|
1
|
Finnerup NB, Kuner R and Jensen TS:
Neuropathic Pain: From mechanisms to treatment. Physiol Rev.
101:259–301. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Burke D, Fullen BM, Stokes D and Lennon O:
Neuropathic pain prevalence following spinal cord injury: A
systematic review and meta-analysis. Eur J Pain. 21:29–44. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hergenroeder GW, Redell JB, Choi HA,
Schmitt L, Donovan W, Francisco GE, Schmitt K, Moore AN and Dash
PK: Increased levels of circulating glial fibrillary acidic protein
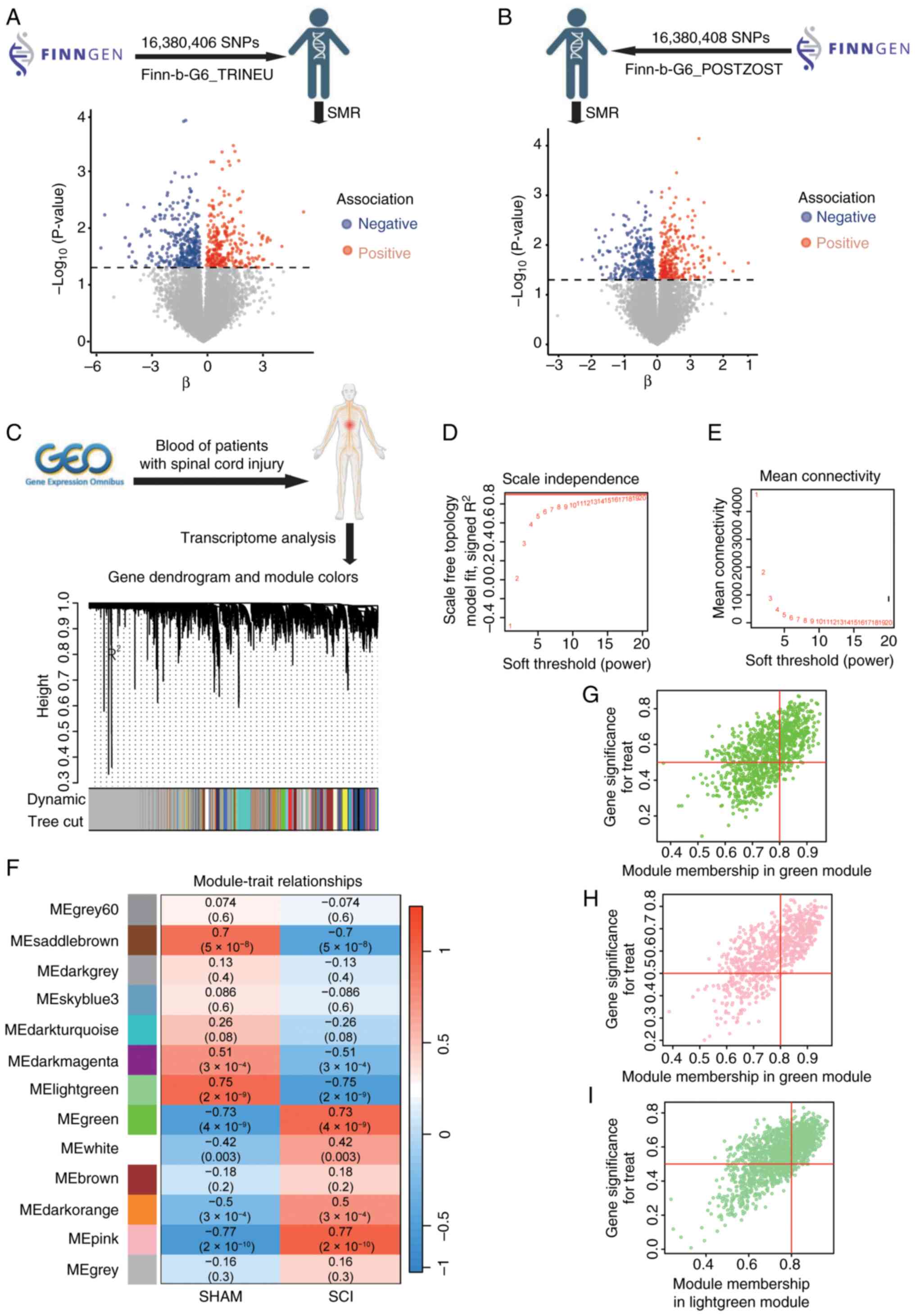
and collapsin response mediator Protein-2 autoantibodies in the
acute stage of spinal cord injury predict the subsequent
development of neuropathic pain. J Neurotraum. 35:2530–2539. 2018.
View Article : Google Scholar
|
|
4
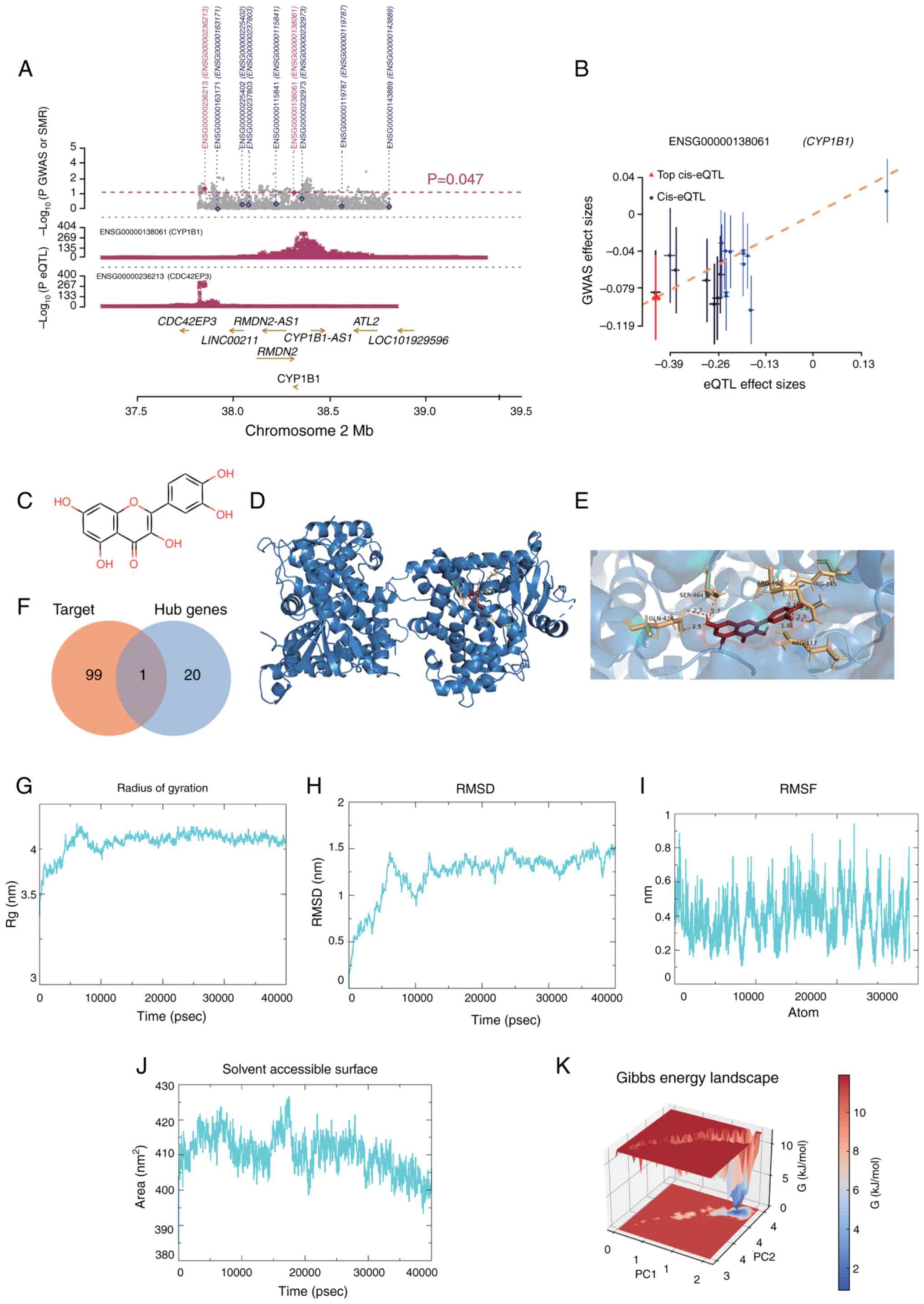
|
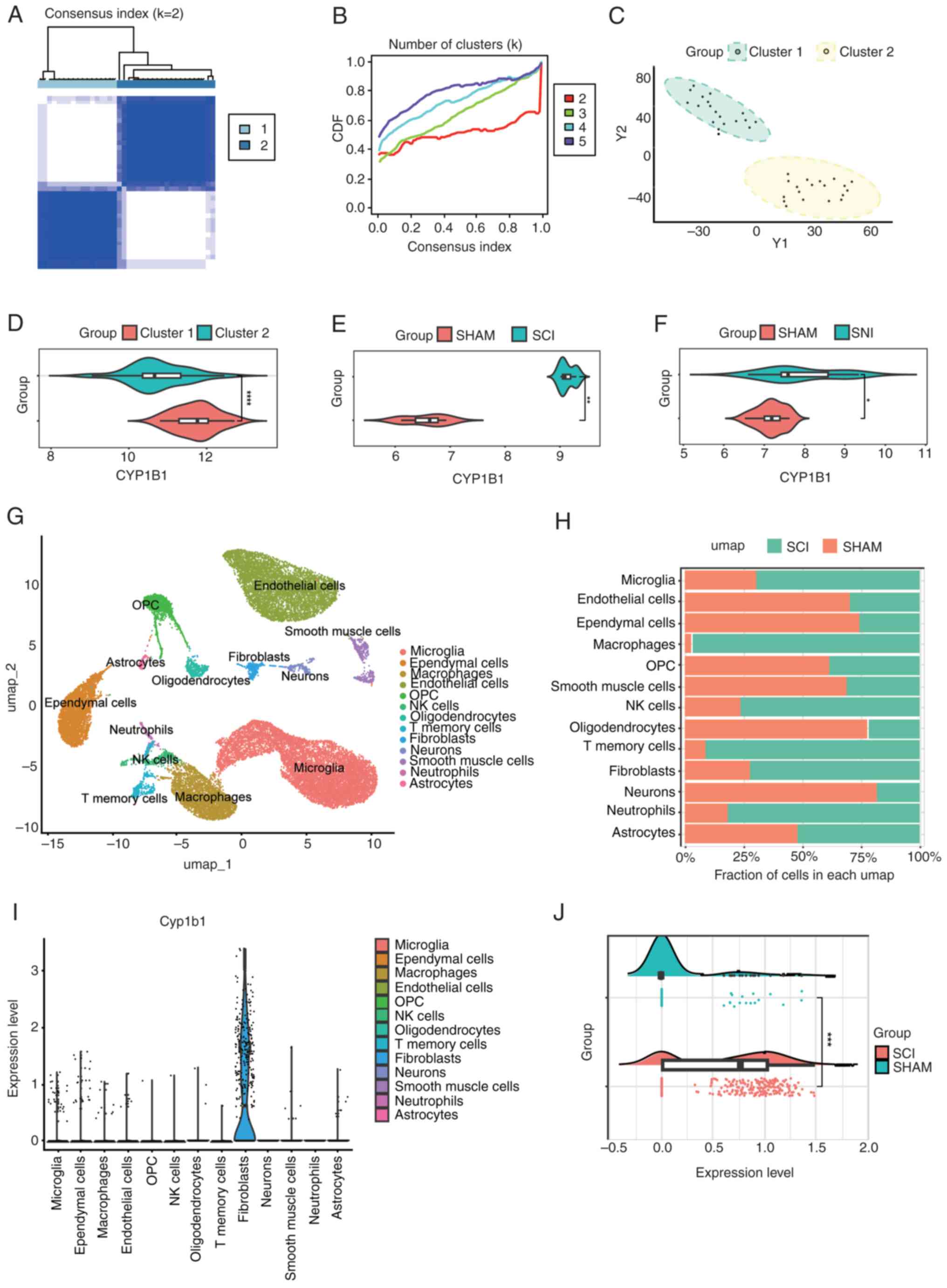
Widerström-Noga E: Neuropathic pain and
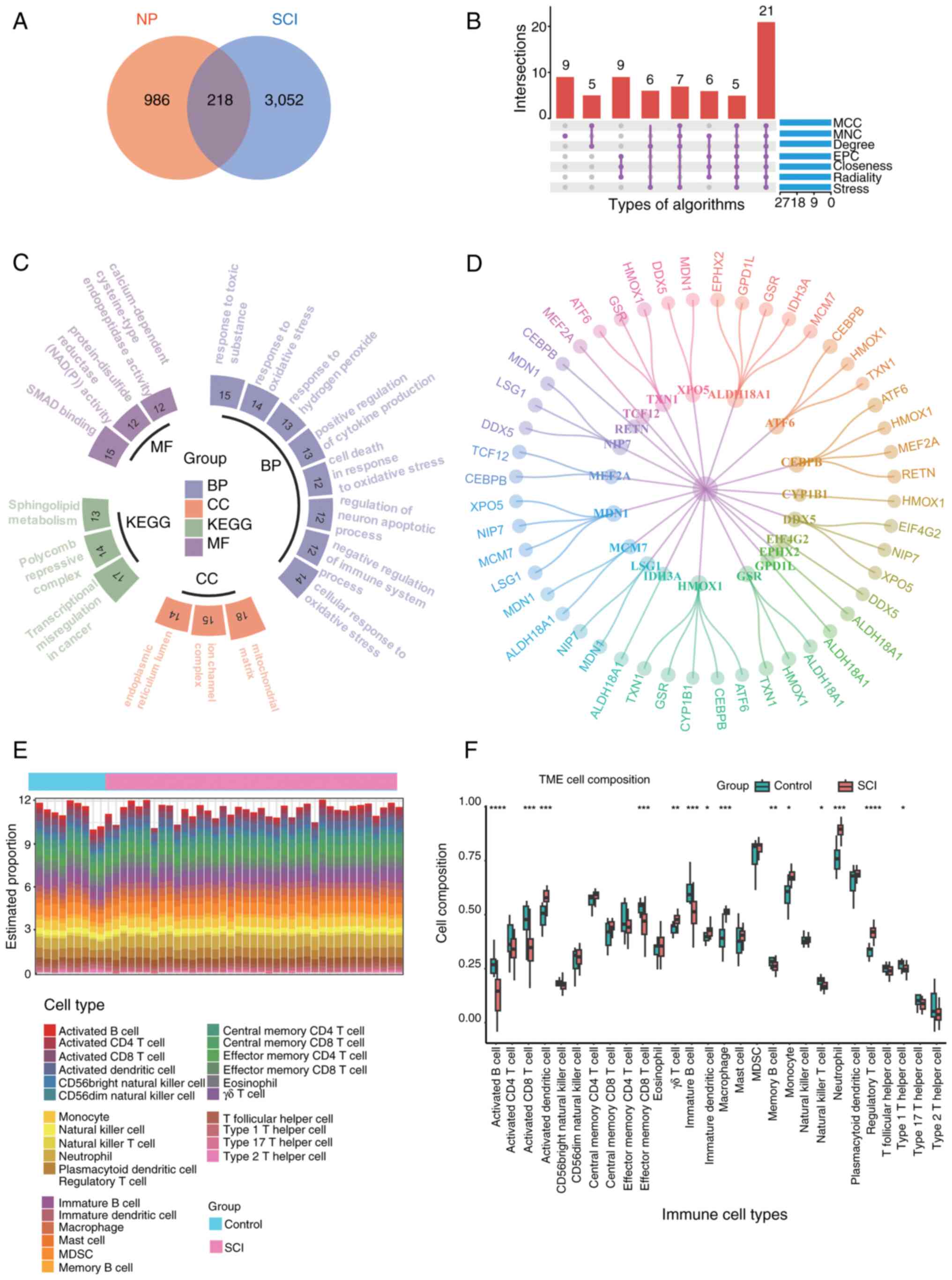
spinal cord injury: Phenotypes and pharmacological management.
Drugs. 77:967–984. 2017. View Article : Google Scholar
|
|
5
|
Orr MB and Gensel JC: Spinal cord injury
scarring and inflammation: Therapies targeting glial and
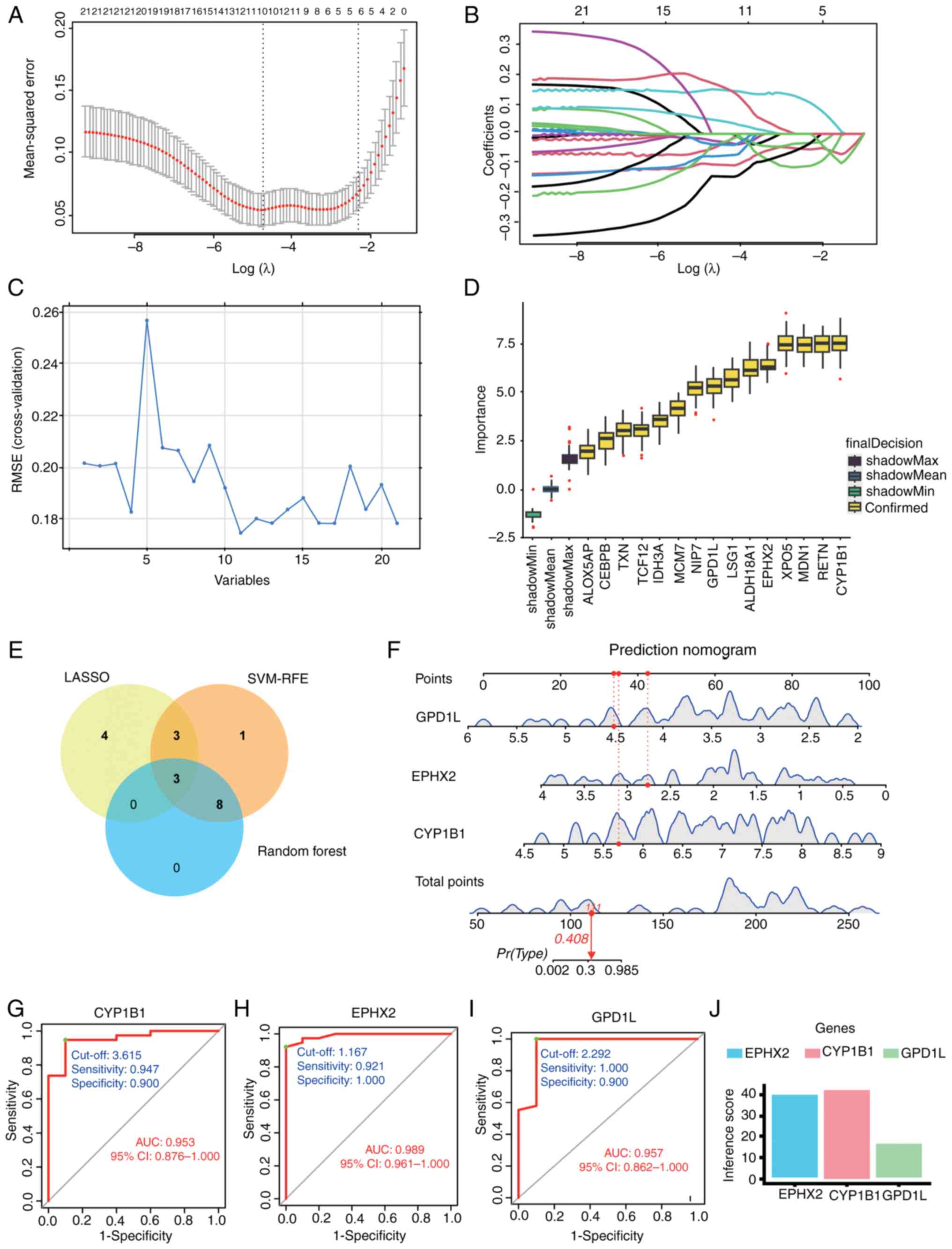
inflammatory responses. Neurotherapeutics. 15:541–553. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
O'Shea TM, Burda JE and Sofroniew MV: Cell
biology of spinal cord injury and repair. J Clin Invest.
127:3259–3270. 2017. View Article : Google Scholar
|
|
7
|
Boldt I, Eriks-Hoogland I, Brinkhof MW, de
Bie R, Joggi D and von Elm E: Non-pharmacological interventions for
chronic pain in people with spinal cord injury. Cochrane Database
Syst Rev. 2014:CD0091772014. View Article : Google Scholar : PubMed/NCBI
|
|
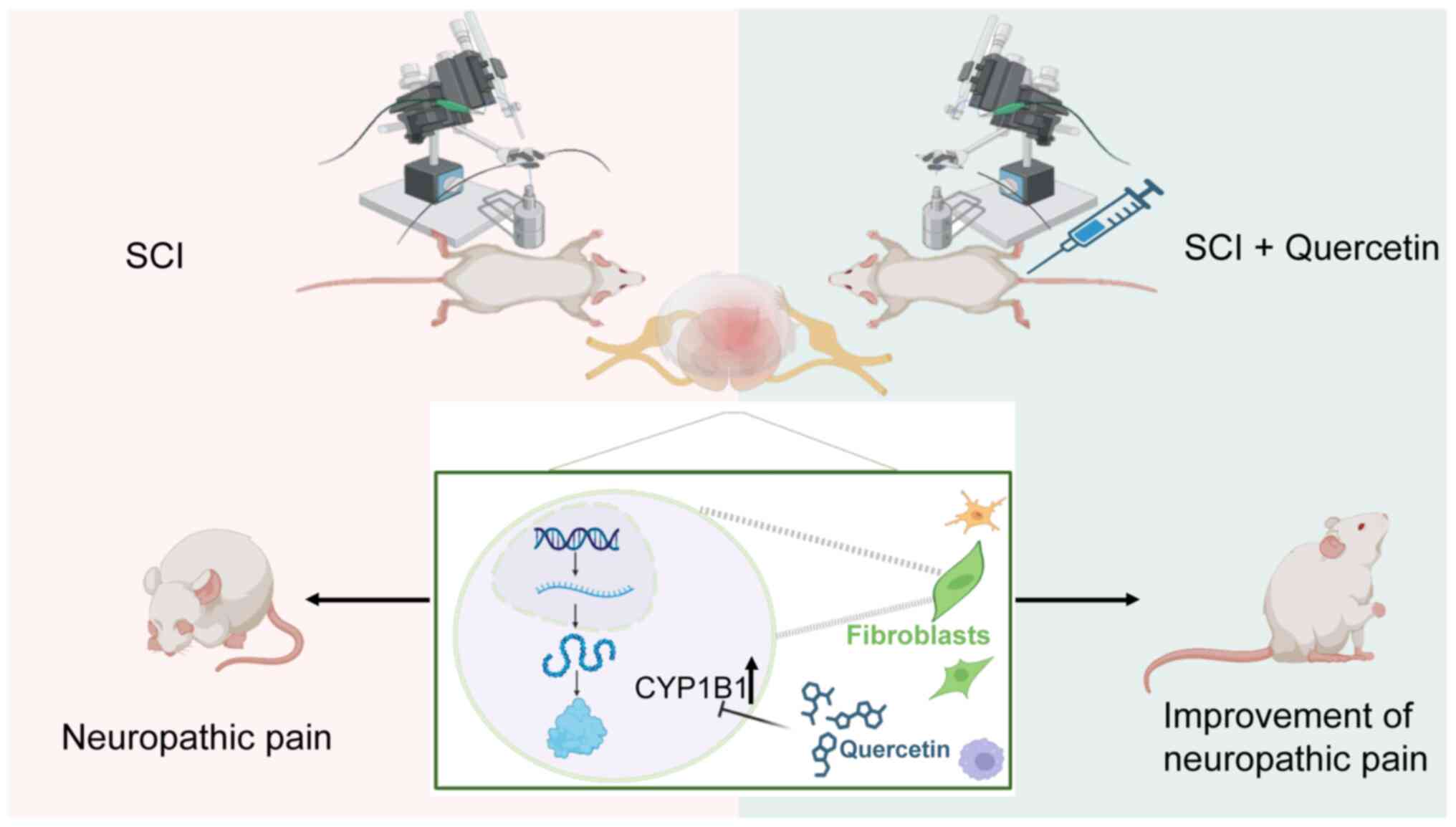
8
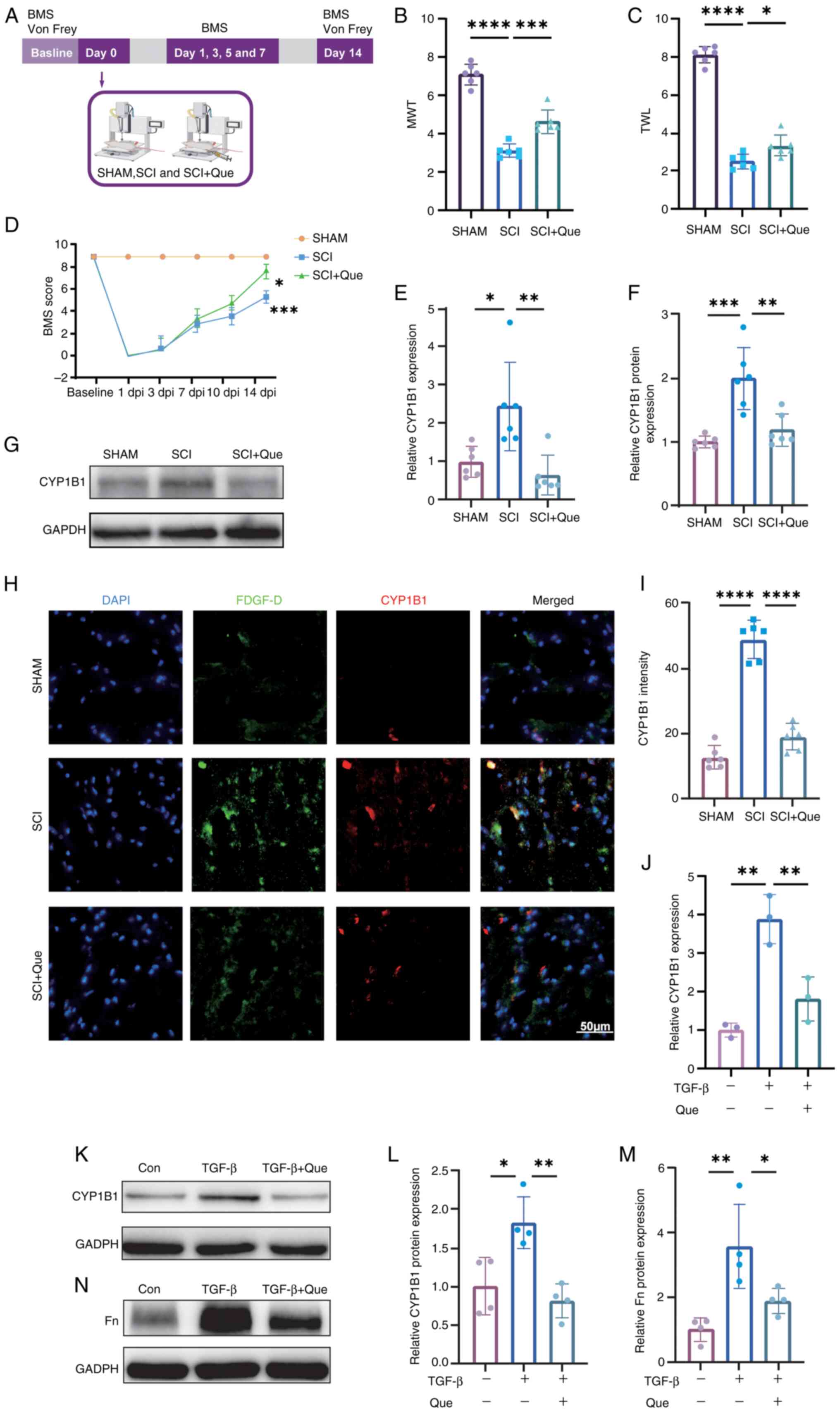
|
Mehta S, McIntyre A, Janzen S, Loh E and
Teasell R; Spinal Cord Injury Rehabilitation Evidence Team, :
Systematic review of pharmacologic treatments of pain after spinal
cord injury: An update. Arch Phys Med Rehabil. 97:1381–1391.e1.
2016. View Article : Google Scholar
|
|
9
|
Loh E, Mirkowski M, Agudelo AR, Allison
DJ, Benton B, Bryce TN, Guilcher S, Jeji T, Kras-Dupuis A,
Kreutzwiser D, et al: The CanPain SCI clinical practice guidelines
for rehabilitation management of neuropathic pain after spinal cord
injury: 2021 update. Spinal Cord. 60:548–566. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Liu C, Liu DQ, Tian YK, Mei W, Tian XB, Xu
AJ and Zhou YQ: The emerging role of quercetin in the treatment of
chronic pain. Curr Neuropharmacol. 20:2346–2353. 2022. View Article : Google Scholar
|
|
11
|
Yang H, Yang T, Heng C, Zhou Y, Jiang Z,
Qian X, Du L, Mao S, Yin X and Lu Q: Quercetin improves
nonalcoholic fatty liver by ameliorating inflammation, oxidative
stress, and lipid metabolism in db/db mice. Phytother Res.
33:3140–3152. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gao W, Zan Y, Wang ZJ, Hu XY and Huang F:
Quercetin ameliorates paclitaxel-induced neuropathic pain by
stabilizing mast cells, and subsequently blocking PKCε-dependent
activation of TRPV1. Acta Pharmacol Sin. 37:1166–1177. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang R, Qiu Z, Wang G, Hu Q, Shi N, Zhang
Z, Wu Y and Zhou C: Quercetin attenuates diabetic neuropathic pain
by inhibiting mTOR/p70S6K pathway-mediated changes of synaptic
morphology and synaptic protein levels in spinal dorsal horn of
db/db mice. Eur J Pharmacol. 882:1732662020. View Article : Google Scholar
|
|
14
|
Abbey EL and Rankin JW: Effect of
quercetin supplementation on repeated-sprint performance, xanthine
oxidase activity, and inflammation. Int J Sport Nutr Exerc Metab.
21:91–96. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhao L, Wang H and Du X: The therapeutic
use of quercetin in ophthalmology: Recent applications. Biomed
Pharmacother. 137:1113712021. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Li Y, Yao J, Han C, Yang J, Chaudhry MT,
Wang S, Liu H and Yin Y: Quercetin, inflammation and immunity.
Nutrients. 8:1672016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Costa LG, Garrick JM, Roquè PJ and
Pellacani C: Mechanisms of neuroprotection by Quercetin:
Counteracting oxidative stress and more. Oxid Med Cell Longev.
2016:29867962016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Shao Z, Wang B, Shi Y, Xie C, Huang C,
Chen B, Zhang H, Zeng G, Liang H, Wu Y, et al: Senolytic agent
Quercetin ameliorates intervertebral disc degeneration via the
Nrf2/NF-κB axis. Osteoarthritis Cartilage. 29:413–422. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chiang MC, Tsai TY and Wang CJ: The
potential benefits of quercetin for brain health: A review of
Anti-inflammatory and neuroprotective mechanisms. Int J Mol Sci.
24:63282023. View Article : Google Scholar
|
|
20
|
Grewal AK, Singh TG, Sharma D, Sharma V,
Singh M, Rahman MH, Najda A, Walasek-Janusz M, Kamel M, Albadrani
GM, et al: Mechanistic insights and perspectives involved in
neuroprotective action of quercetin. Biomed Pharmacother.
140:1117292021. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Elsworth B, Lyon B, Alexander T, Liu Y,
Matthews P, Hallett J, Bates P, Palmer T, Haberland V, Smith GD, et
al: The MRC IEU OpenGWAS data infrastructure. bioRxiv. August
10–2020.doi: 10.1101/2020.08.10.244293. View Article : Google Scholar
|
|
22
|
Kurki MI, Karjalainen J, Palta P, Sipilä
TP, Kristiansson K, Donner KM, Reeve MP, Laivuori H, Aavikko M,
Kaunisto MA, et al: FinnGen provides genetic insights from a
well-phenotyped isolated population. Nature. 613:508–518. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Võsa U, Claringbould A, Westra HJ, Bonder
MJ, Deelen P, Zeng B, Kirsten H, Saha A, Kreuzhuber R, Yazar S, et
al: Large-scale cis- and trans-eQTL analyses identify thousands of
genetic loci and polygenic scores that regulate blood gene
expression. Nat Genet. 53:1300–1310. 2021.
|
|
24
|
Kyritsis N, Torres-Espín A, Schupp PG,
Huie JR, Chou A, Duong-Fernandez X, Thomas LH, Tsolinas RE,
Hemmerle DD, Pascual LU, et al: Diagnostic blood RNA profiles for
human acute spinal cord injury. J Exp Med. 218:e202017952021.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Milich LM, Choi JS, Ryan C, Cerqueira SR,
Benavides S, Yahn SL, Tsoulfas P and Lee JK: Single-cell analysis
of the cellular heterogeneity and interactions in the injured mouse
spinal cord. J Exp Med. 218:e202100402021. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Patel M, Li Y, Anderson J, Castro-Pedrido
S, Skinner R, Lei S, Finkel Z, Rodriguez B, Esteban F, Lee KB, et
al: Gsx1 promotes locomotor functional recovery after spinal cord
injury. Mol Ther. 29:2469–2482. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ghazisaeidi S, Muley MM, Tu Y, Finn DP,
Kolahdouzan M, Pitcher GM, Kim D, Sengar AS, Ramani AK, Brudno M
and Salter MW: Conserved transcriptional programming across sex and
species after peripheral nerve injury predicts treatments for
neuropathic pain. Br J Pharmacol. 180:2822–2836. 2023. View Article : Google Scholar
|
|
28
|
Zhu Z, Zhang F, Hu H, Bakshi A, Robinson
MR, Powell JE, Montgomery GW, Goddard ME, Wray NR, Visscher PM and
Yang J: Integration of summary data from GWAS and eQTL studies
predicts complex trait gene targets. Nat Genet May. 48:481–487.
2016. View Article : Google Scholar
|
|
29
|
Langfelder P and Horvath S: WGCNA: An R
package for weighted correlation network analysis. BMC
Bioinformatics. 9:5592008. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Bardou P, Mariette J, Escudié F, Djemiel C
and Klopp C: Jvenn: An interactive Venn diagram viewer. BMC
Bioinformatics. 15:2932014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
The Gene Ontology Consortium, . The Gene
Ontology Resource: 20 years and still GOing strong. Nucleic Acids
Res. 47:D330–D338. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Ogata H, Goto S, Sato K, Fujibuchi W, Bono
H and Kanehisa M: KEGG: Kyoto encyclopedia of genes and genomes.
Nucleic Acids Res. 27:29–34. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Li J, Miao B, Wang S, Dong W, Xu H, Si C,
Wang W, Duan S, Lou J, Bao Z, et al: Hiplot: A comprehensive and
easy-to-use web service for boosting publication-ready biomedical
data visualization. Brief Bioinform. 23:bbac2612022. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Szklarczyk D, Gable AL, Nastou KC, Lyon D,
Kirsch R, Pyysalo S, Doncheva NT, Legeay M, Fang T, Bork P, et al:
The STRING database in 2021: Customizable protein-protein Networks,
and functional characterization of user-uploaded gene/measurement
sets. Nucleic Acids Res. 49:D605–D601. 20212. View Article : Google Scholar
|
|
35
|
Shannon P, Markiel A, Ozier O, Baliga NS,
Wang JT, Ramage D, Amin N, Schwikowski B and Ideker T: Cytoscape: A
software environment for integrated models of biomolecular
interaction networks. Genome Res. 13:2498–2504. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Bindea G, Mlecnik B, Tosolini M,
Kirilovsky A, Waldner M, Obenauf AC, Angell H, Fredriksen T,
Lafontaine L, Berger A, et al: Spatiotemporal dynamics of
intratumoral immune cells reveal the immune landscape in human
cancer. Immunity. 39:782–795. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Barbie DA, Tamayo P, Boehm JS, Kim SY,
Moody SE, Dunn IF, Schinzel AC, Sandy P, Meylan E, Scholl C, et al:
Systematic RNA interference reveals that oncogenic KRAS-driven
cancers require TBK1. Nature. 462:108–112. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Yang C, Delcher C, Shenkman E and Ranka S:
Machine learning approaches for predicting high cost high need
patient expenditures in health care. Biomed Eng Online. 17 (Suppl
1):S1312018. View Article : Google Scholar
|
|
39
|
Sahran S, Albashish D, Abdullah A, Shukor
NA, Hayati Md and Pauzi S: Absolute cosine-based SVM-RFE feature
selection method for prostate histopathological grading. Artif
Intell Med. 87:78–90. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Degenhardt F, Seifert S and Szymczak S:
Evaluation of variable selection methods for random forests and
omics data sets. Brief Bioinform. 20:492–503. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Friedman J, Hastie T and Tibshirani R:
Regularization paths for generalized linear models via coordinate
descent. J Stat Softw. 33:1–22. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Alderden J, Pepper GA, Wilson A, Whitney
JD, Richardson S, Butcher R, Jo Y and Cummins MR: Predicting
pressure injury in critical care patients: A Machine-learning
model. Am J Crit Care. 27:461–468. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Yoon S and Kim S: AdaBoost-based multiple
SVM-RFE for classification of mammograms in DDSM. BMC Med Inform
Decis Mak. 9 (Suppl 1):S12009. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Ding X, Qin J, Huang F, Feng F and Luo L:
The combination of machine learning and untargeted metabolomics
identifies the lipid metabolism-related gene CH25H as a potential
biomarker in asthma. Inflamm Res. 72:1099–1119. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Li Y and Song M: Exact Model-free function
inference using uniform marginal counts for null population.
Bioinformatics. 41:btaf1212025. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Robin X, Turck N, Hainard A, Tiberti N,
Lisacek F, Sanchez JC and Müller M: pROC: An open-source package
for R and S+ to analyze and compare ROC curves. BMC Bioinformatics.
12:772011. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Daina A, Michielin O and Zoete V:
SwissTargetPrediction: Updated data and new features for efficient
prediction of protein targets of small molecules. Nucleic Acids
Res. 47:W357–W364. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Forli S, Huey R, Pique ME, Sanner MF,
Goodsell DS and Olson AJ: Computational Protein-ligand docking and
virtual drug screening with the AutoDock suite. Nat Protoc.
11:905–919. 2016. View Article : Google Scholar
|
|
49
|
Trott O and Olson AJ: AutoDock Vina:
Improving the speed and accuracy of docking with a new scoring
function, efficient optimization, and multithreading. J Comput
Chem. 31:455–461. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
DeLano WL: Unraveling hot spots in binding
interfaces: Progress and challenges. Curr Opin Struct Biol.
12:14–20. 2002. View Article : Google Scholar
|
|
51
|
Hao Y, Hao S, Andersen-Nissen E, Mauck WM
III, Zheng S, Butler A, Lee MJ, Wilk AJ, Darby C, Zager M, et al:
Integrated analysis of multimodal single-cell data. Cell.
184:3573–3587.e29. 2021. View Article : Google Scholar
|
|
52
|
Butler A, Hoffman P, Smibert P, Papalexi E
and Satija R: Integrating single-cell transcriptomic data across
different conditions, technologies, and species. Nat Biotechnol.
36:411–420. 2018. View Article : Google Scholar
|
|
53
|
Valenzi E, Bulik M, Tabib T, Morse C,
Sembrat J, Trejo Bittar H, Rojas M and Lafyatis R: Single-cell
analysis reveals fibroblast heterogeneity and myofibroblasts in
systemic sclerosis-associated interstitial lung disease. Ann Rheum
Dis. 78:1379–1387. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Franzén O, Gan LM and Björkegren JLM:
PanglaoDB: A web server for exploration of mouse and human
single-cell RNA sequencing data. Database (Oxford).
2019:baz0462019.
|
|
55
|
Zhang X, Lan Y, Xu J, Quan F, Zhao E, Deng
C, Luo T, Xu L, Liao G, Yan M, et al: CellMarker: A manually
curated resource of cell markers in human and mouse. Nucleic Acids
Res. 47:D721–D728. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Anjaneyulu M and Chopra K: Quercetin, a
bioflavonoid, attenuates thermal hyperalgesia in a mouse model of
diabetic neuropathic pain. Prog Neuropsychopharmacol Biol
Psychiatry. 27:1001–1005. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Fan H, Tang HB, Shan LQ, Liu SC, Huang DG,
Chen X, Chen Z, Yang M, Yin XH, Yang H and Hao DJ: Quercetin
prevents necroptosis of oligodendrocytes by inhibiting
macrophages/microglia polarization to M1 phenotype after spinal
cord injury in rats. J Neuroinflammation. 16:2062019. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Basso DM, Fisher LC, Anderson AJ, Jakeman
LB, McTigue DM and Popovich PG: Basso mouse scale for locomotion
detects differences in recovery after spinal cord injury in five
common mouse strains. J Neurotrauma. 23:635–659. 2006. View Article : Google Scholar
|
|
59
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using Real-time quantitative PCR and
the 2(−Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Wang X, Fu Y, Botchway BOA, Zhang Y, Zhang
Y, Jin T and Liu X: Quercetin can improve spinal cord injury by
regulating the mTOR signaling pathway. Front Neurol. 13:9056402022.
View Article : Google Scholar
|
|
61
|
Bannister K, Sachau J, Baron R and
Dickenson AH: Neuropathic Pain: Mechanism-based therapeutics. Annu
Rev Pharmacol Toxicol. 60:257–274. 2020. View Article : Google Scholar
|
|
62
|
Torrance N, Ferguson JA, Afolabi E,
Bennett MI, Serpell MG, Dunn KM and Smith BH: Neuropathic pain in
the community: More under-treated than refractory? Pain.
154:690–699. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Jensen TS and Finnerup NB: Allodynia and
hyperalgesia in neuropathic pain: Clinical manifestations and
mechanisms. Lancet Neurol. 13:924–935. 2014. View Article : Google Scholar
|
|
64
|
Szok D, Tajti J, Nyári A and Vécsei L:
Therapeutic approaches for peripheral and central neuropathic pain.
Behav Neurol. 2019:86859542019.
|
|
65
|
McGinnis A and Ji RR: The similar and
distinct roles of satellite glial cells and spinal astrocytes in
neuropathic pain. Cells. 12:9652023. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Calvo M, Dawes JM and Bennett DL: The role
of the immune system in the generation of neuropathic pain. Lancet
Neurol. 11:629–642. 2012. View Article : Google Scholar
|
|
67
|
Hellenbrand DJ, Quinn CM, Piper ZJ,
Morehouse CN, Fixel JA and Hanna AS: Inflammation after spinal cord
injury: A review of the critical timeline of signaling cues and
cellular infiltration. J Neuroinflammation. 18:2842021. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Glaser J, Gonzalez R, Perreau VM, Cotman
CW and Keirstead HS: Neutralization of the chemokine CXCL10
enhances tissue sparing and angiogenesis following spinal cord
injury. J Neurosci Res. 77:701–708. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Garcia E, Aguilar-Cevallos J, Silva-Garcia
R and Ibarra A: Cytokine and growth factor activation in vivo and
in vitro after spinal cord injury. Mediators Inflamm.
2016:94760202016. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Sommer C, Leinders M and Üçeyler N:
Inflammation in the pathophysiology of neuropathic pain. Pain.
159:595–602. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Tang L, Song Z, Wang J, He S and Liu C:
Regulatory role of neuronal guidance proteins in spinal cord
injury. Neural Regen Res. May 6–2025.(Epub ahead of print). doi:
10.4103/NRR.NRR-D-24-00564. View Article : Google Scholar
|
|
72
|
Neshasteh-Riz A, Ramezani F, Kookli K,
Moghaddas Fazeli S, Motamed A, Nasirinezhad F, Janzadeh A, Hamblin
MR and Asadi M: Optimization of the duration and dose of
photobiomodulation therapy (660 nm Laser) for spinal cord injury in
rats. Photobiomodul Photomed Laser Surg. 40:488–498. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Huang Y, Gao P, Qin T, Chu B, Xu T, Yi J,
Wang Q, Yang Z, Jiang T, Fan J, et al: Delayed inhibition of
collagen deposition by targeting bone morphogenetic protein 1
promotes recovery after spinal cord injury. Matrix Biol. 118:69–91.
2023. View Article : Google Scholar
|
|
74
|
Frangogiannis N: Transforming growth
factor-β in tissue fibrosis. J Exp Med. 217:e201901032020.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Zhou X, He X and Ren Y: Function of
microglia and macrophages in secondary damage after spinal cord
injury. Neural Regen Res. 9:1787–1795. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Ji RR, Xu ZZ and Gao YJ: Emerging targets
in neuroinflammation-driven chronic pain. Nat Rev Drug Discov.
13:533–548. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Schoch HJ, Fischer S and Marti HH:
Hypoxia-induced vascular endothelial growth factor expression
causes vascular leakage in the brain. Brain. 125:2549–2557. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Dina OA, Parada CA, Yeh J, Chen X,
McCarter GC and Levine JD: Integrin signaling in inflammatory and
neuropathic pain in the rat. Eur J Neurosci. 19:634–642. 2004.
View Article : Google Scholar
|
|
79
|
Murray GI, Melvin WT, Greenlee WF and
Burke MD: Regulation, function, and tissue-specific expression of
cytochrome P450 CYP1B1. Annu Rev Pharmacol Toxicol. 41:297–316.
2001. View Article : Google Scholar
|
|
80
|
Lu Y, Nanayakkara G, Sun Y, Liu L, Xu K,
Drummer CIV, Shao Y, Saaoud F, Choi ET, Jiang X, et al:
Procaspase-1 patrolled to the nucleus of proatherogenic lipid
LPC-activated human aortic endothelial cells induces ROS promoter
CYP1B1 and strong inflammation. Redox Biol. 47:1021422021.
View Article : Google Scholar
|
|
81
|
Malik KU, Jennings BL, Yaghini FA,
Sahan-Firat S, Song CY, Estes AM and Fang XR: Contribution of
cytochrome P450 1B1 to hypertension and associated pathophysiology:
A novel target for antihypertensive agents. Prostaglandins Other
Lipid Mediat. 98:69–74. 2012. View Article : Google Scholar
|
|
82
|
Singh P, Dutta SR, Song CY, Oh S, Gonzalez
FJ and Malik KU: Brain Testosterone-CYP1B1 (Cytochrome P450 1B1)
generated metabolite 6β-Hydroxytestosterone promotes neurogenic
hypertension and inflammation. Hypertension. 76:1006–1018. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Yu M, Wang Z, Wang D, Aierxi M, Ma Z and
Wang Y: Oxidative stress following spinal cord injury: From
molecular mechanisms to therapeutic targets. J Neurosci Res.
101:1538–1554. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Fakhri S, Abbaszadeh F and Jorjani M: On
the therapeutic targets and pharmacological treatments for pain
relief following spinal cord injury: A mechanistic review. Biomed
Pharmacother. 139:1115632021. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Sun L, Zhang J, Niu C, Deering-Rice CE,
Hughen RW, Lamb JG, Rose K, Chase KM, Almestica-Roberts M, Walter
M, et al: CYP1B1-derived epoxides modulate the TRPA1 channel in
chronic pain. Acta Pharm Sin B. 13:68–81. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Falero-Perez J, Sorenson CM and Sheibani
N: Cyp1b1-deficient retinal astrocytes are more proliferative and
migratory and are protected from oxidative stress and inflammation.
Am J Physiol Cell Physiol. 316:C767–C781. 2019. View Article : Google Scholar
|
|
87
|
Lange KW and Li S: Resveratrol,
pterostilbene, and dementia. Biofactors. 44:83–90. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Azzini E, Peña-Corona SI, Hernández-Parra
H, Chandran D, Saleena LAK, Sawikr Y, Peluso I, Dhumal S, Kumar M,
Leyva-Gómez G, et al: Neuroprotective and anti-inflammatory effects
of curcumin in Alzheimer's disease: Targeting neuroinflammation
strategies. Phytother Res. 38:3169–3189. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Ocal O, Borcek AO, Pasaoglu O, Gundogdu
AC, Kaplanoglu GT and Baykaner MK: Can quercetin be an option for
treatment of spinal cord injury? An experimental study. Turk
Neurosurg. 29:247–253. 2019.PubMed/NCBI
|
|
90
|
Ye G, Lin C, Zhang Y, Ma Z, Chen Y, Kong
L, Yuan L and Ma T: Quercetin alleviates neuropathic pain in the
rat CCI model by mediating AMPK/MAPK pathway. J Pain Res.
14:1289–1301. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Fakhri S, Gravandi MM, Abdian S, Moradi SZ
and Echeverría J: Quercetin derivatives in combating spinal cord
injury: A mechanistic and systematic review. Life (Basel).
12:19602022. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Hou DD, Zhang W, Gao YL, Sun YZ, Wang HX,
Qi RQ, Chen HD and Gao XH: Anti-inflammatory effects of quercetin
in a mouse model of MC903-induced atopic dermatitis. Int
Immunopharmacol. 74:1056762019. View Article : Google Scholar
|
|
93
|
Gao Y, Wang Y, Wu Y and Liu S:
Biomaterials targeting the microenvironment for spinal cord injury
repair: Progression and perspectives. Front Cell Neurosci.
18:13624942024. View Article : Google Scholar
|