|
1
|
Varricchi G, Ferri S, Pepys J, Poto R,
Spadaro G, Nappi E, Paoletti G, Virchow JC, Heffler E and Canonica
WG: Biologics and airway remodeling in severe asthma. Allergy.
77:3538–3552. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cheng Q, Pan J, Zhou ZL, Yin F, Xie HY,
Chen PP, Li JY, Zheng PQ, Zhou L, Zhang W, et al: Caspase-11/4 and
gasdermin D-mediated pyroptosis contributes to podocyte injury in
mouse diabetic nephropathy. Acta Pharmacol Sin. 42:954–963. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Stern J, Pier J and Litonjua AA: Asthma
epidemiology and risk factors. Semin Immunopathol. 42:5–15. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ntontsi P, Photiades A, Zervas E, Xanthou
G and Samitas K: Genetics and epigenetics in asthma. Int J Mol Sci.
22:24122021. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chupp GL, Kaur R and Mainardi A: New
therapies for emerging endotypes of asthma. Annu Rev Med.
71:289–302. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ray A, Das J and Wenzel SE: Determining
asthma endotypes and outcomes: Complementing existing clinical
practice with modern machine learning. Cell Rep Med. 3:1008572022.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Liu T, Prescott WG and Zhou X: Advances in
non-type 2 asthma in the severe cases: From molecular insights to
novel treatment strategies. Eur Respir J. 64:23008262024.
View Article : Google Scholar : PubMed/NCBI
|
|
8
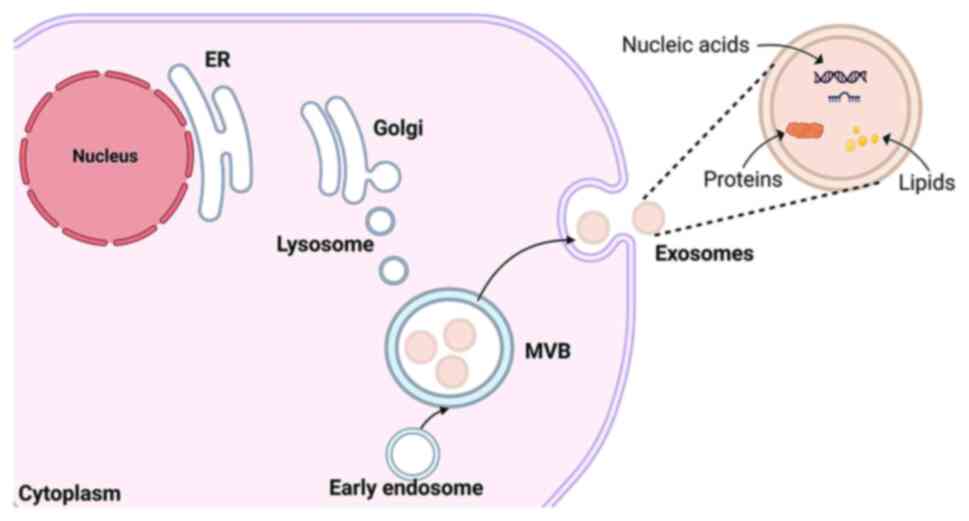
|
von Mutius E and Smits HH: Primary
prevention of asthma: From risk and protective factors to targeted
strategies for prevention. Lancet. 396:854–866. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lommatzsch M, Brusselle GG, Levy ML,
Canonica GW, Pavord ID, Schatz M and Virchow JC: A2BCD:
A concise guide for asthma management. Lancet Respir Med.
11:573–576. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
McDowell PJ, McDowell R, Busby J, Eastwood
MC, Patel PH, Jackson DJ, Mansur A, Patel M, Burhan H, Doe S, et
al: Clinical remission with biologic therapies in severe asthma: A
matter of definition. Eur Respir J. 63:24001602024. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wenzel SE: Severe adult asthmas:
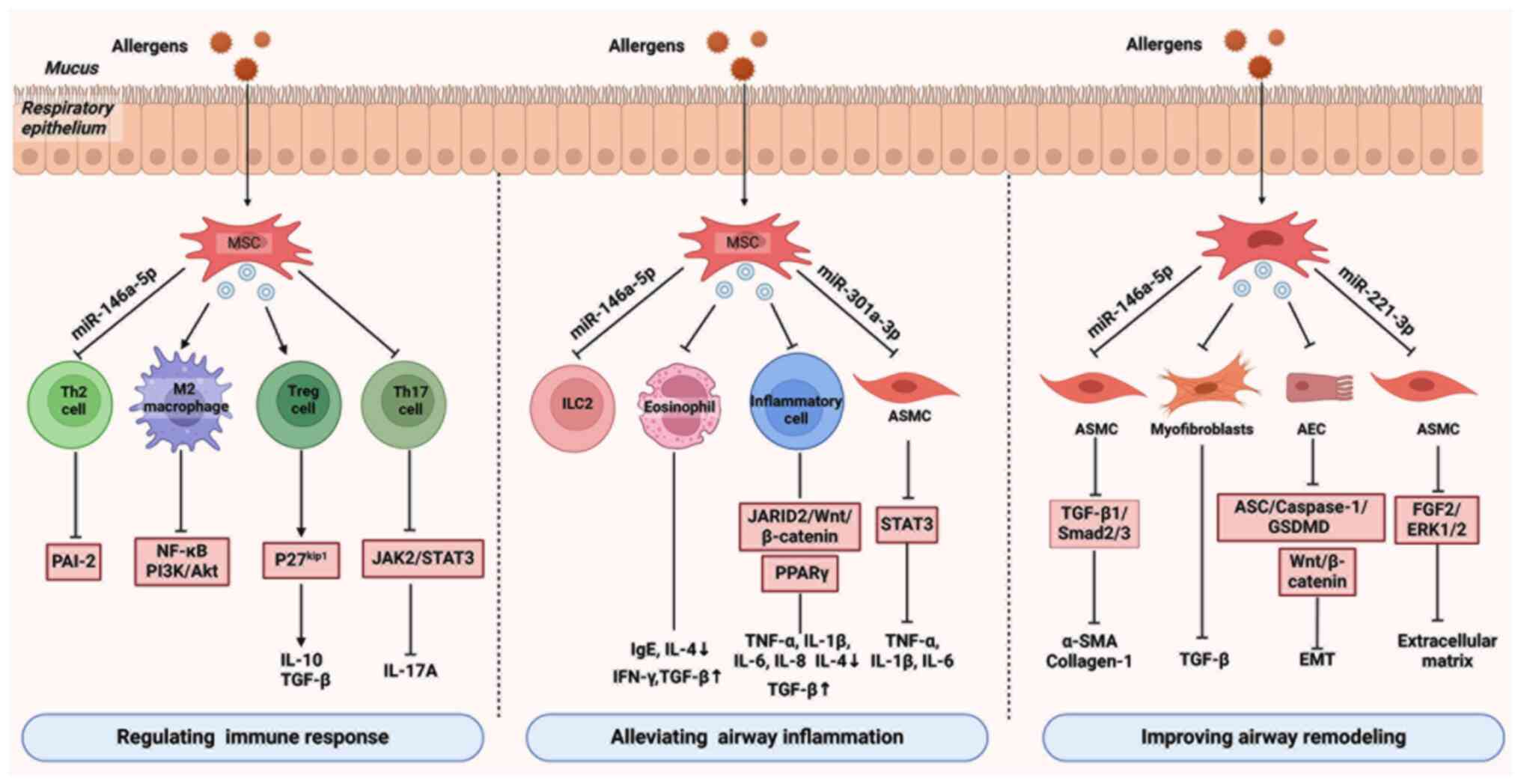
Integrating clinical features, biology, and therapeutics to improve
outcomes. Am J Respir Crit Care Med. 203:809–821. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Thomas D, McDonald VM, Pavord ID and
Gibson PG: Asthma remission: What is it and how can it be achieved?
Eur Respir J. 60:21025832022. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Coleman C, Khaleva E, Rattu A, Frankemölle
B, Nielsen H, Roberts G and Williams C: Narrative review to capture
patients' perceptions and opinions about Non-response and response
to biological therapy for severe asthma. Eur Respir J.
61:22008372023. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhou T, Yuan Z, Weng J, Pei D, Du X, He C
and Lai P: Challenges and advances in clinical applications of
mesenchymal stromal cells. J Hematol Oncol. 14:242021. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mathieu M, Martin-Jaular L, Lavieu G and
Thery C: Specificities of secretion and uptake of exosomes and
other extracellular vesicles for cell-to-cell communication. Nat
Cell Biol. 21:9–17. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wang Y, Fang J, Liu B, Shao C and Shi Y:
Reciprocal regulation of mesenchymal stem cells and immune
responses. Cell Stem Cell. 29:1515–1530. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Li P, Gong Z, Shultz LD and Ren G:
Mesenchymal stem cells: From regeneration to cancer. Pharmacol
Ther. 200:42–54. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Varderidou-Minasian S and Lorenowicz MJ:
Mesenchymal stromal/stem cell-derived extracellular vesicles in
tissue repair: Challenges and opportunities. Theranostics.
10:5979–5997. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
van Griensven M and Balmayor ER:
Extracellular vesicles are key players in mesenchymal stem cells'
dual potential to regenerate and modulate the immune system. Adv
Drug Deliv Rev. 207:1152032024. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhu X, Ma D, Yang B, An Q, Zhao J, Gao X
and Zhang L: Research progress of engineered mesenchymal stem cells
and their derived exosomes and their application in
autoimmune/inflammatory diseases. Stem Cell Res Ther. 14:712023.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wang S, Lei B, Zhang E, Gong P, Gu J, He
L, Han L and Yuan Z: Targeted therapy for inflammatory diseases
with mesenchymal stem cells and their derived exosomes: From basic
to clinics. Int J Nanomedicine. 17:1757–1781. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Brusselle GG and Koppelman GH: Biologic
therapies for severe asthma. N Engl J Med. 386:157–171. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ma Y, Liu X, Long Y and Chen Y: Emerging
therapeutic potential of mesenchymal stem Cell-derived
extracellular vesicles in chronic respiratory diseases: An overview
of recent progress. Front Bioeng Biotechnol. 10:8450422022.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bao Y and Zhu X: Role of chemokines and
inflammatory cells in respiratory allergy. J Asthma Allergy.
15:1805–1822. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kim YM, Kim H, Lee S, Kim S, Lee JU, Choi
Y, Park HW, You G, Kang H, Lee S, et al: Airway G-CSF identifies
neutrophilic inflammation and contributes to asthma progression.
Eur Respir J. 55:19008272020. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Al-Shaikhly T, Murphy RC, Parker A, Lai Y,
Altman MC, Larmore M, Altemeier WA, Frevert CW, Debley JS,
Piliponsky AM, et al: Location of eosinophils in the airway wall is
critical for specific features of airway hyperresponsiveness and T2
inflammation in asthma. Eur Respir J. 60:21018652022. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Nagakumar P, Puttur F, Gregory LG, Denney
L, Fleming L, Bush A, Lloyd CM and Saglani S: Pulmonary type-2
innate lymphoid cells in paediatric severe asthma: Phenotype and
response to steroids. Eur Respir J. 54:18018092019. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Wang W, Xu Y, Wang L, Zhu Z, Aodeng S,
Chen H, Cai M, Huang Z, Han J, Wang L, et al: Single-cell profiling
identifies mechanisms of inflammatory heterogeneity in chronic
rhinosinusitis. Nat Immunol. 23:1484–1494. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Tiotiu A, Badi Y, Kermani NZ, Sanak M,
Kolmert J, Wheelock CE, Hansbro PM, Dahlén SE, Sterk PJ, Djukanovic
R, et al: Association of differential mast cell activation with
granulocytic inflammation in severe asthma. Am J Respir Crit Care
Med. 205:397–411. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Dwyer DF, Ordovas-Montanes J, Allon SJ,
Buchheit KM, Vukovic M, Derakhshan T, Feng C, Lai J, Hughes TK,
Nyquist SK, et al: Human airway mast cells proliferate and acquire
distinct inflammation-driven phenotypes during type 2 inflammation.
Sci Immunol. 6:eabb72212021. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Chacón P, Vega-Rioja A, Doukkali B, Del
Valle Rodriguez A, Fernández-Delgado L, Domínguez-Cereijo L, Segura
C, Pérez-Machuca BM, Perkins JR, El Bekay R, et al: Human
neutrophils couple nitric oxide production and extracellular traps
formation in allergic asthma. Am J Respir Crit Care Med.
210:593–606. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Jesenak M, Durdik P, Oppova D, Franova S,
Diamant Z, Golebski K, Banovcin P, Vojtkova J and Novakova E:
Dysfunctional mucociliary clearance in asthma and airway
remodeling-new insights into an old topic. Respir Med.
218:1073722023. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Li Z, Cheng T, Guo Y, Gao R, Ma X, Mao X
and Han X: Cd147 induces asthmatic airway remodeling and activation
of circulating fibrocytes in a mouse model of asthma. Respir Res.
25:62024. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Defnet AE, Shah SD, Huang W, Shapiro P,
Deshpande DA and Kane MA: Dysregulated retinoic acid signaling in
airway smooth muscle cells in asthma. FASEB J. 35:e220162021.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Shimizu K, Tanabe N, Oguma A, Kimura H,
Suzuki M, Yokota I, Makita H, Sato S, Hirai T, Nishimura M and
Konno S: Parenchymal destruction in asthma: Fixed airflow
obstruction and lung function trajectory. J Allergy Clin Immunol.
149:934–942.e8. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Halwani R, Al-Muhsen S, Al-Jahdali H and
Hamid Q: Role of transforming growth factor-β in airway remodeling
in asthma. Am J Respir Cell Mol Biol. 44:127–133. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Kraik K, Tota M, Laska J, Lacwik J,
Pazdzierz L, Sedek L and Gomulka K: The Role of Transforming Growth
Factor-β (TGF-β) in Asthma and Chronic Obstructive Pulmonary
Disease (COPD). Cells. 13:12712024. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Musiol S, Alessandrini F, Jakwerth CA,
Chaker AM, Schneider E, Guerth F, Schnautz B, Grosch J,
Ghiordanescu I, Ullmann JT, et al: TGF-β1 drives inflammatory th
cell but not treg cell compartment upon allergen exposure. Front
Immunol. 12:7632432021. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Whitehead GS, Thomas SY, Nakano K, Royer
DJ, Burke CG, Nakano H and Cook DN: A neutrophil/TGF-β axis limits
the pathogenicity of allergen-specific CD4+ T cells. JCI Insight.
7:e1502512022. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Lim JO, Kim WI, Pak SW, Lee SJ, Park SH,
Shin IS and Kim JC: Toll-like receptor 4 is a key regulator of
asthma exacerbation caused by aluminum oxide nanoparticles via
regulation of NF-κB phosphorylation. J Hazard Mater.
448:1308842023. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Athari SS: Targeting cell signaling in
allergic asthma. Signal Transduct Target Ther. 4:452019. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
de Jesús TJ, Centore JT and Ramakrishnan
P: Differential regulation of basal expression of inflammatory
genes by NF-κB family subunits. Cell Mol Immunol. 16:720–723. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Shang L, Wang L, Shi X, Wang N, Zhao L,
Wang J and Liu C: HMGB1 was negatively regulated by HSF1 and
mediated the TLR4/MyD88/NF-κB signal pathway in asthma. Life Sci.
241:1171202020. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Kuzmich NN, Sivak KV, Chubarev VN, Porozov
YB, Savateeva-Lyubimova TN and Peri F: TLR4 signaling pathway
modulators as potential therapeutics in inflammation and sepsis.
Vaccines (Basel). 5:342017. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Liu JH, Li C, Zhang CH and Zhang ZH:
LncRNA-CASC7 enhances corticosteroid sensitivity via inhibiting the
PI3K/AKT signaling pathway by targeting miR-21 in severe asthma.
Pulmonology. 26:18–26. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Kwak HJ, Park DW, Seo JY, Moon JY, Kim TH,
Sohn JW, Shin DH, Yoon HJ, Park SS and Kim SH: The wnt/β-catenin
signaling pathway regulates the development of airway remodeling in
patients with asthma. Exp Mol Med. 47:e1982015. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Wang H, Zhong B, Geng Y, Hao J, Jin Q,
Zhang Y, Dong L, Gao D, Li J and Hou W: TIPE2 inhibits
PDGF-BB-induced phenotype switching in airway smooth muscle cells
through the PI3K/Akt signaling pathway. Respir Res. 22:2382021.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Dai Y, Li Y, Cheng R, Gao J, Li Y and Lou
C: TRIM37 inhibits PDGF-BB-induced proliferation and migration of
airway smooth muscle cells. Biomed Pharmacother. 101:24–29. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Friedenstein AJ, Piatetzky S II and
Petrakova KV: Osteogenesis in transplants of bone marrow cells. J
Embryol Exp Morphol. 16:381–390. 1966.PubMed/NCBI
|
|
50
|
Pærregaard SI, Wulff L, Schussek S, Niss
K, Mörbe U, Jendholm J, Wendland K, Andrusaite AT, Brulois KF,
Nibbs RJB, et al: The small and large intestine contain related
mesenchymal subsets that derive from embryonic gli1+
precursors. Nat Commun. 14:23072023. View Article : Google Scholar
|
|
51
|
Miclau K, Hambright WS, Huard J, Stoddart
MJ and Bahney CS: Cellular expansion of mscs: Shifting the
regenerative potential. Aging Cell. 22:e137592023. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Zhang P, Dong J, Fan X, Yong J, Yang M,
Liu Y, Zhang X, Lv L, Wen L, Qiao J, et al: Characterization of
mesenchymal stem cells in human fetal bone marrow by single-cell
transcriptomic and functional analysis. Signal Transduct Target
Ther. 8:1262023. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Yu H, Huang Y and Yang L: Research
progress in the use of mesenchymal stem cells and their derived
exosomes in the treatment of osteoarthritis. Ageing Res Rev.
80:1016842022. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Huang CW, Lu SY, Huang TC, Huang BM, Sun
HS, Yang SH, Chuang JI, Hsueh YY, Wu YT and Wu CC: FGF9 induces
functional differentiation to Schwann cells from human adipose
derived stem cells. Theranostics. 10:2817–2831. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Wang J, Yue BL, Huang YZ, Lan XY, Liu WJ
and Chen H: Exosomal RNAs: Novel potential biomarkers for
diseases-A review. Int J Mol Sci. 23:24612022. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Krylova SV and Feng D: The machinery of
exosomes: Biogenesis, release, and uptake. Int J Mol Sci.
24:13372023. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Gurung S, Perocheau D, Touramanidou L and
Baruteau J: The exosome journey: From biogenesis to uptake and
intracellular signalling. Cell Commun Signal. 19:472021. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Hessvik NP and Llorente A: Current
knowledge on exosome biogenesis and release. Cell Mol Life Sci.
75:193–208. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Colombo M, Raposo G and Thery C:
Biogenesis, secretion, and intercellular interactions of exosomes
and other extracellular vesicles. Annu Rev Cell Dev Biol.
30:255–289. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Feng Y, Guo K, Jiang J and Lin S:
Mesenchymal stem cell-derived exosomes as delivery vehicles for
non-coding RNAs in lung diseases. Biomed Pharmacother.
170:1160082024. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Niazi V, Parseh B, Ahani M, Karami F,
Gilanchi S, Atarodi K, Soufi M, Soleimani M, Ghafouri-Fard S,
Taheri M and Zali H: Communication between stromal and
hematopoietic stem cell by exosomes in normal and malignant bone
marrow niche. Biomed Pharmacother. 132:1108542020. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Yaghoubi Y, Movassaghpour A, Zamani M,
Talebi M, Mehdizadeh A and Yousefi M: Human umbilical cord
mesenchymal stem cells Derived-exosomes in diseases treatment. Life
Sci. 233:1167332019. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Dilsiz N: A comprehensive review on recent
advances in exosome isolation and characterization: Toward clinical
applications. Transl Oncol. 50:1021212024. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Li K, Wong DK, Hong KY and Raffai RL:
Cushioned-density gradient ultracentrifugation (C-DGUC): A refined
and high performance method for the isolation, characterization,
and use of exosomes. Methods Mol Biol. 1740:69–83. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Boing AN, van der Pol E, Grootemaat AE,
Coumans FA, Sturk A and Nieuwland R: Single-step isolation of
extracellular vesicles by Size-exclusion chromatography. J
Extracell Vesicles. 32014.doi: 10.3402/jev.v3.23430.
|
|
66
|
Rahmatinejad F, Kharat Z, Jalili H, Renani
MK and Mobasheri H: Comparison of morphology, protein
concentration, and size distribution of bone marrow and Wharton's
jelly-derived mesenchymal stem cells exosomes isolated by
ultracentrifugation and Polymer-based precipitation techniques.
Tissue Cell. 88:1024272024. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Mousavi SM, Amin Mahdian SM, Ebrahimi MS,
Taghizadieh M, Vosough M, Sadri Nahand J, Hosseindoost S, Vousooghi
N, Javar HA, Larijani B, et al: Microfluidics for detection of
exosomes and microRNAs in cancer: State of the art. Mol Ther
Nucleic Acids. 28:758–791. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Mondal SK and Whiteside TL:
Immunoaffinity-Based isolation of melanoma Cell-Derived and T
Cell-derived exosomes from plasma of melanoma patients. Methods Mol
Biol. 2265:305–321. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Sharma V, Nikolajeff F and Kumar S:
Employing nanoparticle tracking analysis of salivary neuronal
exosomes for early detection of neurodegenerative diseases. Transl
Neurodegener. 12:72023. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Wen J, Zhang Z, Feng G, Zhang Y, Li H,
Lambert C, Mallouk N and Li G: Transmission electron microscopy
assessment of a novel method for isolating pure exosomes from
serum. Biotech Histochem. 98:391–395. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Lyu TS, Ahn Y, Im YJ, Kim SS, Lee KH, Kim
J, Choi Y, Lee D, Kang E, Jin G, et al: The characterization of
exosomes from fibrosarcoma cell and the useful usage of Dynamic
Light Scattering (DLS) for their evaluation. PLoS One.
16:e02319942021. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Miron RJ and Zhang Y: Understanding
exosomes: Part 1-Characterization, quantification and isolation
techniques. Periodontol. 94:231–256. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Su N, Hao Y, Wang F, Hou W, Chen H and Luo
Y: Mesenchymal stromal Exosome-functionalized scaffolds induce
innate and adaptive immunomodulatory responses toward tissue
repair. Sci Adv. 7:eabf72072021. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Tan F, Li X, Wang Z, Li J, Shahzad K and
Zheng J: Clinical applications of Stem cell-derived exosomes.
Signal Transduct Target Ther. 9:172024. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Planat-Benard V, Varin A and Casteilla L:
MSCs and inflammatory cells crosstalk in regenerative medicine:
Concerted actions for optimized resolution driven by energy
metabolism. Front Immunol. 12:6267552021. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Li W, Liu Q, Shi J, Xu X and Xu J: The
role of TNF-α in the fate regulation and functional reprogramming
of mesenchymal stem cells in an inflammatory microenvironment.
Front Immunol. 14:10748632023. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Li H, Tian Y, Xie L, Liu X, Huang Z and Su
W: Mesenchymal stem cells in allergic diseases: Current status.
Allergol Int. 69:35–45. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Cruz FF, Borg ZD, Goodwin M, Sokocevic D,
Wagner DE, Coffey A, Antunes M, Robinson KL, Mitsialis SA,
Kourembanas S, et al: Systemic administration of human bone
Marrow-derived mesenchymal stromal cell extracellular vesicles
ameliorates aspergillus hyphal Extract-induced allergic airway
inflammation in immunocompetent mice. Stem Cells Transl Med.
4:1302–1316. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Saikumar Jayalatha AK, Ketelaar ME, Hesse
L, Badi YE, Zounemat-Kermani N, Brouwer S, Dijk NF, van den Berge
M, Guryev V, Sayers I, et al: IL-33 induced gene expression in
activated Th2 effector cells is dependent on IL-1RL1 haplotype and
asthma status. Eur Respir J. 63:24000052024. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Stark JM, Liu J, Tibbitt CA, Christian M,
Ma J, Wintersand A, Dunst J, Kreslavsky T, Murrell B, Adner M, et
al: Recombinant multimeric dog allergen prevents airway
hyperresponsiveness in a model of asthma marked by vigorous TH 2
and TH 17 cell responses. Allergy. 77:2987–3001. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Zhou J, Lu Y, Wu W and Feng Y:
HMSC-Derived Exosome Inhibited Th2 Cell Differentiation via
Regulating miR-146a-5p/SERPINB2 Pathway. J Immunol Res.
2021:66965252021. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Xie Y, Abel PW, Casale TB and Tu Y: TTH17
cells and corticosteroid insensitivity in severe asthma. J Allergy
Clin Immunol. 149:467–479. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Fang SB, Zhang HY, Wang C, He BX, Liu XQ,
Meng XC, Peng YQ, Xu ZB, Fan XL, Wu ZJ, et al: Small extracellular
vesicles derived from human mesenchymal stromal cells prevent group
2 innate lymphoid cell-dominant allergic airway inflammation
through delivery of miR-146a-5p. J Extracell Vesicles.
9:17232602020. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Zhou JY, Alvarez CA and Cobb BA:
Integration of IL-2 and IL-4 signals coordinates divergent
regulatory T cell responses and drives therapeutic efficacy. Elife.
10:e574172021. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Du YM, Zhuansun YX, Chen R, Lin L, Lin Y
and Li JG: Mesenchymal stem cell exosomes promote immunosuppression
of regulatory T cells in asthma. Exp Cell Res. 363:114–120. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Zhuansun Y, Du Y, Huang F, Lin L, Chen R,
Jiang S and Li J: MSCs exosomal miR-1470 promotes the
differentiation of CD4+CD25+FOXP3+ Tregs in asthmatic patients by
inducing the expression of P27KIP1. Int Immunopharmacol.
77:1059812019. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Bencivenga D, Stampone E, Roberti D, Della
Ragione F and Borriello A: p27Kip1, an intrinsically unstructured
protein with scaffold properties. Cells. 10:22542021. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Li C, Deng C, Zhou T, Hu J, Dai B, Yi F,
Tian N, Jiang L, Dong X, Zhu Q, et al: MicroRNA-370 carried by M2
macrophage-derived exosomes alleviates asthma progression through
inhibiting the FGF1/MAPK/STAT1 axis. Int J Biol Sci. 17:1795–1807.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Dong B, Wang C, Zhang J, Zhang J, Gu Y,
Guo X, Zuo X, Pan H, Hsu AC, Wang G and Wang F: Exosomes from human
umbilical cord mesenchymal stem cells attenuate the inflammation of
severe Steroid-resistant asthma by reshaping macrophage
polarization. Stem Cell Res Ther. 12:2042021. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Dehnavi S, Khodadadi A, Asadirad A and
Ghadiri AA: Immune response modulation by allergen loaded into
mesenchymal stem Cell-derived exosomes as an effective carrier
through sublingual immunotherapy. Immunobiology. 228:1523612023.
View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Bandeira E, Jang SC, Lässer C, Johansson
K, Rådinger M and Park KS: Effects of mesenchymal stem Cell-derived
nanovesicles in experimental allergic airway inflammation. Respir
Res. 24:32023. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Li X, Yang N, Cheng Q, Zhang H, Liu F and
Shang Y: MiR-21-5p in Macrophage-derived exosomes targets Smad7 to
promote epithelial mesenchymal transition of airway epithelial
cells. J Asthma Allergy. 14:513–524. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Shan L, Liu S, Zhang Q, Zhou Q and Shang
Y: Human bone marrow-mesenchymal stem cell-derived exosomal
microRNA-188 reduces bronchial smooth muscle cell proliferation in
asthma through suppressing the JARID2/Wnt/β-catenin axis. Cell
Cycle. 21:352–367. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Zucca E, Corsini E, Galbiati V,
Lange-Consiglio A and Ferrucci F: Evaluation of amniotic
mesenchymal cell derivatives on cytokine production in equine
alveolar macrophages: An in vitro approach to lung inflammation.
Stem Cell Res Ther. 7:1372016. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Zulueta A, Colombo M, Peli V, Falleni M,
Tosi D, Ricciardi M, Baisi A, Bulfamante G, Chiaramonte R and
Caretti A: Lung mesenchymal stem Cells-derived extracellular
vesicles attenuate the inflammatory profile of cystic fibrosis
epithelial cells. Cell Signal. 51:110–118. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Feng CY, Bai SY, Li ML, Zhao JY, Sun JM,
Bao HJ, Ren Y and Su XM: Adipose-derived mesenchymal stem
cell-derived exosomal miR-301a-3p regulates airway smooth muscle
cells during asthma by targeting STAT3. J Asthma Allergy.
15:99–110. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Abbaszadeh H, Ghorbani F, Abbaspour-Aghdam
S, Kamrani A, Valizadeh H, Nadiri M, Sadeghi A, Shamsasenjan K,
Jadidi-Niaragh F, Roshangar L and Ahmadi M: Chronic obstructive
pulmonary disease and asthma: Mesenchymal stem cells and their
extracellular vesicles as potential therapeutic tools. Stem Cell
Res Ther. 13:2622022. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Liu H, Chen Y, Yin G and Xie Q:
Therapeutic prospects of MicroRNAs carried by mesenchymal stem
Cells-derived extracellular vesicles in autoimmune diseases. Life
Sci. 277:1194582021. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
de Castro LL, Xisto DG, Kitoko JZ, Cruz
FF, Olsen PC, Redondo PAG, Ferreira TPT, Weiss DJ, Martins MA,
Morales MM and Rocco PRM: Human adipose tissue mesenchymal stromal
cells and their extracellular vesicles act differentially on lung
mechanics and inflammation in experimental allergic asthma. Stem
Cell Res Ther. 8:1512017. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Song J, Zhu XM and Wei QY: MSCs reduce
airway remodeling in the lungs of asthmatic rats through the
Wnt/β-catenin signaling pathway. Eur Rev Med Pharmacol Sci.
24:11199–11211. 2020.PubMed/NCBI
|
|
101
|
Peng YQ, Deng XH, Xu ZB, Wu ZC and Fu QL:
Mesenchymal stromal cells and their small extracellular vesicles in
allergic diseases: From immunomodulation to therapy. Eur J Immunol.
53:e21495102023. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Yuan JY, Wang XY, Tong ZY, Dong YC, Zhao
JY, Zhang Y and Shang Y: Promising therapeutic functions of bone
marrow mesenchymal stem cells Derived-exosome in asthma. Can Respir
J. 2022:14857192022.PubMed/NCBI
|
|
103
|
Liu W, Lin H, Nie W, Wan J, Jiang Q and
Zhang A: Exosomal miR-221-3p derived from bone marrow mesenchymal
stem cells alleviates asthma progression by targeting FGF2 and
inhibiting the ERK1/2 signaling pathway. Evid Based Complement
Alternat Med. 2022:59108742022.PubMed/NCBI
|
|
104
|
Dong L, Wang Y, Zheng T, Pu Y, Ma Y, Qi X,
Zhang W, Xue F, Shan Z, Liu J, et al: Hypoxic hUCMSC-derived
extracellular vesicles attenuate allergic airway inflammation and
airway remodeling in chronic asthma mice. Stem Cell Res Ther.
12:42021. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Li X and Yang N: Exosome miR-223-3p in the
bone marrow-derived mesenchymal stem cells alleviates the
inflammation and airway remodeling through NLRP3-induced
ASC/Caspase-1/GSDMD signaling pathway. Int Immunopharmacol.
123:1107462023. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Sadeghi M, Dehnavi S, Khodadadi A, Ghadiri
AA, Ganji A, Sharifat M and Asadirad A: Immunomodulatory features
of MSC-derived exosomes decorated with DC-specific aptamer for
improving sublingual immunotherapy in allergic mouse model. Stem
Cell Res Ther. 15:4812024. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Xu W, Wang Y, Ma Y and Yang J: MiR-223
plays a protecting role in neutrophilic asthmatic mice through the
inhibition of NLRP3 inflammasome. Respir Res. 21:1162020.
View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Kim JY, Stevens P, Karpurapu M, Lee H,
Englert JA, Yan P, Lee TJ, Pabla N, Pietrzak M, Park GY, et al:
Targeting ETosis by miR-155 inhibition mitigates mixed granulocytic
asthmatic lung inflammation. Front Immunol. 13:9435542022.
View Article : Google Scholar : PubMed/NCBI
|