Introduction
In December 2019, novel coronavirus disease 2019
(COVID-19; now termed severe acute respiratory syndrome coronavirus
2; SARS-CoV-2) infection was first reported in Wuhan, Hubei
Province, China. Since then, it has become a global pandemic. The
basic reproduction number (R0) of COVID-19 reported by Wu et
al (1) was estimated to be
2.68, indicating >two new cases were generated by a SARS-CoV-2
infected patient. Asymptomatic carriers can also infect healthy
individuals (2). Recent studies
have reported that the mortality rate of COVID-19 fluctuates
between 4.3 and 11% (3,4). Up to March 27, 2021, there were
>125 million infected individuals and 2.77 million deaths
worldwide. Given the higher mortality rate and enormous infectivity
of COVID-19, it is vital to detect suspected cases, evaluate the
disease severity and track patients with COVID-19 pneumonia in a
timely manner.
Nucleic acid detection of SARS-CoV-2 remains the
gold standard for diagnosing COVID-19 using reverse transcription
PCR (5). Chest radiology evaluation
is often key to identify suspected patients with COVID-19 (6). Prompt recognition of COVID-19 is
invaluable to ensure timely treatment, and rapid patient isolation
is crucial for containment of this communicable disease (6). Fang et al (7) reported that the sensitivity of nucleic
acid detection was 71%, whereas the sensitivity of computerized
tomography (CT) scans for SARS-CoV-2 infection was 98% in the early
stages of infection (within 3 days of the disease onset). Based on
the current understanding that chest imaging features may precede
the clinical symptoms, imaging examination is critical to detect
suspected SARS-CoV-2 infected patients (8). Ground-glass opacities (GGO), reticular
and/or interlobular septal thickening, consolidation and bilateral
lung involvement are the most frequent CT features observed
(9). To date, two reports (8,10) have
described the temporal radiological changes of COVID-19 pneumonia
for mildly and moderately affected patients.
At present, there are a limit number of published
data regarding the temporal profile of CT images. Therefore, the
present study examined the temporal changes in CT images in severe
cases of COVID-19 pneumonia.
Materials and methods
Study design and patients
The present retrospective study was performed in
Xiangyang No. 1 People's Hospital (Xiangyang, China), and consisted
of 33 severe patients (20 male patients and 13 female patients) who
had been diagnosed with COVID-19 in our hospital between January 31
and March 10, 2020. The median age was 65 years (range, 25–90
years). The diagnostic criteria and the severity of COVID-19 were
determined according to the guidance provided by the National
Health Commission of the People's Republic of China and the
National Administration of Traditional Chinese Medicine (11). The confirmed infected patients who
met the following criteria were regarded as severe patients: i)
Respiratory distress with a respiratory rate ≥30 breaths per
minute; ii) oxygen saturation ≤93% under resting conditions; and
iii) arterial blood oxygen partial pressure
(PaO2)/fraction of inspiration oxygen (FiO2)
≤300 mmHg. In addition, those patients who had a rapid progression
>50% on CT imaging within 24–48 h were also enrolled in the
present study. Children, pregnant women and patients who were
infected with other viruses or bacteria were excluded from the
present study. The present study was approved by the Ethics
Commissions of Xiangyang No. 1 People's Hospital (approval no.
2020GCP011). All enrolled patients provided informed oral consent
for the use of their samples in scientific research.
Data collection
Clinical and laboratory data were extracted from the
electronic medical records of patients by two physicians with
extensive experience (Mr. Helun Cai and Mrs. Yan Dong). Sex, age,
underlying diseases, symptoms and laboratory findings, including
leukocyte, lymphocyte, procalcitonin (PCT) and C-reactive protein
(CRP) counts, were collected at admission.
CT scans and evaluation
The time points of chest CT follow-up was based on
the development of COVID-19 in each individual patient. All CT
findings were reviewed by two radiologists (Mr. Yong Wang and Mrs.
Lisha Wang). Imaging findings were reviewed independently, and
final decisions were reached by consensus.
The following CT features were evaluated: GGO,
patchy/punctate GGO, consolidation, fibrous stripe and irregular
solid nodules. The affected maximum cross-section of each lobe was
used to assess its score on CT scans. The score of each lobe was
evaluated according to the following criteria (10): i) 0, no involvement; ii) 1, ≤25%
involvement; iii) 2, 25–50% involvement; iv) 3, 50–75% involvement;
and v) 4, >75% involvement. The degree of aggravation in
follow-up CT scans was evaluated according to the following
criteria (12): i) 1, minimal
aggravation to a lobe; ii) 2, mild aggravation to a lobe; iii) 3,
moderate aggravation to a lobe; and iv) 4, severe aggravation to a
lobe. The total scores were the sum of each lobar score. The
initial evaluation was the basis for the subsequent evaluation in
the present study. Therefore, the features in the initial chest CT
scan were highlighted.
Statistical analysis
Statistical analysis was performed using SPSS
version 22 (IBM, Corp.). Continuous variables are expressed as the
mean ± standard deviation or as the median and range. Categorical
variables are expressed as frequency rates and percentages.
Results
Patient clinical characteristics
As shown in Table I,
the most prevalent symptoms were fever (84.6%), cough (51.5%) and
shortness of breath (45.5%). Of the recruited patients, 25 had
hypertension, 9 patients had diabetes, 6 patients had
cardio-cerebrovascular diseases, 3 patients had chronic obstructive
pulmonary disease and 10 patients had >1 comorbidity. On
admission, the majority of patients had a normal leukocyte count
(28/33) and a decreased lymphocyte count (27/33). CRP and PCT
levels were above the normal range in 25 patients and 9 patients,
respectively. By April 7, 2020, 24 patients had been discharged,
and 9 patients had died. The days from the symptom onset to
admission ranged from 1–10 days. The hospital days were 13–35 days
for survivors and 6–20 days for non-survivors.
 | Table I.Demographic characteristics of the
enrolled patients (n=33). |
Table I.
Demographic characteristics of the
enrolled patients (n=33).
| Clinical
characteristics | Patients |
|---|
| Age, years | 73±15 (25–90) |
| Sex |
|
| Female, n
(%) | 13 (39.4) |
| Male, n
(%) | 20 (60.6) |
| Hospital
admission |
|
|
Survivors, days | 13–35 |
|
Non-survivors, days | 6–20 |
| Days from symptom
onset to hospital admission | 1–10 |
| Clinical
outcomes |
|
|
Discharged, n (%) | 24 (72.3) |
| Died, n
(%) | 9
(27.3) |
| Symptoms |
|
| Fever, n
(%) | 28 (84.8) |
| Cough, n
(%) | 17 (51.5) |
| Shortness
of breath, n (%) | 15 (45.5) |
| Underlying
disease |
|
|
Hypertension, n (%) | 25 (75.8) |
| Diabetes,
n (%) | 9
(27.3) |
|
Cardio-cerebrovascular
disease, n (%) | 6
(18.2) |
| COPD, n
(%) | 3 (9.1) |
| Comorbidity |
|
| Acute
respiratory distress syndrome, n (%) | 9
(27.3) |
| Acute
renal injury, n (%) | 7
(21.2) |
| Shock, n
(%) | 5
(15.2) |
| Laboratory data |
|
| PCT
increase, n (%) | 9
(27.3) |
| CRP
increase, n (%) | 25 (75.8) |
|
Lymphocyte decrease, n
(%) | 27 (82.8) |
| Leukocyte
normal, n (%) | 28 (84.5) |
Initial chest CT findings in severe
patients with COVID-19 pneumonia
As shown in Table
II, of the 33 patients, 6 (18.2%) patients had 1 affected lobe,
6 (18.2%) patients had 2 affected lobes, 5 (15.2%) patients had 3
affected lobes, 9 (27.3%) patients had 4 affected lobes and 7
(21.2%) patients had 5 affected lobes. Additionally, 29 (87.9%)
patients had GGOs, 20 (60.6%) patients had patchy GGO, 22 (66.7%)
patients had patchy consolidation, 9 (27.3%) patients had fibrous
stripes and 3 (9.1%) patients had irregular solid nodules. The
total lung severity score ranged from 1–14, with a mean score of
7.
 | Table II.Initial CT findings of the enrolled
patients (n=33). |
Table II.
Initial CT findings of the enrolled
patients (n=33).
| Parameters regarding
CT findings | Patients |
|---|
| Number of affected
lobes | Number (%) |
| 1 | 6 (18.2) |
| 2 | 6 (18.2) |
| 3 | 5 (15.2) |
| 4 | 9 (27.3) |
| 5 | 7 (21.2) |
| Total CT score, mean
± SD | 7±4 |
| CT features | Number (%) |
| GGOs | 29 (87.9) |
| Patchy
GGOs | 20 (60.6) |
| Patchy
consolidation | 22 (66.7) |
| Fibrous
stripes | 9
(27.3) |
| Solid
nodules | 3 (9.1) |
Follow-up chest CT findings in severe
patients with COVID-19 pneumonia
As shown in Table
III, five stages of lung CT scans were determined: Initial
stage (n=33), the first follow-up stage (n=33), the second
follow-up stage (n=28), the third follow-up stage (n=27) and the
fourth follow-up stage (n=5). In total, 9 non-survivors underwent
at least two chest CT scans and 24 survivors underwent >three
chest CT scans during hospitalization (data not shown). The mean
interval time between two consecutive chest CT scans was 4.5 days
(range, 3–9 days) (data not shown). At the first follow-up, no
patients demonstrated improvement, 2 (6.1%) of the 33 patients
demonstrated minimal progression, 9 (27.3%) demonstrated mild
progression, 13 (39.3%) demonstrated moderate progression and 9
patients (27.3%) demonstrated severe progression. At the second
follow-up, 28 patients received a CT scan and 5 patients were
excluded (4 patients died and 1 severe patient received an X-ray).
Of these, 2 of the 28 patients (7.1%) demonstrated disease
improvement, 5 (17.9%) demonstrated minimal progression, 10 (35.7%)
demonstrated mild progression, 8 (28.6%) demonstrated moderate
progression and 3 (10.7%) demonstrated severe progression. At the
third follow-up, 27 patients received CT scans, of which 5 patients
died, and 1 patient was discharged. Of these, 22 of the 27 patients
(81.5%) demonstrated improvement, 2 (7.4%) demonstrated minimal
progression, 2 (7.4%) demonstrated mild progression, 1 (3.7%)
demonstrated moderate progression and no patients demonstrated
severe progression. At the fourth follow-up, only 5 patients
received a CT scan (19 patients were discharged and 9 patients
died). Of the 5 patients, 2 (40%) demonstrated no changes, and 3
(60%) demonstrated disease improvement. After ~3 weeks of disease
onset, the presence of fibrous stripes and the decreased extent and
density of consolidation or GGO indicated that these patients had
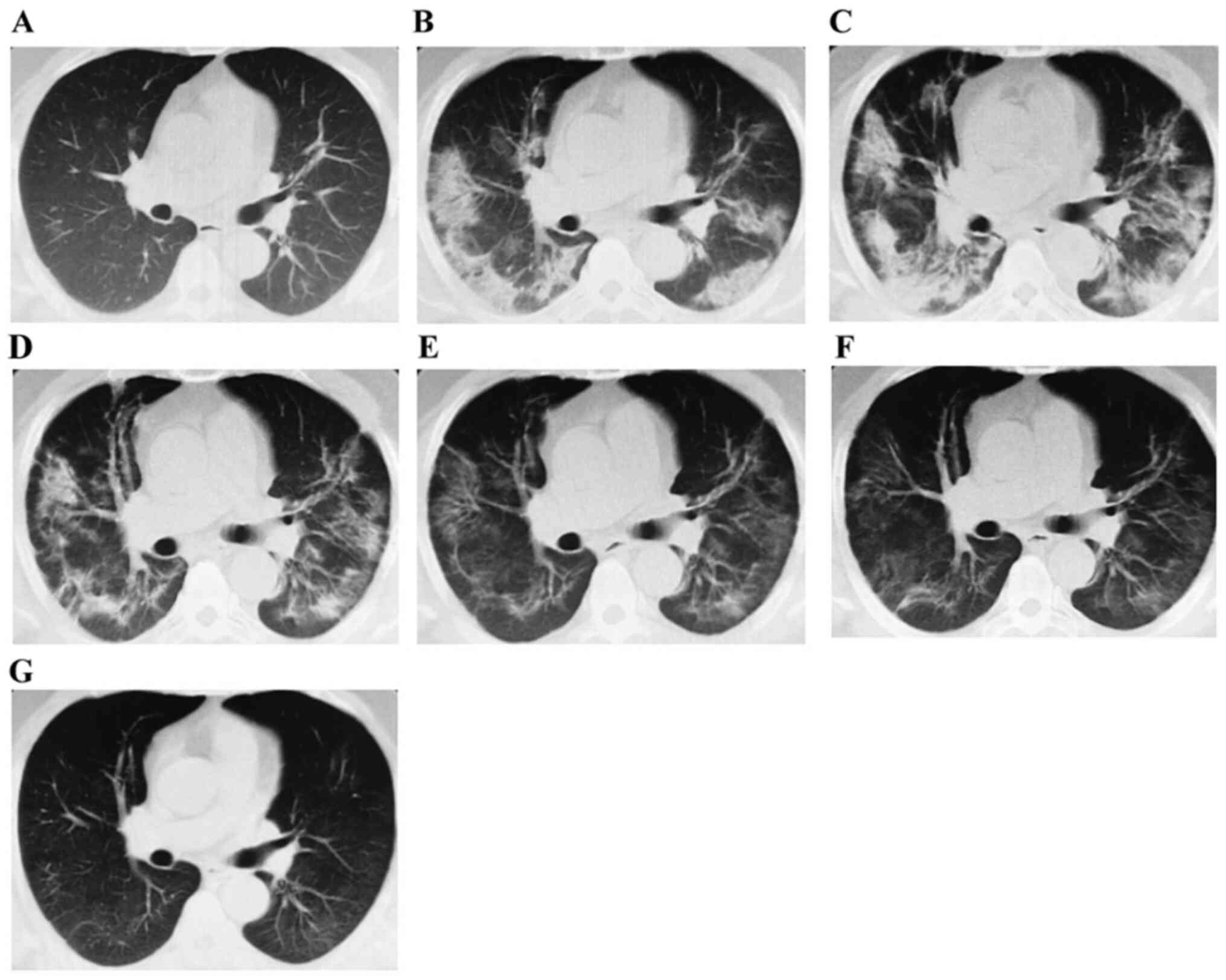
improved (Fig. 1). In detail,
Fig. 1 shows a typical temporal
process of CT findings in a severe patient (a 54-year male patient)
with novel coronavirus pneumonia. Scattered ground glass opacities
were observed in the initial stage, and then an increased range of
opacities and density of consolidation were observed 5 days after
admission. Moreover, fibrous stripes began to appear at 3 weeks
after admission, along with a deceased extent and density of
consolidation or GGOs.
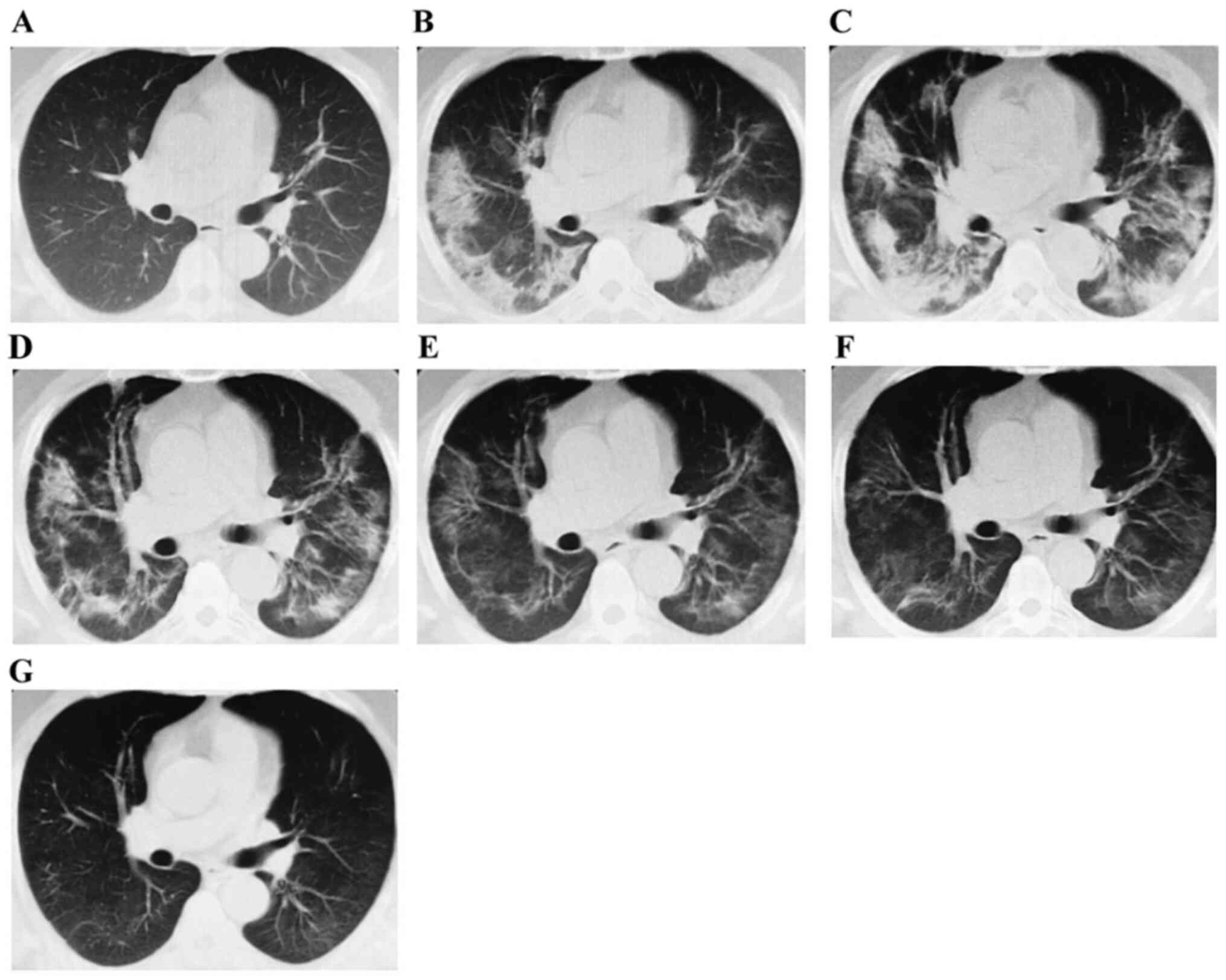 | Figure 1.Temporal profiles of CT imaging
findings of a 54-year-old male patient with novel coronavirus
pneumonia. (A) Initial CT imaging findings obtained on January 25,
2020, showed scattered ground glass opacities. (B) First follow-up
CT image, which showed an increasing range of opacities and density
of consolidation on January 30, 2020. (C) Second follow-up CT image
on February 8, 2020. (D) Third follow-up CT image on February 18,
2020. (E) Fourth follow-up CT image on February 27, 2020. (F) Fifth
follow-up CT image on March 5, 2020. (G) Sixth follow-up CT image
on April 9, 2020. CT, computerized tomography. |
 | Table III.Qualitative changes at follow-up chest
CT examination in enrolled patients (n=33). |
Table III.
Qualitative changes at follow-up chest
CT examination in enrolled patients (n=33).
|
| Follow-up CT
findings |
|---|
|
|
|
|---|
| Disease
progression | First (n=33) | Second (n=28) | Third (n=27) | Fourth (n=5) |
|---|
| No change, n (%) | 0 | 0 | 0 | 2 (40.0) |
| Disease improvement,
n (%) | 0 | 2 (7.1) | 22 (81.5) | 3 (60.0) |
| Minimal progression,
n (%) | 2 (6.1) | 5 (17.9) | 2 (7.4) | 0 |
| Mild progression, n
(%) | 9 (27.3) | 10 (35.7) | 2 (7.4) | 0 |
| Moderate progression,
n (%) | 13 (39.3) | 8 (28.6) | 1 (3.7) | 0 |
| Severe progression, n
(%) | 9 (27.3) | 3 (10.7) | 0 | 0 |
Discussion
In the present study, the majority of severe
patients were elderly adults (>60 years old, 23 elderly
patients). Fever, cough and shortness of breath were the most
common clinical manifestations. Additionally, the temporal changes
in the chest CT findings of severe patients with COVID-119
pneumonia were observed. GGO, consolidation and interlobular septal
thickening were the most common CT abnormalities. Severe patients
with COVID-19 pneumonia had features of rapid progression and slow
absorption on chest CT images. Follow-up CT examination may assist
in observing progression and identify patients at risk in a more
timely manner.
CoVs constitute a large family of viruses that
possess a single-strand, positive sense RNA genome 26–32 Kb in
length. As well-known causes of severe infections, two major
zoonotic pathogenic CoVs, SARS-CoV and Middle East Respiratory
Syndrome CoV (MERS-CoV) caused a global outbreak with far-reaching
effects on public health during 2002–2003 and in 2012, respectively
(13–15). COVID-19 is a new subtype in the CoV
family, which is 82% similar to SARS-CoV in genetic structure
(4). Although the mortality rate of
COVID-19 is less than that of SARS-CoV and MERS-CoV infection, the
total number of COVID-19 infections is increasing rapidly and has
far exceeded the previous CoV outbreaks. Asymptomatic pneumonia
with SARS-CoV-2 infection has been reported (16), and asymptomatic patients are also a
major source of transmission. Therefore, early detection and
management of these asymptomatic patients is of great
significance.
It has been previously reported that CT findings
have a higher sensitivity than PCR in the early stage of COVID-19
(4). Fang et al (7) reported the sensitivity of nucleic acid
detection was 71%, whereas the sensitivity of CT scans for
SARS-CoV-2 infection was 98% in the early stage (within 3 days from
the onset of disease). Chest CT scans are a key screening tool for
the diagnosis of patients suspected of being infected or suffering
from asymptomatic pneumonia.
In the present study, findings from imaging of
COVID-19 pneumonia are consistent with typical viral pneumonia
manifestations. The images demonstrated that the majority of
patients showed multifocal GGO along with or without consolidation
and bilateral involvement on CT findings in the early stages of the
disease, which is different from previous findings in patients with
SARS-CoV (typically unifocal lung lesion) (17). The lesions were primarily
distributed under the pleura during the initial stage and became
random or diffuse during the course of the disease in these severe
patients. Other CT abnormalities, such as pneumothorax and pleural
effusion were also observed in the present study (data not shown).
Imaging findings of viral pneumonia are varied and rapid. As the
disease progressed, the extent and density of GGO increased
gradually and consolidation began to appear. These patients showed
improvement at the third follow-up CT examination (~3 weeks after
the onset of disease), which included the presence of a fibrous
stripe and a decreased extent and density of consolidation or GGO.
At the fourth follow-up (~4 weeks after the onset of disease), most
severe patients showed notable improvement, including complete
absorption or only a few fibrous stripes remaining. Based on the
fact that patients who have recovered from MERS-infected pneumonia
have residual fibrotic changes, it was hypothesized that the
patients with COVID-19 pneumonia may also respond and heal in a
similar manner (18). In the
present study, irregular solid nodules were found during the early
stage, enlarged and merged nodules during the middle stage, and
reduced and absorbed nodules at the later stage in a few severe
patients (data not shown). Initial CT scans were performed for all
patients at admission. However, the days from symptom onset to
hospital admission were different among these patients. Therefore,
the present study tracked the temporal profiles of CT based on the
development of COVID-19.
In the present study, severe cases were primarily
observed in elderly patients. It has been reported that CT score
was positively correlated with age, the level of inflammatory
biomarkers, severity of disease, underlying co-morbidities and
disease progression (19).
Lymphopenia was observed in most patients with COVID-19, which may
be associated with the immunosenescence and the high mortality
rates. However, the exact relationship between lymphopenia,
immunosenescence and high mortality rates requires further study.
Underlying comorbidities is another factor that affects COVID-19
outcomes, particularly in elderly patients with COVID-19. These
clinical features have been extensively confirmed by numerous other
reports (19,20). Psychiatric disorders are also a
major factor of higher mortality rates. The majority of elderly
patients had mild cognitive impairment and frailty, which may
underlie the high mortality rates in elderly patients (21).
The present study has several limitations. First,
chest X-ray findings were not included in the present study. For
severe patients with invasive respiratory support, chest X-rays are
the major tool used to understand the dynamic changes in a timely
manner, thus the present study may be missing important results. A
large white lung was observed in a patient who succumbed to the
disease, which led to decreased scores at the follow-up stages.
Second, the slice thickness of CT scans was 5 or 8 mm for these
patients, which may have meant subtle features were missed. Third,
the number of enrolled patients was relatively small. Xiangyang
No.1 People's Hospital (Hubei, China) was one of the designated
hospitals for COVID-19. Some patients were admitted to other
hospitals, and the number of critically ill patients was
limited.
In summary, the present study demonstrated the
dynamic changes of CT findings in severe patients with COVID-19
pneumonia, with the intention of highlighting changes and possible
clinical manifestations in the lungs following infection. Severe
patients with COVID-19 pneumonia had features of rapid progression
and slow absorption on chest CT imaging. Chest CT scans are vital
for the early detection of suspected cases, evaluation of the
disease severity and follow-up of patients with COVID-19
pneumonia.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
PL, HC and YD conceived and designed the study. PL,
HC and YD consulted the literature, contributed to the writing of
the manuscript and final edits. LW and YW produced the figures. PL,
HC, YD and JH contributed the interpretation of the data and the
critical revision of the manuscript. All authors had accessed the
authenticity of all raw data and taken responsibility for the
authenticity of all data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Commissions of Xiangyang No. 1 People's Hospital (approval no.
2020GCP011; Xiangyang, China). All enrolled patients provided
informed oral consent for the use of their samples in scientific
research. Clinical data for all enrolled patients were collected.
This study did not interfere with the diagnosis and treatment of
each patient. The personal information of each patient will not be
disclosed.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wu JT, Leung K and Leung GM: Nowcasting
and forecasting the potential domestic and international spread of
the 2019-nCoV outbreak originating in Wuhan, China: A modelling
study. Lancet. 395:689–697. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rothe C, Schunk M, Sothmann P, Bretzel G,
Froeschl G, Wallrauch C, Zimmer T, Thiel V, Janke C, Guggemos W, et
al: Transmission of 2019-nCoV infection from an asymptomatic
contact in germany. N Engl J Med. 382:970–971. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J,
Wang B, Xiang H, Cheng Z, Xiong Y, et al: Clinical characteristics
of 138 Hospitalized patients with 2019 novel coronavirus-infected
pneumonia in Wuhan, China. JAMA. 323:1061–1069. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chen Y, Liu Q and Guo D: Emerging
coronaviruses: Genome structure, replication, and pathogenesis. J
Med Virol. 92:418–423. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chen ZM, Fu JF, Shu Q, Chen YH, Hua CZ, Li
FB, Lin R, Tang LF, Wang TL, wang W, et al: Diagnosis and treatment
recommendations for pediatric respiratory infection caused by the
2019 novel coronavirus. World J Pediatr. 16:240–246. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bernheim A, Mei X, Huang M, Yang Y, Fayad
ZA, Zhang N, Diao K, Lin B, Zhu X, Li K, et al: Chest CT findings
in coronavirus Disease-19 (COVID-19): Realtionship to duration of
infection. Radiology. 295:2004632020. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fang Y, Zhang H, Xie J, Lin M, Ying L,
Pang P and Ji W: Sensitivity of chest CT for COVID-19: Comparison
to RT-PCR. Radiology. 296:E115–E117. 2020. View Article : Google Scholar
|
|
8
|
Pan Y, Guan H, Zhou S, Wang Y, Li Q, Zhu
T, Hu Q and Xia L: Initial CT findings and temporal changes in
patients with the novel coronavirus pneumonia (2019-nCoV): A study
of 63 patients in Wuhan, China. Eur Radiol. 30:3306–3309. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Song F, Shi N, Shan F, Zhang Z, Shen J, Lu
H, Ling Y, Jiang Y and Shi Y: Emerging 2019 Novel Coronavirus
(2019-nCoV) Pneumonia. Radiology. 297:E3462020. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Pan F, Ye T, Sun P, Gui S, Liang B, Li L,
Zheng D, Wang J, Hesketh RL, Yang L, et al: Time course of lung
changes at chest CT during recovery from coronavirus disease 2019
(COVID-19). Radiology. 295:715–721. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lin L and Li TS: Interpretation of
‘Guidelines for the diagnosis and treatment of novel coronavirus
(2019-nCoV) infection by the national health commission (Trial
Version 5)’. Zhonghua Yi Xue Za Zhi. 100:805–807. 2020.(In
Chinese). PubMed/NCBI
|
|
12
|
Chung M, Bernheim A, Mei X, Zhang N, Huang
M, Zeng X, Cui J, Xu W, Yang Y, Fayad ZA, et al: CT Imaging
features of 2019 novel coronavirus (2019-nCoV). Radiology.
295:202–207. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Drosten C, Günther S, Preiser W, van der
Werf S, Brodt HR, Becker S, Rabenau H, Panning M, Kolesnikova L,
Fouchier RA, et al: Identification of a novel coronavirus in
patients with severe acute respiratory syndrome. N Engl J Med.
348:1967–1976. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ksiazek TG, Erdman D, Goldsmith CS, Zaki
SR, Peret T, Emery S, Tong S, Urbani C, Comer JA, Lim W, et al: A
novel coronavirus associated with severe acute respiratory
syndrome. N Engl J Med. 348:1953–1966. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Assiri A, Al-Tawfiq JA, Al-Rabeeah AA,
Al-Rabiah FA, Al-Hajjar S, Al-Barrak A, Flemban H, Al-Nassir WN,
Balkhy HH, Al-Hakeem RF, et al: Epidemiological, demographic, and
clinical characteristics of 47 cases of Middle East respiratory
syndrome coronavirus disease from Saudi Arabia: A descriptive
study. Lancet Infect Dis. 13:752–761. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chan JF, Yuan S, Kok KH, To KK, Chu H,
Yang J, Xing F, Liu J, Yip CC, Poon RW, et al: A familial cluster
of pneumonia associated with the 2019 novel coronavirus indicating
person-to-person transmission: A study of a family cluster. Lancet.
395:514–523. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wong KT, Antonio GE, Hui DS, Lee N, Yuen
EH, Wu A, Leung CB, Rainer TH, Cameron P, Chung SS, et al: Severe
acute respiratory syndrome: Radiographic appearances and pattern of
progression in 138 patients. Radiology. 228:401–406. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Choi WJ, Lee KN, Kang EJ and Lee H: Middle
East respiratory syndrome-coronavirus infection: A case report of
serial computed tomographic findings in a young male patient.
Korean J Radiol. 17:166–170. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Dang JZ, Zhu GY, Yang YJ and Zheng F:
Clinical characteristics of coronavirus disease 2019 in patients
aged 80 years and older. J Integr Med. 18:395–400. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H,
Wu Y, Zhang L, Yu Z, Fang M, et al: Clinical course and outcomes of
critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China:
A single-centered, retrospective, observational study. Lancet
Respir Med. 8:475–481. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
van den Berg KS, Wiersema C, Hegeman JM,
van den Brink RHS, Rhebergen D, Marijnissen RM and Oude Voshaar RC:
Clinical characteristics of late-life depression predicting
mortality. Aging Ment Health. 25:476–483. 2021. View Article : Google Scholar : PubMed/NCBI
|