|
1
|
Adamo AM and Oteiza PI: Zinc deficiency
and neurodevelopment: The case of neurons. Biofactors. 36:117–124.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Joe P, Getz M, Redman S, Petrilli M, Kranz
TM, Ahmad S and Malaspina D: Serum zinc levels in acute psychiatric
patients: A case series. Psychiatry Res. 261:344–350. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Stachowicz K: Regulation of COX-2
expression by selected trace elements and heavy metals: Health
implications, and changes in neuronal plasticity. A review. J Trace
Elem Med Biol. 79:1272262023. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pfeiffer CC and Iliev V: A study of Zn
deficiency and copper excess in the schizophrenias. Pfeiffer CC:
Neurobiology of Trace Metals Zinc and Copper. Academic Press; New
York: pp. 141–165. 1972
|
|
5
|
Scassellati C, Bonvicini C, Benussi L,
Ghidoni R and Squitti R: Neurodevelopmental disorders: Metallomics
studies for the identification of potential biomarkers associated
to diagnosis and treatment. J Trace Elem Med Biol. 60:1264992020.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nakashima AS and Dyck RH: Zinc and
cortical plasticity. Brain Res Rev. 59:347–373. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Młyniec K, Davies CL, de Agüero Sánchez
IG, Pytka K, Budziszewska B and Nowak G: Essential elements in
depression and anxiety. Part I. Pharmacol Rep. 66:534–544. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kawahara M, Tanaka KI and Kato-Negishi M:
Zinc, carnosine, and neurodegenerative diseases. Nutrients.
10:1472018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tamano H and Takeda A: Age-dependent
modification of intracellular Zn2+ buffering in the
hippocampus and its impact. Biol Pharm Bull. 42:1070–1075. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Moynahan EJ: Letter: Zinc deficiency and
disturbances of mood and visual behaviour. Lancet. 1:911976.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Prasad AS: Discovery of human zinc
deficiency: Its impact on human health and disease. Adv Nutr.
4:176–190. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang J, Um P, Dickerman BA and Liu J:
Zinc, magnesium, selenium and depression: A review of the evidence,
potential mechanisms and implications. Nutrients. 10:5842018.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Teschke R: Aluminum, arsenic, beryllium,
cadmium, chromium, cobalt, copper, iron, lead, mercury, molybdenum,
nickel, platinum, thallium, titanium, vanadium, and zinc: Molecular
aspects in experimental liver injury. Int J Mol Sci. 23:122132022.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chauhan AK, Mittra N, Patel DV and Singh
C: Cyclooxygenase-2 directs microglial activation-mediated
inflammation and oxidative stress leading to intrinsic apoptosis in
Zn-induced parkinsonism. Mol Neurobiol. 55:2162–2173. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kimura K and Kumura J: Preliminary reports
on the metabolism of trace elements in neuro psychiatric diseases.
I. Zinc in schizophrenia. Proc Jap Acad Sci. 41:943–947. 1965.
View Article : Google Scholar
|
|
16
|
Grønli O, Kvamme JM, Friborg O and Wynn R:
Zinc deficiency is common in several psychiatric disorders. PLoS
One. 8:e827932013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Petrilli MA, Kranz TM, Kleinhaus K, Joe P,
Getz M, Johnson P, Chao MV and Malaspina D: The emerging role for
zinc in depression and psychosis. Front Pharmacol. 8:4142017.
View Article : Google Scholar : PubMed/NCBI
|
|
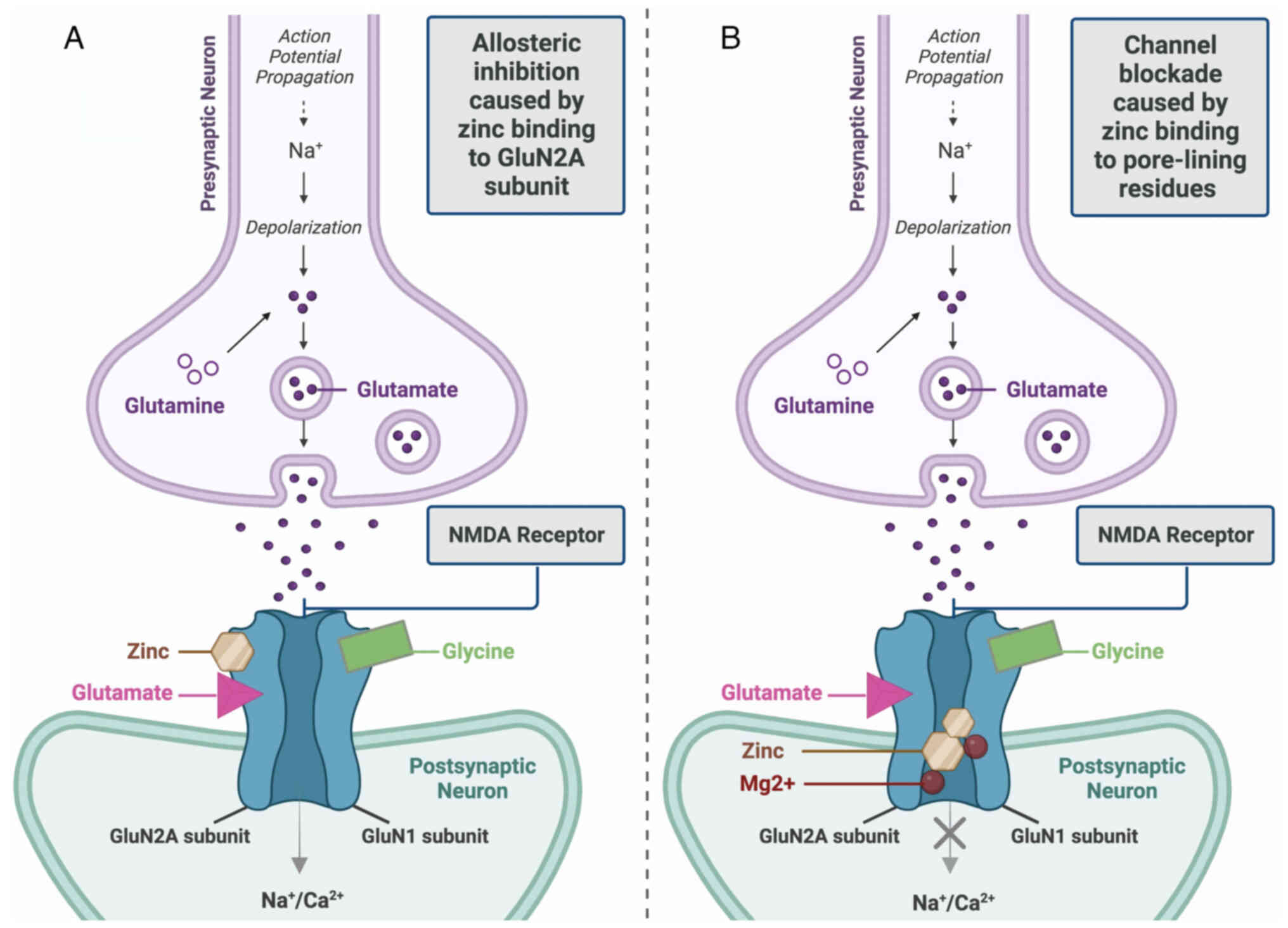
18
|
Murray RM and Lewis SW: Is schizophrenia a
neurodevelopmental disorder? Br Med J (Clin Res Ed). 295:681–682.
1987. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Weinberger DR: Implications of normal
brain development for the pathogenesis of schizophrenia. Arch Gen
Psychiatry. 44:660–669. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sandstead HH, Frederickson CJ and Penland
JG: History of zinc as related to brain function. J Nutr. 130 (2S
Suppl):496S–502S. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Takeda A and Tamano H: Insight into zinc
signaling from dietary zinc deficiency. Brain Res Rev. 62:33–44.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Han S, Gilmartin M, Sheng W and Jin VX:
Integrating rare variant genetics and brain transcriptome data
implicates novel schizophrenia putative risk genes. Schizophr Res.
276:205–213. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
McLardy T: Hippocampal zinc in chronic
alcoholism and schizophrenia. IRCS Med Sci. 2:10101973.
|
|
24
|
Adams CE, Demasters B and Freedman R:
Regional zinc staining in postmortem hippocampus from schizophrenic
patients. Schizophr Res. 18:71–77. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kornhuber J, Lange KW, Kruzik P, Rausch
WD, Gabriel E, Jellinger K and Riederer P: Iron, copper, zinc,
magnesium, and calcium in postmortem brain tissue from
schizophrenic patients. Biol Psychiatry. 36:31–34. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Li D, Achkar JP, Haritunians T, Jacobs JP,
Hui KY, D'Amato M, Brand S, Radford-Smith G, Halfvarson J, Niess
JH, et al: A pleiotropic missense variant in SLC39A8 is associated
with Crohn's disease and human gut microbiome composition.
Gastroenterology. 151:724–732. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Pickrell JK, Berisa T, Liu JZ, Ségurel L,
Tung JY and Hinds DA: Detection and interpretation of shared
genetic influences on 42 human traits. Nat Genet. 48:709–717. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Marger L, Schubert CR and Bertrand D:
Zinc: An underappreciated modulatory factor of brain function.
Biochem Pharmacol. 91:426–435. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Theleritis C, Stefanou MI, Demetriou M,
Alevyzakis E, Triantafyllou K, Smyrnis N, Spandidos DA and Rizos E:
Association of gut dysbiosis with first-episode psychosis (review).
Mol Med Rep. 30:1302024. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Steiner J, Jacobs R, Panteli B, Brauner M,
Schiltz K, Bahn S, Herberth M, Westphal S, Gos T, Walter M, et al:
Acute schizophrenia is accompanied by reduced T cell and increased
B cell immunity. Eur Arch Psychiatry Clin Neurosci. 260:509–518.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Carrera N, Arrojo M, Sanjuán J, Ramos-Ríos
R, Paz E, Suárez-Rama JJ, Páramo M, Agra S, Brenlla J, Martínez S,
et al: Association study of nonsynonymous single nucleotide
polymorphisms in schizophrenia. Biol Psychiatry. 71:169–177. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Li S, Ma C, Li Y, Chen R, Liu Y, Wan LP,
Xiong Q, Wang C, Huo Y, Dang X, et al: The schizophrenia-associated
missense variant rs13107325 regulates dendritic spine density.
Transl Psychiatry. 12:3612022. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Tseng WC, Reinhart V, Lanz TA, Weber ML,
Pang J, Le KXV, Bell RD, O'Donnell P and Buhl DL:
Schizophrenia-associated SLC39A8 polymorphism is a loss-of-function
allele altering glutamate receptor and innate immune signaling.
Transl Psychiatr. 11:1362021. View Article : Google Scholar
|
|
34
|
Scarr E, Udawela M, Greenough MA, Neo J,
Suk SM, Money TT, Upadhyay A, Bush AI, Everall IP, Thomas EA and
Dean B: Increased cortical expression of the zinc transporter
SLC39A12 suggests a breakdown in zinc cellular homeostasis as part
of the pathophysiology of schizophrenia. NPJ Schizophr.
2:160022016. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Perez-Becerril C, Morris AG, Mortimer A,
McKenna PJ and de Belleroche J: Allelic variants in the zinc
transporter-3 gene, SLC30A3, a candidate gene identified from gene
expression studies, show gender-specific association with
schizophrenia. Eur Psychiatry. 29:172–178. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Sun Y, Hu D, Liang J, Bao YP, Meng SQ, Lu
L and Shi J: Association between variants of zinc finger genes and
psychiatric disorders: Systematic review and meta-analysis.
Schizophr Res. 162:124–137. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Lima VB, Sampaio Fde A, Bezerra DL, Moita
Neto JM and Marreiro Ddo N: Parameters of glycemic control and
their relationship with zinc concentrations in blood and with
superoxide dismutase enzyme activity in type 2 diabetes patients.
Arq Bras Endocrinol Metabol. 55:701–707. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Noleto Magalhães RC, Guedes Borges de
Araujo C, Batista de Sousa Lima V, Machado Moita Neto J, do
Nascimento Nogueira N and do Nascimento Marreiro D: Nutritional
status of zinc and activity superoxide dismutase in chronic renal
patients undergoing hemodialysis. Nutr Hosp. 26:1456–1461.
2011.PubMed/NCBI
|
|
39
|
Marreiro DDN, Cruz KJC, Morais JBS,
Beserra JB, Severo JS and de Oliveira ARS: Zinc and oxidative
stress: Current mechanisms. Antioxidants (Basel). 6:242017.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Skalny AV, Rink L, Ajsuvakova OP, Aschner
M, Gritsenko VA, Alekseenko SI, Svistunov AA, Petrakis D, Spandidos
DA, Aaseth J, et al: Zinc and respiratory tract infections:
Perspectives for COVID-19 (review). Int J Mol Med. 46:17–26.
2020.PubMed/NCBI
|
|
41
|
Consolo M, Amoroso A, Spandidos DA and
Mazzarino MC: Matrix metalloproteinases and their inhibitors as
markers of inflammation and fibrosis in chronic liver disease
(review). Int J Mol Med. 24:143–152. 2009.PubMed/NCBI
|
|
42
|
Tsatsakis A, Renieri E, Tsoukalas D, Buga
AM, Sarandi E, Vakonaki E, Fragkiadaki P, Alegakis A, Nikitovic D,
Calina D, et al: A novel nutraceutical formulation increases
telomere length and activates telomerase activity in middle-aged
rats. Mol Med Rep. 28:2322023. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Tsoukalas D, Buga AM, Docea AO, Sarandi E,
Mitrut R, Renieri E, Spandidos DA, Rogoveanu I, Cercelaru L,
Niculescu M, et al: Reversal of brain aging by targeting
telomerase: A nutraceutical approach. Int J Mol Med. 48:1992021.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Santa Cruz EC, Madrid KC, Arruda MAZ and
Sussulini A: Association between trace elements in serum from
bipolar disorder and schizophrenia patients considering treatment
effects. J Trace Elem Med Biol. 59:1264672020. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Nowak G: Does interaction between zinc and
glutamate system play a significant role in the mechanism of
antidepressant action? Acta Pol Pharm. 58:73–75. 2001.PubMed/NCBI
|
|
46
|
Prakash A, Bharti K and Majeed AB: Zinc:
indications in brain disorders. Fundam Clin Pharmacol. 29:131–149.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Salim S: Oxidative stress and
psychological disorders. Curr Neuropharmacol. 12:140–147. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Akarsu S, Bolu A, Aydemir E, Znir SB, Kurt
YG, Znir S, Erdem M and Uzun Ö: The relationship between the number
of manic episodes and oxidative stress indicators in bipolar
disorder. Psychiatry Investig. 15:514–519. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Guo CH, Chen PC, Yeh MS, Hsiung DY and
Wang CL: Cu/Zn ratios are associated with nutritional status,
oxidative stress, inflammation, and immune abnormalities in
patients on peritoneal dialysis. Clin Biochem. 44:275–280. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Kunz M, Gama CS, Andreazza AC, Salvador M,
Ceresér KM, Gomes FA, Belmonte-de-Abreu PS, Berk M and Kapczinski
F: Elevated serum superoxide dismutase and thiobarbituric acid
reactive substances in different phases of bipolar disorder and in
schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry.
32:1677–1681. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Hendouei N, Farnia S, Mohseni F, Salehi A,
Bagheri M, Shadfar F, Barzegar F, Hoseini SD, Charati JY and Shaki
F: Alterations in oxidative stress markers and its correlation with
clinical findings in schizophrenic patients consuming perphenazine,
clozapine and risperidone. Biomed Pharmacother. 103:965–972. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Al-Hakeim HK, Al-Musawi AF, Al-Mulla A,
Al-Dujaili AH, Debnath M and Maes M: The
interleukin-6/interleukin-23/T helper 17-axis as a driver of
neuro-immune toxicity in the major neurocognitive psychosis or
deficit schizophrenia: A precision nomothetic psychiatry analysis.
PLoS One. 17:e02758392022. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Al-Hakeim HK, Altufaili MF, Almulla AF,
Moustafa SR and Maes M: Increased lipid peroxidation and lowered
antioxidant defenses predict methamphetamine induced psychosis.
Cells. 11:36942022. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Pfeiffer CC and Bacchi D: Copper, zinc,
manganese, niacin and pyridoxine in the schizophrenias. Appl Nutr.
27:9–39. 1975.
|
|
55
|
Srinivasan DP, Marr S, Wareing RA and
Birch NJ: Magnesium Zn and copper in acute psychiatric patients.
Mag Bull. 4:45–48. 1982.
|
|
56
|
Gillin JC, Carpenter WT, Hambidge KM,
Wyatt RJ and Henkin RI: Zinc and copper in patients with
schizophrenia. Encephale. 8:435–444. 1982.PubMed/NCBI
|
|
57
|
Potkin SG, Shore D, Torrey EF, Weinberger
DR, Gillin JC, Henkin RI, Agarwal RP and Wyatt RJ: Cerebrospinal
fluid zinc concentrations in ex-heroin addicts and patients with
schizophrenia: Some preliminary observations. Biol Psychiatry.
17:1315–1322. 1982.PubMed/NCBI
|
|
58
|
Vaddadi KS, Gilleard CJ, Mindham RH and
Butler R: A controlled trial of prostaglandin E1 precursor in
chronic neuroleptic resistant schizophrenic patients.
Psychopharmacology (Berl). 88:362–367. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Craven C, Duggan PF, Buckley N and
Gaughran F: Serum zinc levels in patients with schizophrenia and
their mothers. Schizophr Res. 26:83–84. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Herrán A, García-Unzueta MT,
Fernández-González MD, Vázquez-Barquero JL, Alvarez C and Amado JA:
Higher levels of serum copper in schizophrenic patients treated
with depot neuroleptics. Psychiatry Res. 94:51–58. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Stanley PC and Wakwe VC: Toxic trace
metals in the mentally ill patients. Niger Postgrad Med J.
9:199–204. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Tokdemir M, Polat SA, Acik Y, Gursu F,
Cikim G and Deniz O: Blood zinc and copper concentrations in
criminal and noncriminal schizophrenic men. Arch Androl.
49:365–368. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Nechifor M, Vaideanu C, Palamaru I, Borza
C and Mindreci I: The influence of some antipsychotics on
erythrocyte magnesium and plasma magnesium, calcium, copper and
zinc in patients with paranoid schizophrenia. J Am Coll Nutr.
23:549S–551S. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Yanik M, Kocyigit A, Tutkun H, Vural H and
Herken H: Plasma manganese, selenium, zinc, copper, and iron
concentrations in patients with schizophrenia. Biol Trace Elem Res.
98:109–117. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Farzin D, Mansouri N and Yazdani T:
Elevated plasma copper/zinc ratios in patients with schizophrenia.
Eur Neuropsychopharmacol. 16:S364–S365. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Devi PU, Chinnaswamy P, Murugan S and
Selvi S: Plasma levels of trace elements in patients with different
symptoms of schizophrenia. Biosci Biotechnol Res Asia. 5:261–268.
2008.
|
|
67
|
Rahman A, Azad MAK, Hossain I, Qusar MMAS,
Bari W, Begum F, Huq SMI and Hasnat A: Zinc, manganese, calcium,
copper, and cadmium level in scalp hair samples of schizophrenic
patients. Biol Trace Elem Res. 127:102–108. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Ghanem AEA, Ali EMM, El-Bakary AA, El
Morsi D, Elkanishi SMH, Saleh ES and El-Said H: Copper and Zinc
levels in hair of both schizophrenic and depressed. Mansoura J
Forensic Med Clin Toxicol. 17:89–102. 2009. View Article : Google Scholar
|
|
69
|
Arinola G, Idonije B, Akinlade K and
Ihenyen O: Essential trace metals and heavy metals in newly
diagnosed schizophrenic patients and those on anti-psychotic
medication. J Res Med Sci. 15:245–249. 2010.PubMed/NCBI
|
|
70
|
Kaya B, Akdağ N, Fadıllıoğlu E, Taycan SE,
Emre MH, Unal S, Sayal A, Erdoğan H and Polat R: Elements levels
and glucose-6-phosphate dehydrogenase activity in blood of patients
with schizophrenia. J Psychiatry Neurol Sci. 25:198–205. 2012.
|
|
71
|
Cai L, Chen T, Yang J, Zhou K, Yan X, Chen
W, Sun L, Li L, Qin S, Wang P, et al: Serum trace element
differences between schizophrenia patients and controls in the Han
Chinese population. Sci Rep. 5:150132015. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Olabanji O, Ngila JC, Msagati TAM, Oluyemi
EA, Fatoye FO and Mamba BB: Effect of metal poisoning and the
implications of gender and age on the elemental composition in
patients with mental behavioural disorders. Afr J Biotechnol.
10:3585–3593. 2011.
|
|
73
|
Vidović B, Dorđević B, Milovanović S,
Škrivanj S, Pavlović Z, Stefanović A and Kotur-Stevuljević J:
Selenium, zinc, and copper plasma levels in patients with
schizophrenia: relationship with metabolic risk factors. Biol Trace
Elem Res. 156:22–28. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Sharma SK, Sood S, Sharma A and Gupta ID:
Estimation of serum zinc and copper levels patients with
schizophrenia: A preliminary study. SL J Psychiatry. 5:14–17.
2013.
|
|
75
|
Asare G, Tetteh R, Amedonu E, Asiedu B and
Doku D: Toxicity, deficiency and dysmetabolism of trace elements in
Ghanaian clinically stable schizophrenics. Open Access Maced J Med
Sci. 2:293–298. 2014. View Article : Google Scholar
|
|
76
|
Nawaz R, Zahir E, Siddiqui S, Usmani A and
Shad KF: The role of trace metals and environmental factors in the
onset and progression of schizophrenia in Pakistani population.
World J Neurosci. 4:450–460. 2014. View Article : Google Scholar
|
|
77
|
Liu T, Lu QB, Yan L, Guo J, Feng F, Qiu J
and Wang J: Comparative study on serum levels of 10 trace elements
in schizophrenia. PLoS One. 10:e01336222015. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Lin T, Liu T, Lin Y, Yan L, Chen Z and
Wang J: Comparative study on serum levels of macro and trace
elements in schizophrenia based on supervised learning methods. J
Trace Elem Med Biol. 43:202–208. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Velthorst E, Smith L, Bello G, Austin C,
Gennings C, Modabbernia A, Franke N, Frangou S, Wright R, de Haan
L, et al: New research strategy for measuring pre- and postnatal
metal dysregulation in psychotic disorders. Schizophr Bull.
43:1153–1157. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Modabbernia A, Velthorst E, Gennings C, De
Haan L, Austin C, Sutterland A, Mollon J, Frangou S, Wright R,
Arora M and Reichenberg A: Early-life metal exposure and
schizophrenia: A proof-of-concept study using novel tooth-matrix
biomarkers. Eur Psychiatry. 36:1–6. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Chen X, Li Y, Zhang T, Yao Y, Shen C and
Xue Y: Association of serum trace elements with schizophrenia and
effects of antipsychotic treatment. Biol Trace Elem Res. 181:22–30.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Li Z, Liu Y, Li X, Ju W, Wu G, Yang X, Fu
X and Gao X: Association of elements with schizophrenia and
intervention of selenium supplements. Biol Trace Elem Res.
183:16–21. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Cao B, Yan L, Ma J, Jin M, Park C, Nozari
Y, Kazmierczak OP, Zuckerman H, Lee Y, Pan Z, et al: Comparison of
serum essential trace metals between patients with schizophrenia
and healthy controls. J Trace Elem Med Biol. 51:79–85. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Ma J, Yan L, Guo T, Yang S, Liu Y, Xie Q,
Ni D and Wang J: Association between serum essential metal elements
and the risk of schizophrenia in China. Sci Rep. 10:108752020.
View Article : Google Scholar : PubMed/NCBI
|
|
85
|
de Souza Pessôa G, de Jesus JR, Balbuena
TS and Arruda MAZ: Metallomics-based platforms for comparing the
human blood serum profiles between bipolar disorder and
schizophrenia patients. Rapid Commun Mass Spectrom. 34 (Suppl
3):e86982020. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Uddin SMN, Sultana F, Uddin MG, Dewan SMR,
Hossain MK and Islam MS: Effect of antioxidant, malondialdehyde,
macro-mineral, and trace element serum concentrations in
Bangladeshi patients with schizophrenia: A case-control study.
Health Sci Rep. 4:e2912021. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Awais MH, Aamir M, Bibi A, Ali S, Ahmed W
and Safdar SA: Association of trace metals in patients with
schizophrenia. J Coll Physicians Surg Pak. 32:193–196. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Lotan A, Luza S, Opazo CM, Ayton S, Lane
DJR, Mancuso S, Pereira A, Sundram S, Weickert CS, Bousman C, et
al: Perturbed iron biology in the prefrontal cortex of people with
schizophrenia. Mol Psychiatry. 28:2058–2070. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Dos Santos AB, Bezerra MA, Rocha ME,
Barreto GE and Kohlmeier KA: Higher zinc concentrations in hair of
Parkinson's disease are associated with psychotic complications and
depression. J Neural Transm (Vienna). 126:1291–1301. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Tabata K, Miyashita M, Yamasaki S, Toriumi
K, Ando S, Suzuki K, Endo K, Morimoto Y, Tomita Y, Yamaguchi S, et
al: Hair zinc levels and psychosis risk among adolescents.
Schizophrenia (Heidelb). 8:1072022. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Joe P, Petrilli M, Malaspina D and
Weissman J: Zinc in schizophrenia: A meta-analysis. Gen Hosp
Psychiatry. 53:19–24. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Zaks N, Austin C, Arora M and Reichenberg
A: Reprint of: Elemental dysregulation in psychotic spectrum
disorders: A review and research synthesis. Schizophr Res.
247:33–40. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
da Paulsen Bda S, Cardoso SC, Stelling MP,
Cadilhe DV and Rehen SK: Valproate reverts zinc and potassium
imbalance in schizophrenia-derived reprogrammed cells. Schizophr
Res. 154:30–35. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Mortazavi M, Farzin D, Zarhghami M,
Hosseini SH, Mansoori P and Nateghi G: Efficacy of zinc sulfate as
an add-on therapy to risperidone versus risperidone alone in
patients with schizophrenia: A double-blind randomized
placebo-controlled trial. Iran J Psychiatry Behav Sci. 9:e8532015.
View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Pfeiffer CC and Sohler A: Treatment of
pyroluric schizophrenia with large doses of pyridoxine and a
dietary supplement of zinc. J Orthomol Med. 3:292–300. 1974.
|
|
96
|
Grabrucker AM and Rowan Garner CC:
Brain-delivery of zinc-ions as potential treatment for neurological
diseases: Mini review. Drug Deliv Lett. 1:13–23. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Rohde J, Claussen MC, Kuechenhoff B,
Seifritz E and Schuepbach D: Combined symptomatology of psychosis,
pica syndrome, and hippocampal sclerosis: A case report. Int J Eat
Disord. 46:89–91. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Russo AJ and de Vito R: Decreased serum
hepatocyte growth factor (HGF) in individuals with schizophrenia
normalizes after zinc and B-6 therapy. Proteomics Insights.
3:71–77. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Russo A: Decreased serum hepatocyte growth
factor (HGF) in individuals with bipolar disorder normalizes after
zinc and anti-oxidant therapy. Nutr Metab Insights. 3:49–55. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Czerniak P and Haim DB: Phenothiazine
derivatives and brain zinc. Turnover radioactive isotope study.
Arch Neurol. 24:555–560. 1971. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Alizadeh F, Davoodian N, Kazemi H,
Ghasemi-Kasman M and Shaerzadeh F: Prenatal zinc supplementation
attenuates lipopolysaccharide-induced behavioral impairments in
maternal immune activation model. Behav Brain Res. 377:1122472020.
View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Mousaviyan R, Davoodian N, Alizadeh F,
Ghasemi-Kasman M, Mousavi SA, Shaerzadeh F and Kazemi H: Zinc
supplementation during pregnancy alleviates
lipopolysaccharide-induced glial activation and inflammatory
markers expression in a rat model of maternal immune activation.
Biol Trace Elem Res. 199:4193–4204. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Savareh E, Davoodian N, Mousaviyan R,
Ghasemi-Kasman M, Atashabparvar A and Eftekhar E: Prenatal zinc
supplementation ameliorates hippocampal astrocytes activation and
inflammatory cytokines expression induced by lipopolysaccharide in
a rat model of maternal immune activation. Basic Clin Neurosci.
13:335–347. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Coyle P, Tran N, Fung JNT, Summers BL and
Rofe AM: Maternal dietary zinc supplementation prevents aberrant
behaviour in an object recognition task in mice offspring exposed
to LPS in early pregnancy. Behav Brain Res. 197:210–218. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Onaolapo OJ, Ademakinwa OQ, Olalekan TO
and Onaolapo AY: Ketamine-induced behavioural and brain oxidative
changes in mice: An assessment of possible beneficial effects of
zinc as mono- or adjunct therapy. Psychopharmacology (Berl).
234:2707–2725. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Joshi M, Akhtar M, Najmi AK, Khuroo AH and
Goswami D: Effect of zinc in animal models of anxiety, depression
and psychosis. Hum Exp Toxicol. 31:1237–1243. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Bayer TA, Falkai P and Maier W: Genetic
and non-genetic vulnerability factors in schizophrenia: The basis
of the ‘two hit hypothesis’. J Psychiatr Res. 33:543–548. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Giannopoulou I, Georgiades S, Stefanou MI,
Spandidos DA and Rizos E: Links between trauma and psychosis
(review). Exp Ther Med. 26:3862023. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Morgan C, Charalambides M, Hutchinson G
and Murray RM: Migration, ethnicity, and psychosis: Toward a
sociodevelopmental model. Schizophr Bull. 36:655–664. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Davis EG, Humphreys KL, McEwen LM, Sacchet
MD, Camacho MC, MacIsaac JL, Lin DTS, Kobor MS and Gotlib IH:
Accelerated DNA methylation age in adolescent girls: Associations
with elevated diurnal cortisol and reduced hippocampal volume.
Transl Psychiatry. 7:e12232017. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Chen Q, Li D, Jin W, Shi Y, Li Z, Ma P,
Sun J, Chen S, Li P and Lin P: Research progress on the correlation
between epigenetics and schizophrenia. Front Neurosci.
15:6887272021. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Alameda L, Rodriguez V, Carr E, Aas M,
Trotta G, Marino P, Vorontsova N, Herane-Vives A, Gadelrab R,
Spinazzola E, et al: A systematic review on mediators between
adversity and psychosis: Potential targets for treatment. Psychol
Med. 50:1966–1976. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Fraker PJ and King LE: Reprogramming of
the immune system during zinc deficiency. Annu Rev Nutr.
24:277–298. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Charmandari E, Kino T, Souvatzoglou E and
Chrousos GP: Pediatric stress: Hormonal mediators and human
development. Horm Res. 59:161–179. 2003.PubMed/NCBI
|
|
115
|
Lardinois M, Lataster T, Mengelers R, Van
Os J and Myin-Germeys I: Childhood trauma and increased stress
sensitivity in psychosis. Acta Psychiatr Scand. 123:28–35. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Walker EF, Brennan PA, Esterberg M,
Brasfield J, Pearce B and Compton MT: Longitudinal changes in
cortisol secretion and conversion to psychosis in at-risk youth. J
Abnorm Psychol. 119:401–408. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Walker EF, Trotman HD, Pearce BD,
Addington J, Cadenhead KS, Cornblatt BA, Heinssen R, Mathalon DH,
Perkins DO, Seidman LJ, et al: Cortisol levels and risk for
psychosis: Initial findings from the North American prodrome
longitudinal study. Biol Psychiatry. 74:410–417. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Sapolsky RM: Glucocorticoids and
hippocampal atrophy in neuropsychiatric disorders. Arch Gen
Psychiatry. 57:925–935. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Vita A, De Peri L, Silenzi C and Dieci M:
Brain morphology in first-episode schizophrenia: A meta-analysis of
quantitative magnetic resonance imaging studies. Schizophr Res.
82:75–88. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Thompson Ray M, Weickert CS, Wyatt E and
Webster MJ: Decreased BDNF, trkB-TK+ and GAD67 mRNA expression in
the hippocampus of individuals with schizophrenia and mood
disorders. J Psychiatry Neurosci. 36:195–203. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Daskalakis NP, De Kloet ER, Yehuda R,
Malaspina D and Kranz TM: Early life stress effects on
glucocorticoid-BDNF interplay in the hippocampus. Front Mol
Neurosci. 8:682015. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Rizos EN, Rontos I, Laskos E, Arsenis G,
Michalopoulou PG, Vasilopoulos D, Gournellis R and Lykouras L:
Investigation of serum BDNF levels in drug-naive patients with
schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry.
32:1308–1311. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Rizos EN, Papathanasiou M, Michalopoulou
PG, Mazioti A, Douzenis A, Kastania A, Nikolaidou P, Laskos E,
Vasilopoulou K and Lykouras L: Association of serum BDNF levels
with hippocampal volumes in first psychotic episode drug-naive
schizophrenic patients. Schizophr Res. 129:201–204. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Rizos EN, Michalopoulou PG, Siafakas N,
Stefanis N, Douzenis A, Rontos I, Laskos E, Kastania A, Zoumpourlis
V and Lykouras L: Association of serum brain-derived neurotrophic
factor and duration of untreated psychosis in first-episode
patients with schizophrenia. Neuropsychobiology. 62:87–90. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Theleritis C, Fisher HL, Shäfer I, Winters
L, Stahl D, Morgan C, Dazzan P, Breedvelt J, Sambath I, Vitoratou
S, et al: Brain derived neurotropic factor (BDNF) is associated
with childhood abuse but not cognitive domains in first episode
psychosis. Schizophr Res. 159:56–61. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Tsang BL, Holsted E, McDonald CM, Brown
KH, Black R, Mbuya MNN, Grant F, Rowe LA and Manger MS: Effects of
foods fortified with zinc, alone or cofortified with multiple
micronutrients, on health and functional outcomes: A systematic
review and meta-analysis. Adv Nutr. 12:1821–1837. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Flores G, Morales-Medina JC and Diaz A:
Neuronal and brain morphological changes in animal models of
schizophrenia. Behav Brain Res. 301:190–203. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Bronson SL and Bale TL: Prenatal
stress-induced increases in placental inflammation and offspring
hyperactivity are male-specific and ameliorated by maternal
antiinflammatory treatment. Endocrinology. 155:2635–2646. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Walker CK, Ashwood P and Hertz-Picciotto
I: Preeclampsia, placental insufficiency, autism, and
antiphospholipid antibodies-reply. JAMA Pediatr. 169:606–607. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Kurita H, Ohsako S, Hashimoto S, Yoshinaga
J and Tohyama C: Prenatal zinc deficiency-dependent epigenetic
alterations of mouse metallothionein-2 gene. J Nutr Biochem.
24:256–266. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Tellez-Merlo G, Morales-Medina JC,
Camacho-Ábrego I, Juárez-Díaz I, Aguilar-Alonso P, de la Cruz F,
Iannitti T and Flores G: Prenatal immune challenge induces
behavioral deficits, neuronal remodeling, and increases brain
nitric oxide and zinc levels in the male rat offspring.
Neuroscience. 406:594–605. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Camacho-Abrego I, González-Cano SI,
Aguilar-Alonso P, Brambila E, de la Cruz F and Flores G: Changes in
nitric oxide, zinc and metallothionein levels in limbic regions at
pre-pubertal and post-pubertal ages presented in an animal model of
schizophrenia. J Chem Neuroanat. 111:1018892021. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Lee K, Mills Z, Cheung P, Cheyne JE and
Montgomery JM: The role of zinc and NMDA receptors in autism
spectrum disorders. Pharmaceuticals (Basel). 16:12022. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Paz RD, Tardito S, Atzori M and Tseng KY:
Glutamatergic dysfunction in schizophrenia: From basic neuroscience
to clinical psychopharmacology. Eur Neuropsychopharmacol.
18:773–786. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Walsh WJ, Isaacson HR, Rehman F and Hall
A: Elevated blood copper/zinc ratios in assaultive young males.
Physiol Behav. 62:327–329. 1997. View Article : Google Scholar : PubMed/NCBI
|