Introduction
Acute respiratory tract infections (ARIs) are common
and frequently-occurring diseases in childhood. Pneumonia is
responsible for 260,000 deaths in children each year in China
(1). Mycoplasma pneumoniae
(MP) is one of the main pathogens associated with ARIs in children.
Notably, ~40% of patients with community-acquired pneumonia are
infected with MP and ~18% patients require hospitalization
(2). MP is the most common pathogen
responsible for atypical pneumonia in children, and the infection
rate increases with age. The detection rate of MP in children >6
years old is as high as 62% (3).
Most patients with MP pneumonia (MPP) recover after
treatment with macrolides or tetracycline (4); however, due to the increasing use of
antibiotics in recent years, resistant strains of MP have emerged
and the number of clinically refractory MPP cases have been
increasing annually (5,6). Refractory MPP often causes a variety
of complications that can involve multiple organs and systems, such
as atelectasis, lung necrosis, encephalitis, loss of red blood
cells and even death (7).
Therefore, the search for effective treatments for MPP,
particularly those that reduce lung injury and other complications,
has become the focus of research in numerous countries. As a
result, the Chinese medical treatment for MPP has received more
attention.
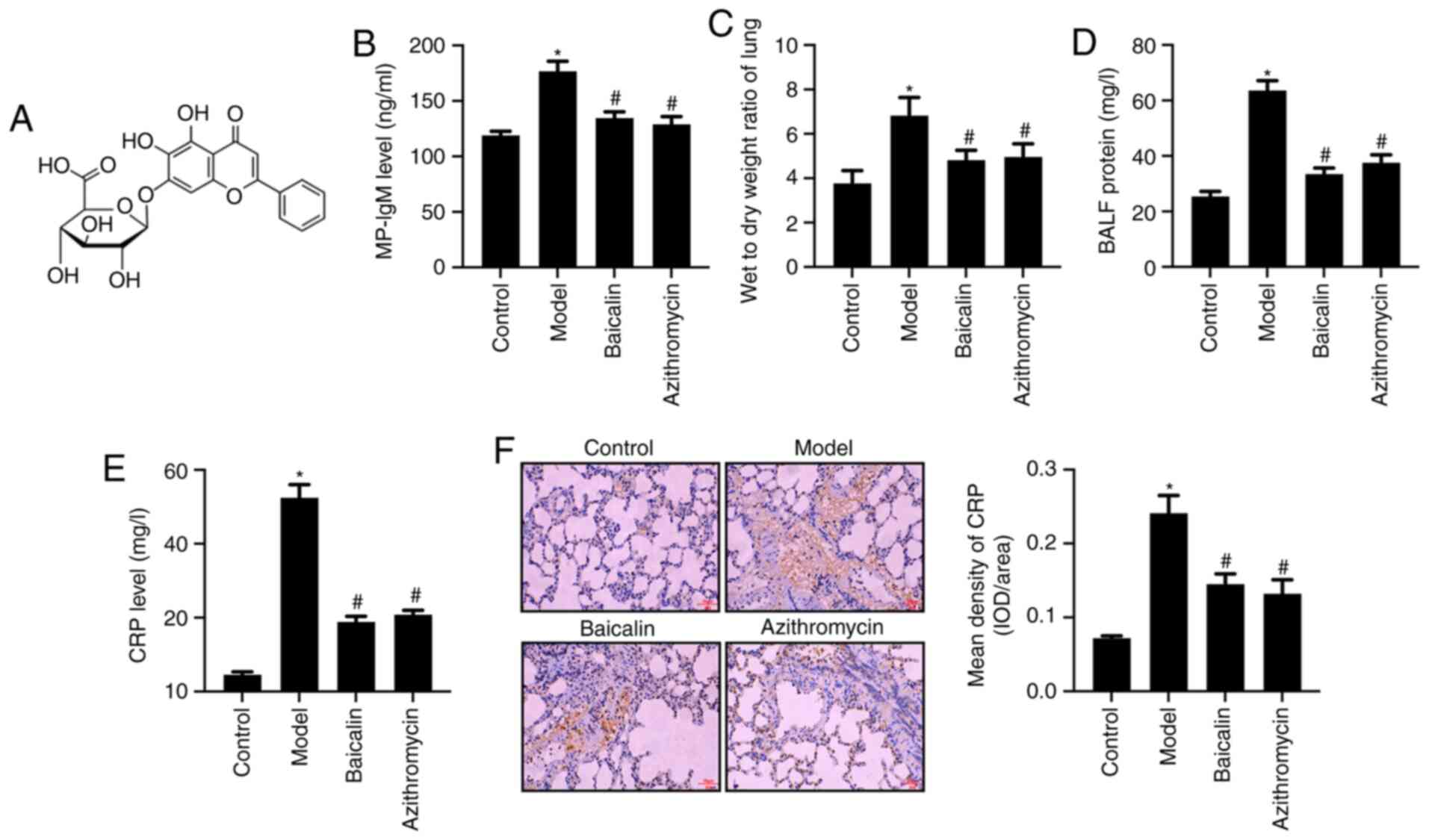
Baicalin
(C21H18O11; Fig. 1A) is a flavonoid extracted from the
dried roots of Scutellaria baicalensis Georgi.
Pharmacological studies have demonstrated that Baicalin has a
variety of therapeutic effects, including antibacterial,
anti-inflammatory, anti-allergic, diuretic, cholesterol-lowering
and antithrombotic activities (8–10). It
is clinically used for the treatment of acute and chronic
persistent hepatitis, and chronic active hepatitis, and can also be
used for the treatment of nephritis, pyelonephritis and allergic
diseases (11–13). Baicalin has been shown to regulate
the SDF-1/CXCR4 signaling pathway to inhibit hypoxia-induced
proliferation and migration of pulmonary artery smooth muscle cells
(14). Baicalin has also been shown
to exert anti-airway inflammation and resistance in a rat model of
chronic obstructive pulmonary disease (15). In addition, Baicalin may exert a
protective effect on acute lung injury caused by severe burns
(16), thus suggesting that
Baicalin has a significant protective effect on lung tissue.
However, there is little known about the potential protective
effects of Baicalin on lung injury caused by MP infection.
Although the pathogenesis of MPP is not fully
understood, it is characterized by disruption to respiratory
epithelial adsorption, immunological pathogenesis and MP invasion
(17). At present, immunological
pathology has garnered much attention (18). There are common antigenic components
in cell membranes of the body and the cell membrane glycolipid
antigen of MP (19). After MP
infection, the inflammatory response produced by macrophages,
neutrophils and lymphocytes infiltrating around the alveolar and
bronchial vessels is the pathological feature of MPP autoimmunity
(20). After MP invades the
respiratory tract, it produces a complex autoimmune response.
Neutrophils rapidly move to the site of infection and become
activated, and excessive inflammatory reactions are induced by the
production of various specific proteases. Inflammatory factors,
such as IL-1β, IL-6, IL-18 and TNF-α, are released, causing
immunological damage to lung tissue, which in turn can induce
damage to multiple organs and systems outside the lungs (21,22).
MicroRNAs (miRNAs/miRs) are a class of non-coding
RNAs that consist of 18–24 nucleotides, which can inhibit the
expression of target mRNA, and participate in cell proliferation,
differentiation and apoptosis (23). Previous studies have revealed that
miRNAs serve important regulatory roles in immune inflammatory
processes; in particular, miR-155, miR-146a, miR-221 and miR-192
have been suggested to be involved in the development and
progression of numerous inflammatory diseases (24–26).
TLRs are pattern recognition receptors that initiate
innate and acquired immunity (27).
TLR2 recognizes mycoplasma lipoproteins, whereas TLR5 and TLR6
recognize the bis-acyl lipopeptides of Mycoplasma. TLRs are
closely related to the pathogenesis of MPP (28,29).
Shimizu (30) reported that lung
inflammation was more serious in TLR2-knockout mice compared with
that in wild type mice infected with MPP; this previous study also
demonstrated that the inflammatory response was related to TLR4 and
autophagy. TLR4 could promote the sensitivity of the body to the
endotoxin inducing the release of inflammatory factors and
stimulating the immune response, indicating that TLR4 may have an
important role in the pathogenesis of MP. It has been reported that
mice overexpressing TLR4 and TLR2 genes are easily infected by
chlamydia bacteria (31).
Gram-positive cocci can synergistically interact with TLR2,
upregulate TLR4 protein expression, activate the TLR4 signaling
pathway and release the inflammatory factor IL-6, which can mediate
inflammation by regulating NF-κB signaling pathways (32,33).
Collectively, these findings suggested that miRNAs
and TLRs have a critical role in the inflammatory response caused
by MPP. The present study aimed to investigate the potential
protective effects of Baicalin treatment on MP infection-induced
lung injury and its molecular mechanism. The present study prepared
a mouse model of MPP injury, and studied the relationship between
miR-221 and the TLR4/NF-κB signaling pathway.
Materials and methods
Drug preparation and MP
cultivation
Baicalin (molecular weight, 446.36; purity,
>95.4%; batch no. 110715-201821; Fig. 1A) and azithromycin (batch no.
130609-201706) were purchased from National Institutes for Food and
Drug Control in China. Baicalin and azithromycin were dissolved in
ddH2O, prepared as a 1 mg/ml solution and stored at 4°C.
Standard MP FH (ATCC 15531) was purchased from American Type
Culture Collection, was dissolved in complete PPLO broth medium (BD
Biosciences), mixed thoroughly and incubated at 37°C. MP in the
logarithmic growth phase was quantified by color change unit (CCU)
and was adjusted to the required concentration using DMEM
containing 10% fetal bovine serum (both from Gibco; Thermo Fisher
Scientific, Inc.) (34).
Animal grouping and preparation of MPP
model mice
Female BALB/C mice (age, 4–6 weeks; weight, 15±1 g)
were purchased from Beijing Vital River Laboratory Animal
Technology Co., Ltd., and bred and housed at the animal center at
China Medical University. Mice were housed at 21°C, 55% humidity,
under a 12-h light/dark cycle with free access to food and water.
Mice were randomly divided into the following seven groups
(n=10/group): Control group, MPP model group, Baicalin group,
azithromycin group, miR-221 mimic group, miR-221 negative control
group and Baicalin + miR-221 mimic group. Mice were housed and
maintained in cages containing five mice/cage. To induce MP
infection, each mouse was anesthetized by intraperitoneal injection
of 40 mg/kg pentobarbital (Nembutal; Sumitomo Dainippon Pharma Co.,
Ltd.) (35). Once anesthetized, the
mice in the control group were treated with saline. The mice in all
other groups were intranasally inoculated with 50 µl MP solution
containing 1×1010 CCU/l. This procedure was performed
once a day for 3 consecutive days to prepare an MPP model (36). After the last MP inoculation, mice
in the treatment groups were intragastrically injected with 80
mg/kg Baicalin or 22.5 mg/kg azithromycin. Mice in the MPP model
group and the control group were intraperitoneally injected with
the same amount of saline. Mice in the miR-221 mimic group, miR-221
negative control group and Baicalin + miR-221 mimic group received
100 µl miR-221 mimic lentivirus or miR-221 negative control
lentivirus at concentration of 1×108 TU/ml by intranasal
infusion for 7 consecutive days (37). The miR-221 mimic and negative
control sequences are shown in Table
I. Lentiviruses containing miR-221-mimics and miR-221-negative
control were constructed and synthesized by Shanghai GenePharma
Co., Ltd.. Blood samples were collected by cardiac puncture into
ETDA-containing plasma separation tubes (BD Biosciences) after
anesthesia with 40 mg/kg sodium pentobarbital. Subsequently, mice
were euthanized with 120 mg/kg sodium pentobarbital
(intraperitoneal) and necropsied immediately. The bronchoalveolar
lavage fluid (BALF) and lung tissues of mice were collected and
stored at −80°C for further experiments. The animal experiments
were approved by the Institutional Animal Care and Use Committee
(IACUC) of China Medical University (IACUC no. CMU2018309;
Shenyang, China).
 | Table I.Sequences of miR-221 mimics and
negative control. |
Table I.
Sequences of miR-221 mimics and
negative control.
| Name | Sequence
(5′-3′) |
|---|
| miR-221 mimics |
AGCUACAUUGUCUGCUGGGUUUC |
| miR-221 negative
control |
UUCUCCGAACGUGUCACGUTT |
ELISA of serum levels of
MP-immunoglobulin (Ig)M and C-reactive protein (CRP)
The serum levels of MP-IgM (cat. no. SEA543Mu; Wuhan
USCN Business Co., Ltd.) and CRP (cat. no. SEA821Mu; Wuhan USCN
Business Co., Ltd.) in mice were determined using ELISA kits,
according to the manufacturers' instructions.
Detection of CRP expression in lung
tissue by immunohistochemistry
After mice were sacrificed, the left lung lobe was
dissected and fixed with 4% paraformaldehyde at room temperature
for 48 h, dehydrated, embedded in paraffin and then sliced into
5-µm sections. The tissue sections were then placed in citrate
buffer for antigen retrieval. After being boiled three times (5 min
each), the sections were blocked with 3% H2O2
and incubated for 10 min to eliminate the internal peroxidase
activity at room temperature. CRP primary antibody (1:500; cat. no.
ab211631; Abcam) was added to the sections for 2 h at room
temperature and the sections were then incubated with an
HRP-labeled secondary antibody (1:1,000; cat. no. sc-2004; Santa
Cruz Biotechnology, Inc.) for 1 h at room temperature. The sections
were exposed to DAB in the dark for 6 min and counterstained with
hematoxylin for 10 min at room temperature, then dehydrated and
sealed by neutral gum. Eight randomly selected sections from mice
in each group were assessed. The expression of CRP in the lung
tissue was observed under a light microscope. The optical density
values were analyzed and measured using Image-Pro Plus 6.0 software
(Media Cybernetics, Inc.).
ELISA assay for IL-1β, IL-6, IL-18 and
TNF-α in BALF
Mice were euthanized, the thoracic cavity was
opened, and the right main bronchus was ligated at the left and
right bronchial bifurcations. Pre-cooled PBS was used to perform
bronchoalveolar lavage of the right lung three times; each time,
0.4 ml BALF was recovered. The BALF was transferred to a tube,
centrifuged at 1,800 × g at 4°C for 15 min and the supernatant was
collected. The levels of inflammatory factors, IL-1β (cat. no.
MLB00C), IL-6 (cat. no. M6000B), IL-18 (cat. no. 7625) and TNF-α
(cat. no. MTA00B), in the BALF were detected by ELISA according to
manufacturer's protocols. The ELISA kits were purchased from
R&D Systems, Inc.. The concentration of Protein in the BALF was
measured using the BCA method (Bio-Rad Laboratories, Inc.).
Lung wet-to-dry weight ratio
After mice were euthanized, the trachea and
esophagus were separated from the lungs by blunt dissection, and
the left lung was weighed (wet weight). The lung was flushed with
PBS before incubation at 65°C for 48 h. The dry weight of the
ventricle was measured and the ratio of wet-to-dry weight was
calculated.
Quantitative detection of inflammatory
cells in BALF
Cells in the BALF were suspended in 1 ml PBS and
mixed with 0.4% trypan blue stain in a 1:1 ratio. After mixing, 10
µl buffer was applied to the chamber slide, and the slide was
inserted into an automatic cell counter. The total cell count was
performed. The cell precipitation was resuspended to prepare a
smear for staining. Inflammatory cells including eosinophils,
neutrophils, lymphocytes and macrophages in the BALF were counted
using Wright-Giemsa-staining. Briefly, slides were stained by
fixing for 2 min with a one-step methanol-based Wright-Giemsa
stain. Following that, the slides were stained in Diff-Quik I
solution for 5–10 sec and taken out immediately. The slides were
then stained in Diff-Quik II solution for 10–20 sec and taken out
immediately at room temperature, according to the instructions of
the Diff-Quik whole blood stain kit (Baxter Scientific). A total of
200–300 cells from each sample were then counted from a randomly
chosen field using an automatic cell counter. The percentage of a
leukocyte subset was multiplied by the total number of leukocytes
to give the absolute number of the specific leukocyte subset.
Reverse transcription-quantitative PCR
(RT-qPCR) for detection of miR-221 in lung tissue
Total RNA was extracted from lung tissue using
TRIzol® (Invitrogen; Thermo Fisher Scientific, Inc.).
Briefly, a 100 mg sample was added to 1 ml TRIzol and homogenized.
Subsequently, cDNA was synthesized according to the PrimeScript RT
reagent kit instructions (Takara Bio, Inc.). cDNA (2 µl) was used
as a template and amplification was carried out according to the
RT-qPCR kit instructions (Invitrogen; Thermo Fisher Scientific,
Inc.). Primer sequences are shown in Table II. The relative changes in mRNA
expression levels were calculated using the 2−ΔΔCq
Method (38). The reaction
conditions were as follows: Pre-denaturation at 95°C for 5 min,
followed by 30 cycles at 94°C for 30 sec, 55°C for 30 sec and 72°C
for 60 sec, and a final extension step at 72°C for 1 min.
 | Table II.miR-221 and U6 primer sequences. |
Table II.
miR-221 and U6 primer sequences.
| Primer name | Primer sequence
(5′-3′) |
|---|
| miR-221 upstream
primer |
GGGAAGCTACATTGTCTGC |
| miR-221 downstream
primer |
CAGTGCGTGTCGTGGAGT |
| U6 upstream
primer |
CTCGCTTCGTCGGCAGCACA |
| U6 downstream
primer |
AACGCTTCACGAATTTGCGT |
H&E staining
The lung tissue slices were dried in a constant
temperature oven at 40°C. The slices were dewaxed with xylene,
hydrated with a gradient of ethanol solutions and rinsed with
distilled water for 1 min. Subsequently, the tissues were stained
with Harris hematoxylin at 60°C for 5 min, washed with Harris
hematoxylin for 5–10 sec, washed with water for 5–10 sec, rinsed
with 1% ammonia for 5–10 sec and then rinsed with water for 15–30
sec. The tissues were then counterstained with eosin for 30–60 sec,
and observed under a light microscope to verify changes of color.
The tissues were rinsed with ddH2O for 5–10 sec and
dehydrated with a gradient of ethanol solutions: 80% ethanol for
1–2 sec, 95% ethanol for 1–2 sec, 100% ethanol for 1–2 sec.
Subsequently, the slices were soaked in xylene for 2–3 sec, then
dried before being sealed with neutral gum. The slices were then
observed and scored under a light microscope. The score for
substantial pneumonia was based on the degree of neutrophil
alveolar infiltration (39), as
follows: 0 points, no inflammatory cells around the bronchi; 1
point, scattered small inflammatory cells observed around the
bronchi; 2 points, inflammation was a cell layer thick; 3 points,
inflammation was between two and four cell layers thick around the
trachea; 4 points, inflammation was four cell layers thick around
the trachea.
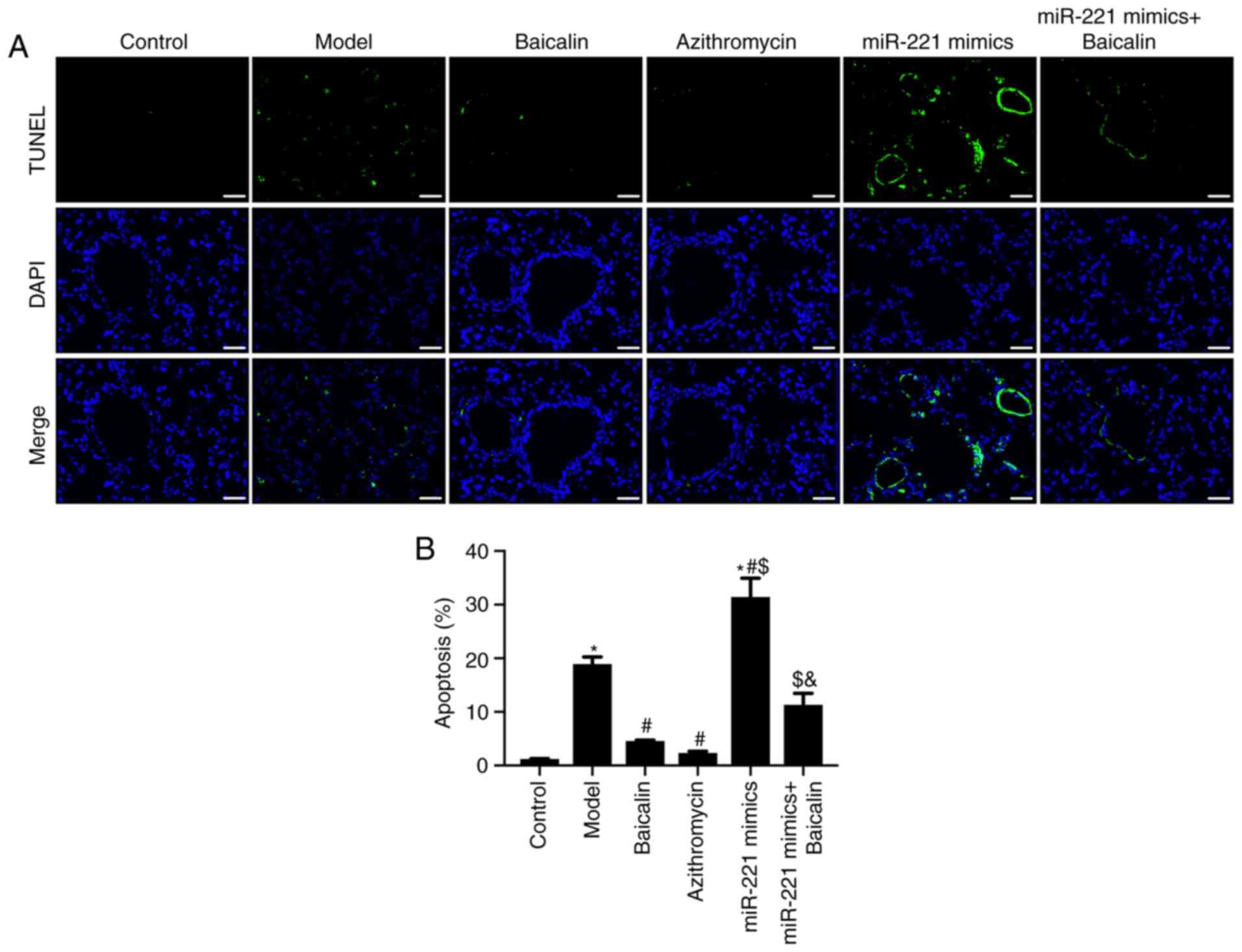
TUNEL assay
Apoptosis of lung tissue was detected using the
TUNEL assay with an Apoptosis Assay kit (Roche Diagnostics GmbH).
The lung tissue slices were naturally dried, dewaxed with xylene
and dehydrated with a gradient of alcohol solutions. The tissues
were then added to 50 µl TdT enzyme reaction solution and incubated
at 37°C for 60 min in the dark, then washed with PBS. Subsequently,
tissue slices were added to 50 µl Streptavidin-TRITC labeling
solution and incubated in a wet box at 37°C for 30 min. After
washing with PBS, tissues were counterstained with DAPI solution,
incubated for 15 min, sealed with mounting medium and observed
under a fluorescence microscope (Olympus IX71; Olympus
Corporation). TUNEL-positive cells in the images were counted using
ImageJ software (version 6.0; National Institutes of Health).
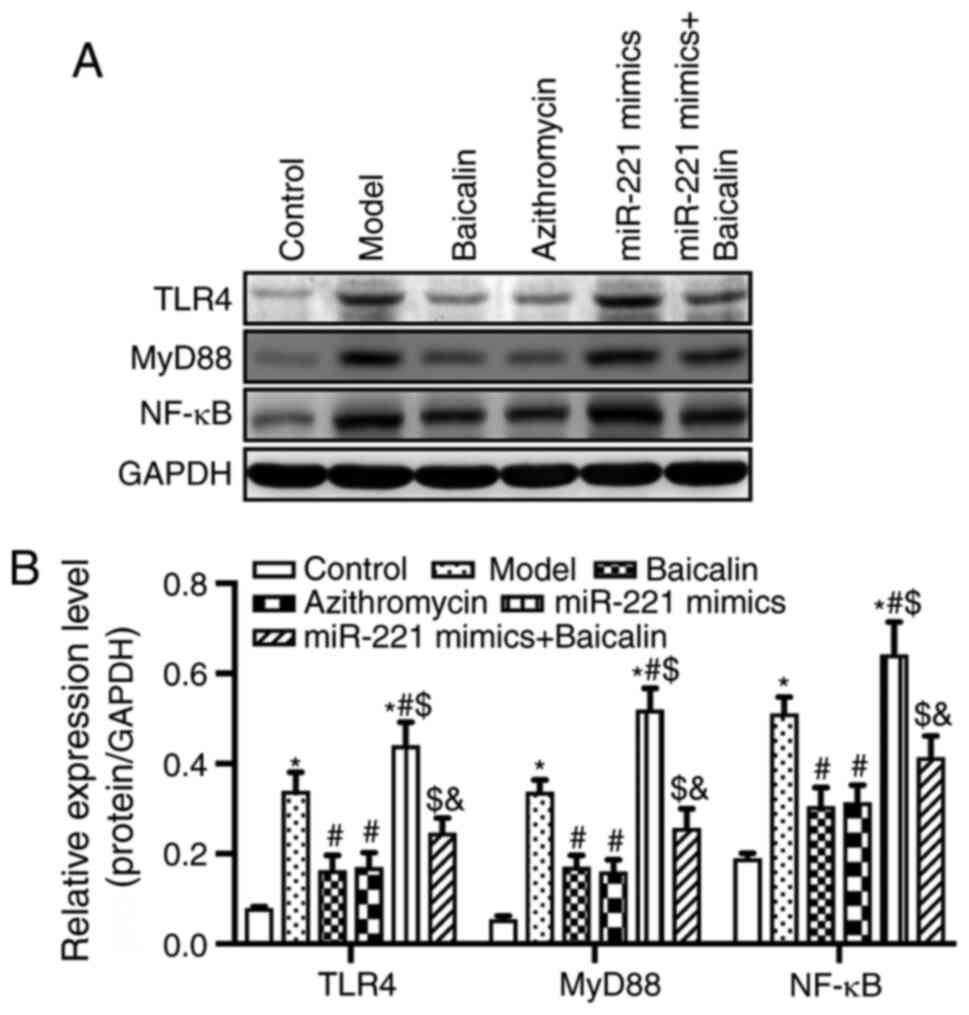
Western blot analysis
The lung tissue of mice was collected and digested
by pre-cooled tissue protein RIPA lysis buffer (Beyotime Institute
of Biotechnology). The protein content in the sample was determined
by a BCA kit after being denatured in boiling water. Proteins (~30
µg/lane) were separated by SDS-polyacrylamide gel electrophoresis
on 10% gels, then transferred to PVDF membranes and blocked in 5%
skim milk/TBS-0.1% Tween (TBST) solution for 1 h at room
temperature. The membranes were then incubated with the following
primary antibodies: Anti-TLR4 (1:1,000; cat. no. ab13556; Abcam),
anti-MyD88 (1:1,000; cat. no. ab219413; Abcam), anti-NF-κB
(1:1,000; cat. no. 8242; Cell Signaling Technology, Inc.) and
anti-GAPDH (1:1,000; cat. no. ab9485; Abcam) overnight at 4°C.
After washing with TBST three times, HRP-labeled secondary antibody
(1:1,000; cat. no. ab7090; Abcam) was added to the membranes for 1
h at room temperature, then washed with PBS. ECL (GE Healthcare)
was used to visualize the blots and images were captured using an
ImageQuant gel imaging system (GE Healthcare Bio-Sciences). The
optical density ratio of the target band was then calculated by
ImageJ software (version 6.0; National Institutes of Health). GAPDH
was used as the loading control.
Statistical analysis
All experiments were performed with at least three
independent replicates. Statistical analysis was performed using
SPSS 18.0 software (SPSS, Inc.). The experimental results are
presented as the mean ± SD and were analyzed using one-way ANOVA
followed by Tukey post hoc test. Moreover, the inflammation score
results, presented as median and range, were analyzed by
Kruskal-Wallis test followed by post hoc Tukey-Kramer test.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Baicalin reduces serum MP-IgM levels
and the expression levels of CRP in lung tissue
To evaluate the effect of Baicalin on acquired
immunity, the serum levels of MP-IgM in MPP model mice were
detected. MP-IgM is the earliest specific antibody associated with
MP infection, which can be detected as early as 1 week after
exposure (40). The results
revealed that the serum levels of MP-IgM in the MP model group were
significantly increased compared with those in the control group.
Furthermore, Baicalin or azithromycin treatment significantly
reduced the serum levels of MP-IgM in MPP model mice (Fig. 1B). Additionally, Baicalin or
azithromycin treatment decreased the wet-to-dry ratio of the lungs
compared with that in the MPP model group (Fig. 1C). Moreover, BALF concentration was
reduced under Baicalin or azithromycin treatment compared with in
the MPP model group (Fig. 1D). CRP
has been reported to bind with leukocytes and lymphocyte receptors,
promoting leukocyte migration and phagocytosis, thus participating
in the T lymphocyte-mediated immune response; CRP has also been
suggested as an indicator for evaluating MP (41). The present results revealed that
Baicalin or azithromycin treatment significantly decreased the
levels of CRP in serum (Fig. 1E)
and in lung tissue (Fig. 1F)
compared with those in the MPP model mice.
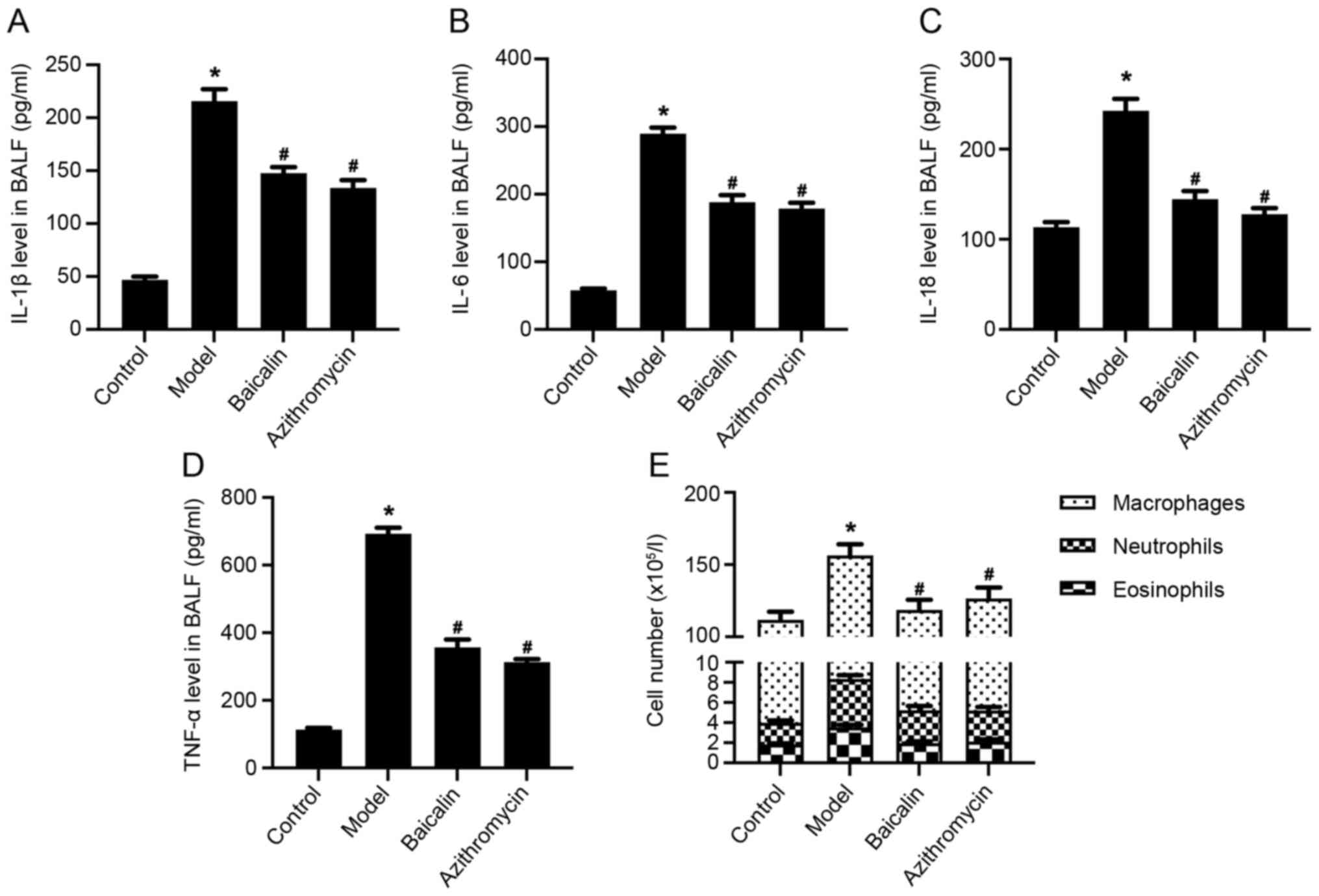
Baicalin inhibits inflammatory
response in BALF in MPP model mice
Inflammatory cell infiltration around the alveolar
and bronchial vessels, which can cause an inflammatory response, is
an important pathological feature of MPP autoimmunity (21). As MP infection develops,
inflammatory factors, including IL-1, IL-2, IL-5, IL-6, IL-8,
IL-12, IL-18, TNF-α and IFN-γ, and anti-inflammatory factors, such
as IL-4, IL-10 and TNF-β, have been shown to be produced (42). In addition, ILs are related to the
pathogenesis of MPP (43). The
present study demonstrated that the levels of inflammatory factors,
IL-1β, IL-6, IL-18 and TNF-α, in the BALF of the MPP model group
were significantly higher compared with those in the control group,
whereas Baicalin or azithromycin treatment significantly reduced
the levels of inflammatory factors in the BALF of MPP model mice
(Fig. 2A-D). Moreover, Baicalin
decreased the number of white blood cells, particularly
eosinophils, neutrophils and macrophages in the BALF of MPP model
mice (Fig. 2E).
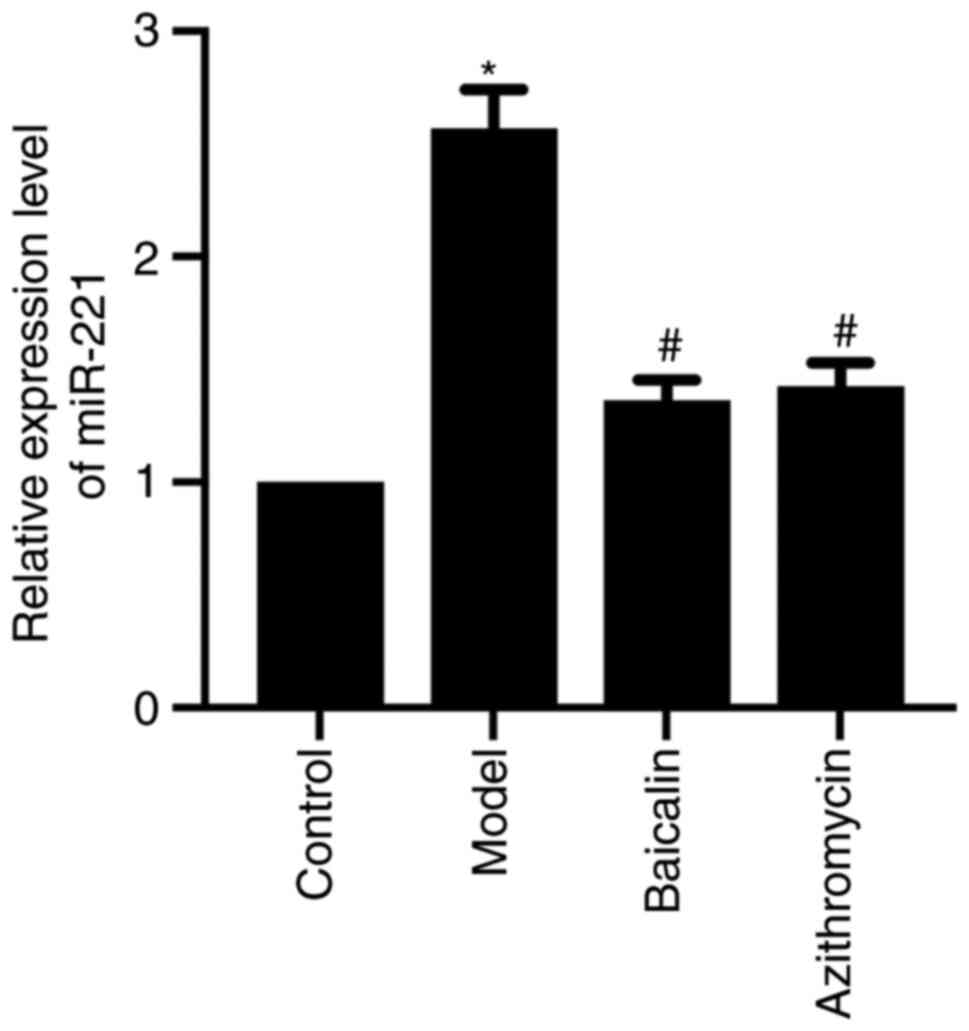
Baicalin downregulates miR-221 in the
lung tissue of MPP model mice
miR-221 was revealed to be highly expressed in the
lung tissue of MPP model mice. Notably, miR-221 expression levels
were significantly increased in the lung tissue of the MPP model
group compared with those in the control group, whereas Baicalin
could downregulate the expression levels of miR-221 in the lung
tissue of MPP model mice (Fig. 3).
These data indicated that the therapeutic effect of Baicalin on MPP
model mice may be related to downregulation of miR-221.
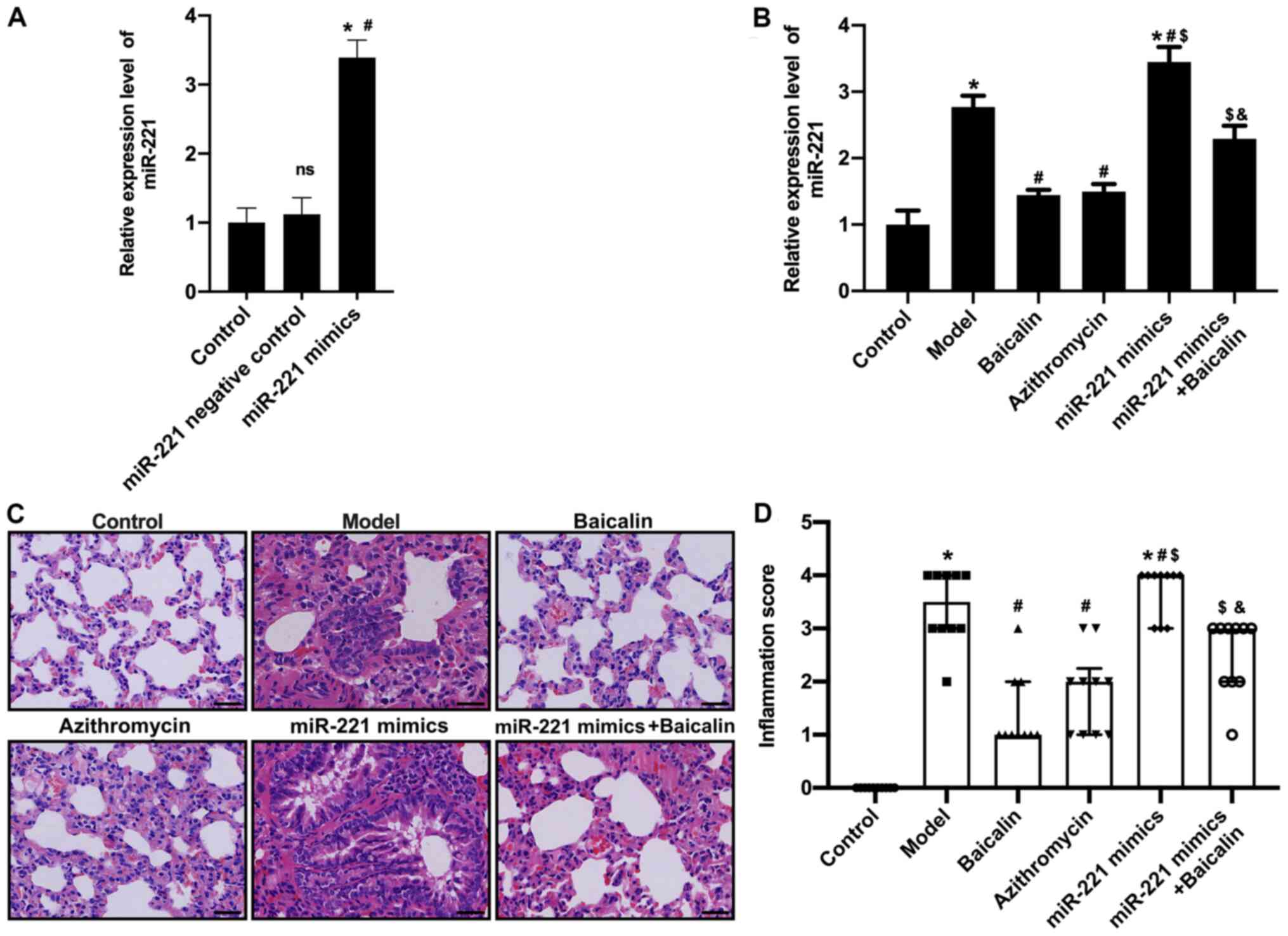
Baicalin alleviates pathological lung
damage in MPP model mice by regulating miR-221
To further investigate the relationship between
Baicalin and miR-221, mice were transfected with a miR-221
lentivirus (miR-221 mimic) (Fig.
4A) and then exposed to MP. The results demonstrated that
miR-221 mimics reversed the effects of Baicalin on downregulation
of miR-221 (Fig. 4B). In addition,
H&E staining showed that there were no obvious lesions in the
bronchial, alveolar and blood vessels of the saline control group,
and there was no obvious abnormality in the alveolar wall and no
inflammatory cell infiltration in lung tissue. By contrast, mice in
the MPP model group exhibited a looser alveolar structure,
thickened alveolar wall edema and a large degree of inflammatory
cell infiltration in lung tissue. In comparison, Baicalin or
azithromycin markedly improved alveolar structure and wall
thickening of lung tissue, and reduced inflammatory cell
infiltration compared with in the MPP model group (Fig. 4C). However, the positive effects of
Baicalin on the pathological damage to lung tissue was blocked by
miR-221 mimics. In addition, lung tissue damage was evaluated
according to the inflammatory scoring criteria. Compared with those
in the control group, the inflammatory infiltration scores of the
mice in the MPP model group were significantly increased. Baicalin
and azithromycin significantly reduced the inflammatory
infiltration scores (Fig. 4D);
however, when mice were transfected with miR-221 mimics and treated
with Baicalin, the inflammatory infiltration scores were
significantly increased. These results indicated that Baicalin may
reduce pathological lung damage by downregulating miR-221.
Baicalin inhibits lung tissue
apoptosis in MPP model mice by regulating miR-221
To investigate the effects of Baicalin on apoptosis
in the lung tissue of MPP model mice, lung tissue sections were
stained with TUNEL. Compared with that in the control group, the
number of TUNEL-positive cells was significantly increased in the
lung tissue of the MPP model group (Fig. 5A and B). Compared with that in the
model group, the number of TUNEL-positive cells in the Baicalin and
azithromycin groups was significantly decreased (Fig. 5A and B). In addition, the inhibitory
effect of Baicalin on lung tissue apoptosis was attenuated by
miR-221 mimics (Fig. 5A and B).
These results indicated that Baicalin may inhibit the apoptosis of
lung tissue cells in MPP model mice by downregulating miR-221.
Baicalin inhibits the TLR4/NF-κB
signaling pathway via regulating miR-221
miR-221 has been reported to serve an important role
in lung epithelial-mesenchymal transition, which is the main cause
of pulmonary fibrosis (44).
Notably, miR-221 has been demonstrated to be upregulated in the
airway smooth muscle cells of patients with asthma (45). Furthermore, miR-221 has been
reported to increase the secretion of the inflammatory factor IL-6,
which suggests that an association exists between miR-221 and the
respiratory inflammatory response (46). miR-221 has also been reported to
regulate the TLR4/NF-κB signaling pathway, which has an important
regulatory role in MPP (47,48).
Based on these previous studies, the present study further explored
whether Baicalin could inhibit lung injury in MPP model mice by
downregulating miR-221 and inhibiting the activity of the
TLR4/NF-κB signaling pathway. The results revealed that the protein
expression levels of TLR4, MyD88 and NF-κB were significantly
increased in the lung tissue of the MPP model group. Conversely,
Baicalin inhibited the expression levels of TLR4, MyD88 and NF-κB
in the lung tissue compared with those in the MPP model group
(Fig. 6). Notably, the inhibition
of these proteins was blocked by miR-221 mimics, suggesting that
Baicalin may reduce lung tissue damage via the miR-221/TLR4/NF-κB
axis in MPP model mice.
Discussion
Baicalin is an effective traditional Chinese
medicine that utilizes an ingredient extracted from Scutellaria
baicalensis Georgi. Baicalin has been reported to inhibit the
growth of breast cancer and induce apoptosis of pancreatic cancer
cells (49,50). Baicalin has also been suggested to
exert an anti-apoptosis and anti-inflammatory effect by inhibiting
the expression of the inflammation-associated gene COX-2, thereby
reducing c-Jun expression and AP-1 activation in A549 cells
(51). Baicalin may also inhibit
vascular permeability, cellular adhesion molecule expression and
adhesion, and leukocyte migration, when used as systemic therapy
for endotoxin-induced vascular inflammatory diseases (52). Moreover, Baicalin has been reported
to downregulate the expression of MP adhesion protein P1 and
upregulate epidermal growth factor to promote the repair of lung
epithelial cells (53). Taken
together, these findings indicated that Baicalin may have potential
therapeutic value in respiratory and immunoinflammatory diseases
(54). Therefore, the present study
investigated the therapeutic effect of Baicalin on a mouse model of
MPP and assessed its molecular mechanism.
MPP is a common respiratory disease in children and
the global incidence of MMP has been increasing annually (43,55).
MP is a prokaryotic microbial organism, and is the smallest and
simplest independent pathogenic microorganism. As MP lacks a cell
wall, it is an extracellular pathogen that adheres to the mucosal
surface of the respiratory tract and genitals. After invading the
human body, MP fuses with host cell membranes to induce immune
responses (56,57). In addition to causing respiratory
diseases, MP also causes numerous other diseases, such as
myocarditis, nephritis and encephalitis, and can be fatal (58). Due to the lack of a cell wall,
several antibiotics, including penicillin, cannot inhibit MP
(55). Although macrolide
antibiotics have anti-inflammatory properties and strong
antibacterial activity when used to treat MP infection, repeated
treatment with azithromycin can lead to adverse reactions
associated with clinical treatment failure, including toxicity,
side effects and drug resistance (59). Therefore, it is important to
investigate safe and effective treatments for MPP.
It has been reported that various Igs and
complements serve a role in Mycoplasma infection. IgM is the
main Ig produced in the early stage of human immune response, which
is an indicator for MP infection (40). The present results revealed that
serum MP-IgM levels were significantly lower in the
Baicalin-treated mice compared with those in the MPP model group,
indicating that Baicalin significantly inhibited MP growth. CRP is
an acute phase reaction protein, and is an abnormal protein
synthesized by the liver in the early stages of infectious diseases
caused by microbial invasion or tissue damage (60). CRP detection is a classic test used
to identify bacterial and non-bacterial infections (61); however, whether the expression of
CRP can be used as a diagnostic indicator of MPP is still not
clear. The results of the present study demonstrated that the
expression levels of CRP in the lung tissue of the model group were
significantly increased after MP infection. On the other hand,
Baicalin significantly reduced the expression levels of CRP in
MP-infected lung tissue.
The production of CRP is mainly regulated by
inflammatory factors, such as IL-6 and TNF-α, and these
inflammatory factors serve an important role in mediating
inflammation and immune regulation (62). It has previously been demonstrated
that the expression of these inflammatory factors may be
significantly increased in MPP, and numerous inflammatory cells can
infiltrate around the alveolar and bronchial vessels. Furthermore,
the strength of these inflammatory reactions may be related to
various autoimmune and inflammatory diseases (63).
Inflammatory factors produced by MP infection may
activate caspase-9 through signaling pathways, such as Janus
kinase/signal transducer and transcriptional activators, releasing
more apoptosis-inducing factors and finally activating caspase-3.
Activation of the caspase cascade causes DNA fragmentation and
chromatin aggregation, leading to irreversible cell apoptosis
(64). Therefore, the present study
analyzed the levels of inflammatory factors and the number of
inflammatory cells in the BALF of MPP mice treated with or without
Baicalin. The results demonstrated that Baicalin reduced the number
of eosinophils and neutrophils, and decreased the levels of IL-1β,
IL-6, IL-18 and TNF-α in the BALF of MPP model mice. These results
indicated that Baicalin may significantly alleviate infiltration of
inflammatory cells and improve the inflammatory response.
TLRs are a key participant in innate and adaptive
immune responses to pathogenic and non-infectious tissue damage,
and TLR-related factors have been reported to serve an important
role in the development of inflammation (65,66).
Notably, TLR4 and TLR9 have been shown to serve key roles in lung
injury caused by various factors, such as lipopolysaccharide,
hemorrhage and ischemia-reperfusion (67,68).
TLR4 is an upstream factor of inflammatory response and a key
factor in the innate immune response. MyD88 is an adaptor protein
in TLR and an important downstream factor of TLR4 signaling. After
TLR4 binds to a ligand that has crossed the cell membrane, it
recruits the downstream adaptor molecule, MyD88, and ultimately
activates NF-κB. This subsequently induces transcription of
pro-inflammatory genes, including genes encoding cytokines
(69–72). The present study investigated the
effect of Baicalin on the expression levels of miR-221 and the
TLR4/NF-κB signaling pathway-related proteins. The results revealed
that miR-221 was highly expressed in the MPP model group and was
reduced in response to Baicalin treatment. Baicalin-based
inhibition of miR-221 expression suggested that Baicalin may have a
regulatory effect on miR-221 expression. Therefore, it was
hypothesized that Baicalin could alleviate lung injury and prevent
apoptosis in MPP model mice, and regulate miR-221 expression.
Subsequently, the present study transfected miR-221 mimics into MP
mice, which had been treated with Baicalin. The results
demonstrated that Baicalin significantly alleviated pathological
damage to lung tissue, reduced the number of TUNEL-positive cells
in the lung tissue of MPP mice, and inhibited the expression levels
of TLR4, MyD88 and NF-κB. These effects of Baicalin were impaired
or blocked by miR-221 mimics.
In conclusion, Baicalin was able to reduce the serum
levels of MP-IgM and the expression levels of CRP in lung tissue,
reduce the levels of inflammatory factors and the number of
inflammatory cells in the BALF, and improve MP-induced lung injury.
In addition, Baicalin decreased inflammatory infiltration and
pathological changes in mouse lung tissue, and reduced inflammation
and apoptosis in the lung tissue. Notably, these protective
properties may be achieved by inhibiting miR-221 expression and
targeting the TLR4/NF-κB signaling pathway.
Acknowledgements
Not applicable.
Funding
The present study was supported by the program for
Liaoning Innovation Talents in University (grant no.
LR2018479).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HZ designed the study. HZ, XL and JW performed the
experiments. GW provided administrative support and analyzed data.
YS and QC analyzed the data. All authors confirm the authenticity
of the raw data. All authors wrote the manuscript, and read and
approved the final manuscript.
Ethics approval and consent to
participate
The animal experiments were approved by the
Institutional Animal Care and Use Committee (IACUC) of China
Medical University (IACUC no. CMU2018309; Shenyang, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Anjum MU, Riaz H and Tayyab HM: Acute
respiratory tract infections (ARIS); clinico-epidemiolocal profile
in children of less than five years of age. Professional Med J.
24:322–325. 2017. View Article : Google Scholar
|
|
2
|
Guillet E, Mas C, Bauvin I, Beze Beyrie P,
Mansir T and Guérin B: Extrarespiratory manifestations of
Mycoplasma pneumoniae: A case report. Arch Pediatr.
21:381–383. 2014.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hanzawa F, Fuchigami T, Ishii W, Nakajima
S, Kawamura Y, Endo A, Arakawa C, Kohira R, Fujita Y and Takahashi
S: A 3-year-old boy with Guillain-Barré syndrome and encephalitis
associated with Mycoplasma pneumoniae infection. J Infect
Chemother. 20:134–138. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Esposito S, Blasi F, Arosio C, Fioravanti
L, Fagetti L, Droghetti R, Tarsia P, Allegra L and Principi N:
Importance of acute Mycoplasma pneumoniae and chlamydia
pneumoniae infections in children with wheezing. Eur Respir J.
16:1142–1146. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Liu WK, Liu Q, Chen DH, Liang HX, Chen XK,
Chen MX, Qiu SY, Yang ZY and Zhou R: Epidemiology of acute
respiratory infections in children in Guangzhou: A three-year
study. PLoS One. 9:e966742014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gullsby K and Bondeson K: No detection of
macrolide-resistant Mycoplasma pneumoniae from Swedish
patients, 1996–2013. Infect Ecol Epidemiol. 6:313742016.PubMed/NCBI
|
|
7
|
Lu A, Wang C, Zhang X, Wang L and Qian L:
Lactate dehydrogenase as a biomarker for prediction of refractory
Mycoplasma pneumoniae pneumonia in children. Respir Care.
60:1469–1475. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yang JY, Li M, Zhang CL and Liu D:
Pharmacological properties of baicalin on liver diseases: A
narrative review. Pharmacol Rep. Feb 17–2021.(Epub ahead of print).
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hu Q, Zhang W, Wu Z, Tian X, Xiang J, Li
L, Li Z, Peng X, Wei S, Ma X and Zhao Y: Baicalin and the liver-gut
system: Pharmacological bases explaining its therapeutic effects.
Pharmacol Res. 165:1054442021. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Singh S, Meena A and Luqman S: Baicalin
mediated regulation of key signaling pathways in cancer. Pharmacol
Res. 164:1053872021. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yu FY, Huang SG, Zhang HY, Ye H, Chi HG,
Zou Y, Lv RX and Zheng XB: Effects of baicalin in CD4 + CD29 + T
cell subsets of ulcerative colitis patients. World J Gastroenterol.
20:15299–15309. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang CZ, Zhang CF, Chen L, Anderson S, Lu
F and Yuan CS: Colon cancer chemopreventive effects of baicalein,
an active enteric microbiome metabolite from baicalin. Int J Oncol.
47:1749–1758. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lee W, Ku SK and Bae JS: Anti-inflammatory
effects of baicalin, baicalein, and wogonin in vitro and in vivo.
Inflammation. 38:110–125. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Huang X, Mao W, Zhang T, Wang M, Wang X,
Li Y, Zhang L, Yao D, Cai X and Wang L: Baicalin promotes apoptosis
and inhibits proliferation and migration of hypoxia-induced
pulmonary artery smooth muscle cells by up-regulating A2a receptor
via the SDF-1/CXCR4 signaling pathway. BMC Complement Altern Med.
18:3302018. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wang G, Mohammadtursun N, Lv Y, Zhang H,
Sun J and Dong J: Baicalin exerts anti-airway inflammation and
anti-remodelling effects in severe stage rat model of chronic
obstructive pulmonary disease. Evid Based Complement Alternat Med.
2018:75913482018. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bai C, Li T, Sun Q, Xin Q, Xu T, Yu J,
Wang Y and Wei L: Protective effect of baicalin against severe
burn-induced remote acute lung injury in rats. Mol Med Rep.
17:2689–2694. 2018.PubMed/NCBI
|
|
17
|
Chaudhry R, Ghosh A and Chandolia A:
Pathogenesis of Mycoplasma pneumoniae: An update. Indian J
Med Microbiol. 34:7–16. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Martin RJ, Kraft M, Chu HW, Berns EA and
Cassell GH: A link between chronic asthma and chronic infection. J
Allergy Clin Immunol. 107:595–601. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ramien M: Reactive infectious
mucocutaneous eruption: Mycoplasma pneumoniae-induced rash
and mucositis and other parainfectious eruptions. Clin Exp
Dermatol. 46:420–429. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Jiang Z, Li S, Zhu C, Zhou R and Leung
PHM: Mycoplasma pneumoniae infections: Pathogenesis and
vaccine development. Pathogens. 10:1192021. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Saraya T, Kurai D, Nakagaki K, Sasaki Y,
Niwa S, Tsukagoshi H, Nunokawa H, Ohkuma K, Tsujimoto N, Hirao S,
et al: Novel aspects on the pathogenesis of Mycoplasma
pneumoniae pneumonia and therapeutic implications. Front
Microbiol. 5:4102014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yano T, Komatsu S, Araki K, Kuboshiro M,
Ichikawa Y, Ohizumi K and Arai S: Role of transiently accumulated
neutrophils in the lung of hamster in development of pneumonia due
to Mycoplasma pneumoniae. Kansenshogaku Zasshi. 65:365–373.
1991.(In Japanese). View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wang Z, Liao Y, Wang L, Lin Y, Ye Z, Zeng
X, Liu X, Wei F and Yang N: Small RNA deep sequencing reveals novel
miRNAs in peripheral blood mononuclear cells from patients with IgA
nephropathy. Mol Med Rep. 22:3378–3386. 2020.PubMed/NCBI
|
|
24
|
Duan Q, Mao X, Xiao Y, Liu Z, Wang Y, Zhou
H, Zhou Z, Cai J, Xia K, Zhu Q, et al: Super enhancers at the
miR-146a and miR-155 genes contribute to self-regulation of
inflammation. Biochim Biophys Acta. 1859:564–571. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Yamamoto M, Singh A, Ruan J, Gauvreau GM,
O'Byrne PM, Carlsten CR, FitzGerald JM, Boulet LP and Tebbutt SJ:
Decreased miR-192 expression in peripheral blood of asthmatic
individuals undergoing an allergen inhalation challenge. BMC
Genomics. 13:6552012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zhou Y, Yang Q, Xu H, Zhang J, Deng H, Gao
H, Yang J, Zhao D and Liu F: miRNA-221-3p enhances the secretion of
interleukin-4 in mast cells through the phosphatase and tensin
homolog/p38/nuclear factor-kappaB pathway. PLoS One.
11:e01488212016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Amarante-Mendes GP, Adjemian S, Branco LM,
Zanetti LC, Weinlich R and Bortoluci KR: Pattern recognition
receptors and the host cell death molecular machinery. Front
Immunol. 9:23792018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Poddighe D: Mycoplasma
pneumoniae-related hepatitis in children. Microb Pathog.
139:1038632020. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Naghib M, Hatam-Jahromi M, Niktab M,
Ahmadi R and Kariminik A: Mycoplasma pneumoniae and
toll-like receptors: A mutual avenue. Allergol Immunopathol (Madr).
46:508–513. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Shimizu T: Inflammation -inducing Factors
of Mycoplasma pneumoniae. Front Microbiol. 7:4142016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Pal S, Ausar SF, Tifrea DF, Cheng C,
Gallichan S, Sanchez V, de la Maza LM and Visan L: Protection of
outbred mice against a vaginal challenge by a chlamydia trachomatis
serovar E recombinant major outer membrane protein vaccine is
dependent on phosphate substitution in the adjuvant. Hum Vaccin
Immunother. 16:2537–2547. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chandler CE and Ernst RK: Bacterial
lipids: Powerful modifiers of the innate immune response. F1000Res.
6:F10002017. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Dickson K and Lehmann C: Inflammatory
response to different toxins in experimental sepsis models. Int J
Mol Sci. 20:43412019. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Narita M: Pathogenesis of extrapulmonary
manifestations of Mycoplasma pneumoniae infection with
special reference to pneumonia. J Infect Chemother. 16:162–169.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Sun H, Zhang L, Shi C, Hu P, Yan W, Wang
Z, Duan Q, Lu F, Qin L, Lu T, et al: TOPK is highly expressed in
circulating tumor cells, enabling metastasis of prostate cancer.
Oncotarget. 6:12392–12404. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Meng Y, Yang Y, Lu W, Wang Y, Qian F, Wang
X, Zhang Z and Wang W: The inhibition of Platycodin D on
Mycoplasma pneumoniae proliferation and its effect on
promoting cell growth after anti-Mycoplasma pneumoniae
treatment. Front Cell Infect Microbiol. 4:1922015. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Liu Y, Miao Y, Gao X, Wang YY, Wang H,
Zheng YW and Zhao ZY: MicroRNA-200a affects the proliferation of
airway smooth muscle cells and airway remodeling by targeting FOXC1
via the PI3K/AKT signaling pathway in ovalbumin-induced asthmatic
mice. Cell Physiol Biochem. 50:2365–2389. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Kita H: Eosinophils: Multifaceted
biological properties and roles in health and disease. Immunol Rev.
242:161–177. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Zhang Y, Yang X, Qian J, Gu X, Zhang J,
Liu J and Hu Z: Simultaneous detection of Mycoplasma
pneumoniae IgG and IgM using dual-label time resolved
fluoroimmunoassay. Anal Biochem. 548:1–6. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Seo YH, Kim JS, Seo SC, Seo WH, Yoo Y,
Song DJ and Choung JT: Predictive value of C-reactive protein in
response to macrolides in children with macrolide-resistant
Mycoplasma pneumoniae pneumonia. Korean J Pediatr.
57:186–192. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Miyashita N, Obase Y, Ouchi K, Kawasaki K,
Kawai Y, Kobashi Y and Oka M: Clinical features of severe
Mycoplasma pneumoniae pneumonia in adults admitted to an
intensive care unit. J Med Microbiol. 56:1625–1629. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Yang M, Meng F, Wang K, Gao M, Lu R, Li M,
Zhao F, Huang L, Zhang Y, Cheng G and Wang X: Interleukin 17A as a
good predictor of the severity of Mycoplasma pneumoniae
pneumonia in children. Sci Rep. 7:129342017. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Wang YC, Liu JS, Tang HK, Nie J, Zhu JX,
Wen LL and Guo QL: miR-221 targets HMGA2 to inhibit
bleomycin-induced pulmonary fibrosis by regulating
TGF-β1/Smad3-induced EMT. Int J Mol Med. 38:1208–1216. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Perry MM, Baker JE, Gibeon DS, Adcock IM
and Chung KF: Airway smooth muscle hyperproliferation is regulated
by microRNA-221 in severe asthma. Am J Respir Cell Mol Biol.
50:7–17. 2014.PubMed/NCBI
|
|
46
|
Lino Cardenas CL, Kaminski N and Kass DJ:
Micromanaging microRNAs: Using murine models to study microRNAs in
lung fibrosis. Drug Discov Today Dis Models. 10:e145–e151. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Zhu L, Gong X, Gong J, Xuan Y, Fu T, Ni S,
Xu L and Ji N: Notoginsenoside R1 upregulates miR-221-3p expression
to alleviate ox-LDL-induced apoptosis, inflammation, and oxidative
stress by inhibiting the TLR4/NF-κB pathway in HUVECs. Braz J Med
Biol Res. 53:e93462020. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Gu H, Zhu Y, Zhou Y, Huang T, Zhang S,
Zhao D and Liu F: LncRNA MALAT1 affects Mycoplasma
pneumoniae pneumonia via NF-κB regulation. Front Cell Dev Biol.
8:5636932020. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Wang CZ, Li XL, Wang QF, Mehendale SR and
Yuan CS: Selective fraction of Scutellaria baicalensis and
its chemopreventive effects on MCF-7 human breast cancer cells.
Phytomedicine. 17:63–68. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Takahashi H, Chen MC, Pham H, Angst E,
King JC, Park J, Brovman EY, Ishiguro H, Harris DM, Reber HA, et
al: Baicalein, a component of Scutellaria baicalensis,
induces apoptosis by Mcl-1 down-regulation in human pancreatic
cancer cells. Biochim Biophys Acta. 1813:1465–1474. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Chen LG, Hung LY, Tsai KW, Pan YS, Tsai
YD, Li YZ and Liu YW: Wogonin, a bioactive flavonoid in herbal tea,
inhibits inflammatory cyclooxygenase-2 gene expression in human
lung epithelial cancer cells. Mol Nutr Food Res. 52:1349–1357.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Ku SK and Bae JS: Baicalin, baicalein and
wogonin inhibits high glucose-induced vascular inflammation in
vitro and in vivo. BMB Rep. 48:519–524. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Yuan H, et al: Study on inhibitory effect
of baicalein on mycoplasma pneumonia and protection mechanism of
pulmonary epithelial cells of mice. J Chin Phys. 919–922.
2014.PubMed/NCBI
|
|
54
|
Meng Y, Huo J, Lu W, Wang X, Zhang J and
Wang W: Modulation of P1 and EGF expression by baicalin. Int J Mol
Sci. 14:146–157. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Waites KB: New concepts of Mycoplasma
pneumoniae infections in children. Pediatr Pulmonol.
36:267–278. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Rottem S: Interaction of mycoplasmas with
host cells. Physiol Rev. 83:417–432. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Dimitrov DS, Franzoso G, Salman M,
Blumenthal R, Tarshis M, Barile MF and Rottem S: Mycoplasma
fermentans (incognitus strain) cells are able to fuse with T
lymphocytes. Clin Infect Dis. 17 (Suppl 1):S305–S308. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Chan ED and Welsh CH: Fulminant
Mycoplasma pneumoniae pneumonia. West J Med. 162:133–142.
1995.PubMed/NCBI
|
|
59
|
Lee H, Yun KW, Lee HJ and Choi EH:
Antimicrobial therapy of macrolide-resistant Mycoplasma
pneumoniae pneumonia in children. Expert Rev Anti Infect Ther.
16:23–34. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Ingle PV and Patel DM: C-reactive protein
in various disease condition-an overview. Asian J Pharm Clin Res.
4:9–13. 2011.
|
|
61
|
Dulay AT, Buhimschi IA, Zhao G, Bahtiyar
MO, Thung SF, Cackovic M and Buhimschi CS: Compartmentalization of
acute phase reactants interleukin-6, C-reactive protein and
procalcitonin as biomarkers of intra-amniotic infection and
chorioamnionitis. Cytokine. 76:236–243. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Baumeister D, Akhtar R, Ciufolini S,
Pariante CM and Mondelli V: Childhood trauma and adulthood
inflammation: A meta-analysis of peripheral C-reactive protein,
interleukin-6 and tumour necrosis factor-α. Mol Psychiatry.
21:642–649. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Meylan E, Tschopp J and Karin M:
Intracellular pattern recognition receptors in the host response.
Nature. 442:39–44. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Kolsuz M, Erginel S, Alataş O, Alataş F,
Metintaş M, Uçgun I, Harmanci E and Colak O: Acute phase reactants
and cytokine levels in unilateral community-acquired pneumonia.
Respiration. 70:615–622. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
O'Neill LA and Bowie AG: The family of
five: TIR-domain-containing adaptors in Toll-like receptor
signalling. Nat Rev Immunol. 7:353–364. 2007. View Article : Google Scholar
|
|
66
|
Huang C, Pan L, Lin F, Dai H and Fu R:
Monoclonal antibody against Toll-like receptor 4 attenuates
ventilator-induced lung injury in rats by inhibiting MyD88- and
NF-κB-dependent signaling. Int J Mol Med. 39:693–700. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Prakash A, Mesa KR, Wilhelmsen K, Xu F,
Dodd-o JM and Hellman J: Alveolar macrophages and Toll-like
receptor 4 mediate ventilated lung ischemia reperfusion injury in
mice. Anesthesiology. 117:822–835. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
He Z, Gao Y, Deng Y, Li W, Chen Y, Xing S,
Zhao X, Ding J and Wang X: Lipopolysaccharide induces lung
fibroblast proliferation through Toll-like receptor 4 signaling and
the phosphoinositide3-kinase-Akt pathway. PLoS One. 7:e359262012.
View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Fuchs Y and Steller H: Programmed cell
death in animal development and disease. Cell. 147:742–758. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Liu Y, Yin H, Zhao M and Lu Q: TLR2 and
TLR4 in autoimmune diseases: A comprehensive review. Clin Rev
Allergy Immunol. 47:136–147. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Perkins DJ and Vogel SN: Inflammation:
Species-specific TLR signalling-insight into human disease. Nat Rev
Rheumatol. 12:198–200. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
So EY, Kim SH, Park HH, Cho BS and Lee CE:
Corticosteroid inhibits IL-4 signaling through down-regulation of
IL-4 receptor and STAT6 activity. FEBS Lett. 518:53–59. 2002.
View Article : Google Scholar : PubMed/NCBI
|