|
1
|
Gao X, Cai S, Li X and Wu G:
Sepsis-induced immunosuppression: Mechanisms, biomarkers and
immunotherapy. Front Immunol. 16:15771052025. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Evans L, Rhodes A, Alhazzani W, Antonelli
M, Coopersmith CM, French C, Machado FR, Mcintyre L, Ostermann M,
Prescott HC, et al: Surviving sepsis campaign: International
guidelines for management of sepsis and septic shock 2021.
Intensive Care Med. 47:1181–1247. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
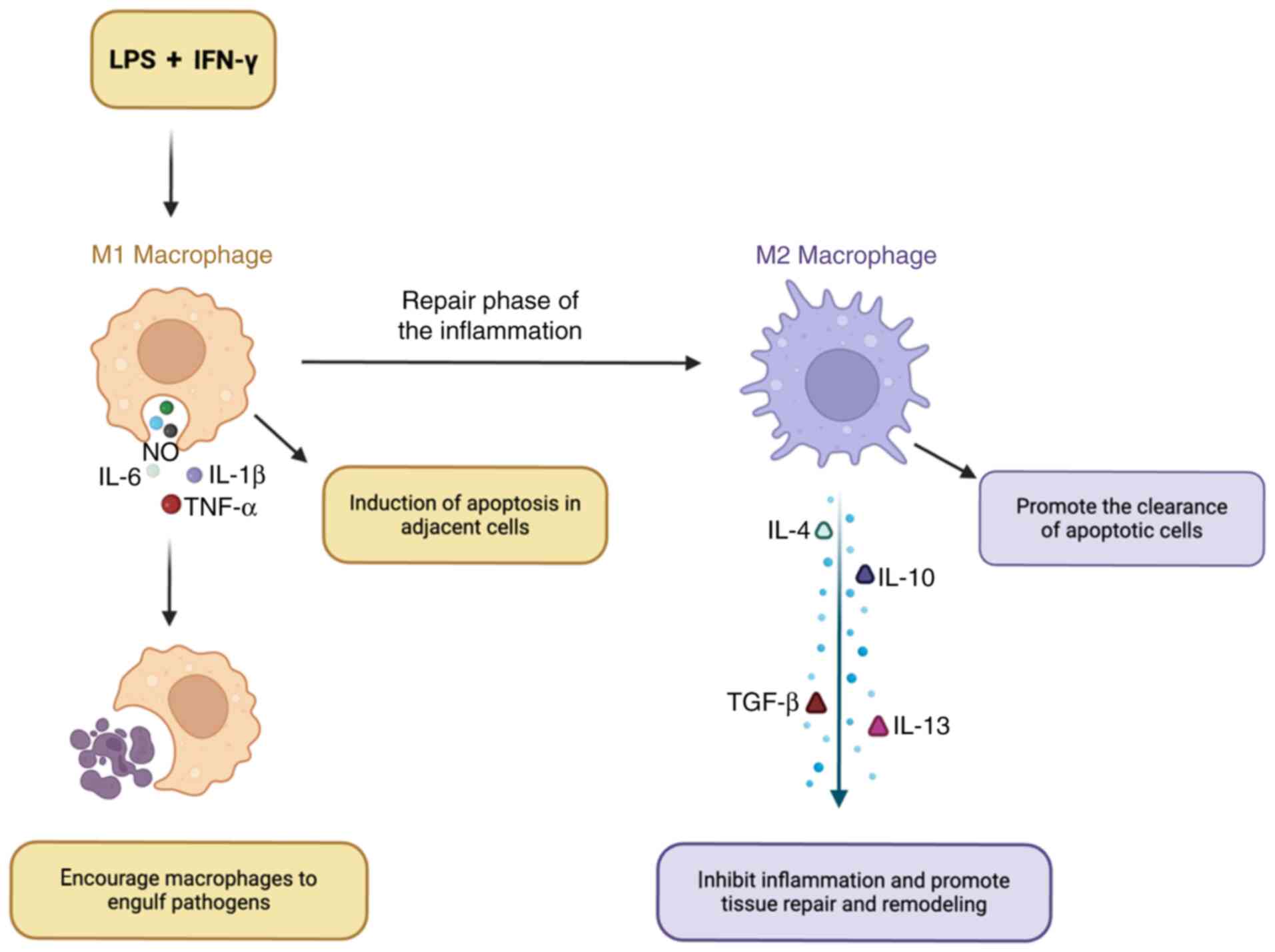
Xie J, Wang H, Kang Y, Zhou L, Liu Z, Qin
B, Ma X, Cao X, Chen D, Lu W, et al: The epidemiology of sepsis in
Chinese ICUs: A National cross-sectional survey. Crit Care Med.
48:e209–e218. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Dulhunty JM, Brett SJ, De Waele JJ,
Rajbhandari D, Billot L, Cotta MO, Davis JS, Finfer S, Hammond NE,
Knowles S, et al: Continuous vs Intermittent β-lactam antibiotic
infusions in critically Ill patients with sepsis: The BLING III
Randomized clinical trial. JAMA. 332:629–637. 2024. View Article : Google Scholar : PubMed/NCBI
|
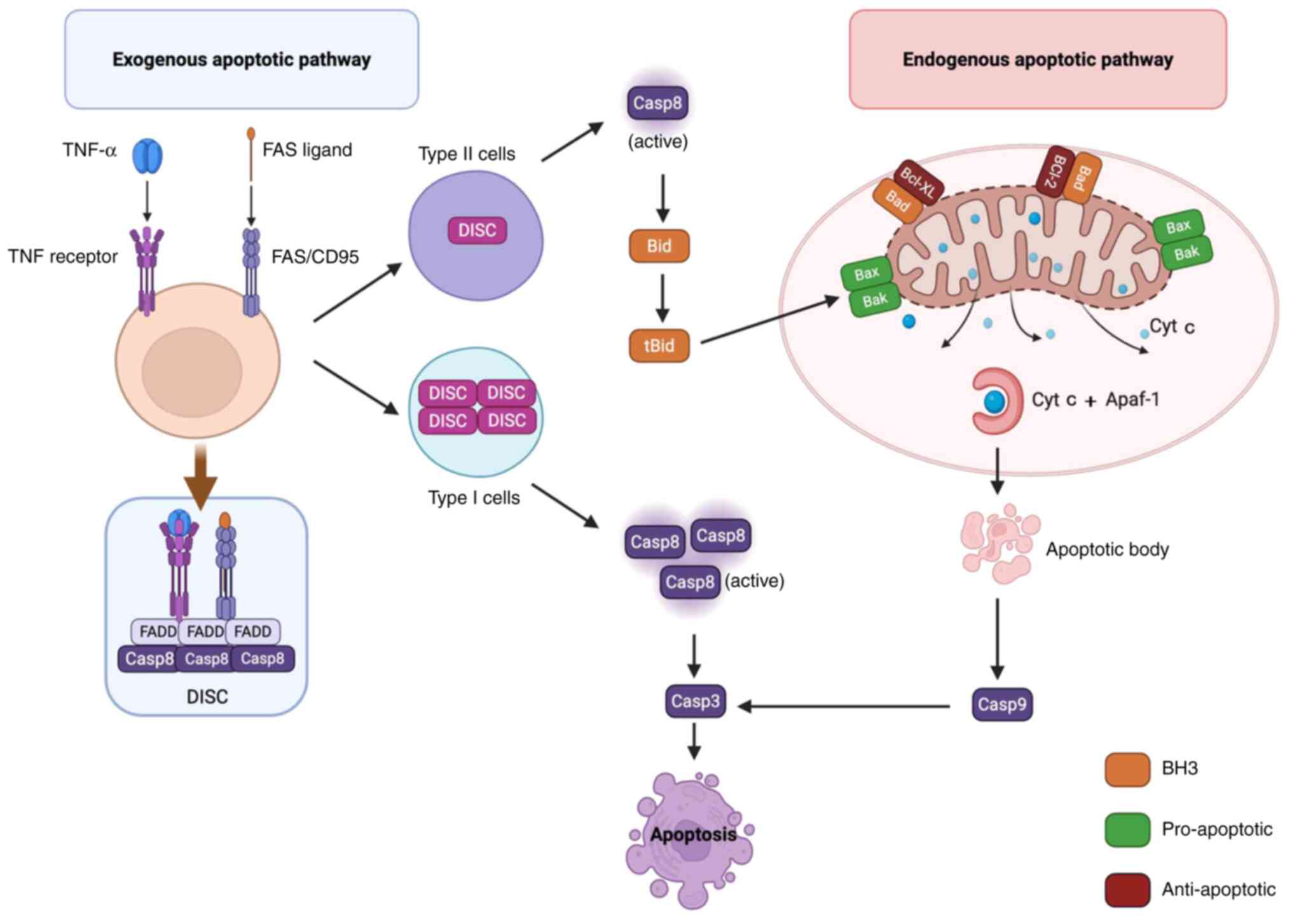
|
5
|
Li W, Li D, Chen Y, Abudou H, Wang H, Cai
J, Wang Y, Liu Z, Liu Y and Fan H: Classic signaling pathways in
alveolar injury and repair involved in sepsis-induced ALI/ARDS: New
research progress and prospect. Dis Markers.
2022:63623442022.PubMed/NCBI
|
|
6
|
Vincent JL, Opal SM, Marshall JC and
Tracey KJ: Sepsis definitions: Time for change. Lancet.
381:774–775. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Jiang J, Huang K, Xu S, Garcia JGN, Wang C
and Cai H: Targeting NOX4 alleviates sepsis-induced acute lung
injury via attenuation of redox-sensitive activation of
CaMKII/ERK1/2/MLCK and endothelial cell barrier dysfunction. Redox
Biol. 36:1016382020. View Article : Google Scholar : PubMed/NCBI
|
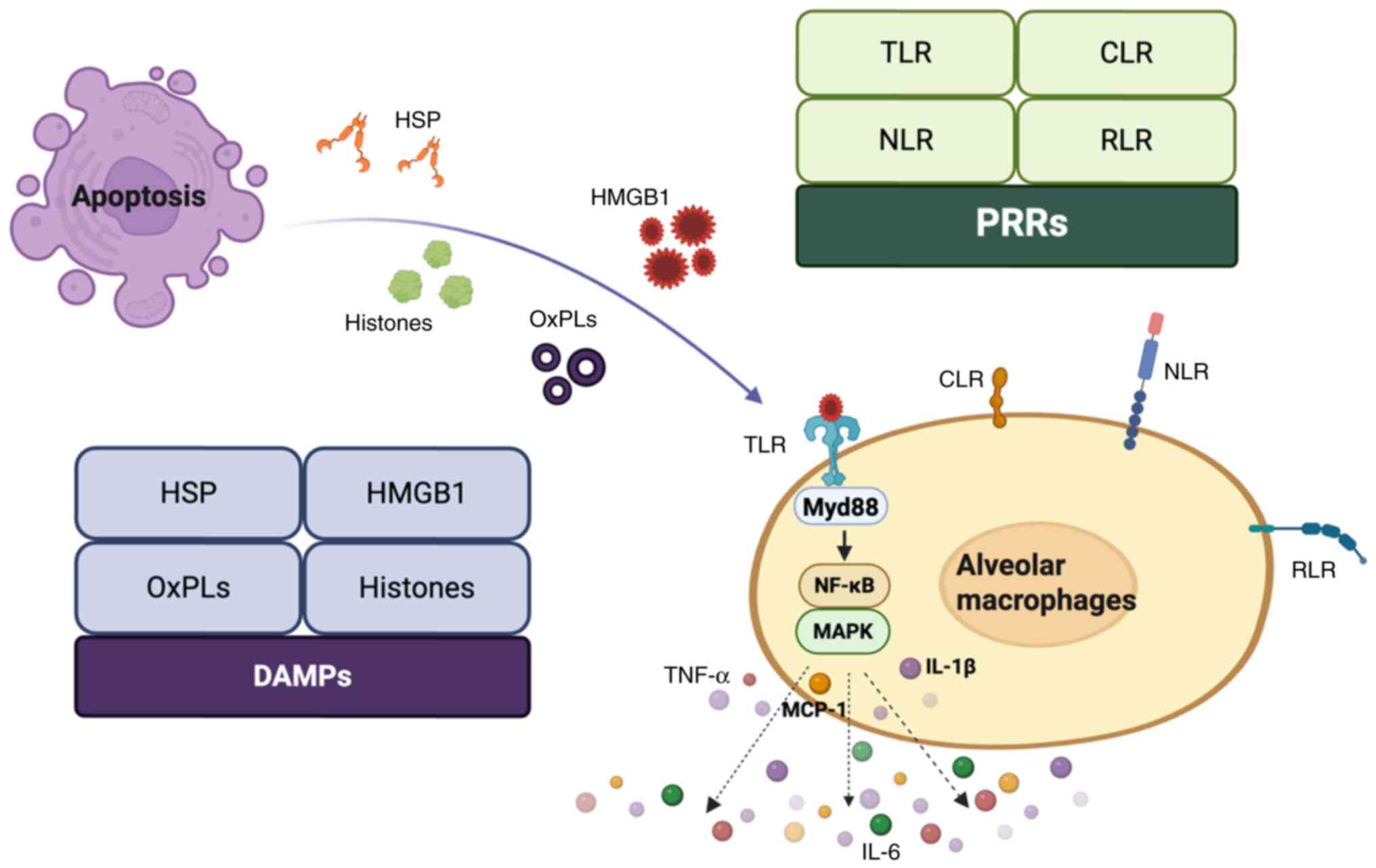
|
8
|
Boada-Romero E, Martinez J, Heckmann BL
and Green DR: The clearance of dead cells by efferocytosis. Nat Rev
Mol Cell Biol. 21:398–414. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Qu J, Jin J, Zhang M and Ng LG: Neutrophil
diversity and plasticity: Implications for organ transplantation.
Cell Mol Immunol. 20:993–1001. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zi SF, Wu XJ, Tang Y, Liang YP, Liu X,
Wang L, Li SL, Wu CD, Xu JY, Liu T, et al: Endothelial cell-derived
extracellular vesicles promote aberrant neutrophil trafficking and
subsequent remote lung injury. Adv Sci (Weinh). 11:e24006472024.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yang R, Zheng T, Xiang H, Liu M and Hu K:
Lung single-cell RNA profiling reveals response of pulmonary
capillary to sepsis-induced acute lung injury. Front Immunol.
15:13089152024. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Serhan CN, Chiang N and Van Dyke TE:
Resolving inflammation: Dual anti-inflammatory and pro-resolution
lipid mediators. Nat Rev Immunol. 8:349–361. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
do Nascimento MF, Ferreira LRP, Vieira
Junior JM, Deheinzelin D, Aparecida Santos Nussbaum AC, Toshihiro
Sakamoto LH, Vasconcelos RO, Salomao R, Waisberg J, Azevedo LCP, et
al: Circulating extracellular vesicles as potential biomarkers and
mediators of acute respiratory distress syndrome in sepsis. Sci
Rep. 15:55122025. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gupta S and Sahni V: The intriguing
commonality of NETosis between COVID-19 & Periodontal disease.
Med Hypotheses. 144:1099682020. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Scozzi D, Liao F, Krupnick AS, Kreisel D
and Gelman AE: The role of neutrophil extracellular traps in acute
lung injury. Front Immunol. 13:9531952022. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kumar S, Payal N, Srivastava VK, Kaushik
S, Saxena J and Jyoti A: Neutrophil extracellular traps and organ
dysfunction in sepsis. Clin Chim Acta. 523:152–162. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
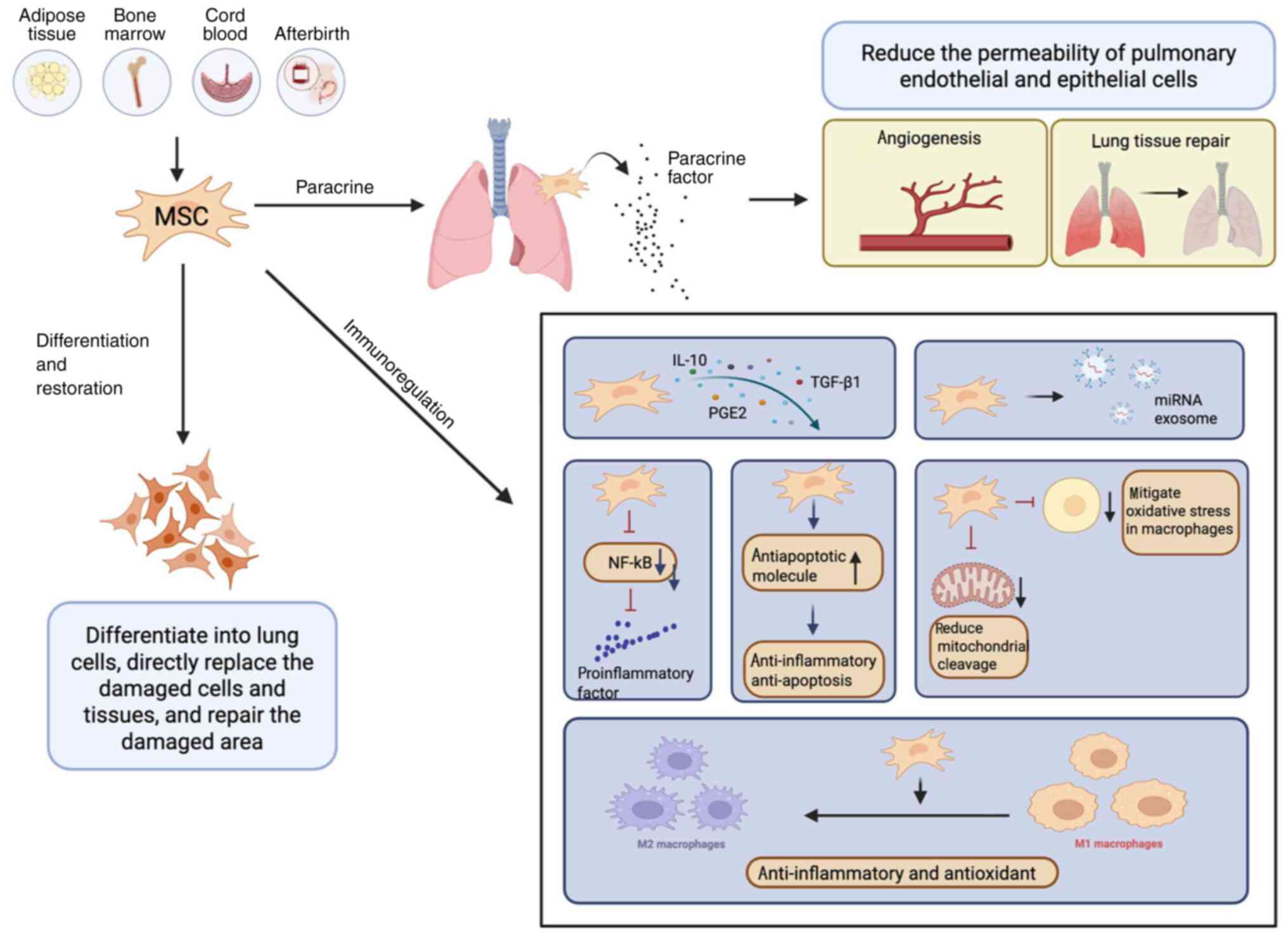
17
|
Zhang H, Wang Y, Qu M, Li W, Wu D, Cata JP
and Miao C: Neutrophil, neutrophil extracellular traps and
endothelial cell dysfunction in sepsis. Clin Transl Med.
13:e11702023. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Fuchs TA, Brill A, Duerschmied D,
Schatzberg D, Monestier M, Myers DD Jr, Wrobleski SK, Wakefield TW,
Hartwig JH and Wagner DD: Extracellular DNA traps promote
thrombosis. Proc Natl Acad Sci USA. 107:15880–15885. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Peng Y, Zhou M, Yang H, Qu R, Qiu Y, Hao
J, Bi H and Guo D: Regulatory mechanism of M1/M2 macrophage
polarization in the development of autoimmune diseases. Mediators
Inflamm. 2023:88216102023. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Dang W, Tao Y, Xu X, Zhao H, Zou L and Li
Y: The role of lung macrophages in acute respiratory distress
syndrome. Inflamm Res. 71:1417–1432. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wang Z and Wang Z: The role of macrophages
polarization in sepsis-induced acute lung injury. Front Immunol.
14:12094382023. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Li S, Feng T, Zhang Y, Shi Q, Wang W, Ren
J, Shen G, Gu H, Luo C and Li Y: Lianhua Qingwen protects
LPS-induced acute lung injury by promoting M2 macrophage
infiltration. J Ethnopharmacol. 320:1174672024. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Yang J, Huang X, Yu Q, Wang S, Wen X, Bai
S, Cao L, Zhang K, Zhang S and Wang X: Extracellular vesicles
derived from M2-like macrophages alleviate acute lung injury in a
miR-709-mediated manner. J Extracell Vesicles. 13:e124372024.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Morrell ED, Bhatraju PK, Mikacenic CR,
Radella F II, Manicone AM, Stapleton RD, Wurfel MM and Gharib SA:
Alveolar macrophage transcriptional programs are associated with
outcomes in acute respiratory distress Syndrome. Am J Respir Crit
Care Med. 200:732–741. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zenga J, Loi GWZ, Saipuljumri EN, Romero
Durán MA, Silva-García O, Perez-Aguilar JM, Baizabal-Aguirre VM and
Lo CH: Peptide-based allosteric inhibitor targets TNFR1
conformationally active region and disables receptor-ligand
signaling complex. Proc Natl Acad Sci USA. 121:e23081321212024.
View Article : Google Scholar
|
|
26
|
Crijns H, Vanheule V and Proost P:
Targeting chemokine-glycosaminoglycan interactions to inhibit
inflammation. Front Immunol. 11:4832020. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Karin N and Wildbaum G: The role of
chemokines in shaping the balance between CD4+ T cell subsets and
its therapeutic implications in autoimmune and cancer diseases.
Front Immunol. 6:6092015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Yang S, Yu J, Dong X, Zeng J, Tan L, Zhang
H, Sun R, Tuo Y, Yang J, Wan C and Bai H: CCR2 signaling regulates
anti-chlamydia T cell immune responses in the airway. PLoS Pathog.
21:e10129122025. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Cheng PP, He XL, Jia ZH, Hu SH, Feng X,
Jiang YH, Li Q, Zhao LQ, Cui XL, Ye SY, et al: Midkine, a novel
MCP-1 activator mediated PM2.5-aggravated experimental pulmonary
fibrosis. Environ Int. 197:1093542025. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Neehus AL, Carey B, Landekic M, Panikulam
P, Deutsch G, Ogishi M, Arango-Franco CA, Philippot Q, Modaresi M,
Mohammadzadeh I, et al: Human inherited CCR2 deficiency underlies
progressive polycystic lung disease. Cell. 187:390–408. e232024.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Molino S, Pisarevsky A, Badu S, Wu Q,
Mingorance FL, Vega P, Stefanolo JP, Repetti J, Ludueña G, Pepa P,
et al: Randomized placebo-controlled trial of oral tannin
supplementation on COVID-19 symptoms, gut dysbiosis and cytokine
response. J Funct Foods. 99:1053562022. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Hammock BD, Wang W, Gilligan MM and
Panigrahy D: Eicosanoids: The overlooked storm in coronavirus
disease 2019 (COVID-19)? Am J Pathol. 190:1782–1788. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Wu J, Ye J, Kong W, Zhang S and Zheng Y:
Programmed cell death pathways in hearing loss: A review of
apoptosis, autophagy and programmed necrosis. Cell Prolif.
53:e129152020. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Dho SH, Cho M, Woo W, Jeong S and Kim LK:
Caspases as master regulators of programmed cell death: apoptosis,
pyroptosis and beyond. Exp Mol Med. 57:1121–1132. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Carneiro BA and El-Deiry WS: Targeting
apoptosis in cancer therapy. Nat Rev Clin Oncol. 17:395–417. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Algeciras-Schimnich A, Shen L, Barnhart
BC, Murmann AE, Burkhardt JK and Peter ME: Molecular ordering of
the initial signaling events of CD95. Mol Cell Biol. 22:207–220.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Fu Y, Sacco O, DeBitetto E, Kanshin E,
Ueberheide B and Sfeir A: Mitochondrial DNA breaks activate an
integrated stress response to reestablish homeostasis. Mol Cell.
83:3740–3753. e92023. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Bilen M, Benhammouda S, Slack RS and
Germain M: The integrated stress response as a key pathway
downstream of mitochondrial dysfunction. Curr Opinion Physiol.
27:1005552022. View Article : Google Scholar
|
|
39
|
Breckenridge DG, Stojanovic M, Marcellus
RC and Shore GC: Caspase cleavage product of BAP31 induces
mitochondrial fission through endoplasmic reticulum calcium
signals, enhancing cytochrome c release to the cytosol. J Cell
Biol. 160:1115–1127. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Du Y, Wang G, Liu B, Guo M, Yan X, Dou M,
Yu F, Ba Y and Zhou G: Naringin alleviates fluoride-induced
neurological impairment: A focus on the regulation of energy
metabolism mediated by mitochondrial permeability transition pore.
Sci Total Environ. 955:1770732024. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Xue Y, Wang J, Huang Y, Gao X, Kong L,
Zhang T and Tang M: Comparative cytotoxicity and apoptotic pathways
induced by nanosilver in human liver HepG2 and L02 cells. Hum Exp
Toxicol. 37:1293–1309. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Chang X, Niu S, Shang M, Li J, Guo M,
Zhang W, Sun Z, Li Y, Zhang R, Shen X, et al: ROS-Drp1-mediated
mitochondria fission contributes to hippocampal HT22 cell apoptosis
induced by silver nanoparticles. Redox Biol. 63:1027392023.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Wang HW, Zhang Y, Tan PP, Jia LS, Chen Y
and Zhou BH: Mitochondrial respiratory chain dysfunction mediated
by ROS is a primary point of fluoride-induced damage in Hepa1-6
cells. Environ Pollut. 255((Pt 3)): 1133592019. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Kushnareva Y, Andreyev AY, Kuwana T and
Newmeyer DD: Bax activation initiates the assembly of a multimeric
catalyst that facilitates bax pore formation in mitochondrial outer
membranes. PLoS Biol. 10:e10013942012. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Vandenabeele P, Bultynck G and Savvides
SN: Pore-forming proteins as drivers of membrane permeabilization
in cell death pathways. Nat Rev Mol Cell Biol. 24:312–333. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
An J, Park SH, Ko IG, Jin JJ, Hwang L, Ji
ES, Kim SH, Kim CJ, Park SY, Hwang JJ and Choi CW:
Polydeoxyribonucleotide ameliorates lipopolysaccharide-induced lung
injury by inhibiting apoptotic cell death in rats. Int J Mol Sci.
18:18472017. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Wang H, Guo M, Wei H and Chen Y: Targeting
p53 pathways: Mechanisms, structures, and advances in therapy.
Signal Transduct Target Ther. 8:922023. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Chen L, Liu S and Tao Y: Regulating tumor
suppressor genes: Post-translational modifications. Signal
Transduct Target Ther. 5:902020. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Wei H, Qu L, Dai S, Li Y, Wang H, Feng Y,
Chen X, Jiang L, Guo M, Li J, et al: Structural insight into the
molecular mechanism of p53-mediated mitochondrial apoptosis. Nat
Commun. 12:22802021. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Aubrey BJ, Kelly GL, Janic A, Herold MJ
and Strasser A: How does p53 induce apoptosis and how does this
relate to p53-mediated tumour suppression? Cell Death Differ.
25:104–113. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Wang S, Zhong S, Huang Y, Zhu S, Chen S,
Wang R, Wangmo S, Peng B, Lv H, Yang J, et al: MDM2 is essential to
maintain the homeostasis of epithelial cells by targeting p53. J
Innate Immun. 16:397–412. 2024.PubMed/NCBI
|
|
52
|
Lane K, Andres-Terre M, Kudo T, Monack DM
and Covert MW: Escalating threat levels of bacterial infection can
be discriminated by distinct MAPK and NF-kappaB signaling dynamics
in single host cells. Cell Syst. 8:183–196. e42019. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
DeCuzzi NL, Oberbauer D, Chmiel KJ,
Pargett M, Ferguson JM, Murphy D, Hardy M, Ram A, Zeki AA and
Albeck JG: Spatiotemporal clusters of extracellular
signal-regulated kinase activity coordinate cytokine-induced
inflammatory responses in human airway epithelial cells. Am J
Respir Cell Mol Biol. 72:520–532. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Mokra D: Acute lung injury - from
pathophysiology to treatment. Physiol Res. 69 (Suppl 3):S353–S366.
2020.PubMed/NCBI
|
|
55
|
McMinimy R, Manford AG, Gee CL,
Chandrasekhar S, Mousa GA, Chuang J, Phu L, Shih KY, Rose CM,
Kuriyan J, et al: Reactive oxygen species control protein
degradation at the mitochondrial import gate. Mol Cell.
84:4612–4628. e132024. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Zhang J, Wei Y, Yue Y, Jiao H, Wu Y, Fu W,
Lin KM, Lu C, Mou S and Zhong Q: RIPK4 promotes oxidative stress
and ferroptotic death through the downregulation of ACSM1. Proc
Natl Acad Sci USA. 121:e24106281212024. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Liang J, Cao R, Wang X, Zhang Y, Wang P,
Gao H, Li C, Yang F, Zeng R, Wei P, et al: Mitochondrial PKM2
regulates oxidative stress-induced apoptosis by stabilizing Bcl2.
Cell Res. 27:329–351. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Ma M, Jiang W and Zhou R: DAMPs and
DAMP-sensing receptors in inflammation and diseases. Immunity.
57:752–771. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Deng C, Zhao L, Yang Z, Shang JJ, Wang CY,
Shen MZ, Jiang S, Li T, Di WC, Chen Y, et al: Targeting HMGB1 for
the treatment of sepsis and sepsis-induced organ injury. Acta
Pharmacol Sin. 43:520–528. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Dutta S, Dutta S, Somanath PR, Narayanan
SP, Wang X and Zhang D: Circulating nucleosomes and histones in the
development of lung injury and sepsis. Curr Issues Mol Biol.
47:1332025. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Pei Q, Ni W, Yuan Y, Yuan J, Zhang X and
Yao M: HSP70 Ameliorates Septic Lung Injury via Inhibition of
Apoptosis by Interacting with KANK2. Biomolecules. 12:4102022.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Karki P, Zhang CO, Promnares K, Li Y, Ke
Y, Birukova AA and Birukov KG: Truncated oxidized phospholipids
exacerbate endothelial dysfunction and lung injury caused by
bacterial pathogens. Cell Signal. 109:1108042023. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Munemasa Y: Histone H2B induces retinal
ganglion cell death through toll-like receptor 4 in the vitreous of
acute primary angle closure patients. Lab Invest. 100:1080–1089.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Beltran-Garcia J, Osca-Verdegal R,
Perez-Cremades D, Novella S, Hermenegildo C, Pallardó FV and
García-Giménez JL: Extracellular histones activate endothelial
NLRP3 inflammasome and are associated with a severe sepsis
phenotype. J Inflamm Res. 15:4217–4238. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Orecchioni M, Kobiyama K, Winkels H,
Ghosheh Y, McArdle S, Mikulski Z, Kiosses WB, Fan Z, Wen L, Jung Y,
et al: Olfactory receptor 2 in vascular macrophages drives
atherosclerosis by NLRP3-dependent IL-1 production. Science.
375:214–221. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Dong Y and Yong VW: Oxidized phospholipids
as novel mediators of neurodegeneration. Trends Neurosci.
45:419–429. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Elliott MR, Chekeni FB, Trampont PC,
Lazarowski ER, Kadl A, Walk SF, Park D, Woodson RI, Ostankovich M,
Sharma P, et al: Nucleotides released by apoptotic cells act as a
find-me signal to promote phagocytic clearance. Nature.
461:282–286. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Yang M, Liu J, Piao C, Shao J and Du J:
ICAM-1 suppresses tumor metastasis by inhibiting macrophage M2
polarization through blockade of efferocytosis. Cell Death Dis.
6:e17802015. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Wang Y, Zhang W, Xu Y, Wu D, Gao Z, Zhou
J, Qian H, He B and Wang G: Extracellular HMGB1 impairs
macrophage-mediated efferocytosis by suppressing the
Rab43-controlled cell surface transport of CD91. Front Immunol.
13:7676302022. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Bondue B, Vosters O, de Nadai P, Glineur
S, De Henau O, Luangsay S, Van Gool F, Communi D, De Vuyst P,
Desmecht D and Parmentier M: ChemR23 dampens lung inflammation and
enhances anti-viral immunity in a mouse model of acute viral
pneumonia. PLoS Pathog. 7:e10023582011. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Duvall MG, Bruggemann TR and Levy BD:
Bronchoprotective mechanisms for specialized pro-resolving
mediators in the resolution of lung inflammation. Mol Aspects Med.
58:44–56. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Bos LDJ and Ware LB: Acute respiratory
distress syndrome: Causes, pathophysiology, and phenotypes. Lancet.
400:1145–1156. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Burgess CL, Huang J, Bawa PS, Alysandratos
KD, Minakin K, Ayers LJ, Morley MP, Babu A, Villacorta-Martin C,
Yampolskaya M, et al: Generation of human alveolar epithelial type
I cells from pluripotent stem cells. Cell Stem Cell. 31:657–675.
e82024. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Meyer NJ, Gattinoni L and Calfee CS: Acute
respiratory distress syndrome. Lancet. 398:622–637. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Rizzo AN, Haeger SM, Oshima K, Yang Y,
Wallbank AM, Jin Y, Lettau M, McCaig LA, Wickersham NE, McNeil JB,
et al: Alveolar epithelial glycocalyx degradation mediates
surfactant dysfunction and contributes to acute respiratory
distress syndrome. JCI Insight. 7:e1545732022. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Han S, Lee M, Shin Y, Giovanni R,
Chakrabarty RP, Herrerias MM, Dada LA, Flozak AS, Reyfman PA,
Khuder B, et al: Mitochondrial integrated stress response controls
lung epithelial cell fate. Nature. 620:890–897. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Xi Q, Liu L, Zhao Q and Zhu S: KLF13
attenuates lipopolysaccharide-induced alveolar epithelial cell
damage by regulating mitochondrial quality control via binding
PGC-1α. J Interferon Cytokine Res. 45:227–237. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Wang C, Wu Z, Li Z, Wang Z, Ke H and Huang
X: Beneficial effect of the mitochondrial ATP-sensitive potassium
channel-specific opener nicorandil on the collapsed lung via
inhibition of apoptosis in clinical thoracic surgery. Mol Med Rep.
27:612023. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Lei X, Liu X, Yu J, Li K, Xia L, Su S, Lin
P, Zhang D and Li Y: 3-methyladenine ameliorates acute lung injury
by inhibiting oxidative damage and apoptosis. Heliyon.
10:e339962024. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Lanzoni G, Linetsky E, Correa D, Messinger
Cayetano S, Alvarez RA, Kouroupis D, Alvarez Gil A, Poggioli R,
Ruiz P, Marttos AC, et al: Umbilical cord mesenchymal stem cells
for COVID-19 acute respiratory distress syndrome: A double-blind,
phase 1/2a, randomized controlled trial. Stem Cells Transl Med.
10:660–673. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Collada A, Cruz A and Perez-Gil J:
Studying the interfacial activity and structure of pulmonary
surfactant complexes. Chem Phys Lipids. 266:1054592025. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Inoue S, Nagao J, Kawamoto K, Kan-O K,
Fukuyama S, Sasaki S, Kudo S, Okamoto I and Sera T: Overstretching
alveolar epithelial type II cells decreases surfactant secretion
via actin polymerization and intracellular trafficking alteration.
Heliyon. 10:e334992024. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Hanusrichterova J, Mokry J, Al-Saiedy MR,
Koetzler R, Amrein MW, Green FHY and Calkovska A: Factors
influencing airway smooth muscle tone: A comprehensive review with
a special emphasis on pulmonary surfactant. Am J Physiol Cell
Physiol. 327:C798–C816. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Bastani MN and Jalilian S: Unraveling the
enigma: The emerging significance of pulmonary surfactant proteins
in predicting, diagnosing, and managing COVID-19. Immun Inflamm
Dis. 12:e13022024. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Jacob IB, Lawal AO, Mahmoud SS, Kopsack
EM, Reynolds ES, Meng Q, Fan H, Massa PT, Thangamani S, Jia H and
Wang G: Differential immunoregulation by human surfactant protein A
variants determines severity of SARS-CoV-2-induced lung disease.
Front Immunol. 16:14622782025. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Zhu Y, Choi D, Somanath PR and Zhang D:
Lipid-laden macrophages in pulmonary diseases. Cells. 13:8892024.
View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Zhang J, Deng Y, Li G and Sun X: Interplay
of surfactant protein A and tumor necrosis factor α in lung and
intestinal tissues of rats with severe pneumonia. Mol Biotechnol.
Apr 24–2025.(Epub ahead of print). View Article : Google Scholar
|
|
88
|
Dargaville PA, Kamlin COF, Orsini F, Wang
X, De Paoli AG, Kanmaz Kutman HG, Cetinkaya M, Kornhauser-Cerar L,
Derrick M, Özkan H, et al: Two-year outcomes after minimally
invasive surfactant therapy in preterm infants: Follow-Up of the
OPTIMIST-A Randomized clinical trial. JAMA. 330:1054–1063. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Schupp JC, Adams TS, Cosme C Jr, Raredon
MSB, Yuan Y, Omote N, Poli S, Chioccioli M, Rose KA, Manning EP, et
al: Integrated single-cell atlas of endothelial cells of the human
lung. Circulation. 144:286–302. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Whitney JE, Zhang B, Koterba N, Chen F,
Bush J, Graham K, Lacey SF, Melenhorst JJ, Teachey DT, Mensinger
JL, et al: Systemic endothelial activation is associated with early
acute respiratory distress syndrome in children with extrapulmonary
sepsis. Crit Care Med. 48:344–352. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Runkle EA and Mu D: Tight junction
proteins: From barrier to tumorigenesis. Cancer Lett. 337:41–48.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Guo X, Eitnier RA, Beard RS Jr, Meegan JE,
Yang X, Aponte AM, Wang F, Nelson PR and Wu MH: Focal adhesion
kinase and Src mediate microvascular hyperpermeability caused by
fibrinogen- үC-terminal fragments. PLoS One. 15:e02317392020.
View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Garcia-Flores AE, Gross CM, Zemskov EA, Lu
Q, Tieu K, Wang T and Black SM: Loss of SOX18/CLAUDIN5 disrupts the
pulmonary endothelial barrier in ventilator-induced lung injury.
Front Physiol. 13:10665152022. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Rezk-Hanna M, Rossman MJ, Ludwig K, Sakti
P, Cheng CW, Brecht ML, Benowitz NL and Seals DR: Electronic hookah
(waterpipe) vaping reduces vascular endothelial function: The role
of nicotine. Am J Physiol Heart Circ Physiol. 326:H490–H496. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Solomon SD, Lowenstein CJ, Bhatt AS,
Peikert A, Vardeny O, Kosiborod MN, Berger JS, Reynolds HR,
Mavromichalis S, Barytol A, et al: Effect of the P-selectin
inhibitor crizanlizumab on survival free of organ support in
patients hospitalized for COVID-19: A Randomized controlled trial.
Circulation. 148:381–390. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Zhu J, Yang L, Jia Y, Balistrieri A,
Fraidenburg DR, Wang J, Tang H and Yuan JX: Pathogenic mechanisms
of pulmonary arterial hypertension: Homeostasis imbalance of
endothelium-derived relaxing and contracting factors. JACC Asia.
2:787–802. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Boron M, Hauzer-Martin T, Keil J and Sun
XL: Circulating thrombomodulin: Release mechanisms, measurements,
and levels in diseases and medical procedures. TH Open.
6:e194–e212. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Sanchez-Santillan RN, Sierra-Vargas MP,
Gonzalez-Islas D, Aztatzi-Aguilar OG, Pérez-Padilla R, Orea-Tejeda
A, Debray-García Y, Ortega-Romero M, Keirns-Davis C, Loaeza-Roman A
and Rios-Pereda A: Endothelial biomarkers (Von willebrand factor,
BDCA3, urokinase) as predictors of mortality in COVID-19 patients:
Cohort study. BMC Pulm Med. 24:3252024. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Neubauer K and Zieger B: Endothelial cells
and coagulation. Cell Tissue Res. 387:391–398. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Naderpour Z, Aliannejad R, Mehrtash V,
Mollazadeh R, Hosseini SE, Amini S, Pak N, Motlaq TM, Khodaei B,
Jafarzadeh B, et al: Tissue plasminogen activator for
COVID-19-induced severe acute respiratory distress Syndrome: A
controlled clinical trial. Infect Disord Drug Targets. 2025.(Epub
ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Tung YT, Wei CH, Yen CC, Lee PY, Ware LB,
Huang HE, Chen W and Chen CM: Aspirin attenuates hyperoxia-induced
acute respiratory distress Syndrome (ARDS) by suppressing pulmonary
inflammation via the NF-kappaB signaling pathway. Front Pharmacol.
12:7931072022. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Li XG, Song X, Wang JY, Sun CH, Li ZQ,
Meng LL and Chi SH: Fibroblast growth factor 18 alleviates
hyperoxia-induced lung injury in mice by adjusting oxidative stress
and inflammation. Eur Rev Med Pharmacol Sci. 25:1485–1494.
2021.PubMed/NCBI
|
|
103
|
Hu Z, Dai J, Xu T, Chen H, Shen G, Zhou J,
Ma H, Wang Y and Jin L: FGF18 alleviates sepsis-induced acute lung
injury by inhibiting the NF-ĸB pathway. Respir Res. 25:1082024.
View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Wang T, Lv L, Feng H and Gu W: Unlocking
the potential: Quercetin and its natural derivatives as promising
therapeutics for sepsis. Biomedicines. 12:4442024. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Malekinejad Z, Baghbanzadeh A, Nakhlband
A, Baradaran B, Jafari S, Bagheri Y, Raei F, Montazersaheb S and
Farahzadi R: Recent clinical findings on the role of kinase
inhibitors in COVID-19 management. Life Sci. 306:1208092022.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Sun DZ, Song CQ, Xu YM and Dong XS: Role
of the MAPK pathway in human lung epithelial-like A549 cells
apoptosis induced by paraquat. Genet Mol Biol. 43:e201901372020.
View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Grassme H, Kirschnek S, Riethmueller J,
Riehle A, von Kürthy G, Lang F, Weller M and Gulbins E: CD95/CD95
ligand interactions on epithelial cells in host defense to
Pseudomonas aeruginosa. Science. 290:527–530. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Sun R, Jiang K, Zeng C, Zhu R, Chu H, Liu
H and Du J: Synergism of TNF-α and IFN-β triggers human airway
epithelial cells death by apoptosis and pyroptosis. Mol Immunol.
153:160–169. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Luo Z, Wang Q, Fan X, Koh XQ, Loh XJ, Wu
C, Li Z and Wu YL: ROS-driven nanoventilator for MRSA-induced acute
lung injury treatment via in situ oxygen supply, anti-inflammation
and immunomodulation. Adv Sci (Weinh). 12:e24060602025. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Hansberg W: Monofunctional Heme-Catalases.
Antioxidants (Basel). 11:21732022. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Flohe L, Toppo S and Orian L: The
glutathione peroxidase family: Discoveries and mechanism. Free
Radic Biol Med. 187:113–122. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Chen Y, Yang H, Hu X, Yang T, Zhao Y, Liu
H and Fan H: Coenzyme Q10 ameliorates lipopolysaccharide-induced
acute lung injury by attenuating oxidative stress and NLRP3
inflammation through regulating mitochondrial dynamics. Int
Immunopharmacol. 141:1129412024. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Wang Y, Lilienfeldt N and Hekimi S:
Understanding coenzyme Q. Physiol Rev. 104:1533–1610. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Honsho M and Fujiki Y: Asymmetric
distribution of plasmalogens and their roles-A mini review.
Membranes (Basel). 13:7642023. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Steenberge LH, Rogers S, Sung AY, Fan J
and Pagliarini DJ: Coenzyme Q(4) is a functional substitute for
coenzyme Q(10) and can be targeted to the mitochondria. J Biol
Chem. 300:1072692024. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Traber MG, Leonard SW, Vasu VT, Morrissey
BM, Lei HJ, Atkinson J and Cross CE: α-Tocopherol pharmacokinetics
in adults with cystic fibrosis: Benefits of supplemental vitamin C
administration. Nutrients. 14:37172022. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Traber MG and Head B: Vitamin E: How much
is enough, too much and why! Free Radic Biol Med. 177:212–225.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Kazemi A, Iraji A, Esmaealzadeh N, Salehi
M and Hashempur MH: Peppermint and menthol: A review on their
biochemistry, pharmacological activities, clinical applications,
and safety considerations. Crit Rev Food Sci Nutr. 65:1553–1578.
2025. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Huang M, Liu X, Ren Y, Huang Q, Shi Y,
Yuan P and Chen M: Quercetin: A flavonoid with potential for
treating acute lung injury. Drug Des Devel Ther. 18:5709–5728.
2024. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Martini D, Negrini L, Marino M, Riso P,
Del Bo C and Porrini M: What is the current direction of the
research on carotenoids and human health? An overview of registered
clinical trials. Nutrients. 14:11912022. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Shanaida M, Lysiuk R, Mykhailenko O, Hudz
N, Abdulsalam A, Gontova T, Oleshchuk O, Ivankiv Y, Shanaida V,
Lytkin D and Bjørklund G: Alpha-lipoic Acid: An antioxidant with
anti-aging properties for disease therapy. Curr Med Chem. 32:23–54.
2025. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Maia LB, Maiti BK, Moura I and Moura JJG:
Selenium-more than just a fortuitous sulfur substitute in redox
biology. Molecules. 29:1202023. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Shin JY, Choi JW, Kim DG, Zhou ZQ, Shin
YK, Seo JH, Song HJ, Choi BM, Bae GS and Park SJ: Protective
effects of Coenzyme Q10 against acute pancreatitis. Int
Immunopharmacol. 88:1069002020. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Hou J, Fang F, Kang S, Wang Z and Yang Y:
Curcumin from Jianghuang (Rhizoma Curcumae Longae) protects against
exposure to ultraviolet B by antioxidation and attenuating
mitochondrion-dependent apoptosis. J Tradit Chin Med. 40:782–791.
2020.PubMed/NCBI
|
|
125
|
Yao J, Peng T, Shao C and Liu Y, Lin H and
Liu Y: The antioxidant action of astragali radix: Its active
components and molecular basis. Molecules. 29:16912024. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Zhao J, Zhang J, Liu Q, Wang Y, Jin Y,
Yang Y, Ni C and Zhang L: Hongjingtian injection protects against
myocardial ischemia reperfusion-induced apoptosis by blocking ROS
induced autophagic-flux. Biomed Pharmacother. 135:1112052021.
View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Shafabakhsh R, Mobini M, Raygan F,
Aghadavod E, Ostadmohammadi V, Amirani E, Mansournia MA and Asemi
Z: Curcumin administration and the effects on psychological status
and markers of inflammation and oxidative damage in patients with
type 2 diabetes and coronary heart disease. Clin Nutr ESPEN.
40:77–82. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
O'Connor EA, Evans CV, Ivlev I, Rushkin
MC, Thomas RG, Martin A and Lin JS: Vitamin and mineral supplements
for the primary prevention of cardiovascular disease and cancer:
Updated evidence report and systematic review for the US preventive
services task force. JAMA. 327:2334–2347. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Monsel A, Zhu YG, Gennai S, Hao Q, Liu J
and Lee JW: Cell-based therapy for acute organ injury: Preclinical
evidence and ongoing clinical trials using mesenchymal stem cells.
Anesthesiology. 121:1099–1121. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Matthay MA, Calfee CS, Zhuo H, Thompson
BT, Wilson JG, Levitt JE, Rogers AJ, Gotts JE, Wiener-Kronish JP,
Bajwa EK, et al: Treatment with allogeneic mesenchymal stromal
cells for moderate to severe acute respiratory distress syndrome
(START study): A randomised phase 2a safety trial. Lancet Respir
Med. 7:154–162. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Xu Q, Hou W, Zhao B, Fan P, Wang S, Wang L
and Gao J: Mesenchymal stem cells lineage and their role in disease
development. Mol Med. 30:2072024. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Muzes G and Sipos F: Mesenchymal stem
cell-derived secretome: A potential therapeutic option for
autoimmune and immune-mediated inflammatory diseases. Cells.
11:23002022. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Zhou T, Yuan Z, Weng J, Pei D, Du X, He C
and Lai P: Challenges and advances in clinical applications of
mesenchymal stromal cells. J Hematol Oncol. 14:242021. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Xu Z, Shi L, Wang Y, Zhang J, Huang L,
Zhang C, Liu S, Zhao P, Liu H, Zhu L, et al: Pathological findings
of COVID-19 associated with acute respiratory distress syndrome.
Lancet Respir Med. 8:420–422. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Mehta P, McAuley DF, Brown M, Sanchez E,
Tattersall RS and Manson JJ; HLH Across Speciality Collaboration
UK, : COVID-19: Consider cytokine storm syndromes and
immunosuppression. Lancet. 395:1033–1034. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Homma K, Bazhanov N, Hashimoto K, Shimizu
M, Heathman T, Hao Q, Nawgiri R, Muthukumarana V, Lee JW, Prough DS
and Enkhbaatar P: Mesenchymal stem cell-derived exosomes for
treatment of sepsis. Front Immunol. 14:11369642023. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Mastrolia I, Foppiani EM, Murgia A,
Candini O, Samarelli AV, Grisendi G, Veronesi E, Horwitz EM and
Dominici M: Challenges in clinical development of mesenchymal
stromal/stem cells: Concise review. Stem Cells Transl Med.
8:1135–1148. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Park WS, Ahn SY, Sung SI, Ahn JY and Chang
YS: Strategies to enhance paracrine potency of transplanted
mesenchymal stem cells in intractable neonatal disorders. Pediatr
Res. 83:214–222. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Kakabadze Z, Kipshidze N, Paresishvili T,
Kipshidze N, Vadachkoria Z and Chakhunashvili D: Human placental
mesenchymal stem cells for the treatment of ARDS in Rat. Stem Cells
Int. 2022:84185092022. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Pharoun J, Berro J, Sobh J, Abou-Younes
MM, Nasr L, Majed A, Khalil A, Joseph Stephan and Faour WH:
Mesenchymal stem cells biological and biotechnological advances:
Implications for clinical applications. Eur J Pharmacol.
977:1767192024. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Wang J, Huang R, Xu Q, Zheng G, Qiu G, Ge
M, Shu Q and Xu J: Mesenchymal stem cell-derived extracellular
vesicles alleviate acute lung injury via transfer of miR-27a-3p.
Crit Care Med. 48:e599–e610. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Murata M and Teshima T: Treatment of
steroid-refractory acute graft-versus-host disease using commercial
mesenchymal stem cell products. Front Immunol. 12:7243802021.
View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Levy O, Kuai R, Siren EMJ, Bhere D, Milton
Y, Nissar N, De Biasio M, Heinelt M, Reeve B, Abdi R, et al:
Shattering barriers toward clinically meaningful MSC therapies. Sci
Adv. 6:eaba68842020. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Shan Y, Zhang M, Tao E, Wang J, Wei N, Lu
Y, Liu Q, Hao K, Zhou F and Wang G: Pharmacokinetic characteristics
of mesenchymal stem cells in translational challenges. Signal
Transduct Target Ther. 9:2422024. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Cen M, Ouyang W, Zhang W, Yang L, Lin X,
Dai M, Hu H, Tang H, Liu H, Xia J and Xu F: MitoQ protects against
hyperpermeability of endothelium barrier in acute lung injury via a
Nrf2-dependent mechanism. Redox Biol. 41:1019362021. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Moslemi M, Hejazian SM, Shaddelan M,
Javanali F, Mirghaffari A, Sadeghi A, Valizadeh H, Sharifi A,
Haramshahi M, Ardalan M and Zununi Vahed S: Evaluating the effect
of Edaravone on clinical outcome of patients with severe COVID-19
admitted to ICU: A randomized clinical trial. Inflammopharmacology.
30:1277–1282. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Ding P, Yang R, Li C, Fu HL, Ren GL, Wang
P, Zheng DY, Chen W, Yang LY, Mao YF, et al: Fibroblast growth
factor 21 attenuates ventilator-induced lung injury by inhibiting
the NLRP3/caspase-1/GSDMD pyroptotic pathway. Crit Care.
27:1962023. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Gao J, Liu Q, Li J, Hu C, Zhao W, Ma W,
Yao M and Xing L: Fibroblast Growth Factor 21 dependent
TLR4/MYD88/NF-ĸB signaling activation is involved in
lipopolysaccharide-induced acute lung injury. Int Immunopharmacol.
80:1062192020. View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Yan F, Yuan L, Yang F, Wu G and Jiang X:
Emerging roles of fibroblast growth factor 21 in critical disease.
Front Cardiovasc Med. 9:10539972022. View Article : Google Scholar : PubMed/NCBI
|