAGE pathway and disordered
unsaturated fatty acid metabolism in the pathogenesis of
HS-associated AKI.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
The study was supported by National Natural Science
Foundation of China (grant no. 81200533), Sichuan Clinical Research
Center for Nephropathy (grant no. 2019YFS0537-4) and Luzhou
Municipal Government-Southwest Medical University Strategic
Cooperation Fund (grant no. 2016LZXNYD-J20).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LX and WW designed the study and participated in
animal experiments. LX and WG participated in the study design and
drafting the manuscript. LL and SO were responsible for statistical
analysis of the metabolomic data. TZ performed in vivo
animal experiments. LC and WD performed PET/CT scanning and data
analysis. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
All animal experiments complied with the guidelines
of the Animal Care and Use Committee of the Southwest Medical
University. The study protocol was approved by the same
committee.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
18FDG
|
18F-deoxyglucose
|
|
ALS
|
amyotrophic lateral sclerosis
|
|
AKI
|
acute kidney injury
|
|
ARF
|
acute renal failure
|
|
DIC
|
disseminated intravascular
coagulation
|
|
DHA
|
docosahexaenoic acid
|
|
EHS
|
exertional heat stroke
|
|
EPA
|
eicosapentaenoic acid
|
|
HMGB1
|
high-mobility group box 1
|
|
HS
|
heat stroke
|
|
IHC
|
immunohistochemistry
|
|
LC-MS
|
liquid chromatography-mass
spectrometry
|
|
LPS
|
lipopolysaccharides
|
|
micro-PET/CT
|
micro-positron emission
tomography-computed tomography
|
|
MODS
|
multiple organ dysfunction
syndrome
|
|
NEHS
|
non-exertional HS
|
|
OPLS-DA
|
orthogonal partial least squares
discriminant analysis
|
|
PCA
|
principal component analysis
|
|
RAGE
|
receptor for advanced glycosylation
end products
|
|
SIRS
|
systemic inflammatory response
syndrome
|
|
TEM
|
transmission electron microscopy
|
References
|
1
|
Laitano O, Murray KO and Leon LR:
Overlapping mechanisms of exertional heat stroke and malignant
hyperthermia: Evidence vs.conjecture. Sports Med. 50:1581–1592.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gaudio FG and Grissom CK: Cooling methods
in heat stroke. J Emerg Med. 50:607–616. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Barriopedro D, Fischer EM, Luterbacher J,
Trigo RM and Garcia-Herrera R: The hot summer of 2010: Redrawing
the temperature record map of Europe. Science. 332:220–224. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kovats RS and Kristie LE: Heatwaves and
public health in Europe. Eur J Public Health. 16:592–599. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Argaud L, Ferry T, Le QH, Marfisi A,
Ciorba D, Achache P, Ducluzeau R and Robert D: Short- and long-term
outcomes of heatstroke following the 2003 heat wave in Lyon,
France. Arch Intern Med. 167:2177–2183. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Roux-Buisson N, Monnier N, Sagui E, Abriat
A, Brosset C, Bendahan D, Kozak-Ribbens G, Gazzola S, Quesada JL,
Foutrier-Morello C, et al: Identification of variants of the
ryanodine receptor type 1 in patients with exertional heat stroke
and positive response to the malignant hyperthermia in vitro
contracture test. Br J Anaesth. 116:566–568. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yang M, Zhang Y, Zhao Y and Kang H:
Research progress in the multiple organ dysfunction syndrome caused
by heat stroke. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 29:188–192.
2017.(In Chinese). PubMed/NCBI
|
|
8
|
Chen CM, Hou CC, Cheng KC, Tian RL, Chang
CP and Lin MT: Activated protein C therapy in a rat heat stroke
model. Crit Care Med. 34:1960–1966. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ren MQ, Kazman JB, Abraham PA, Atias-Varon
D, Heled Y and Deuster PA: Gene expression profiling of humans
under exertional heat stress: Comparisons between persons with and
without exertional heat stroke. J Therm. 85:1024232019.
|
|
10
|
Lumlertgul D, Chuaychoo B, Thitiarchakul
S, Srimahachota S, Sangchun K and Keoplung M: Heat stroke-induced
multiple organ failure. Ren Fail. 14:77–80. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Deutsch M, Koskinas J, Emmanuel T,
Kountouras D and Hadziyannis S: Heat stroke and multi-organ failure
with liver involvement in an asylum-seeking refugee. J Emerg Med.
31:255–257. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
McGeehin MA and Mirabelli M: The potential
impacts of climate variability and change on temperature-related
morbidity and mortality in the United States. Environ Health
Perspect. 109 (Suppl 2):S185–S189. 2001. View Article : Google Scholar
|
|
13
|
Bouchama A and Knochel JP: Heat stroke. N
Engl J Med. 346:1978–1988. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Woodrow G, Brownjohn AM and Turney JH: The
clinical and biochemical features of acute renal failure due to
rhabdomyolysis. Ren Fail. 17:467–474. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chen GM, Chen YH, Zhang W, Yu Y, Chen JH
and Chen J: Therapy of severe heatshock in combination with
multiple organ dysfunction with continuous renal replacement
therapy: A clinical study. Medicine (Baltimore). 94:e12122015.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Inoue N, Sato A, Ikawa Y, Shimizu M,
Okajima M, Taniguchi T and Yachie A: Successful treatment of
exertional heat stroke using continuous plasma diafiltration. J
Clin Apher. 31:490–492. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hamaya H, Hifumi T, Kawakita K, Okazaki T,
Kiridume K, Shinohara N, Abe Y, Takano K, Hagiike M and Kuroda Y:
Successful management of heat stroke associated with multiple-organ
dysfunction by active intravascular cooling. Am J Emerg Med.
33:124.e5–e7. 2015. View Article : Google Scholar
|
|
18
|
Ye J, Mo W, Chen Y and Yang A: An analysis
of laboratory results of parameters of organ function in patients
with heat stroke. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue.
27:658–661. 2015.(In Chinese). PubMed/NCBI
|
|
19
|
Zhao JJ, Zhou JJ, Hu J, Zhou FH, Kang HJ,
Liu H, Pan L and Song Q: Analysis of risk factors affecting
prognosis of exertional heat stroke. Zhonghua Wei Zhong Bing Ji Jiu
Yi Xue. 25:515–518. 2013.PubMed/NCBI
|
|
20
|
Segev G, Bruchim Y, Berl N, Cohen A and
Aroch I: Effects of fenoldopam on kidney function parameters and
its therapeutic efficacy in the management of acute kidney injury
in dogs with heatstroke. J Vet Intern Med. 32:1109–1115. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Peng N, Geng Y, Zhang S, Tang Y, Wen Q,
Tong H, Liu Y, Liu Z and Su L: Correlation of kidney injury and
inflammatory response in rats with classic severe heatstroke.
Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 27:327–331. 2015.(In
Chinese). PubMed/NCBI
|
|
22
|
Protasi F, Paolini C and Dainese M:
Calsequestrin-1: A new candidate gene for malignant hyperthermia
and exertional/environmental heat stroke. J Physiol. 587:3095–3100.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Leon LR and Helwig BG: Heat stroke: Role
of the systemic inflammatory response. J Appl Physiol (1985).
109:1980–1988. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Roberts GT, Ghebeh H, Chishti MA,
Al-Mohanna F, El-Sayed R, Al-Mohanna F and Bouchama A:
Microvascular injury, thrombosis, inflammation, and apoptosis in
the pathogenesis of heatstroke: A study in baboon model.
Arterioscler Thromb Vasc Biol. 28:1130–1136. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Rosendal L, Langberg H, Skov-Jensen A and
Kjaer M: Incidence of injury and physical performance adaptations
during military training. Clin J Sport Med. 13:157–163. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Yang PC, He SH and Zheng PY: Investigation
into the signal transduction pathway via which heat stress impairs
intestinal epithelial barrier function. J Gastroenterol Hepatol.
22:1823–1831. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Mittal R and Coopersmith CM: Redefining
the gut as the motor of critical illness. Trends Mol Med.
20:214–223. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Clayton TA, Lindon JC, Cloarec O, Antti H,
Charuel C, Hanton G, Provost JP, Le Net JL, Baker D, Walley RJ, et
al: Pharmaco-metabonomic phenotyping and personalized drug
treatment. Nature. 440:1073–1077. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kork F, Holthues J, Hellweg R, Jankowski
V, Tepel M, Ohring R, Heuser I, Bierbrauer J, Peters O, Schlattmann
P, et al: A possible new diagnostic biomarker in early diagnosis of
Alzheimer's disease. Curr Alzheimer Res. 6:519–524. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Laitano O, Garcia CK, Mattingly AJ,
Robinson GP, Murray KO, King MA, Ingram B, Ramamoorthy S, Leon LR
and Clanton TL: Delayed metabolic dysfunction in myocardium
following exertional heat stroke in mice. J Physiol. 598:967–985.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Li Y, Zhu X, Zhang M, Tong H and Su L:
Heatstroke-induced hepatocyte exosomes promote liver injury by
activating the NOD-like receptor signaling pathway in mice. PeerJ.
7:e82162019. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Tai PA, Chang CK, Niu KC, Lin MT, Chiu WT
and Lin JW: Reduction of ischemic and oxidative damage to the
hypothalamus by hyperbaric oxygen in heatstroke mice. J Biomed
Biotechnol. 2010:6095262010. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Umemura Y, Ogura H, Matsuura H, Ebihara T,
Shimizu K and Shimazu T: Bone marrow-derived mononuclear cell
therapy can attenuate systemic inflammation in rat heatstroke.
Scand J Trauma Resusc Emerg Med. 26:972018. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Yeh CH, Chen ZC, Hsu CC, Lin MT and Chen
CC: Protection in rats with heatstroke: Hyperbaric oxygen vs
activated protein C therapy. Eur J Pharmacol. 635:103–108. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Yayi H, Yeda X, Huaxin W, Yang W, Qian S
and Zhongyuan X: Toll-like receptor 7 involves the injury in acute
kidney ischemia/reperfusion of STZ-induced diabetic rats. Acta Cir
Bras. 31:448–455. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Satirapoj B, Kongthaworn S, Choovichian P
and Supasyndh O: Electrolyte disturbances and risk factors of acute
kidney injury patients receiving dialysis in exertional heat
stroke. BMC Nephrol. 17:552016. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
López-Ibáñez J, Pazos F and Chagoyen M:
MBROLE 2.0-functional enrichment of chemical compounds. Nucleic
Acids Res. 44((W1)): W201–W204. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Kanehisa M, Sato Y, Furumichi M, Morishima
K and Tanabe M: New approach for understanding genome variations in
KEGG. Nucleic Acids Res. 47(D1): D590–D595. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Alele F, Malau-Aduli B, Malau-Aduli A and
Crowe M: Systematic review of gender differences in the
epidemiology and risk factors of exertional heat illness and heat
tolerance in the armed forces. BMJ Open. 10:e0318252020. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Li L, Tan H, Zou Z, Gong J, Zhou J, Peng
N, Su L, Maegele M, Cai D and Gu Z: Preventing necroptosis by
scavenging ROS production alleviates heat stress-induced intestinal
injury. Int J Hyperthermia. 37:517–530. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Thongprayoon C, Qureshi F, Petnak T,
Cheungpasitporn W, Chewcharat A, Cato LD, Boonpheng B, Bathini T,
Hansrivijit P, Vallabhajosyula S and Kaewput W: Impact of acute
kidney injury on outcomes of hospitalizations for heat stroke in
the United States. Diseases. 8:282020. View Article : Google Scholar
|
|
42
|
Weigand K, Riediger C, Stremmel W,
Flechtenmacher C and Encke J: Are heat stroke and physical
exhaustion underestimated causes of acute hepatic failure? World J
Gastroenterol. 13:306–309. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Hu J, Kang HJ, Liu C, Hu P, Yang MM and
Zhou FH: Response of regulatory T cells to classic heat stroke in
mice. Exp Ther Med. 16:4609–4615. 2018.PubMed/NCBI
|
|
44
|
Shapiro Y, Alkan M, Epstein Y, Newman F
and Magazanik A: Increase in rat intestinal permeability to
endotoxin during hyperthermia. Eur J Appl Physiol Occup Physiol.
55:410–412. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Gathiram P, Wells MT, Raidoo D, Brock-Utne
JG and Gaffin SL: Portal and systemic plasma lipopolysaccharide
concentrations in heat-stressed primates. Circ Shock. 25:223–230.
1988.PubMed/NCBI
|
|
46
|
Gathiram P, Wells MT, Brock-Utne JG and
Gaffin SL: Antilipopolysaccharide improves survival in primates
subjected to heat stroke. Circ Shock. 23:157–164. 1987.PubMed/NCBI
|
|
47
|
Huisse MG, Pease S, Hurtado-Nedelec M,
Arnaud B, Malaquin C, Wolff M, Gougerot-Pocidalo MA, Kermarrec N,
Bezeaud A, Guillin MC, et al: Leukocyte activation: The link
between inflammation and coagulation during heatstroke. A study of
patients during the 2003 heat wave in Paris. Crit Care Med.
36:2288–2295. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Tong HS, Tang YQ, Chen Y, Qiu JM, Wen Q
and Su L: Early elevated HMGB1 level predicting the outcome in
exertional heatstroke. J Trauma. 71:808–814. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Pozner RG, Ure AE, Jaquenod de Giusti C,
D'Atri LP, Italiano JE, Torres O, Romanowski V, Schattner M and
Gómez RM: Junín virus infection of human hematopoietic progenitors
impairs in vitro proplatelet formation and platelet release via a
bystander effect involving type I IFN signaling. PLoS Pathog.
6:e10008472010. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Chen HS, Tong HS, Zhao Y, Hong CY, Bin JP
and Su L: Differential expression pattern of exosome long
non-coding RNAs (lncRNAs) and MicroRNAs (miRNAs) in vascular
endothelial cells under heat stroke. Med Sci Monit. 24:7965–7974.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Thulesius O: Thermal reactions of blood
vessels in vascular stroke and heatstroke. Med Princ Pract.
15:316–321. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Fan H, Zhao Y, Zhu JH, Song FC, Ye JH,
Wang ZY and Le JW: Thrombocytopenia as a predictor of severe acute
kidney injury in patients with heat stroke. Ren Fail. 37:877–881.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Michels S, Buchholz HG, Rosar F, Heinrich
I, Hoffmann MA, Schweiger S, Tüscher O and Schreckenberger M:
18F-FDG PET/CT: An unexpected case of Huntington's disease. BMC
Neurol. 19:782019. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Wan Y, Sun SS, Fu HY, Xu YK, Liu Q, Yin JT
and Wan B: Adjuvant rhubarb alleviates organs dysfunction and
inhibits inflammation in heat stroke. Exp Ther Med. 16:1493–1498.
2018.PubMed/NCBI
|
|
55
|
Yang TH, Shih MF, Wen YS, Ho WY, Leu KL,
Wang MY and Liu CC: Attenuation of circulatory shock and cerebral
ischemia injury in heat stroke by combination treatment with
dexamethasone and hydroxyethyl starch. Exp Transl Stroke Med.
2:192010. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Kurts C, Panzer U, Anders HJ and Rees AJ:
The immune system and kidney disease: Basic concepts and clinical
implications. Nat Rev Immunol. 13:738–753. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Chen Q, Guan X, Zuo X, Wang J and Yin W:
The role of high mobility group box 1 (HMGB1) in the pathogenesis
of kidney diseases. Acta Pharm Sin B. 6:183–188. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Liu GQ, Zuo XH, Jiang LN, Zhang YP, Zhang
LM, Zhao ZG and Niu CY: Inhibitory effect of post-hemorrhagic shock
mesenteric lymph drainage on the HMGB1 and RAGE in mouse kidney.
Ren Fail. 38:131–136. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Miriyala S, Thippakorn C, Chaiswing L, Xu
Y, Noel T, Tovmasyan A, Batinic-Haberle I, Vander Kooi CW, Chi W,
Latif AA, et al: Novel role of 4-hydroxy-2-nonenal in
AIFm2-mediated mitochondrial stress signaling. Free Radic Biol Med.
91:68–80. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Qin S, Wang H, Yuan R, Li H, Ochani M,
Ochani K, Rosas-Ballina M, Czura CJ, Huston JM, Miller E, et al:
Role of HMGB1 in apoptosis-mediated sepsis lethality. J Exp Med.
203:1637–1642. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Adato B, Dubnov-Raz G, Gips H, Heled Y and
Epstein Y: Fatal heat stroke in children found in parked cars:
Autopsy findings. Eur J Pediatr. 175:1249–1252. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Xu L, Zhao K, Shen X, Fan XX, Ding K, Liu
RM and Wang F: Blockade of extracellular high-mobility group box 1
attenuates systemic inflammation and coagulation abnormalities in
rats with acute traumatic coagulopathy. Med Sci Monit.
22:2561–2570. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Xiao G, Yuan F, Geng Y, Qiu X, Liu Z, Lu
J, Tang L, Zhang Y and Su L: Eicosapentaenoic acid enhances
heatstroke-impaired intestinal epithelial barrier function in rats.
Shock. 44:348–356. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Wei W, Chen M, Zhu Y, Wang J, Zhu P, Li Y
and Li J: Down-regulation of vascular HMGB1 and RAGE expression by
n-3 polyunsaturated fatty acids is accompanied by amelioration of
chronic vasculopathy of small bowel allografts. J Nutr Biochem.
23:1333–1340. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Ying S, Xiao X, Chen T and Lou J: PPAR
ligands function as suppressors that target biological actions of
HMGB1. PPAR Res. 2016:26127432016. View Article : Google Scholar : PubMed/NCBI
|