|
1
|
Dankhara N, Holla I, Ramarao S and
Kalikkot Thekkeveedu R: Bronchopulmonary dysplasia: Pathogenesis
and pathophysiology. J Clin Med. 12:42072023. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Collaco JM and McGrath-Morrow SA:
Long-term outcomes of infants with severe BPD. Semin Perinatol.
48:1518912024. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gilfillan M, Bhandari A and Bhandari V:
Diagnosis and management of bronchopulmonary dysplasia. BMJ.
375:n19742021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Shukla VV and Ambalavanan N: Recent
advances in bronchopulmonary dysplasia. Indian J Pediatr.
88:690–695. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chen X, Yuan L, Jiang S, Gu X, Lei X, Hu
L, Xiao T, Zhu Y, Dang D, Li W, et al: Synergistic effects of
achieving perinatal interventions on bronchopulmonary dysplasia in
preterm infants. Eur J Pediatr. 183:1711–1721. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
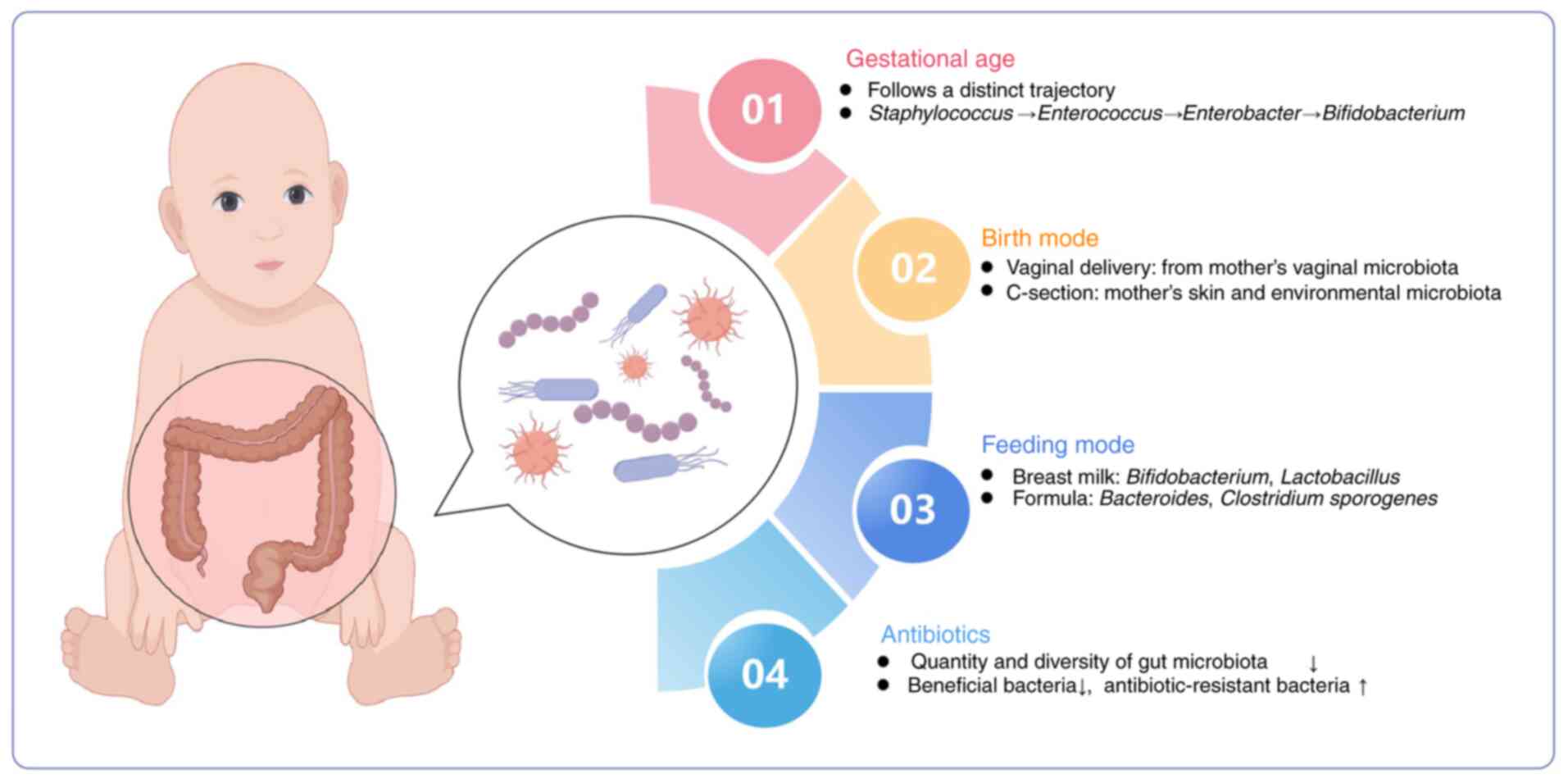
Lu D, Huang Y, Kong Y, Tao T and Zhu X:
Gut microecology: Why our microbes could be key to our health.
Biomed Pharmacother. 131:1107842020. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wang H, Zheng Y, Yang M, Wang L, Xu Y, You
S, Mao N, Fan J and Ren S: Gut microecology: Effective targets for
natural products to modulate uric acid metabolism. Front Pharmacol.
15:14467762024. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gu S, Chen Y, Wu Z, Chen Y, Gao H, Lv L,
Guo F, Zhang X, Luo R, Huang C, et al: Alterations of the gut
microbiota in patients with coronavirus disease 2019 or H1N1
influenza. Clin Infect Dis. 71:2669–2678. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
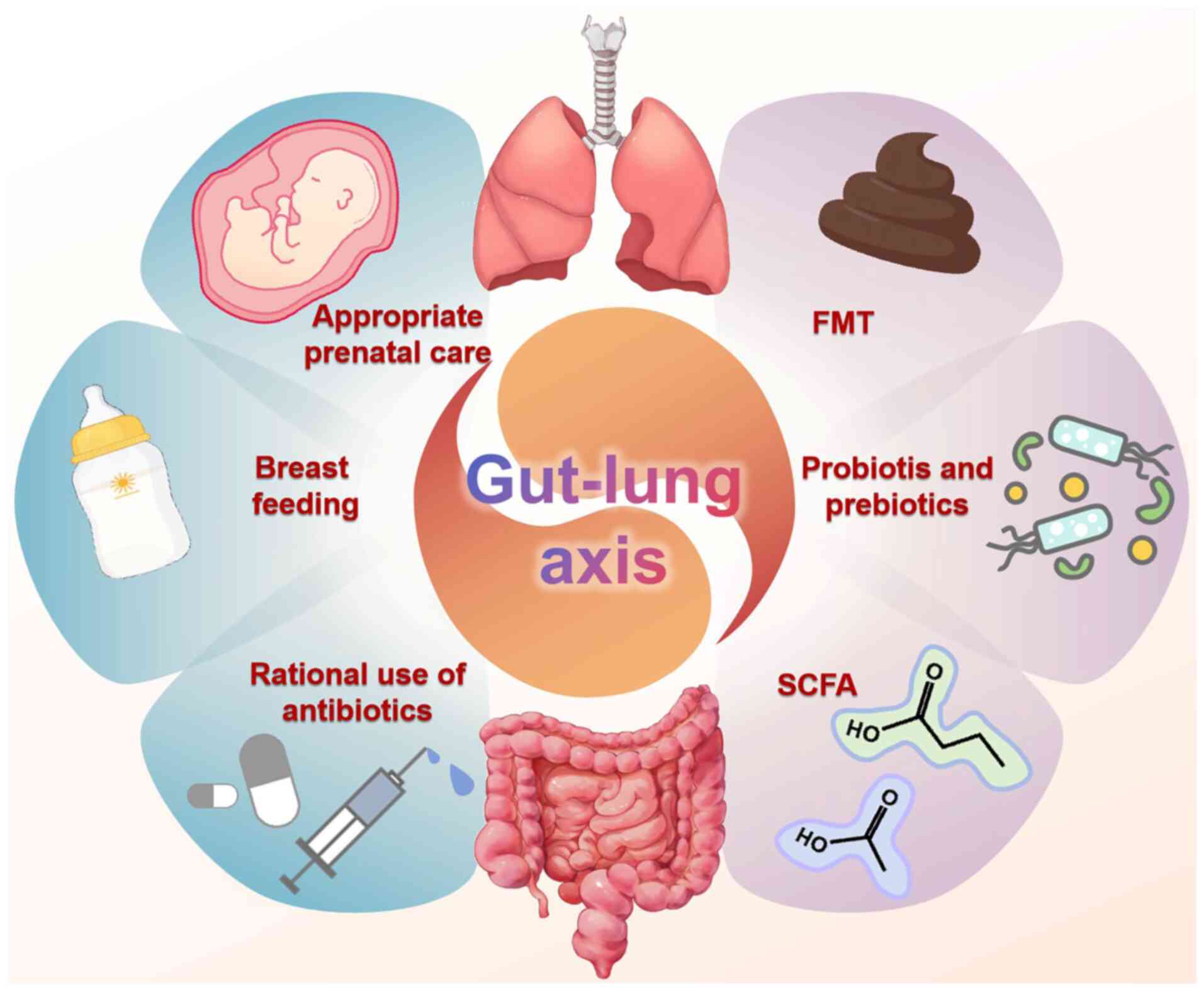
9
|
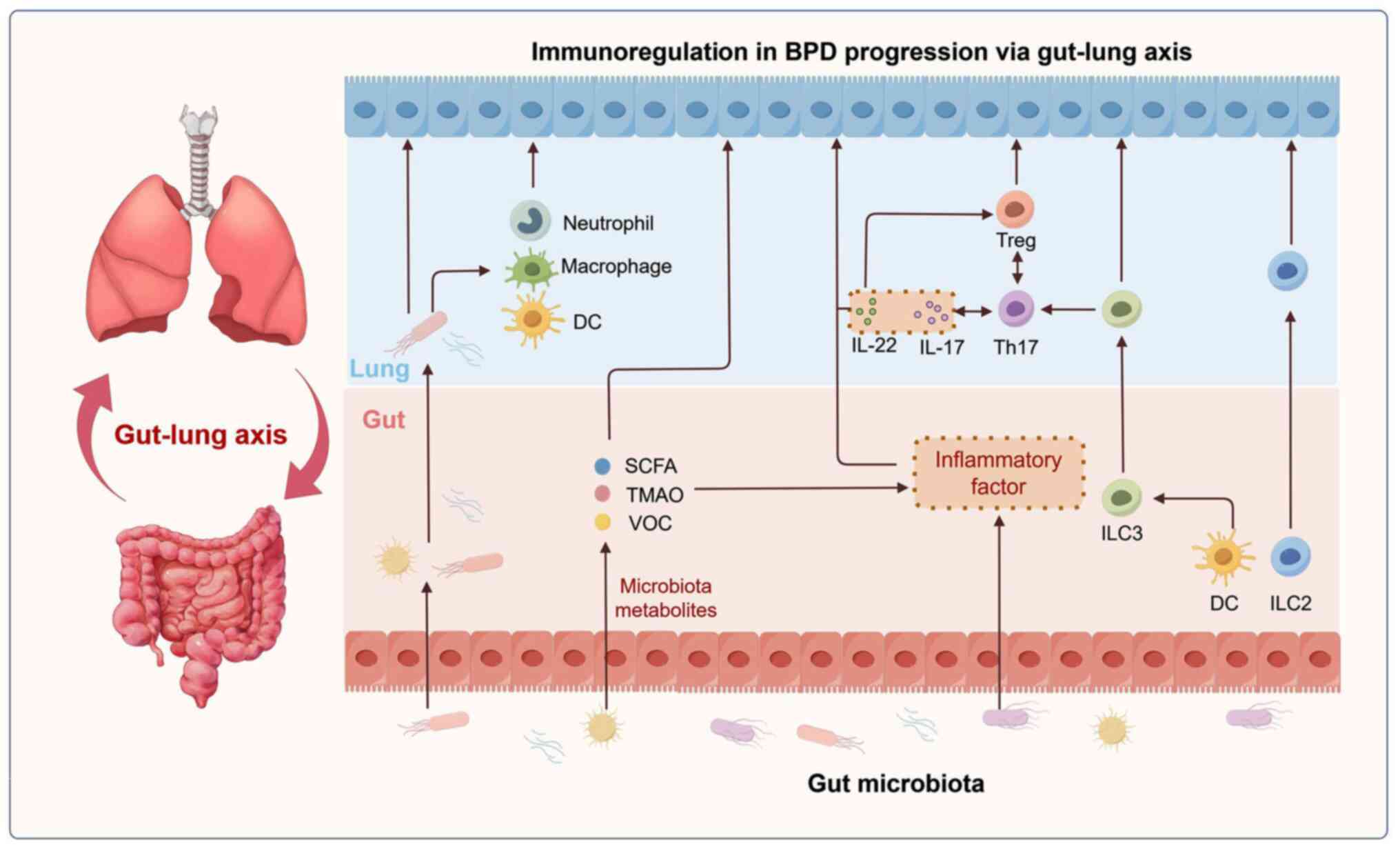
Raftery AL, Tsantikos E, Harris NL and
Hibbs ML: Links between inflammatory bowel disease and chronic
obstructive pulmonary disease. Front Immunol. 11:21442020.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ryan FJ, Drew DP, Douglas C, Leong LEX,
Moldovan M, Lynn M, Fink N, Sribnaia A, Penttila I, McPhee AJ, et
al: Changes in the composition of the gut microbiota and the blood
transcriptome in preterm infants at less than 29 weeks gestation
diagnosed with bronchopulmonary dysplasia. mSystems. 4:e00484–19.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chen SM, Lin CP and Jan MS: Early gut
microbiota changes in preterm infants with bronchopulmonary
dysplasia: A pilot Case-control study. Am J Perinatol.
38:1142–1149. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhao L, Song W and Chen YG:
Mesenchymal-epithelial interaction regulates gastrointestinal tract
development in mouse embryos. Cell Rep. 40:1110532022. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Batki J, Hetzel S, Schifferl D, Bolondi A,
Walther M, Wittler L, Grosswendt S, Herrmann BG and Meissner A:
Extraembryonic gut endoderm cells undergo programmed cell death
during development. Nat Cell Biol. 26:868–877. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Fang Y and Li X: Metabolic and epigenetic
regulation of endoderm differentiation. Trends Cell Biol.
32:151–164. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Aros CJ, Pantoja CJ and Gomperts BN: Wnt
signaling in lung development, regeneration, and disease
progression. Commun Biol. 4:6012021. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Aspal M and Zemans RL: Mechanisms of
ATII-to-ATI cell differentiation during lung regeneration. Int J
Mol Sci. 21:31882020. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yang J, Wang J, Ding B, Jiang Z, Yu F, Li
D, Sun W, Wang L, Xu H and Hu S: Feedback delivery of BMP 7 on the
pathological oxidative stress via smart hyaluronic acid hydrogel
potentiated the repairing of the gut epithelial integrity. Int J
Biol Macromol. 282:1367942024. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Herriges MJ, Tischfield DJ, Cui Z, Morley
MP, Han Y, Babu A, Li S, Lu M, Cendan I, Garcia BA, et al: The
NANCI-Nkx2.1 gene duplex buffers Nkx2.1 expression to maintain lung
development and homeostasis. Genes Dev. 31:889–903. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chelladurai P, Kuenne C, Bourgeois A,
Günther S, Valasarajan C, Cherian AV, Rottier RJ, Romanet C,
Weigert A, Boucherat O, et al: Epigenetic reactivation of
transcriptional programs orchestrating fetal lung development in
human pulmonary hypertension. Sci Transl Med. 14:eabe54072022.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Dolmatov IY, Kalacheva NV, Tkacheva ES,
Shulga AP, Zavalnaya EG, Shamshurina EV, Girich AS, Boyko AV and
Eliseikina MG: Expression of Piwi, MMP, TIMP, and Sox during Gut
Regeneration in Holothurian Eupentacta fraudatrix (Holothuroidea,
Dendrochirotida). Genes (Basel). 12:12922021. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Budden KF, Gellatly SL, Wood DL, Cooper
MA, Morrison M, Hugenholtz P and Hansbro PM: Emerging pathogenic
links between microbiota and the gut-lung axis. Nat Rev Microbiol.
15:55–63. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Thursby E and Juge N: Introduction to the
human gut microbiota. Biochem J. 474:1823–1836. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Keely S, Talley NJ and Hansbro PM:
Pulmonary-intestinal cross-talk in mucosal inflammatory disease.
Mucosal Immunol. 5:7–18. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Keely S and Hansbro PM: Lung-gut cross
talk: A potential mechanism for intestinal dysfunction in patients
with COPD. Chest. 145:199–200. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Liu G, Mateer SW, Hsu A, Goggins BJ, Tay
H, Mathe A, Fan K, Neal R, Bruce J, Burns G, et al: Platelet
activating factor receptor regulates Colitis-induced pulmonary
inflammation through the NLRP3 inflammasome. Mucosal Immunol.
12:862–873. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Fricker M, Goggins BJ, Mateer S, Jones B,
Kim RY, Gellatly SL, Jarnicki AG, Powell N, Oliver BG,
Radford-Smith G, et al: Chronic cigarette smoke exposure induces
systemic hypoxia that drives intestinal dysfunction. JCI Insight.
3:e940402018. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Mateer SW, Maltby S, Marks E, Foster PS,
Horvat JC, Hansbro PM and Keely S: Potential mechanisms regulating
pulmonary pathology in inflammatory bowel disease. J Leukoc Biol.
98:727–737. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Mateer SW, Mathe A, Bruce J, Liu G, Maltby
S, Fricker M, Goggins BJ, Tay HL, Marks E, Burns G, et al: IL-6
drives Neutrophil-mediated pulmonary inflammation associated with
bacteremia in murine models of colitis. Am J Pathol. 188:1625–1639.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Anand S and Mande SS: Diet, microbiota and
gut-lung connection. Front Microbiol. 9:21472018. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Marsland BJ, Trompette A and Gollwitzer
ES: The Gut-lung axis in respiratory disease. Ann Am Thorac Soc. 12
(Suppl 2):S150–S56. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Dang AT and Marsland BJ: Microbes,
metabolites, and the gut-lung axis. Mucosal Immunol. 12:843–850.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Al Alam D, Danopoulos S, Grubbs B, Ali N,
MacAogain M, Chotirmall SH, Warburton D, Gaggar A, Ambalavanan N
and Lal CV: human fetal lungs harbor a microbiome signature. Am J
Respir Crit Care Med. 201:1002–1006. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Chakradhar S: A curious connection:
Teasing apart the link between gut microbes and lung disease. Nat
Med. 23:402–404. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Aagaard K, Ma J, Antony KM, Ganu R,
Petrosino J and Versalovic J: The placenta harbors a unique
microbiome. Sci Transl Med. 6:237–265. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Collado MC, Rautava S, Aakko J, Isolauri E
and Salminen S: Human gut colonisation may be initiated in utero by
distinct microbial communities in the placenta and amniotic fluid.
Sci Rep. 6:231292016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Ortiz Moyano R, Raya Tonetti F, Tomokiyo
M, Kanmani P, Vizoso-Pinto MG, Kim H, Quilodrán-Vega S, Melnikov V,
Alvarez S, Takahashi H, et al: The ability of respiratory commensal
bacteria to beneficially modulate the lung innate immune response
is a strain dependent characteristic. Microorganisms. 8:7272020.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Leiby JS, McCormick K, Sherrill-Mix S,
Clarke EL, Kessler LR, Taylor LJ, Hofstaedter CE, Roche AM, Mattei
LM, Bittinger K, et al: Lack of detection of a human placenta
microbiome in samples from preterm and term deliveries. Microbiome.
6:1962018. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
de Goffau MC, Lager S, Sovio U, Gaccioli
F, Cook E, Peacock SJ, Parkhill J, Charnock-Jones DS and Smith GCS:
Human placenta has no microbiome but can contain potential
pathogens. Nature. 572:329–334. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Tauchi H, Yahagi K, Yamauchi T, Hara T,
Yamaoka R, Tsukuda N, Watanabe Y, Tajima S, Ochi F, Iwata H, et al:
Gut microbiota development of preterm infants hospitalised in
intensive care units. Benef Microbes. 10:641–651. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Guittar J, Shade A and Litchman E:
Trait-based community assembly and succession of the infant gut
microbiome. Nat Commun. 10:5122019. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
La Rosa PS, Warner BB, Zhou Y, Weinstock
GM, Sodergren E, Hall-Moore CM, Stevens HJ, Bennett WE Jr, Shaikh
N, Linneman LA, et al: Patterned progression of bacterial
populations in the premature infant gut. Proc Natl Acad Sci USA.
111:12522–12527. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Korpela K, Blakstad EW, Moltu SJ, Strømmen
K, Nakstad B, Rønnestad AE, Brække K, Iversen PO, Drevon CA and de
Vos W: Intestinal microbiota development and gestational age in
preterm neonates. Sci Rep. 8:24532018. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Bresesti I, Salvatore S, Valetti G, Baj A,
Giaroni C and Agosti M: The Microbiota-gut axis in premature
infants: Physio-pathological implications. Cells. 11:3792022.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Stewart CJ, Ajami NJ, O'Brien JL,
Hutchinson DS, Smith DP, Wong MC, Ross MC, Lloyd RE, Doddapaneni H,
Metcalf GA, et al: Temporal development of the gut microbiome in
early childhood from the TEDDY study. Nature. 562:583–588. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Bäckhed F, Roswall J, Peng Y, Feng Q, Jia
H, Kovatcheva-Datchary P, Li Y, Xia Y, Xie H, Zhong H, et al:
Dynamics and stabilization of the human gut microbiome during the
first year of life. Cell Host Microbe. 17:690–703. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Lyons KE, Ryan CA, Dempsey EM, Ross RP and
Stanton C: Breast milk, a source of beneficial microbes and
associated benefits for infant health. Nutrients. 12:10392020.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Quigley M, Embleton ND and McGuire W:
Formula versus donor breast milk for feeding preterm or low birth
weight infants. Cochrane Database Syst Rev.
6:CD0029712018.PubMed/NCBI
|
|
48
|
Aguilar-Lopez M, Dinsmoor AM, Ho TTB and
Donovan SM: A systematic review of the factors influencing
microbial colonization of the preterm infant gut. Gut Microbes.
13:1–33. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Ramirez J, Guarner F, Bustos Fernandez L,
Maruy A, Sdepanian VL and Cohen H: Antibiotics as major disruptors
of gut microbiota. Front Cell Infect Microbiol. 10:5729122020.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Kalbermatter C, Fernandez Trigo N,
Christensen S and Ganal-Vonarburg SC: Maternal microbiota, early
life colonization and breast milk drive immune development in the
newborn. Front Immunol. 12:6830222021. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Colombo SFG, Nava C, Castoldi F, Fabiano
V, Meneghin F, Lista G and Cavigioli F: Preterm Infants' Airway
microbiome: A scoping review of the current evidence. Nutrients.
16:4652024. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Lohmann P, Luna RA, Hollister EB, Devaraj
S, Mistretta TA, Welty SE and Versalovic J: The airway microbiome
of intubated premature infants: Characteristics and changes that
predict the development of bronchopulmonary dysplasia. Pediatr Res.
76:294–301. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Pammi M, Lal CV, Wagner BD, Mourani PM,
Lohmann P, Luna RA, Sisson A, Shivanna B, Hollister EB, Abman SH,
et al: Airway microbiome and development of bronchopulmonary
dysplasia in preterm infants: A systematic review. J Pediatr.
204:126–133.e2. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Sun T, Yu H and Fu J: Respiratory tract
microecology and bronchopulmonary dysplasia in preterm infants.
Front Pediatr. 9:7625452021. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Chen X, Huang X, Lin Y, Lin B and Yang C,
Huang Z and Yang C: Association of Ureaplasma infection pattern and
azithromycin treatment effect with bronchopulmonary dysplasia in
Ureaplasma positive infants: A cohort study. BMC Pulm Med.
23:2292023. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Chung KF and Adcock IM: Multifaceted
mechanisms in COPD: Inflammation, immunity, and tissue repair and
destruction. Eur Respir J. 31:1334–1356. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Song Z, Meng Y, Fricker M, Li X, Tian H,
Tan Y and Qin L: The role of gut-lung axis in COPD: Pathogenesis,
immune response, and prospective treatment. Heliyon. 10:e306122024.
View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Zhang Z, Jiang J, Li Z and Wan W: The
change of cytokines and gut microbiome in preterm infants for
bronchopulmonary dysplasia. Front Microbiol. 13:8048872022.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Lal CV, Kandasamy J, Dolma K, Ramani M,
Kumar R, Wilson L, Aghai Z, Barnes S, Blalock JE, Gaggar A, et al:
Early airway microbial metagenomic and metabolomic signatures are
associated with development of severe bronchopulmonary dysplasia.
Am J Physiol Lung Cell Mol Physiol. 315:L810–L815. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Yang K and Dong W: Perspectives on
probiotics and bronchopulmonary dysplasia. Front Pediatr.
8:5702472020. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Willis KA, Siefker DT, Aziz MM, White CT,
Mussarat N, Gomes CK, Bajwa A, Pierre JF, Cormier SA and Talati AJ:
Perinatal maternal antibiotic exposure augments lung injury in
offspring in experimental bronchopulmonary dysplasia. Am J Physiol
Lung Cell Mol Physiol. 318:L407–L418. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Enaud R, Prevel R, Ciarlo E, Beaufils F,
Wieërs G, Guery B and Delhaes L: The Gut-lung axis in health and
respiratory diseases: A place for inter-organ and inter-kingdom
crosstalks. Front Cell Infect Microbiol. 10:92020. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Wedgwood S, Gerard K, Halloran K,
Hanhauser A, Monacelli S, Warford C, Thai PN, Chiamvimonvat N,
Lakshminrusimha S, Steinhorn RH and Underwood MA: Intestinal
dysbiosis and the developing lung: The role of toll-like receptor 4
in the gut-lung axis. Front Immunol. 11:3572020. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Li Y, He L, Zhao Q and Bo T: Microbial and
metabolic profiles of bronchopulmonary dysplasia and therapeutic
effects of potential probiotics Limosilactobacillus reuteri and
Bifidobacterium bifidum. J Appl Microbiol. 133:908–921. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Shen X, Yang Z, Wang Q, Chen X, Zhu Q, Liu
Z, Patel N, Liu X and Mo X: Lactobacillus plantarum L168 improves
hyperoxia-induced pulmonary inflammation and hypoalveolarization in
a rat model of bronchopulmonary dysplasia. NPJ Biofilms
Microbiomes. 10:442024. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Underwood MA, Lakshminrusimha S, Steinhorn
RH and Wedgwood S: Malnutrition, poor post-natal growth, intestinal
dysbiosis and the developing lung. J Perinatol. 41:1797–1810. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Ding J, Xu J, Wu H, Li M, Xiao Y, Fu J,
Zhu X, Wu N, Sun Q and Liu Y: The cross-talk between the metabolome
and microbiome in a double-hit neonatal rat model of
bronchopulmonary dysplasia. Genomics. 117:1109692025. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Thatrimontrichai A, Praditaukrit M,
Maneenil G, Dissaneevate S, Singkhamanan K and Surachat K:
Characterization of gut microbiota in very low birth weight infants
with versus without bronchopulmonary dysplasia. Clin Exp Pediatr.
68:503–511. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Sodhi CP, Gonzalez Salazar AJ, Kovler ML,
Fulton WB, Yamaguchi Y, Ishiyama A, Wang S, Prindle T Jr, Vurma M,
Das T, et al: The administration of a pre-digested fat-enriched
formula prevents necrotising enterocolitis-induced lung injury in
mice. Br J Nutr. 128:1050–1063. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Jia H, Sodhi CP, Yamaguchi Y, Lu P, Martin
LY, Good M, Zhou Q, Sung J, Fulton WB, Nino DF, et al: Pulmonary
epithelial TLR4 activation leads to lung injury in neonatal
necrotizing enterocolitis. J Immunol. 197:859–871. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Tan JY, Tang YC and Huang J: Gut
microbiota and lung injury. Adv Exp Med Biol. 1238:55–72. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Samuelson DR, Welsh DA and Shellito JE:
Regulation of lung immunity and host defense by the intestinal
microbiota. Front Microbiol. 6:10852015. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Dickson RP, Singer BH, Newstead MW,
Falkowski NR, Erb-Downward JR, Standiford TJ and Huffnagle GB:
Enrichment of the lung microbiome with gut bacteria in sepsis and
the acute respiratory distress syndrome. Nat Microbiol.
1:161132016. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Moreno-Villares JM, Andrade-Platas D,
Soria-López M, Colomé-Rivero G, Catalan Lamban A, Martinez-Figueroa
MG, Espadaler-Mazo J and Valverde-Molina J: Comparative efficacy of
probiotic mixture Bifidobacterium longum KABP042 plus Pediococcus
pentosaceus KABP041 vs. Limosilactobacillus reuteri DSM17938 in the
management of infant colic: A randomized clinical trial. Eur J
Pediatr. 183:5371–5381. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Spreckels JE, Wejryd E, Marchini G,
Jonsson B, de Vries DH, Jenmalm MC, Landberg E, Sverremark-Ekström
E, Martí M and Abrahamsson T: Lactobacillus reuteri
Colonisation of extremely preterm infants in a randomised
Placebo-controlled trial. Microorganisms. 9:9152021. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Zhang Q, Ran X, He Y, Ai Q and Shi Y:
Acetate downregulates the activation of NLRP3 inflammasomes and
attenuates lung injury in neonatal mice with bronchopulmonary
dysplasia. Front Pediat. 8:5951572021. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Fanos V, Pintus MC, Lussu M, Atzori L,
Noto A, Stronati M, Guimaraes H, Marcialis MA, Rocha G, Moretti C,
et al: Urinary metabolomics of bronchopulmonary dysplasia (BPD):
Preliminary data at birth suggest it is a congenital disease. J
Matern Fetal Neonatal Med. 27 (Suppl 2):S39–S45. 2014. View Article : Google Scholar
|
|
78
|
Pintus MC, Lussu M, Dessì A, Pintus R,
Noto A, Masile V, Marcialis MA, Puddu M, Fanos V and Atzori L:
Urinary 1H-NMR metabolomics in the first week of life
can anticipate BPD diagnosis. Oxid Med Cell Longev.
2018:76206712018. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Piersigilli F and Bhandari V: Metabolomics
of bronchopulmonary dysplasia. Clin Chim Acta. 500:109–114. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Zhao Q, Li Y, Chai X, Xu L, Zhang L, Ning
P, Huang J and Tian S: Interaction of inhalable volatile organic
compounds and pulmonary surfactant: Potential hazards of VOCs
exposure to lung. J Hazard Mater. 369:512–520. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Berkhout DJC, Niemarkt HJ, Benninga MA,
Budding AE, van Kaam AH, Kramer BW, Pantophlet CM, van Weissenbruch
MM, de Boer NKH and de Meij TGJ: Development of severe
bronchopulmonary dysplasia is associated with alterations in fecal
volatile organic compounds. Pediatr Res. 83:412–419. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Wright H, Bannaga AS, Iriarte R, Mahmoud M
and Arasaradnam RP: Utility of volatile organic compounds as a
diagnostic tool in preterm infants. Pediatr Res. 89:263–268. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Furusawa Y, Obata Y, Fukuda S, Endo TA,
Nakato G, Takahashi D, Nakanishi Y, Uetake C, Kato K and Kato T:
Commensal microbe-derived butyrate induces the differentiation of
colonic regulatory T cells. Nature. 504:446–450. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Torow N, Hand TW and Hornef MW: Programmed
and environmental determinants driving neonatal mucosal immune
development. Immunity. 56:485–499. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Jugder BE, Kamareddine L and Watnick PI:
Microbiota-derived acetate activates intestinal innate immunity via
the Tip60 histone acetyltransferase complex. Immunity.
54:1683–1697. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Woo V and Alenghat T: Epigenetic
regulation by gut microbiota. Gut Microbes. 14:20224072022.
View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Weiss GA and Hennet T: Mechanisms and
consequences of intestinal dysbiosis. Cell Mol Life Sci.
74:2959–2977. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
McDermott AJ and Huffnagle GB: The
microbiome and regulation of mucosal immunity. Immunology.
142:24–31. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Cai J, Lu H, Su Z, Mi L, Xu S and Xue Z:
Dynamic Changes of NCR-type 3 innate lymphoid cells and their role
in mice with bronchopulmonary dysplasia. Inflammation. 45:497–508.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Li B, Yin GF, Wang YL, Tan YM, Huang CL
and Fan XM: Impact of fecal microbiota transplantation on
TGF-β1/Smads/ERK signaling pathway of endotoxic acute lung injury
in rats. 3 Biotech. 10:522020. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Tirone C, Pezza L, Paladini A, Tana M,
Aurilia C, Lio A, D'Ippolito S, Tersigni C, Posteraro B,
Sanguinetti M, et al: Gut and lung microbiota in preterm infants:
Immunological modulation and implication in neonatal outcomes.
Front Immunol. 10:29102019. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Yao HC, Zhu Y, Lu HY, Ju HM, Xu SQ, Qiao Y
and Wei SJ: Type 2 innate lymphoid cell-derived amphiregulin
regulates type II alveolar epithelial cell transdifferentiation in
a mouse model of bronchopulmonary dysplasia. Int Immunopharmacol.
122:1106722023. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Gray J, Oehrle K, Worthen G, Alenghat T,
Whitsett J and Deshmukh H: Intestinal commensal bacteria mediate
lung mucosal immunity and promote resistance of newborn mice to
infection. Sci Transl Med. 9:eaaf94122017. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Zhu Y, Mi L, Lu H, Ju H, Hao X and Xu S:
ILC2 regulates hyperoxia-induced lung injury via an enhanced Th17
cell response in the BPD mouse model. BMC Pulm Med. 23:1882023.
View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Willis KA and Ambalavanan N: Necrotizing
enterocolitis and the Gut-lung axis. Semin Perinatol.
45:1514542021. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Ngo VL, Lieber CM, Kang HJ, Sakamoto K,
Kuczma M, Plemper RK and Gewirtz AT: Intestinal microbiota
programming of alveolar macrophages influences severity of
respiratory viral infection. Cell Host Microbe. 32:335–348. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Qu Y, Guo S, Liu Y, Wang G and Wu H:
Association between probiotics and bronchopulmonary dysplasia in
preterm infants. Sci Rep. 11:170602021. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Villamor-Martínez E, Pierro M, Cavallaro
G, Mosca F, Kramer B and Villamor E: Probiotic supplementation in
preterm infants does not affect the risk of bronchopulmonary
dysplasia: A Meta-analysis of randomized controlled trials.
Nutrients. 9:11972017. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Yoo S, Jung SC, Kwak K and Kim JS: The
role of prebiotics in modulating gut microbiota: Implications for
human health. Int J Mol Sci. 25:48342024. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Antunes KH, Singanayagam A, Williams L,
Faiez TS, Farias A, Jackson MM, Faizi FK, Aniscenko J, Kebadze T,
Chander Veerati P, et al: Airway-delivered short-chain fatty acid
acetate boosts antiviral immunity during rhinovirus infection. J
Allergy Clin Immunol. 151:447–457. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Ito T, Nakanishi Y, Shibata R, Sato N,
Jinnohara T, Suzuki S, Suda W, Hattori M, Kimura I, Nakano T, et
al: The propionate-GPR41 axis in infancy protects from subsequent
bronchial asthma onset. Gut Microbes. 15:22065072023. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Lee SH, Lee JH and Lee SW: Application of
Microbiome-based therapies in chronic respiratory diseases. J
Microbiol. 62:201–216. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Menegolla MP, Silveira RC, Görgen ARH,
Gandolfi FE and Procianoy RS: Antibiotics and beyond: Unraveling
the dynamics of bronchopulmonary dysplasia in very preterm infants.
Pediatr Pulmonol. 59:3260–3267. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Martin I, Silverberg M, Abdelgawad A,
Tanaka K, Halloran BA, Nicola T, Myers ED, Desai JP, White CT,
Karabayir I, et al: The fungal microbiota modulate neonatal
oxygen-induced lung injury. Microbiome. 13:242025. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Dorshkind K and Crooks G: Layered immune
system development in mice and humans. Immunol Rev. 315:5–10. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Loering S, Cameron GJM, Starkey MR and
Hansbro PM: Lung development and emerging roles for type 2
immunity. J Pathol. 247:686–696. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Moeller AH and Sanders JG: Roles of the
gut microbiota in the adaptive evolution of mammalian species.
Philos Trans R Soc Lond B Biol Sci. 75:201905972020. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Sprockett DD, Price JD, Juritsch AF,
Schmaltz RJ, Real MVF, Goldman SL, Sheehan M, Ramer-Tait AE and
Moeller AH: Home-site advantage for host species-specific gut
microbiota. Sci Adv. 9:54992023. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Gao Y, Wang K, Lin Z, Cai S, Peng A, He L,
Qi H, Jin Z and Qian X: The emerging roles of microbiome and
short-chain fatty acids in the pathogenesis of bronchopulmonary
dysplasia. Front Cell Infect Microbiol. 14:14346872024. View Article : Google Scholar : PubMed/NCBI
|