|
1
|
Bodke H, Wagh V and Kakar G: Diabetes
mellitus and prevalence of other comorbid conditions: A systematic
review. Cureus. 15:e493742023.PubMed/NCBI
|
|
2
|
Sun H, Saeedi P, Karuranga S, Pinkepank M,
Ogurtsova K, Duncan BB, Stein C, Basit A, Chan JCN, Mbanya JC, et
al: IDF diabetes atlas: Global, regional and country-level diabetes
prevalence estimates for 2021 and projections for 2045. Diabetes
Res Clin Pract. 183:1091192022. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
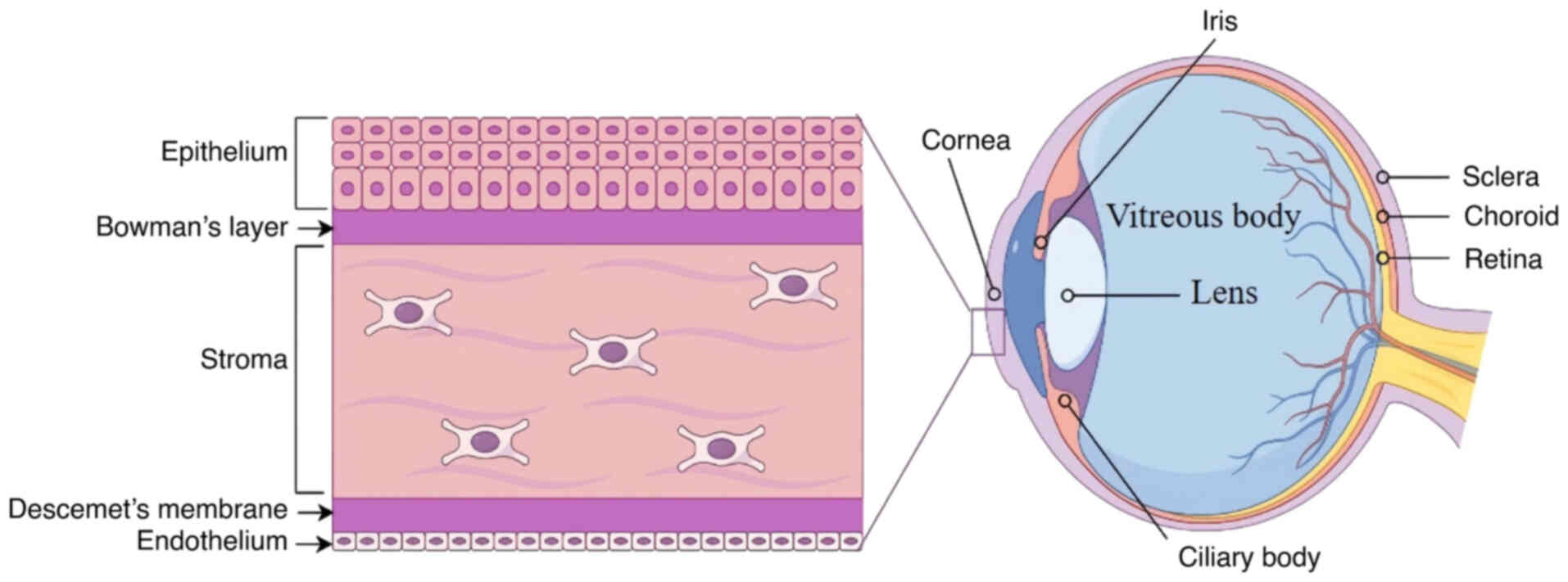
Cole JB and Florez JC: Genetics of
diabetes mellitus and diabetes complications. Nat Rev Nephrol.
16:377–390. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zhu L, Titone R and Robertson DM: The
impact of hyperglycemia on the corneal epithelium: Molecular
mechanisms and insight. Ocul Surf. 17:644–654. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhao H, He Y, Ren YR and Chen BH: Corneal
alteration and pathogenesis in diabetes mellitus. Int J Ophthalmol.
12:1939–1950. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lyu Y, Zeng X, Li F and Zhao S: The effect
of the duration of diabetes on dry eye and corneal nerves. Cont
Lens Anterior Eye. 42:380–385. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Teo ZL, Tham YC, Yu M, Chee ML, Rim TH,
Cheung N, Bikbov MM, Wang YX, Tang Y, Lu Y, et al: Global
prevalence of diabetic retinopathy and projection of burden through
2045: Systematic review and meta-analysis. Ophthalmology.
128:1580–1591. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Priyadarsini S, Whelchel A, Nicholas S,
Sharif R, Riaz K and Karamichos D: Diabetic keratopathy: Insights
and challenges. Surv Ophthalmol. 65:513–529. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Han SB, Yang HK and Hyon JY: Influence of
diabetes mellitus on anterior segment of the eye. Clin Interv
Aging. 14:53–63. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Buonfiglio F, Wasielica-Poslednik J,
Pfeiffer N and Gericke A: Diabetic keratopathy: Redox signaling
pathways and therapeutic prospects. Antioxidants (Basel).
13:1202024. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pelley JW: 17-Protein synthesis and
degradation. Elsevier's Integrated Biochemistry. Pelley JW: Mosby,
Philadelphia: pp. 147–158. 2007, View Article : Google Scholar
|
|
12
|
Goodman SR: Chapter 5-regulation of gene
expression. Medical Cell Biology. (Third Edition). Goodman SR:
Academic Press; San Diego, CA: pp. 149–190. 2008
|
|
13
|
Bernhofer M, Goldberg T, Wolf S, Ahmed M,
Zaugg J, Boden M and Rost B: NLSdb-major update for database of
nuclear localization signals and nuclear export signals. Nucleic
Acids Res. 46:D503–D508. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Li W and Jiang H: Nuclear protein
condensates and their properties in regulation of gene expression.
J Mol Biol. 434:1671512022. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Escandon P, Vasini B, Whelchel AE,
Nicholas SE, Matlock HG, Ma JX and Karamichos D: The role of
peroxisome proliferator-activated receptors in healthy and diseased
eyes. Exp Eye Res. 208:1086172021. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Khatol P, Saraf S and Jain A: Peroxisome
proliferated activated receptors (PPARs): Opportunities and
challenges for ocular therapy. Crit Rev Ther Drug Carrier Syst.
35:65–97. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hou Y, Lan J, Zhang F and Wu X: Expression
profiles and potential corneal epithelial wound healing regulation
targets of high-mobility group box 1 in diabetic mice. Exp Eye Res.
202:1083642021. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Peng Y, Bui CH, Zhang XJ, Chen JS, Tham
CC, Chu WK, Chen LJ, Pang CP and Yam JC: The role of EZH2 in ocular
diseases: A narrative review. Epigenomics. 15:557–570. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rocher N: Anatomy and physiology of the
human eye. Soins. 30–31. 2010.(In French). PubMed/NCBI
|
|
20
|
Mobaraki M, Abbasi R, Omidian Vandchali S,
Ghaffari M, Moztarzadeh F and Mozafari M: Corneal repair and
regeneration: Current concepts and future directions. Front Bioeng
Biotechnol. 7:1352019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Meek KM and Knupp C: Corneal structure and
transparency. Prog Retin Eye Res. 49:1–16. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lavker RM, Kaplan N, Wang J and Peng H:
Corneal epithelial biology: Lessons stemming from old to new. Exp
Eye Res. 198:1080942020. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Doughty MJ and Jonuscheit S: Corneal
structure, transparency, thickness and optical density
(densitometry), especially as relevant to contact lens wear-a
review. Cont Lens Anterior Eye. 42:238–245. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Luke RA, Braun RJ, Driscoll TA, Begley CG
and Awisi-Gyau D: Parameter estimation for evaporation-driven tear
film thinning. Bull Math Biol. 82:712020. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Braun RJ, King-Smith PE, Begley CG, Li L
and Gewecke NR: Dynamics and function of the tear film in relation
to the blink cycle. Prog Retin Eye Res. 45:132–164. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wilson SL, El Haj AJ and Yang Y: Control
of scar tissue formation in the cornea: Strategies in clinical and
corneal tissue engineering. J Funct Biomater. 3:642–687. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Melnyk S and Bollag WB: Aquaporins in the
cornea. Int J Mol Sci. 25:37482024. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Sridhar MS: Anatomy of cornea and ocular
surface. Indian J Ophthalmol. 66:190–194. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wilson SE: Bowman's layer in the
cornea-structure and function and regeneration. Exp Eye Res.
195:1080332020. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
DelMonte DW and Kim T: Anatomy and
physiology of the cornea. J Cataract Refract Surg. 37:588–598.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Hassell JR and Birk DE: The molecular
basis of corneal transparency. Exp Eye Res. 91:326–335. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Marfurt CF, Cox J, Deek S and Dvorscak L:
Anatomy of the human corneal innervation. Exp Eye Res. 90:478–492.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
de Oliveira RC and Wilson SE: Descemet's
membrane development, structure, function and regeneration. Exp Eye
Res. 197:1080902020. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Ljubimov AV: Diabetic complications in the
cornea. Vision Res. 139:138–152. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Mukhija R, Gupta N, Vashist P, Tandon R
and Gupta SK: Population-based assessment of visual impairment and
pattern of corneal disease: Results from the CORE (corneal opacity
rural epidemiological) study. Br J Ophthalmol. 104:994–998. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Chang YS, Tai MC, Ho CH, Chu CC, Wang JJ,
Tseng SH and Jan RL: Risk of corneal ulcer in patients with
diabetes mellitus: A retrospective large-scale cohort study. Sci
Rep. 10:73882020. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Yeung A and Dwarakanathan S: Diabetic
keratopathy. Dis Mon. 67:1011352021. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Huang C, Liao R, Wang F and Tang S:
Characteristics of reconstituted tight junctions after corneal
epithelial wounds and ultrastructure alterations of corneas in type
2 diabetic rats. Curr Eye Res. 41:783–790. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Shih KC, Lam KS and Tong L: A systematic
review on the impact of diabetes mellitus on the ocular surface.
Nutr Diabetes. 7:e2512017. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Alfuraih S, Barbarino A, Ross C, Shamloo
K, Jhanji V, Zhang M and Sharma A: Effect of high glucose on ocular
surface epithelial cell barrier and tight junction proteins. Invest
Ophthalmol Vis Sci. 61:32020. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Liu T, Sun DP, Li DF, Bi WJ and Xie LX:
Observation and quantification of diabetic keratopathy in type 2
diabetes patients using in vivo laser confocal microscopy. Zhonghua
Yan Ke Za Zhi. 56:754–760. 2020.(In Chinese). PubMed/NCBI
|
|
42
|
Xu KP, Li Y, Ljubimov AV and Yu FS: High
glucose suppresses epidermal growth factor
receptor/phosphatidylinositol 3-kinase/Akt signaling pathway and
attenuates corneal epithelial wound healing. Diabetes.
58:1077–1085. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Lan X, Zhang W, Zhu J, Huang H, Mo K, Guo
H, Zhu L, Liu J, Li M, Wang L, et al: dsRNA induced IFNβ-MMP13 axis
drives corneal wound healing. Invest Ophthalmol Vis Sci. 63:142022.
View Article : Google Scholar
|
|
44
|
Di G, Du X, Qi X, Zhao X, Duan H, Li S,
Xie L and Zhou Q: Mesenchymal stem cells promote diabetic corneal
epithelial wound healing through TSG-6-dependent stem cell
activation and macrophage switch. Invest Ophthalmol Vis Sci.
58:4344–4354. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Bikbova G, Oshitari T, Baba T, Bikbov M
and Yamamoto S: Diabetic corneal neuropathy: Clinical perspectives.
Clin Ophthalmol. 12:981–987. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Liu YC, Lin MT and Mehta JS: Analysis of
corneal nerve plexus in corneal confocal microscopy images. Neural
Regen Res. 16:690–691. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Kaplan H, Yüzbaşıoğlu S, Vural G and
Gümüşyayla Ş: Investigation of small fiber neuropathy in patients
with diabetes mellitus by corneal confocal microscopy. Neurophysiol
Clin. 54:1029552024. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Mokhtar SBA, van der Heide FCT, Oyaert
KAM, van der Kallen CJH, Berendschot TTJM, Scarpa F, Colonna A, de
Galan BE, van Greevenbroek MMJ, Dagnelie PC, et al: (Pre)diabetes
and a higher level of glycaemic measures are continuously
associated with corneal neurodegeneration assessed by corneal
confocal microscopy: The maastricht study. Diabetologia.
66:2030–2041. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Carmichael J, Fadavi H, Ishibashi F,
Howard S, Boulton AJM, Shore AC and Tavakoli M: Implementation of
corneal confocal microscopy for screening and early detection of
diabetic neuropathy in primary care alongside retinopathy
screening: Results from a feasibility study. Front Endocrinol
(Lausanne). 13:e8915752022. View Article : Google Scholar
|
|
50
|
Banerjee M, Mukhopadhyay P and Ghosh S,
Basu M, Pandit A, Malik R and Ghosh S: Corneal confocal microscopy
abnormalities in children and adolescents with type 1 diabetes.
Endocr Pract. 29:692–698. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
De Clerck EEB, Schouten JSAG, Berendschot
TTJM, Koolschijn RS, Nuijts RMMA, Schram MT, Schaper NC, Henry RMA,
Dagnelie PC, Ruggeri A, et al: Reduced corneal nerve fibre length
in prediabetes and type 2 diabetes: The maastricht study. Acta
Ophthalmol. 98:485–491. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Mvilongo C, Akono ME, Nkoudou D, Nanfack
C, Nomo A, Dim R and Eballé AO: Clinical profile of corneal
sensitivity in diabetic patients: A case-control study. J Fr
Ophtalmol. 47:1042122024. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Schiano Lomoriello D, Abicca I, Parravano
M, Giannini D, Russo B, Frontoni S and Picconi F: Early alterations
of corneal subbasal plexus in uncomplicated type 1 diabetes
patients. J Ophthalmol. 2019:98182172019. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Torricelli AA and Wilson SE: Cellular and
extracellular matrix modulation of corneal stromal opacity. Exp Eye
Res. 129:151–160. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Priyadarsini S, McKay TB, Sarker-Nag A,
Allegood J, Chalfant C, Ma JX and Karamichos D: Complete metabolome
and lipidome analysis reveals novel biomarkers in the human
diabetic corneal stroma. Exp Eye Res. 153:90–100. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Sinha NR, Balne PK, Bunyak F, Hofmann AC,
Lim RR, Mohan RR and Chaurasia SS: Collagen matrix perturbations in
corneal stroma of Ossabaw mini pigs with type 2 diabetes. Mol Vis.
27:666–678. 2021.PubMed/NCBI
|
|
57
|
Kalteniece A, Ferdousi M, Azmi S, Marshall
A, Soran H and Malik RA: Keratocyte density is reduced and related
to corneal nerve damage in diabetic neuropathy. Invest Ophthalmol
Vis Sci. 59:3584–3590. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Gad H, Al-Jarrah B, Saraswathi S, Mohamed
S, Kalteniece A, Petropoulos IN, Khan A, Ponirakis G, Singh P,
Khodor SA, et al: Corneal confocal microscopy identifies a
reduction in corneal keratocyte density and sub-basal nerves in
children with type 1 diabetes mellitus. Br J Ophthalmol.
106:1368–1372. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Eghrari AO, Riazuddin SA and Gottsch JD:
Overview of the cornea: Structure, function, and development. Prog
Mol Biol Transl Sci. 134:7–23. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
El-Agamy A and Alsubaie S: Corneal
endothelium and central corneal thickness changes in type 2
diabetes mellitus. Clin Ophthalmol. 11:481–486. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Goldstein AS, Janson BJ, Skeie JM, Ling JJ
and Greiner MA: The effects of diabetes mellitus on the corneal
endothelium: A review. Surv Ophthalmol. 65:438–450. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Yalcın SO, Kaplan AT and Sobu E: Corneal
endothelial cell morphology and optical coherence tomography
findings in children with type 1 diabetes mellitus. Eur J
Ophthalmol. 33:1331–1339. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Amador-Muñoz DP, Conforti V, Matheus LM,
Molano-Gonzalez N and Payán-Gómez C: Diabetes mellitus type 1 has a
higher impact on corneal endothelial cell density and pachymetry
than diabetes mellitus type 2, independent of age: A
meta-regression model. Cornea. 41:965–973. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Chowdhury B, Bhadra S, Mittal P and Shyam
K: Corneal endothelial morphology and central corneal thickness in
type 2 diabetes mellitus patients. Indian J Ophthalmol.
69:1718–1724. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Kim YJ and Kim TG: The effects of type 2
diabetes mellitus on the corneal endothelium and central corneal
thickness. Sci Rep. 11:83242021. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Taşlı NG, Icel E, Karakurt Y, Ucak T,
Ugurlu A, Yilmaz H and Akbas EM: The findings of corneal specular
microscopy in patients with type-2 diabetes mellitus. BMC
Ophthalmol. 20:2142020. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Zhang K, Zhao L, Zhu C, Nan W, Ding X,
Dong Y and Zhao M: The effect of diabetes on corneal endothelium: A
meta-analysis. BMC Ophthalmol. 21:782021. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Papadakou P, Chatziralli I, Papathanassiou
M, Lambadiari V, Siganos CS, Theodossiadis P and Kozobolis V: The
effect of diabetes mellitus on corneal endothelial cells and
central corneal thickness: A case-control study. Ophthalmic Res.
63:550–554. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Sekimoto T and Yoneda Y: Intrinsic and
extrinsic negative regulators of nuclear protein transport
processes. Genes Cells. 17:525–535. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Cronshaw JM, Krutchinsky AN, Zhang W,
Chait BT and Matunis MJ: Proteomic analysis of the mammalian
nuclear pore complex. J Cell Biol. 158:915–927. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Jeon P, Ham HJ, Park S and Lee JA:
Regulation of cellular ribonucleoprotein granules: From assembly to
degradation via post-translational modification. Cells.
11:20632022. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Shen F, Kirmani KZ, Xiao Z, Thirlby BH,
Hickey RJ and Malkas LH: Nuclear protein isoforms: Implications for
cancer diagnosis and therapy. J Cell Biochem. 112:756–760. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Simon JA and Lange CA: Roles of the EZH2
histone methyltransferase in cancer epigenetics. Mutat Res.
647:21–29. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Glancy E, Ciferri C and Bracken AP:
Structural basis for PRC2 engagement with chromatin. Curr Opin
Struct Biol. 67:135–144. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Khan NH, Chen HJ, Fan Y, Surfaraz M,
Ahammad MF, Qin YZ, Shahid M, Virk R, Jiang E, Wu DD and Ji XY:
Biology of PEST-containing nuclear protein: A potential molecular
target for cancer research. Front Oncol. 12:7845972022. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Brown JD and Plutzky J: Peroxisome
proliferator-activated receptors as transcriptional nodal points
and therapeutic targets. Circulation. 115:518–533. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Chow BJ, Lee IXY, Liu C and Liu YC:
Potential therapeutic effects of peroxisome proliferator-activated
receptors on corneal diseases. Exp Biol Med (Maywood).
249:101422024. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Kim IS, Silwal P and Jo EK: Peroxisome
proliferator-activated receptor-targeted therapies: Challenges upon
infectious diseases. Cells. 12:6502023. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Mirza AZ, Althagafi II and Shamshad H:
Role of PPAR receptor in different diseases and their ligands:
Physiological importance and clinical implications. Eur J Med Chem.
166:502–513. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Jain N, Bhansali S, Kurpad AV, Hawkins M,
Sharma A, Kaur S, Rastogi A and Bhansali A: Effect of a dual PPAR
α/γ agonist on insulin sensitivity in patients of type 2 diabetes
with hypertriglyceridemia-randomized double-blind
placebo-controlled trial. Sci Rep. 9:190172019. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Lin Y, Wang Y and Li PF: PPARα: An
emerging target of metabolic syndrome, neurodegenerative and
cardiovascular diseases. Front Endocrinol (Lausanne).
13:10749112022. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Hu P, Li K, Peng X, Kan Y, Li H, Zhu Y,
Wang Z, Li Z, Liu HY and Cai D: Nuclear receptor PPARα as a
therapeutic target in diseases associated with lipid metabolism
disorders. Nutrients. 15:47722023. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Matlock HG, Qiu F, Malechka V, Zhou K,
Cheng R, Benyajati S, Whelchel A, Karamichos D and Ma JX:
Pathogenic role of PPARα downregulation in corneal nerve
degeneration and impaired corneal sensitivity in diabetes.
Diabetes. 69:1279–1291. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Liang W, Huang L, Whelchel A, Yuan T, Ma
X, Cheng R, Takahashi Y, Karamichos D and Ma JX: Peroxisome
proliferator-activated receptor-α (PPARα) regulates wound healing
and mitochondrial metabolism in the cornea. Proc Natl Acad Sci USA.
120:e22175761202023. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Teo CHY, Lin MT, Lee IXY, Koh SK, Zhou L,
Goh DS, Choi H, Koh HWL, Lam AYR, Lim PS, et al: Oral peroxisome
proliferator-activated receptor-α agonist enhances corneal nerve
regeneration in patients with type 2 diabetes. Diabetes.
72:932–946. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Mansoor H, Lee IXY, Lin MT, Ang HP, Xue
YC, Krishaa L, Patil M, Koh SK, Tan HC, Zhou L and Liu YC: Topical
and oral peroxisome proliferator-activated receptor-α agonist
ameliorates diabetic corneal neuropathy. Sci Rep. 14:134352024.
View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Jeon KI, Kulkarni A, Woeller CF, Phipps
RP, Sime PJ, Hindman HB and Huxlin KR: Inhibitory effects of PPARγ
ligands on TGF-β1-induced corneal myofibroblast transformation. Am
J Pathol. 184:1429–4145. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Jeon KI, Phipps RP, Sime PJ and Huxlin KR:
Inhibitory effects of PPARγ ligands on TGF-β1-induced CTGF
expression in cat corneal fibroblasts. Exp Eye Res. 138:52–58.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Wang J, Chen S, Zhao X, Guo Q, Yang R,
Zhang C, Huang Y, Ma L and Zhao S: Effect of PPARγ on oxidative
stress in diabetes-related dry eye. Exp Eye Res. 231:1094982023.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Tobita Y, Arima T, Nakano Y, Uchiyama M,
Shimizu A and Takahashi H: Peroxisome proliferator-activated
receptor beta/delta agonist suppresses inflammation and promotes
neovascularization. Int J Mol Sci. 21:52962020. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Goodwin GH and Johns EW: Isolation and
characterisation of two calf-thymus chromatin non-histone proteins
with high contents of acidic and basic amino acids. Eur J Biochem.
40:215–219. 1973. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Thomas JO and Stott K: H1 and HMGB1:
Modulators of chromatin structure. Biochem Soc Trans. 40:341–346.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Kang R, Chen R, Zhang Q, Hou W, Wu S, Cao
L, Huang J, Yu Y, Fan XG, Yan Z, et al: HMGB1 in health and
disease. Mol Aspects Med. 40:1–116. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Bell CW, Jiang W, Reich CF III and
Pisetsky DS: The extracellular release of HMGB1 during apoptotic
cell death. Am J Physiol Cell Physiol. 291:C1318–C1325. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
95
|
van Beijnum JR, Buurman WA and Griffioen
AW: Convergence and amplification of toll-like receptor (TLR) and
receptor for advanced glycation end products (RAGE) signaling
pathways via high mobility group B1 (HMGB1). Angiogenesis.
11:91–99. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Zhang S, Zhong J, Yang P, Gong F and Wang
CY: HMGB1, an innate alarmin, in the pathogenesis of type 1
diabetes. Int J Clin Exp Pathol. 3:24–38. 2009.PubMed/NCBI
|
|
97
|
Lotze MT and Tracey KJ: High-mobility
group box 1 protein (HMGB1): Nuclear weapon in the immune arsenal.
Nat Rev Immunol. 5:331–342. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Taniguchi N, Kawahara K, Yone K,
Hashiguchi T, Yamakuchi M, Goto M, Inoue K, Yamada S, Ijiri K,
Matsunaga S, et al: High mobility group box chromosomal protein 1
plays a role in the pathogenesis of rheumatoid arthritis as a novel
cytokine. Arthritis Rheum. 48:971–981. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Dasu MR, Devaraj S, Park S and Jialal I:
Increased toll-like receptor (TLR) activation and TLR ligands in
recently diagnosed type 2 diabetic subjects. Diabetes Care.
33:861–868. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Skrha J Jr, Kalousová M, Svarcová J,
Muravská A, Kvasnička J, Landová L, Zima T and Skrha J:
Relationship of soluble RAGE and RAGE ligands HMGB1 and EN-RAGE to
endothelial dysfunction in type 1 and type 2 diabetes mellitus. Exp
Clin Endocrinol Diabetes. 120:277–281. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Wu H, Chen Z, Xie J, Kang LN, Wang L and
Xu B: High mobility group box-1: A missing link between diabetes
and its complications. Mediators Inflamm. 2016:38961472016.
View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Steinle JJ: Role of HMGB1 signaling in the
inflammatory process in diabetic retinopathy. Cell Signal.
73:1096872020. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Feng L, Liang L, Zhang S, Yang J, Yue Y
and Zhang X: HMGB1 downregulation in retinal pigment epithelial
cells protects against diabetic retinopathy through the
autophagy-lysosome pathway. Autophagy. 18:320–339. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Guo X, Shi Y, Du P, Wang J, Han Y, Sun B
and Feng J: HMGB1/TLR4 promotes apoptosis and reduces autophagy of
hippocampal neurons in diabetes combined with OSA. Life Sci.
239:1170202019. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Hou Y, Xin M, Li Q and Wu X: Glycyrrhizin
micelle as a genistein nanocarrier: Synergistically promoting
corneal epithelial wound healing through blockage of the HMGB1
signaling pathway in diabetic mice. Exp Eye Res. 204:1084542021.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Liu Y and Yang Q: The roles of EZH2 in
cancer and its inhibitors. Med Oncol. 40:1672023. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Cao J, Pontes KC, Heijkants RC, Brouwer
NJ, Groenewoud A, Jordanova ES, Marinkovic M, van Duinen S,
Teunisse AF, Verdijk RM, et al: Overexpression of EZH2 in
conjunctival melanoma offers a new therapeutic target. J Pathol.
245:433–444. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Lin Y, Su H, Zou B and Huang M: EZH2
promotes corneal endothelial cell apoptosis by mediating H3K27me3
and inhibiting HO-1 transcription. Curr Eye Res. 48:1122–1132.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Zhang L, Wang L, Hu XB, Hou M, Xiao Y,
Xiang JW, Xie J, Chen ZG, Yang TH, Nie Q, et al: MYPT1/PP1-mediated
EZH2 dephosphorylation at S21 promotes epithelial-mesenchymal
transition in fibrosis through control of multiple families of
genes. Adv Sci (Weinh). 9:e21055392022. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Thomas AA, Feng B and Chakrabarti S:
ANRIL: A regulator of VEGF in diabetic retinopathy. Invest
Ophthalmol Vis Sci. 58:470–480. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Wilson SE: Corneal myofibroblasts and
fibrosis. Exp Eye Res. 201:1082722020. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Liao K, Cui Z, Zeng Y, Liu J, Wang Y, Wang
Z, Tang S and Chen J: Inhibition of enhancer of zeste homolog 2
prevents corneal myofibroblast transformation in vitro. Exp Eye
Res. 208:1086112021. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Wan SS, Pan YM, Yang WJ, Rao ZQ and Yang
YN: Inhibition of EZH2 alleviates angiogenesis in a model of
corneal neovascularization by blocking FoxO3a-mediated oxidative
stress. FASEB J. 34:10168–10181. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Duraisamy AJ, Mishra M and Kowluru RA:
Crosstalk between histone and DNA methylation in regulation of
retinal matrix metalloproteinase-9 in diabetes. Invest Ophthalmol
Vis Sci. 58:6440–6448. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Liu T, Wang Y, Wang Y and Chan AM:
Multifaceted regulation of PTEN subcellular distributions and
biological functions. Cancers (Basel). 11:12472019. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Ho J, Cruise ES, Dowling RJO and Stambolic
V: PTEN nuclear functions. Cold Spring Harb Perspect Med.
10:a0360792020. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Li A, Qiu M, Zhou H, Wang T and Guo W:
PTEN, insulin resistance and cancer. Curr Pharm Des. 23:3667–3676.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Liu A, Zhu Y, Chen W, Merlino G and Yu Y:
PTEN dual lipid- and protein-phosphatase function in tumor
progression. Cancers (Basel). 14:36662022. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Li X, Yang P, Hou X and Ji S:
Post-translational modification of PTEN protein: Quantity and
activity. Oncol Rev. 18:14302372024. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Li YZ, Di Cristofano A and Woo M:
Metabolic role of PTEN in insulin signaling and resistance. Cold
Spring Harb Perspect Med. 10:a0361372020. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
D'Amico AG, Maugeri G, Magrì B, Bucolo C
and D'Agata V: Targeting the PINK1/Parkin pathway: A new
perspective in the prevention and therapy of diabetic retinopathy.
Exp Eye Res. 247:1100242024. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Dai Y, Zhao X, Chen P, Yu Y, Wang Y and
Xie L: Neuropeptide FF promotes recovery of corneal nerve injury
associated with hyperglycemia. Invest Ophthalmol Vis Sci.
56:7754–7765. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Li J, Qi X, Wang X, Li W, Li Y and Zhou Q:
PTEN inhibition facilitates diabetic corneal epithelial
regeneration by reactivating Akt signaling pathway. Transl Vis Sci
Technol. 9:52020. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Zhang W, Yu F, Yan C, Shao C, Gu P, Fu Y,
Sun H and Fan X: PTEN inhibition accelerates corneal endothelial
wound healing through increased endothelial cell division and
migration. Invest Ophthalmol Vis Sci. 61:192020. View Article : Google Scholar
|
|
125
|
Liu X, Li X, Wu G, Qi P, Zhang Y, Liu Z,
Li X, Yu Y, Ye X, Li Y, et al: Umbilical cord mesenchymal stem
cell-derived small extracellular vesicles deliver miR-21 to promote
corneal epithelial wound healing through PTEN/PI3K/Akt pathway.
Stem Cells Int. 2022:12525572022. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Penteado AB, Hassanie H, Gomes RA, Silva
Emery FD and Goulart Trossini GH: Human sirtuin 2 inhibitors, their
mechanisms and binding modes. Future Med Chem. 15:291–311. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Vassilopoulos A, Fritz KS, Petersen DR and
Gius D: The human sirtuin family: Evolutionary divergences and
functions. Hum Genomics. 5:485–496. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Wu QJ, Zhang TN, Chen HH, Yu XF, Lv JL,
Liu YY, Liu YS, Zheng G, Zhao JQ, Wei YF, et al: The sirtuin family
in health and disease. Signal Transduct Target Ther. 7:4022022.
View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Tao Z, Jin Z, Wu J, Cai G and Yu X:
Sirtuin family in autoimmune diseases. Front Immunol.
14:11862312023. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Guarente L: Franklin H: Epstein lecture:
Sirtuins, aging, and medicine. N Engl J Med. 364:2235–2244. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Hong Q, Zhang L, Das B, Li Z, Liu B, Cai
G, Chen X, Chuang PY, He JC and Lee K: Increased podocyte Sirtuin-1
function attenuates diabetic kidney injury. Kidney Int.
93:1330–1343. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Hammer SS, Vieira CP, McFarland D, Sandler
M, Levitsky Y, Dorweiler TF, Lydic TA, Asare-Bediako B,
Adu-Agyeiwaah Y, Sielski MS, et al: Fasting and fasting-mimicking
treatment activate SIRT1/LXRα and alleviate diabetes-induced
systemic and microvascular dysfunction. Diabetologia. 64:1674–1689.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Chandrasekaran K, Salimian M, Konduru SR,
Choi J, Kumar P, Long A, Klimova N, Ho CY, Kristian T and Russell
JW: Overexpression of Sirtuin 1 protein in neurons prevents and
reverses experimental diabetic neuropathy. Brain. 142:3737–3752.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Li L, Zeng H, He X and Chen JX: Sirtuin 3
alleviates diabetic cardiomyopathy by regulating TIGAR and
cardiomyocyte metabolism. J Am Heart Assoc. 10:e0189132021.
View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Zhao K, Zhang H and Yang D: SIRT1 exerts
protective effects by inhibiting endoplasmic reticulum stress and
NF-κB signaling pathways. Front Cell Dev Biol. 12:14055462024.
View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Mihanfar A, Akbarzadeh M, Ghazizadeh
Darband S, Sadighparvar S and Majidinia M: SIRT1: A promising
therapeutic target in type 2 diabetes mellitus. Arch Physiol
Biochem. 130:13–28. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Prabhakar PK, Singh K, Kabra D and Gupta
J: Natural SIRT1 modifiers as promising therapeutic agents for
improving diabetic wound healing. Phytomedicine. 76:1532522020.
View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Nebbioso M, Lambiase A, Armentano M,
Tucciarone G, Sacchetti M, Greco A and Alisi L: Diabetic
retinopathy, oxidative stress, and sirtuins: An in depth look in
enzymatic patterns and new therapeutic horizons. Surv Ophthalmol.
67:168–183. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Wei S, Fan J, Zhang X, Jiang Y, Zeng S,
Pan X, Sheng M and Chen Y: Sirt1 attenuates diabetic keratopathy by
regulating the endoplasmic reticulum stress pathway. Life Sci.
265:1187892021. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Wang Y, Zhao X, Wu X, Dai Y, Chen P and
Xie L: microRNA-182 mediates Sirt1-induced diabetic corneal nerve
regeneration. Diabetes. 65:2020–2031. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Hu J, Kan T and Hu X: Sirt3 regulates
mitophagy level to promote diabetic corneal epithelial wound
healing. Exp Eye Res. 181:223–231. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Zhang B, Cui S, Bai X, Zhuo L, Sun X, Hong
Q, Fu B, Wang J, Chen X and Cai G: SIRT3 overexpression antagonizes
high glucose accelerated cellular senescence in human diploid
fibroblasts via the SIRT3-FOXO1 signaling pathway. Age (Dordr).
35:2237–2253. 2013. View Article : Google Scholar : PubMed/NCBI
|