Introduction
Myoepithelial carcinoma is a rare, locally
aggressive, malignant neoplasm that shows exclusive or prominent
myoepithelial cell differentiation (1). Its histopathological features,
immunohistochemical profile and clinical behavior remain to be
delineated and are characterized by a wide range of cytomorphologic
features, such as epithelioid, plasmacytoid, spindle and clear cell
types, rendering a diagnosis difficult. This entity was initially
described in the salivary glands (2). However, it was also identified in the
breast, upper aerodigestive tract, skin and other soft tissues
(3).
Current observations of this entity showed its
invasive behavior as being more infiltrative and metastatic, unlike
previous predictions of low-grade malignancy (4). The rate of recurrence and metastasis
accounts for approximately 60% (3).
Only limited reports on its metastatic behavior are available in
the literature. The metastatic sites included the lungs, kidneys,
cervical lymph nodes, brain, ribs and the scalp (3,5). This
study presents a case of metastatic myoepithelial carcinoma of the
thyroid from the parotid gland, which was not found in the updated
review of the literature. Immunochemical studies are crucial in
order to confirm myoepithelial differentiation of tumor cells.
Knowledge of the clinical history, radiographic characterization
and morphological correlation with the primary tumor are
emphasized.
Patient and methods
Clinical history of patient
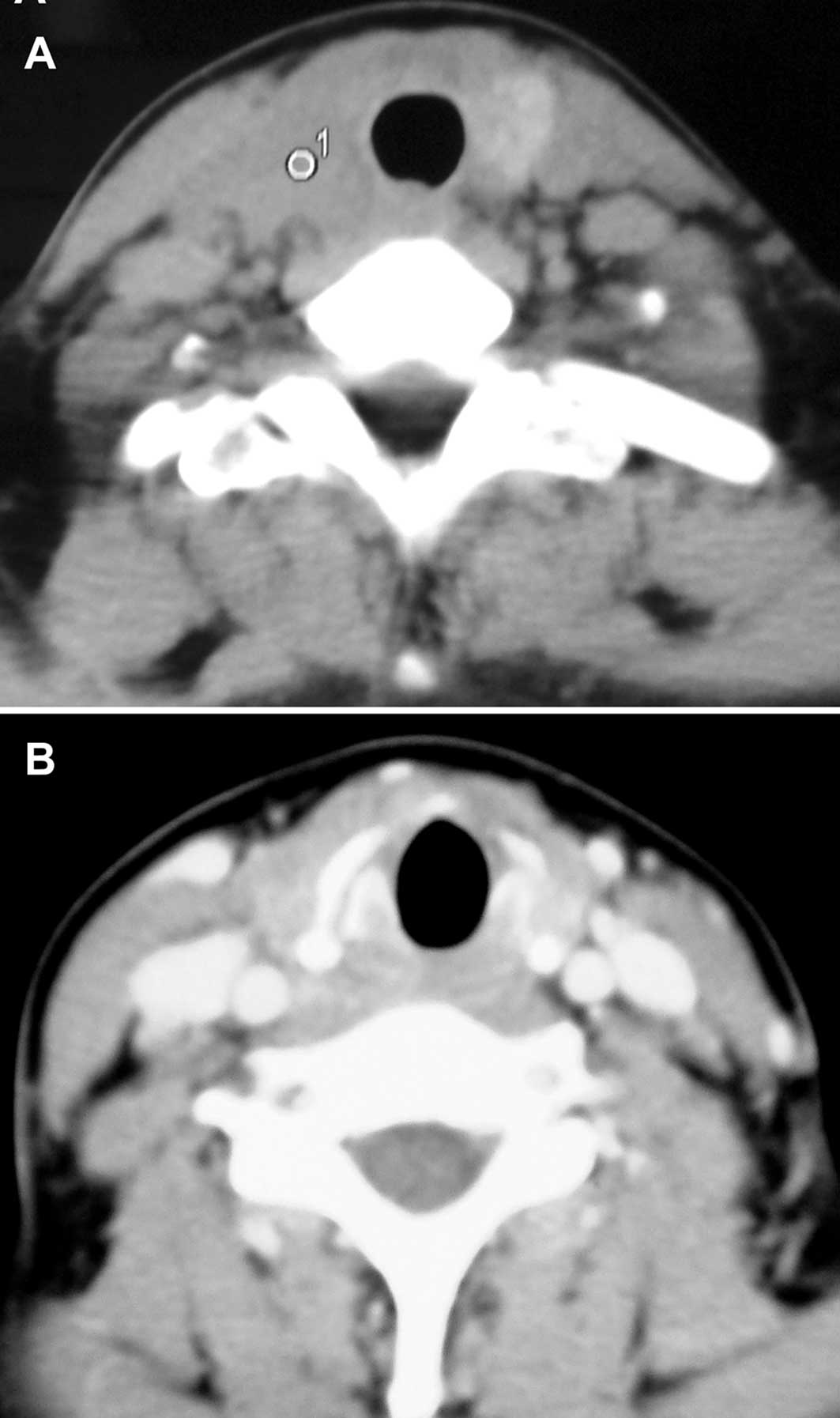
A CT scan (Fig. 1)
revealed that a 39-year-old Chinese female had a 3.3 cm solid mass
in her thyroid, mainly located in the right lobe with bilateral
cervical lymph node enlargement, in March 10, 2010. This occurred
21 months following total resection of the right parotid gland. In
June 2008, the patient had undergone surgery on the right salivary
gland tumor, pathologically diagnosed as ‘the basal cell
adenocarcinoma’. The patient then received local 125I
radioactive bead implantation one month after the operation.
Approximately 12 months later, a soybean-sized tumor appeared on
her neck, followed by dysphagia and hoarseness with thyroid
enlargement. A neck CT examination was performed in March 10, 2010,
showing the thyroid gland and right cervical lymph node
enlargement, with no abnormality in the parotid region. A bilateral
neck dissection with a total right and partial left thyroidectomy
were concomitantly performed. An intraoperative dissection showed
the bilateral cervical lymph nodes and thyroid glands to be
involved, with the former being swollen, solid and showing invasion
into the surrounding tissue, and the latter, particularly the right
lobe, having an indefinite boundary with the surrounding tissue. A
myoepithelial carcinoma was pathologically diagnosed in the lymph
nodes and thyroid postoperatively. Full consent was obtained by the
patient.
Methods
The specimens were routinely processed and stained
with hematoxylin and eosin (H&E). Immunohistochemical staining
for CK5, CK18, p63, Calponin, Ki-67 and S-100 was performed using
standard avidin-biotin techniques.
Results
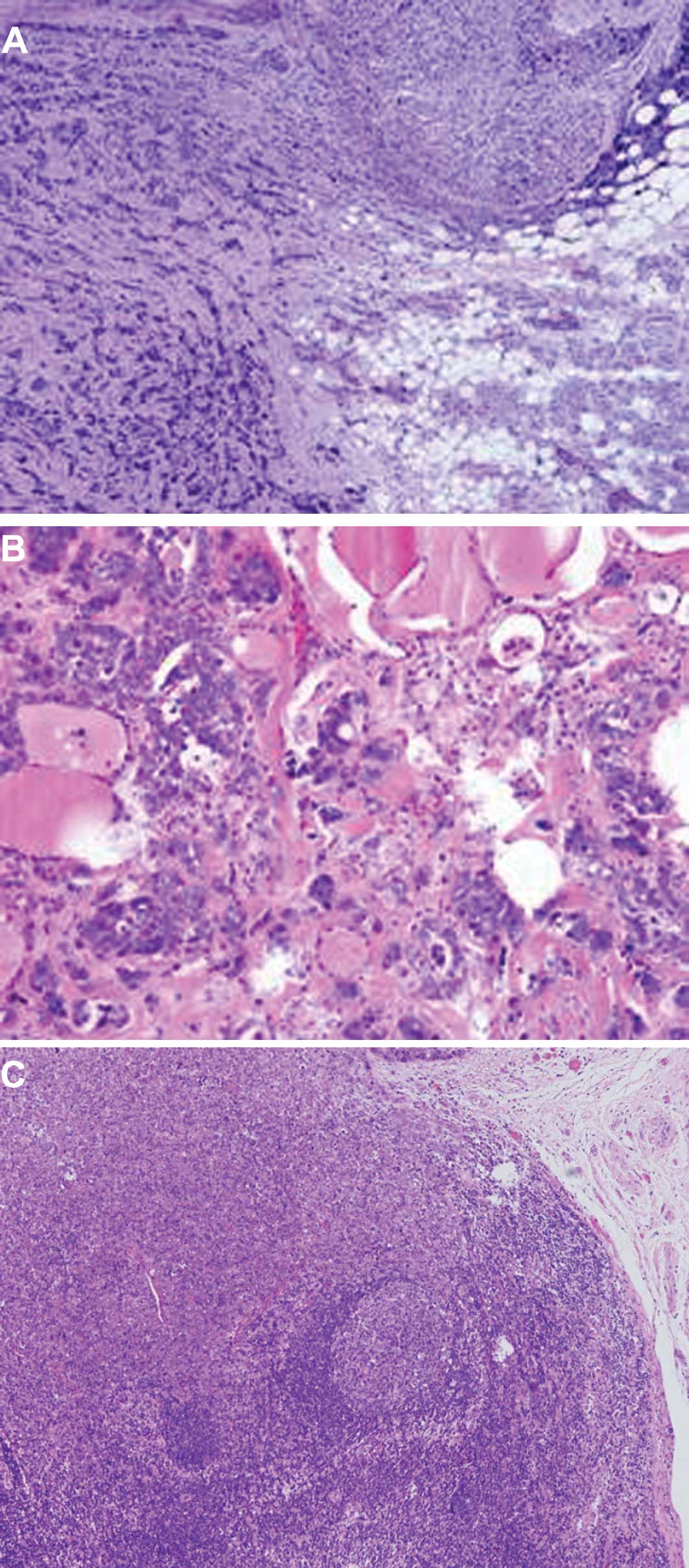
The parotid tumor showed nests or trabecular
architecture divided by fibrous septa with no ductal or acinar
differentiation (Fig. 2A). The
neoplastic cells with a myxoid stroma, from the thyroid, exhibited
mild cytological atypia and minimal cytoplasm without the ductal
lumen structure (Fig. 2B). The
neoplastic cells from the involved lymph nodes showed identical
morphological features to the primary lesion in the parotid gland
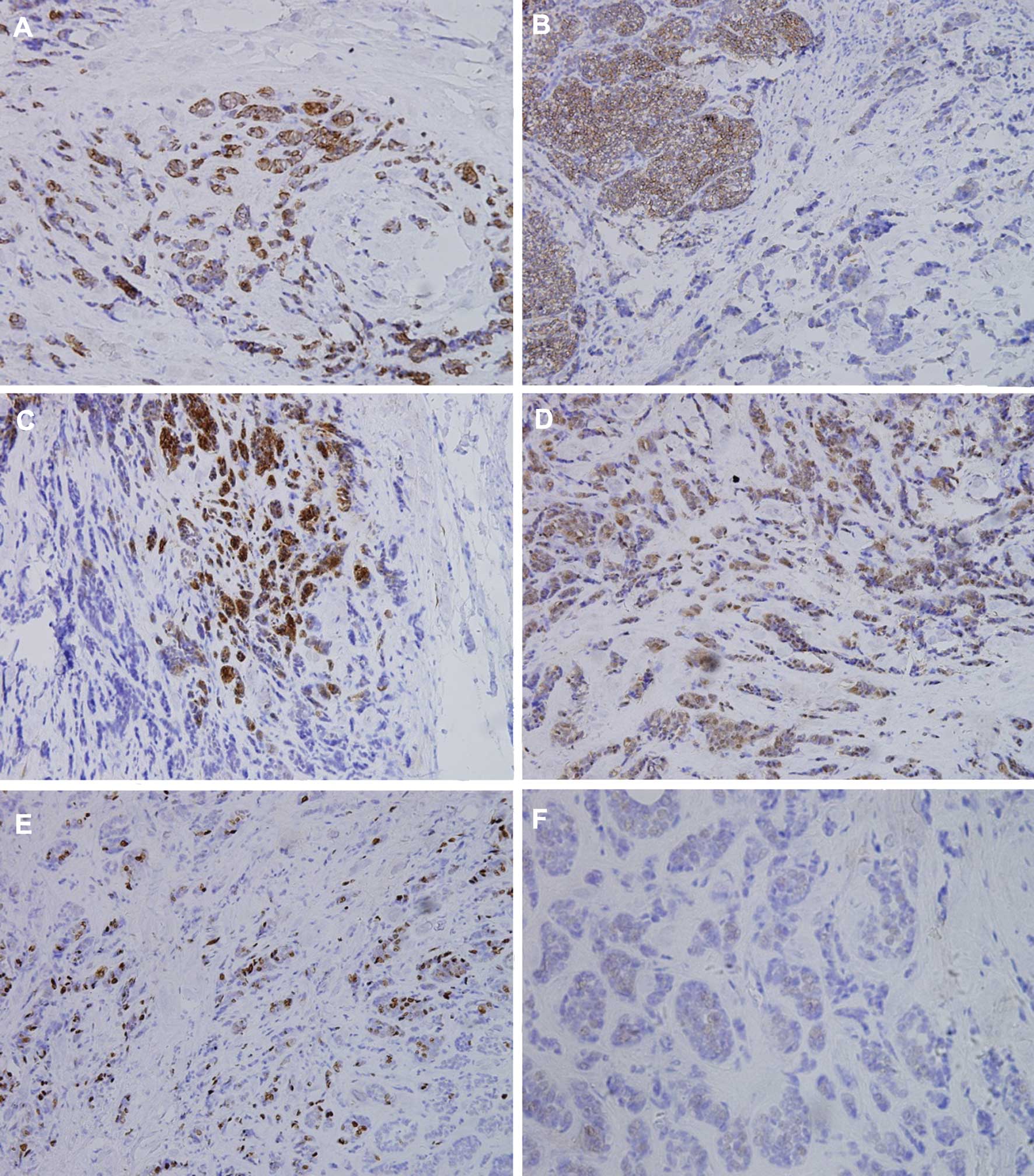
(Fig. 2C). The neoplastic cells
showed positive immunoreaction for CK5, CK18, Calponin, S-100,
Ki-67 and P63, respectively, in Fig.
3, with a strong to weak expression.
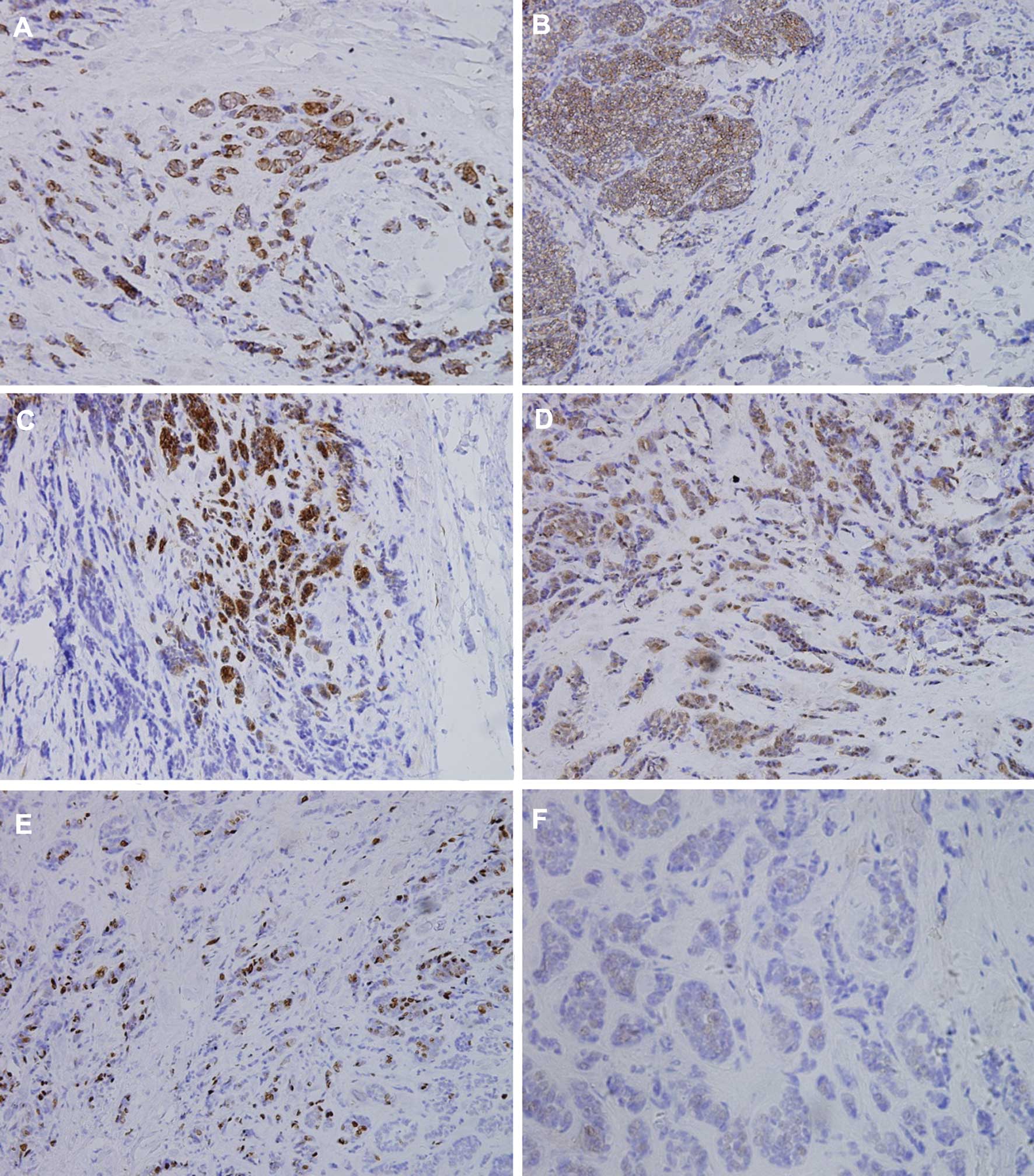 | Figure 3Positive immunohistochemical staining
with (A) CK5, magnification, × 100; (B) CK18, magnification, × 100;
(C) Calponin, magnification, × 100; and (D) S-100, magnification, ×
100. (E) The nuclear staining of Ki-67 in MEC, magnification, ×
100. (F) The tumor cells showed weak nuclear staining of P63 in
MEC, magnification, × 200. |
The cytomorphology and immunohistochemical findings
were similar to those of the previously resected primary
myoepithelial carcinoma (MCA) of the parotid gland. The original
tumor exhibited an infiltrative multilobular growth pattern with
increased mitotic activity (up to 8 mitoses per 10 high power
fields) and proliferative rate (Ki-67 index of >75%).
Discussion
Epidemiology and biological behavior of
myoepithelial carcinomas
Both benign and malignant tumors in the parotid
gland show myoepithelial cell differentiation. Neoplasms composed
exclusively of myoepithelial cells are relatively uncommon; their
incidence has been identified in 1% of all tumors of the parotid
glands, while malignant MCA is extremely rare. The neoplasm occurs
primarily in the large salivary glands (85–90%), particularly in
the parotid (1–6). Approximately 125 cases of
myoepithelial carcinomas have been described thus far (19). The majority of these carcinomas are
located in the salivary glands with the exception of cartain rare
cases found in the nasal cavity, paranasal sinuses, lacrimal
glands, bronchus, lungs or kidneys (7). Due to a lack of myoepithelial
differentiation in the thyroid, MCA is generally considered not to
occur in the thyroid.
Since myoepithelial carcinomas are rare, no mature
and unified identification of their biological behavior exists. The
tumor is recognized to be a low-grade malignant tumor by the World
Health Organization salivary gland classification, due to its low
metastatic potential and potential for local recurrence (8). Nevertheless, with the accumulating
data, more than 50% of cases have high-grade potency (3) and either recurrence or distant
metastasis. The de novo form is considered to be more
aggressive and to have greater metastatic potential (2). However, observations have been
contradictory and the metastatic behavior of MCA has yet to be
elucidated (1).
The primary parotid MCA exhibits not only the lymph
transfer predilection, which often transfers to cervical lymph
nodes, but also distant metastasis, including the lungs, bones and
liver (9). To the best of our
knowledge, this case is the first to involve bilateral thyroids and
cervical lymph nodes.
Histological features and pathological
diagnosis of myoepithelial carcinomas
Cytomorphologically, myoepithelial tumors may
contain four cell types thought to represent various stages in
myoepithelial cell differentiation (10). These cell types include
spindle-shaped, epithelioid, plasmacytoid and clear cells, or
combinations thereof.
The identification of MCA depends on the presence of
infiltrative growth, mitotic count, cellular polymorphism, tumor
necrosis or a combination thereof (1,2).
Few previous studies exist on the histocytological
features of MCA, which showed its cytomorphology to be diverse.
Depending on the predominant cell type and immunohistochemical
analysis within MCA, differential diagnoses include tumors such as
epithelial myoepithelial carcinoma (EMC), clear cell carcinoma
(CCC) and carcinoma ex pleomorphic adenoma, which previously
contained the two carcinomas. EMC, another type of salivary gland
tumors, has both epithelial and myoepithelial differentiation
microscopically with a notable ductal lumen appearance, while CCC
lacks epithelial structure (10–13).
Immunohistochemical studies play a key role in the
confirmation of myoepithelial differentiation. Current
immunohistochemical criteria are dual positivity for the two
cytokeratins (including CK5 and CK18). The myoepithelial markers,
S-100 protein, calponin, p63, GFAP, CD10, maspin and actins, were
shown to be immunohistochemically expressed (14,15).
In this case, mild cytological atypia with little focal necrosis
was noted. Myoepithelial differentiation was confirmed by strong
and diffuse immunoreactivity to keratins 5 and 10, S-100 and
P63.
Studies have shown that the anti-P63 antibody is an
effective marker of myoepithelial cells with higher specificity
(10). However, few studies were
published on the expression of P63 in salivary gland tumors
(14–17). Certain authors considered that
Calponin, an α-smooth muscle actin, is most effective in detecting
myoepithelial carcinomas (18).
Calponin reacts with 75% of myoepithelial carcinomas (3). In this study, the Calponin expression
is strong-positive. Recent research showed that in order to
identify the hyperplasty activity using the Ki-67 antibody,
immunohistostaining was found to aid somewhat in differentiating
the diagnosis of benign from malignant myoepithelialioma. A Ki-67
labeling index of more than 10% may lead to a diagnosis of
non-benign myoepithelial carcinoma. On the other hand, the
cytological appearance, including infiltrative growth, mitotic
count, cellular polymorphism or tumor necrosis, renders it
difficult to differentiate malignant from benign myoepithelial
carcinoma. In this study, the Ki-67 labeling index was more than
75%.
Myoepithelial carcinoma therapy
As in the case of other malignant tumors, the
histological features of MCA have thus far failed to reliably
predict prognosis, including biological behavior and clinical
outcome. Generally speaking, primary MCAs with significant
cytological atypia, high proliferative activity, brisk mitotic rate
and necrosis behave aggressively and are more likely to develop
distant metastasis (3). Since the
clinical manifestation varies from case to case, its pathological
features do not correlate with prognosis and a low neoplasm
incidence rate. Moreover, effective treatment, particularly for
distant metastasis, is scarce. Surgery is the preferred choice of
treatment, whether in the primary or transferred region. We used
125I radioactive bead local implantation for the
recurrence of MCA and yielded satisfactory results, taking into
account the limited period. While the primary lesion is controlled
effectively, the predisposing area for the metastasis should be
carefully monitored. Image examination should be used for the neck
dissection when any subtle changes showing cervical lymph node
metastasis are noted. Due to the high occurrence of distant
metastasis, an examination of the lungs or other organs should be
conducted upon diagnosis of myoepithelial carcinoma. In conclusion,
postoperative chemotherapy or radiotherapy may help to prevent
metastasis and recurrence (1).
References
|
1
|
Nagao T, Sugano I, Ishida Y, Tajima Y,
Matsuzaki O, Konno A, Kondo Y and Nagao K: Salivary gland malignant
myoepithelioma: a clinicopathologic and immunohistochemical study
of ten cases. Cancer. 83:1292–1299. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Di Palma S and Guzzo M: Malignant
myoepithelioma of salivary glands: clinicopathological features of
ten cases. Virchows Arch A Pathol Anat Histopathol. 423:389–396.
1993.PubMed/NCBI
|
|
3
|
Savera AT, Sloman A, Huvos AG and Klimstra
DS, Huvos AG and Klimstra DS: Myoepithelial carcinoma of the
salivary glands: a clinicopathologic study of 25 patients. Am J
Surg Pathol. 24:761–774. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cheuk W and Chan JK: Advances in salivary
gland pathology. Histopathology. 51:1–20. 2007. View Article : Google Scholar
|
|
5
|
Wang Z, Herrington B, Schwartz MR and
Laucirica R: Myoepithelial carcinoma of the parotid gland
metastatic to the kidney: case report and review of the literature.
Diagn Cytopathol. 38:27–282. 2010.
|
|
6
|
Chhieng DC and Paulino AF: Cytology of
myoepithelial carcinoma of the salivary gland. Cancer. 96:32–36.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hornick JL and Fletcher CD: Myoepithelial
tumors of soft tissue: a clinicopathologic and immunohistochemical
study of 101 cases with evaluation of prognostic parameters. Am J
Surg Pathol. 27:1183–1196. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Seifert G and Sobin LH: Histological
typing of salivary gland tumors. World Health Organization
International Histological Classification of Tumors. 2nd edition.
Springer-Verlag; NY: 1991
|
|
9
|
Darvishian F and Lin O: Myoepithelial
cell-rich neoplasms cytologic features of benign and malignant
lesions. Cancer. 102:355–361. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Seethala RR, Barnes EL and Hunt JL:
Epithelial-myoepithelial carcinoma: a review of the
clinicopathologic spectrum and immunophenotypic characteristics in
61 tumors of the salivary glands and upper aerodigestive tract. Am
J Surg Pathol. 31:44–56. 2007. View Article : Google Scholar
|
|
11
|
Wang B, Brandwein M, Gordon R, Robinson R,
Urken M and Zarbo RJ: Primary salivary clear cell tumors – a
diagnostic approach a clinicopathologic and immunohistochemical
study of 20 patients with clear cell carcinoma, clear cell
myoepithelial carcinoma, and epithelial-myoepithelial carcinoma.
Arch Pathol Lab Med. 126:676–685. 2002.
|
|
12
|
Ogawa I, Nishida T, Miyauchi M, Sato S and
Takata T: Dedifferentiated malignant myoepithelioma of the parotid
gland. Pathol Int. 53:704–709. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jain M, Thomas S and Singh S: Epithelial
myoepitheial carcinoma of minor salivary gland – low grade
malignant tumor presenting with nodal metastasis. Indian J Pathol
Microbiol. 49:399–401. 2006.PubMed/NCBI
|
|
14
|
Genelhu MC, Gobbi H, Soares FA, Campos AH,
Ribeiro CA and Cassali GD: Immunohistochemical expression of p63 in
pleomorphic adenomas and carcinomas ex-pleomorphic adenomas of
salivary glands. Oral Oncol. 42:154–160. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Edwards PC, Bhuiya T and Kelsch RD:
Assessment of p63 expression in the salivary gland neoplasms
adenoid cystic carcinoma, polymorphous low-grade adenocarcinoma,
and basal cell and canicular adenomas. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod. 97:613–619. 2004. View Article : Google Scholar
|
|
16
|
Bilal H, Handra-Luca A, Bertrand JC and
Fouret PJ: p63 is expressed in basal and myoepithelial cells of
human normal and tumor salivary gland tissues. J Histochem
Cytochem. 51:133–139. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Emanuel P, Wang B, Wu M and Burstein DA:
p63 immunohistochemistry in the distinction of adenoid cystic
carcinoma from basaloid squamous cell carcinoma. Mod Pathol.
18:645–650. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Furuse C, Sousa SO, Nunes FD, Magalhães MH
and Araújo VC: Myoepithelial cell markers in salivary gland
neoplasms. Int J Surg Pathol. 13:57–65. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kane SV and Bagwan IN: Myoepithelial
carcinoma of the salivary glands: a clinicopathologic study of 51
cases in a tertiary cancer center. Arch Otolaryngol Head Neck Surg.
136:702–712. 2010. View Article : Google Scholar : PubMed/NCBI
|