Introduction
Thymoma is one of the most common tumors in the
mediastinum and accounts for 45% of anterior mediastinal tumors in
adults (1). Since it has a variable
appearance in histology, it is classified based on the predominant
cell types, such as lymphocytic, epithelial or spindle cell
variants. Furthermore, a new classification system with the aim of
grouping thymomas based on cytological differences has been
proposed by the WHO, since a strong association exists between
histological subtype and invasiveness as well as prognosis
(2,3). The Masaoka staging system, which
classifies tumors according to the degree of invasion through the
capsule into the surrounding structures, has also been proposed
(1,4,5). The
Masaoka staging system has been reported to accurately reflect the
prognosis of thymoma (2,6). On the other hand, thymic carcinoma is
relatively rare and, histologically, it commonly manifests as
squamous cell carcinoma or lymphoepithelioma-like carcinoma
(2). In contrast to thymoma, thymic
carcinoma usually features necrosis, cell atypia and mitosis, and
is cytologically and clinically malignant (1,2).
Since divergent infiltration of lymphocytes has been
observed in thymoma and thymic carcinoma, it has been postulated
that, as with other organs (7),
antigen presentation through MHC-II is associated with the amount
of tumor-infiltrating lymphocytes, which reflects the
above-mentioned histological subtypes. Previously, the association
of presumed antigen-presenting cells, which are
immunohistochemically positive for CD1a and S100 protein, in thymic
neoplasms was investigated (8–10).
However, it was subsequently established that CD1a and S100 protein
are not specific markers for antigen-presenting cells. Instead,
immunohistochemically fascin+ cells with dendritic
morphology were found to be more specific for antigen-presenting
mature dendritic cells (DCs) (11,12).
We demonstrated the contribution of fascin+ mature DCs
in tumor-related sarcoid reactions in various types of cancer,
which implicated the occurrence of tumor immunity (12).
Fascin is a 55-kDa actin-binding protein and a major
regulating factor of the cytoskeleton that localizes to
microspikes, filopodia and protrusions under the cytomembrane
(11,13). In normal adult human tissues, fascin
expression is restricted to neurons and DCs; both cell types have
markedly large filopodia and are highly motile (11,13).
Fascin expression in various neoplastic cells has also been
investigated, and its expression has been reported to be associated
with epithelial to mesenchymal progression and invasion of tumor
cells as well as a clinically aggressive manifestation and poorer
prognosis (14–23). However, to the best of our
knowledge, immunohistochemical studies for the detection of
fascin+ mature DCs in thymoma have yet to be performed.
In addition, fascin expression in the epithelial components of
thymomas and thymic carcinomas remains to be investigated. Thus,
the present study was designed to assess fascin expression in DCs
and tumor epithelia in thymomas and thymic carcinomas.
Materials and methods
Case selection and immunohistochemistry
of fascin
In the present study, resected thymoma and thymic
carcinoma specimens were obtained by standard thoracotomies and
tumor resections from patients analyzed between 2003 and 2010.
Following informed patient consent, the tissues were used for the
diagnostic work-up and transferred to the archival files at Kyorin
University Hospital, Tokyo, according to the data and ethics
protection rules of the Medical Faculty. The tissues were fixed by
immersion in 4% formalin for 24 h and embedded in paraffin using
standard techniques. One representative tissue sample that included
the tumor area key to diagnosis was selected in each case. Tissue
sections were stained with hematoxylin and eosin. Additionally, the
immunohistochemical staining of fascin was performed using a mouse
monoclonal anti-fascin antibody (clone 55K-2, dilution 1:500; Dako,
Glostrup, Denmark) on 4-μm paraffin-embedded sections, using a LSAB
method by the Nex-ES IHC staining module (Ventana I-VIEW DAB
universal kit; Ventana Medical Systems Inc., Tucson, AZ, USA). To
expose antigens, sections were autoclaved in citrate buffer (pH
6.0) for 10 min and cooled for 30 min. Nuclear counterstaining was
performed with Mayer’s hematoxylin. For the negative control, the
incubation step with the primary antibody was omitted.
Interpretation of immunohistochemical
results of fascin
Light microscopy performed with a Carl Zeiss HAL 100
instrument and W-PI 10x/23 ocular lens was used to analyze and
quantitate the immunohistochemical data. With regard to the number
of fascin-positive DCs (fascin+ DCs) in each
preparation, immunopositive cells with dendritic morphology were
counted in 1/16 mm2 squares within 8 randomly selected
fields using ×400 magnification, and the sum of all cell counts
within a total of 0.5 mm2 tissue area was allocated a
point score as follows: 0–40 cells, 0; 41–80 cells, 1; 81–120
cells, 2; and >120 cells, 3. Fascin+ DCs occasionally
formed a cluster, where they aggregated and were arranged at even
intervals (DC-cluster). These clusters were analyzed in detail, and
the mean interval between neighboring DCs was measured in each
preparation using ×400 magnification. The ratio of the area where
DCs formed clusters to the total tumor area (DC-cluster ratio) was
then assessed in each preparation using ×100 magnification and
allocated a point score as follows: 0–25%, 0; 26–50%, 1; 51–75%, 2;
and 76–100%, 3. The amount of fascin+ tumor epithelium
was assessed as a ratio of positive cell components to total
epithelial components in each preparation using ×100 magnification
and scored as above: 0–25%, 0; 26–50%, 1; 51–75%, 2; and 76–100%,
3. Using the positively stained blood vessel endothelial cells as
an internal control, the intensity of positive staining in DCs and
tumor epithelium was assessed (intensity of DCs and intensity of
epithelium, respectively) and allocated a point score as follows:
negative, 0; less than the control, 1; equal to the control, 2; and
more than the control, 3, according to the established counting
system of fascin intensity (16).
In specimens where normal thymus were included, fascin expression
in infiltrating DCs and normal thymic epithelium as well as
immunoreactive intensity were assessed, but they were not allocated
characteristic point scores since these factors were generally
negligible in normal thymus.
Clinicopathological and statistical
analysis
Clinico-pathological information was allocated point
scores as follows. For the patients’ gender, scores were assigned
as male, 0 or female, 1. Scores for patients’ age were assigned
according to years: <40, 0; 40–49, 1; 50–59, 2; 60–69, 3; 70–79,
4; and >79, 5. Complications from myasthenia gravis were
assessed and scored as absent, 0 or present, 1. Limited to the
cases in which lymph node dissection was performed, lymph node
metastasis was graded as (−), 0 or (+), 1. The Masaoka staging
system was also utilized and scored as: stage 1, 0; stage 2, 1;
stage 3, 2; stage 4a, 3; and stage 4b, 4. The maximum diameter of
the tumor (tumor diameter) was graded as: <3 cm, 0; 3.1–6 cm, 1;
6.1–9 cm, 2; 9.1–12 cm, 3; 12.1–15 cm, 4; or >15 cm, 5. The
histology of the tumor was subdivided and scored in various ways.
First, differentiation between thymoma and thymic carcinoma
(thymoma vs. carcinoma) was assessed and scored as thymoma, 0 or
thymic carcinoma, 1. Second, limited only to thymoma, ‘histological
variants’ were assigned point scores as: lymphocytic-predominant
(Type B1), 0; intermediate (Types AB and B2), 1; and thymic
epithelial-predominant (Types A and B3), 2 (24). For thymoma alone, histology based on
the origin of thymic epithelium (epithelial origin) was graded as:
medullary epithelium (Type A), 0; mixed (Type AB), 1; or cortical
epithelium (Types B1, B2 and B3), 2 (3). Based on the point scores
described above, statistical analyses using Spearman’s rank
correlation was performed with the SPSS software package (standard
version, release 10.0.7 J; SPSS, Chicago, IL, USA). The data are
presented as the means ± standard deviation where appropriate.
Additional immunostaining for limited
cases
To assess the fascin+ cell types, the
most recent case was selected from each diagnostic category (Types
A, AB, B1, B2 and B3 thymomas; and thymic carcinoma). For these 6
selected samples, additional immunostainings for S100 protein
(polyclonal rabbit, dilution 1:800; Dako), HLA-DR (clone TAL.1B5,
dilution 1:1,000; Dako), CD1a (clone MTB-1, dilution 1:25;
Novocastra, Newcastle upon Tyne, UK) and cytokeratin AE1/AE3 (clone
AE1/AE3, dilution 1/100; Dako), were performed. The above-mentioned
LSAB method by the Nex-ES IHC staining module was used, with the
exception of CD1a visualization, which was performed via the
polymer peroxidase method (ACUITY Advanced Biotin Free HRP Polymer
Detection System; Covance Research Products, Inc., Dedham, MA,
USA). For antigen retrieval, tissues for HLA-DR and CD1a
immunostainings were autoclaved in citrate buffer (pH 6.0) for 10
min and in citrate buffer (pH 9.0) for 5 min, respectively.
Immunopositive cells with dendritic morphology were assessed and
compared to those stained for fascin. These cells were also counted
in 1/16 mm2 squares within 8 randomly selected fields
using ×400 magnification. The sum of the cell counts within a total
of 0.5 mm2 tissue area was then calculated, except in
the assessment of cytokeratin AE1/AE3.
Results
A total of 34 cases of thymoma and 5 cases of thymic
carcinoma diagnosed and resected during the past 8 years at the
Kyorin University Hospital were identified and used in this study.
The clinical data are shown in Table
I. The thymoma cases comprised 23 males and 11 females, whereas
the thymic carcinoma cases included 3 males and 2 females. The mean
age of thymoma patients was 56.1±14.3 years, whereas that of thymic
carcinoma patients was 63.0±5.66 years. In total, 8 cases with
complications from myasthenia gravis were identified, 7 of whom
were male patients. In other cases, thymic neoplasms were found
incidentally. Lymph node dissection was performed in 18 cases,
including 4 thymic carcinomas, and lymph node metastasis was
identified in 7 cases, including 2 thymic carcinomas. Normal thymus
was included in 28 of the analyzed cases.
 | Table IClinicopathological data for analyzed
thymomas and thymic carcinomas. |
Table I
Clinicopathological data for analyzed
thymomas and thymic carcinomas.
| Histological
classification | No. | Gender (male,
female) | Average age | Complication
myasthenia dissection gravis (−, +) | Lymph node from
metastasis (−, +, not performed) | Masaoka staging
system (1, 2, 3, 4a, 4b, not recorded) | Average tumor’s
maximal diameter | Normal thymus
tissue (−, +) |
|---|
| Type A | 4 | 1:3 | 70.3±6.95 | 4:0 | 1:0:3 | 0:1:3:0:0:0 | 5.75±2.53 | 3:1 |
| Type AB | 12 | 8:4 | 56.0±12.9 | 11:1 | 3:2:7 | 7:2:0:0:0:3 | 6.98±2.94a | 3:9 |
| Type B1 | 1 | 1:0 | 36 | 0:1 | 0:0:1 | 0:0:0:0:0:1 | 3.5 | 0:1 |
| Type B2 | 11 | 9:2 | 47.6±13.7 | 5:6 | 4:1:6 | 4:4:2:1:0:0 | 10.25±5.56a | 3:8 |
| Type B3 | 6 | 4:2 | 65.7±8.52 | 6:0 | 1:2:3 | 2:2:0:1:1:0 | 4.58±2.06b | 2:4 |
| Carcinoma | 5 | 3:2 | 63.0±5.66 | 5:0 | 2:2:1 | 0:1:2:0:1:1 | 7.50±2.86a | 0:5 |
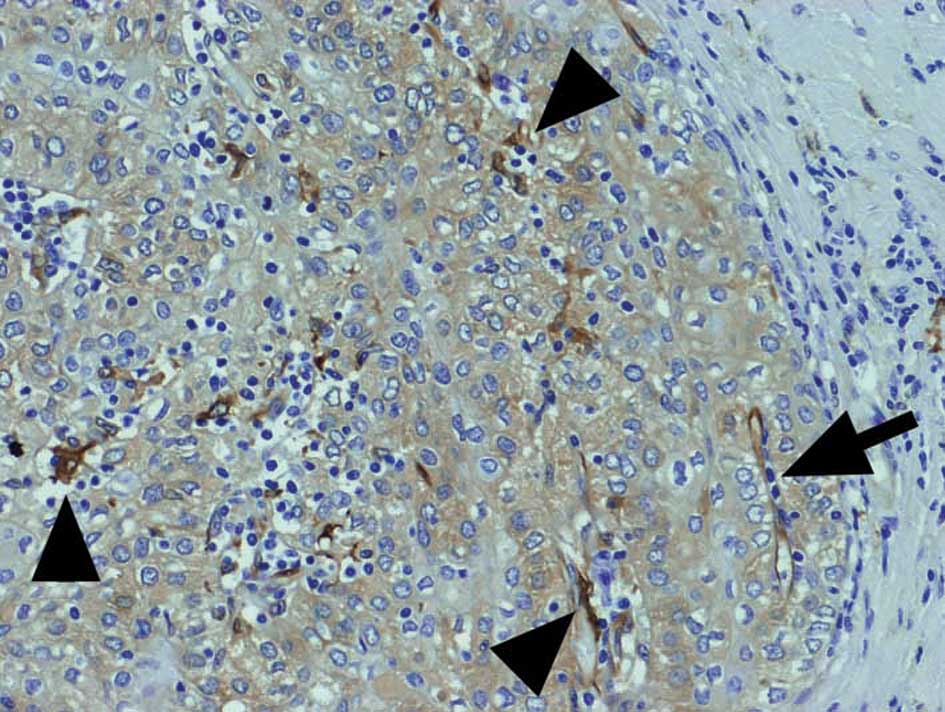
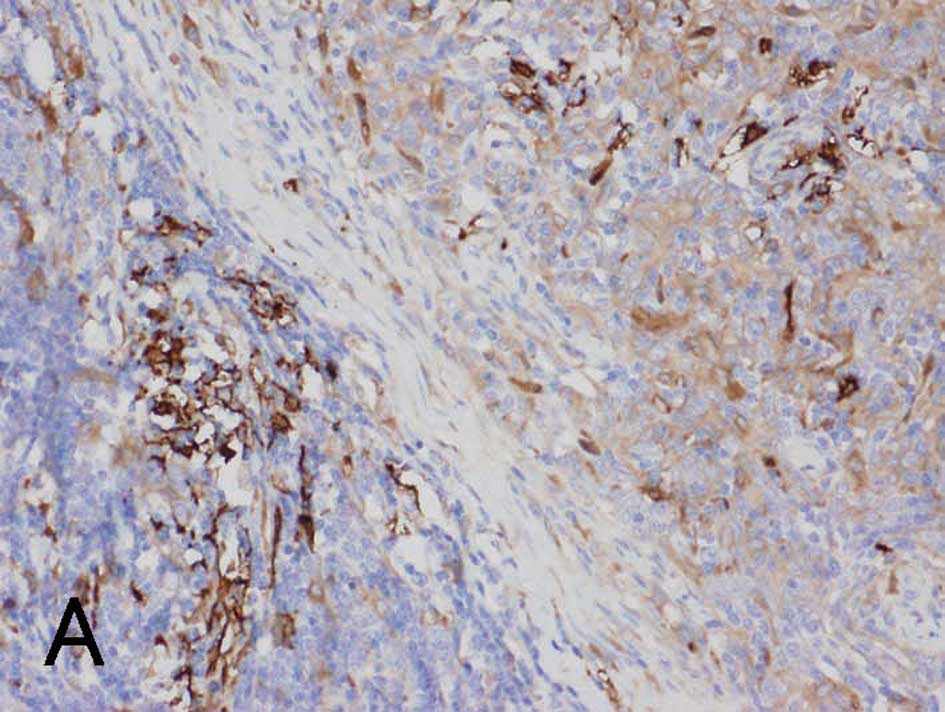
The immunohistochemical results for fascin are shown
in Table II. Fascin+
mature DCs were identified in the thymoma and thymic carcinoma
specimens, particularly in the regions of lymphocytic infiltration
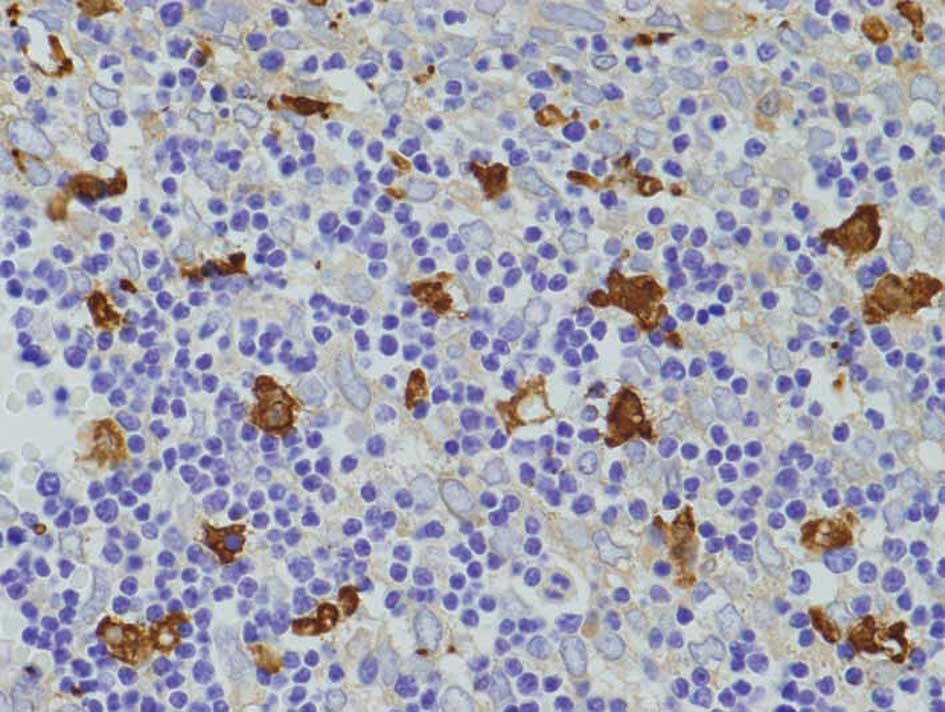
(Fig. 1). Diffuse DC-clusters were
observed in Type B1 thymomas (Fig.
2), whereas DC-clusters were identified in regions of cortical
differentiation in other types of thymomas. The mean interval
between neighboring DCs within the DC-clusters was 25–50 μm in each
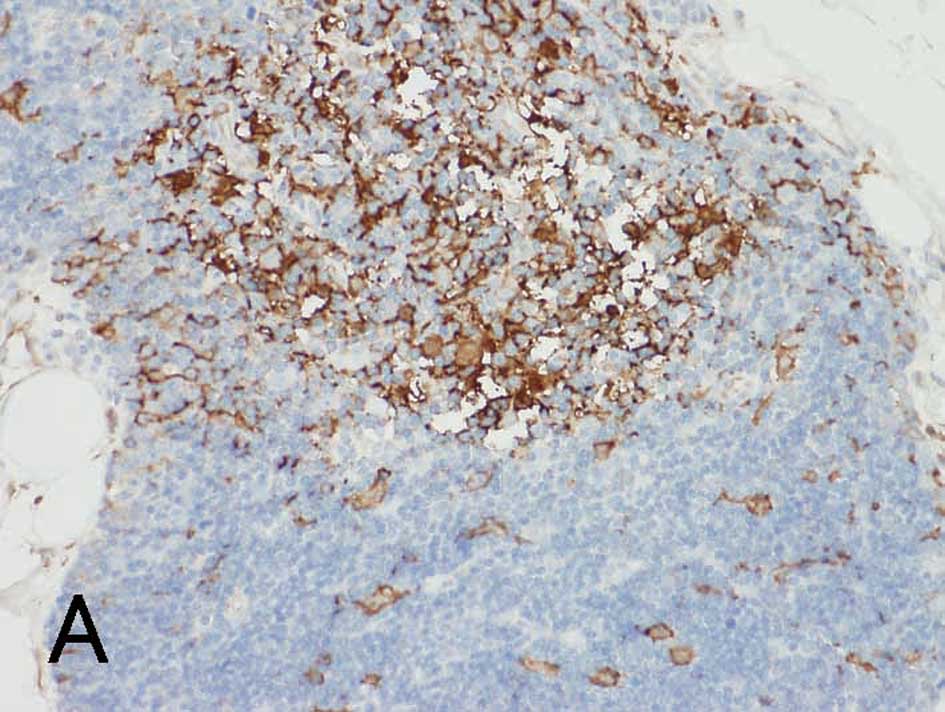
specimen. In normal thymus, DCs in the cortex and medulla were
generally positive for fascin (Fig.
3A). Fascin+ epithelium was observed in all of the
thymoma specimens (Figs. 1 and
2), although the immunoreactive
intensity was variable and generally weaker than the intensity of
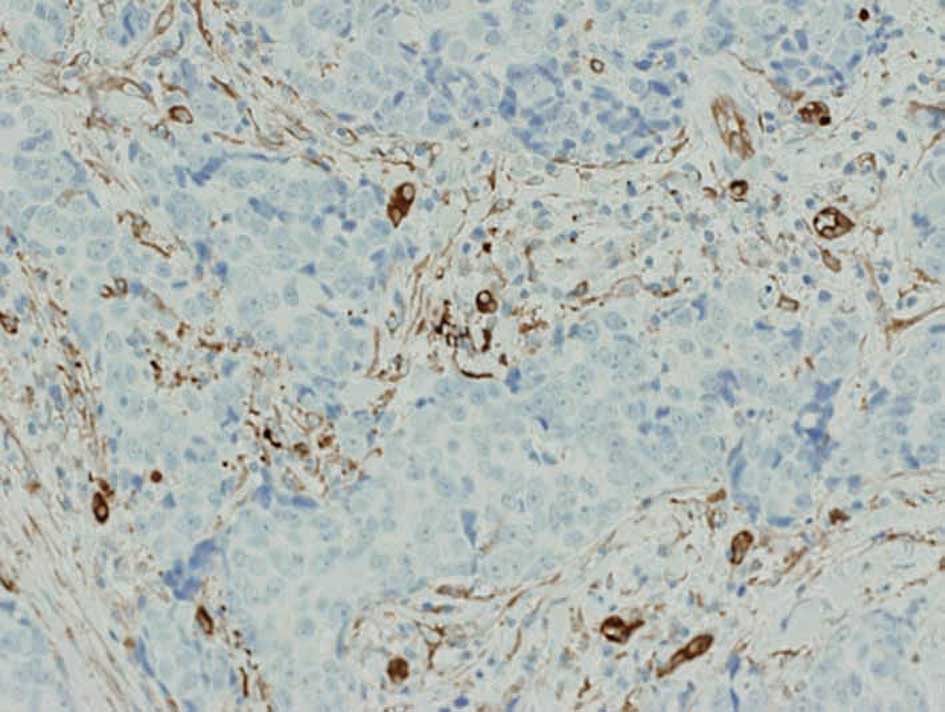
DCs. Only 1 out of 5 thymic carcinoma specimens had
fascin+ epithelium, while no epithelial fascin
expression was observed in the remaining 4 specimens (Fig. 4).
 | Table IISummary of immunohistochemical
results of fascin. |
Table II
Summary of immunohistochemical
results of fascin.
| | Fascin+
DCs | Fascin+
epithelium |
|---|
| |
|
|
|---|
| Histological
classification | No. | Fascin+
DCs (per 0.5 mm2 tissue area) | Intensity of
DCs | Ratio (%) of
DC-cluster | Ratio (%) of
positive cell component: Fascin+ epithelium | Intensity of
epithelium |
|---|
| Type A | 4 | 7.3±7.4 | 0.75±0.96 | 3±5 | 21±17 | 0.75±0.50 |
| Type AB | 12 | 63.0±29 | 2.10±0.29 | 53±22 | 68±24 | 0.91±0.29 |
| Type B1 | 1 | 134 | 2 | 100 | 20 | 1 |
| Type B2 | 11 | 80.0±53 | 2.00±0.63 | 54±38 | 44±37 | 0.81±0.40 |
| Type B3 | 6 | 42.0±33 | 2.00±1.10 | 41±37 | 50±39 | 0.67±0.52 |
| Carcinoma | 5 | 4.0±2.6 | 1.20±1.10 | 4±9 | 14±31 | 0.60±1.30 |
Correlation coefficients were obtained (Tables III and IV) using these clinicopathological and
immunohistochemical data, with plus and minus symbols showing
positive and negative correlations, respectively. Only the
significant results (p<0.05) are appointed Spearman’s rho (‘r’),
a non-parametric measure of correlation that assesses how well an
arbitrary monotonic function describes the relationship between two
variables without making any other assumptions about the particular
nature of the relationship between the variables. Table III shows the correlations between
the clinicopathological and immunohistochemical data, while
Table IV shows the results of
mutual correlations between different immunohistochemical data.
 | Table IIICorrelations between
clinicopathological data and immunohistochemical results of
fascin. |
Table III
Correlations between
clinicopathological data and immunohistochemical results of
fascin.
| Fascin+
DCs | Fascin+
epithelium |
|---|
|
|
|
|---|
| Clinicopathological
data | Fascin+
DCs (per 0.5 mm2 tissue area) | Intensity of
DCs | Ratio (%) of
DC-cluster | Ratio (%) of
positive cell component: Fascin+ epithelium | Intensity of
epithelium |
|---|
| Patients’
gender | r=−0.358,
p=0.025 | ns | ns | ns | ns |
| Patients’ age | ns | ns | ns | ns | ns |
| Complication from
MG | r=+0.478,
p=0.002 | ns | ns | ns | ns |
| Masaoka stage
scores | ns | r=−0.495,
p=0.003 | ns | r=−0.553,
p=0.001 | r=−0.381,
p=0.026 |
| Tumor diameter | r=+0.376,
p=0.029 | ns | ns | ns | ns |
| Lymph node
metastasis | ns | ns | ns | ns | ns |
| Thymoma vs. Ca | r=−0.361,
p=0.024 | r=−0.388,
p=0.026 | r=−0.342,
p=0.033 | ns | ns |
| Histologic
variants | r=−0.513,
p=0.002 | ns | r=−0.391,
p=0.022 | ns | ns |
| Epithelial
origin | r=+0.359,
p=0.037 | r=+0.373,
p=0.030 | ns | ns | ns |
 | Table IVMutual correlations between different
immunohistochemical results of fascin. |
Table IV
Mutual correlations between different
immunohistochemical results of fascin.
| Fascin+
DCsa | Intensity of
DCs | DC-cluster
ratio | Fascin+
epithelium | Intensity of
epithelium |
|---|
| Fascin+
DCs | - | r=+0.382,
p=0.016 | r=+0.780,
p<0.001 | ns | ns |
| Intensity of
DCs | - | - | r=+0.481,
p=0.002 | r=+0.487,
p=0.002 | ns |
| DC-cluster
ratio | - | - | - | r=+0.473,
p=0.002 | r=+0.325,
p=0.043 |
| Fascin+
epithelium | - | - | - | - | r=+0.560,
p<0.001 |
| Intensity of
epithelium | - | - | - | - | - |
As shown in Table
III, fascin+ DCs showed negative correlations with
the patients’ gender, thymoma vs. carcinoma and histological
variants, whereas it demonstrated positive correlations with
complication from myasthenia gravis, tumor diameter and epithelial
origin. Therefore, fascin+ DCs appear more frequently in
benign thymic neoplasms with a greater diameter, which are
lymphocytic-predominant variants and of cortical epithelium origin,
and in male patients with complication from myasthenia gravis.
Intensity of DCs showed a positive correlation with epithelial
origin, while it showed negative correlations with thymoma vs.
carcinoma and the Masaoka stage scores. Therefore, DCs with a
higher intensity of fascin are characteristic of benign thymic
neoplasms of cortical epithelial origin with a lower Masaoka stage.
The ratio of DC-cluster inversely correlated with both thymoma vs.
carcinoma and histological variants, which was identical to the
statistical results of fascin+ DCs. Both the ratio of
fascin+ epithelium and intensity of epithelium
demonstrated a negative correlation with the Masaoka stage scores,
indicating that these immunohistochemical results are
characteristic of specimens with lower Masaoka stage. Patients’ age
and lymph node metastasis did not correlate with any of the
immunohistochemical results. As shown in Table IV, fascin+ DCs
correlated with the intensity of DCs and DC-cluster ratio.
Intensity of DCs also showed positive correlations with DC-cluster
ratio and fascin+ epithelium. DC-cluster ratio further
correlated with fascin+ epithelium and intensity of
epithelium. Statistical analysis also revealed that
fascin+ epithelium was positively correlated with
intensity of epithelium.
With regard to the various immunohistochemical
markers in the selected specimens, the presence of
fascin+ DCs in thymic neoplasms grossly corresponded to
HLA-DR+ DCs. However, a greater number of
fascin+ signals was observed in the cortical
differentiation area, as noted in Types B1 and B2 thymomas.
Fascin+ DCs also occasionally co-expressed S100 protein
in the medullary differentiation area, but did not express CD1a
(Fig. 5A-D). CD1a was also positive
in tumor-infiltrating lymphocytes of Types AB, B1 and B2 thymomas,
but negative in lymphocytes of other types and of carcinoma.
Cytokeratin AE1/AE3 was generally positive in the epithelial
components of thymic neoplasms (Fig.
5E). These results are shown in Table V. Notably, in normal thymus, both
fascin and HLA-DR were positive for DCs in the medulla, while some
fascin+ DCs in the cortex were negative for HLA-DR
(Fig. 3B).
 | Table VImmunohistochemical results of
various markers in selected specimens. |
Table V
Immunohistochemical results of
various markers in selected specimens.
| Cell counts for DCs
per 0.5 mm2 tissue area | |
|---|
|
| |
|---|
| Histological
classification | Fascin | HLA-DR | S100 protein | CD1a | Cytokeratin AE1/AE3
in epithelial component |
|---|
| Type A | 39 | 38 | 3 | 3 | Diffusely
positive |
| Type AB | 91 | 155 | 40 | 123 | Diffusely
positive |
| Type B1 | 134 | 60 | 56 | 0 | Diffusely
positive |
| Type B2 | 112 | 38 | 39 | 10 | Diffusely
positive |
| Type B3 | 14 | 19 | 3 | 21 | Occasionally
positive |
| Carcinoma | 8 | 7 | 20 | 13 | Diffusely
positive |
Discussion
The present study is the first to
immunohistochemically assess the expression of fascin in thymoma
and thymic carcinoma. Infiltrating DCs and tumor epithelium were
confirmed to be positive for fascin in all thymoma tissues, whereas
predominantly infiltrating fascin+ DCs were identified
in the thymic carcinoma tissues. S100 protein was formerly a
commonly used marker for DCs. A number of immunohistochemical
studies for S100 protein in thymomas were previously performed, and
it was reported that abundant S100+ DCs were observed
along with mature T-lymphocytes, especially in
lymphocytic-predominant variants of thymoma (10,25,26).
However, S100 protein is positive in both immature and mature DCs.
Immature DCs are capable of antigen uptake and processing, but are
unable to stimulate naïve T-lymphocytes. On the other hand, mature
DCs bind and stimulate T-lymphocytes (7). Fascin is an actin-bundling protein
expressed by mature DCs and certain other cell types, including
blood vessel endothelial cells (12,27).
In the present study, fascin+ DCs did not correspond to
S100+ DCs, particularly in the cortical differentiation
area in the selected specimens. It has also been proposed that
S100+ DCs are interdigitating reticulum cells, which are
abundant in the medullary differentiation area (10,25).
In the present study, fascin+ DCs were frequently
identified in the cortical differentiation area, as verified by
positive correlation between fascin+ DCs and epithelial
origin, as well as with the co-expression of HLA-DR, a marker of
antigen presentation (28).
Therefore, we postulate that these fascin+ mature DCs
promote tumor immunity through antigen presentation. However, in
the cortex of normal thymus, fascin+ and
HLA-DR− cells were also observed, as reported by other
authors (28). Furthermore, this
study also revealed that fascin+ DCs did not co-express
CD1a, found mostly in immature DCs, although some thymic
lymphocytes were positive for CD1a, as previously reported
(9).
The present study verifies that the observed
fascin+ DC-clusters are mainly associated with benign
thymic neoplasms and lymphocytic-predominant variants, since
fascin+ DCs and DC-cluster ratio inversely correlated
with thymoma vs. carcinoma and histological variants. The positive
correlation found between fascin+ DC and DC-cluster
ratio indicates that the clusters are formed by numerous DCs.
Whether the DCs infiltrate primarily or secondarily to lymphocytic
infiltration remains to be clarified. However, if DCs infiltrate
secondarily to lymphocytic infiltration, evenly-arranged
structures, such as those observed in our cases, could not be
explained. Therefore, it is more likely that mature DCs primarily
capture tumor-related antigens and process and present them to T
lymphocytes for recruitment of other lymphocytes (7). Brunhuber et al, Ambe et
al and Becker have reported that the amounts of
tumor-infiltrating DCs and lymphocytes are interrelated in various
tumors, such as melanoma, thyroid, esophageal, gastric and rectal
cancers (18,29,30).
With regard to the correlations between
clinicopathological data and infiltrating mature DCs, it is
noteworthy that fascin+ DCs correlated with
complications from myasthenia gravis. This may be due to the fact
that only the cases with Types AB, B1 and B2 thymomas, which are
relatively lymphocyte-rich variants, experienced complications from
myasthenia gravis in the present study. This result is in
accordance with the fact that myasthenia gravis is frequently
associated with Types AB, B2 and B3 thymomas (31). Alternatively, the frequent
infiltration of mature DCs in thymomas may explain the reason for
the more favourable prognoses of thymoma patients with myasthenia
gravis, which may initiate tumor immunity, than patients with a
poor prognosis (4).
Fascin+ DCs also correlated with patients’ gender, thus
indicating that mature DCs frequently infiltrate into thymic
neoplasms of male patients. However, this may be a confounding
factor, as 7 out of 8 patients with complications from myasthenia
gravis were males in the present study. The reason for the positive
correlation between fascin+ DCs and tumor diameter may
be that larger tumors are likely to be more frequently recognized
by DCs.
With regard to the fascin expression level in DCs,
it has been reported that increased fascin expression is associated
with enhanced cell motility (14).
In the present study, intensity of DCs correlated with epithelial
origin. Therefore, cortical epithelium may strongly induce mobile
DCs. Cortical epithelium in normal thymus is known to be associated
with maturation of T lymphocytes, by expressing MHC I and II
molecules (28). Modified MHC
molecules during tumor formation may be recognized as antigens by
DCs, thus activated DCs may express increased fascin. Intensity of
DCs further correlated with fascin+ DCs and DC-cluster
ratio, suggesting that activated DCs tend to aggregate and recruit
lymphocytes, resulting in evenly arranged DC structures. Intensity
of DCs exhibited a negative correlation with Masaoka stage scores,
indicating that activated DCs induce immunoreaction and suppress
the invasiveness of the tumor.
Of note is that the ratio of fascin+
epithelium was also inversely correlated with Masaoka stage scores
in the present study. By contrast, it has been reported that
fascin+ tumor epithelium has strong invasiveness with
poorer prognosis in various carcinomas, such as ovarian, breast,
pancreas, lung, cutaneous, brain, gastrointestinal, thyroid,
prostate, urothelial, intrahepatic cholangiocarcinoma and skin
tumors (14–23). The significance of epithelial fascin
expression has been reported to be associated with invasiveness and
metastasis, since it aids in cell migration and proliferation
through increases in lamellipodial and filopodial cell protrusions
(15). Moreover, fascin+
tumor epithelium has been reported to express matrix
metalloproteinase-9 to dissolve the stroma during migration
(20). However, it has also been
reported that epithelial fascin expression does not affect the
prognosis in extrahepatic and hilar cholangiocarcinoma (20). We confirmed that
fascin+-activated tumor epithelium may proliferate
(14,15,19,21)
since there was a positive correlation between intensity of
epithelium and fascin+ epithelium. However, in the
present study, fascin+ epithelium also correlated with
intensity of DCs and DC-cluster ratio. Furthermore, intensity of
epithelium positively correlated with DC-cluster ratio and
inversely correlated with Masaoka stage scores. Therefore, in
thymic neoplasms, invasive tumor epithelium with a wider proportion
and higher intensity of fascin positivity probably induces tumor
immunity through recognition by mature DCs. This may be one reason
for the relatively favorable prognosis of thymoma in general
(2).
It is noteworthy that only 1 out of 5 thymic
carcinomas expressed epithelial fascin. Moreover,
fascin+ DCs, DC-cluster and intensity of DCs were
inversely correlated with thymoma vs. carcinoma, indicating that
the amount and intensity of fascin expression in DCs as well as
cluster-formation are associated predominantly with benign thymic
neoplasms. These results also indicate that malignant
transformation of the thymic neoplasm is associated with a paucity
of activated DCs, presumably due to the poorer epithelial
expression of fascin as mentioned earlier. Alternatively, it is
also speculated that thymic carcinomas tend to proliferate as a
block rather than via infiltration, thus escaping surveillance by
DCs, since it has been reported that fascin is not expressed in the
metastatic foci of colon carcinomas, whereas it is expressed in the
primary tumors (32). However,
since the number of investigated thymic carcinomas in the present
study was small, further studies with larger numbers of cases are
required to elucidate the significance of fascin expression of
thymic carcinomas.
In conclusion, fascin expression in DCs and tumor
epithelium of thymic neoplasms was investigated, and it was
revealed that the amount and/or higher intensity of fascin levels
in DCs with the formation of clusters were associated with
lymphocyte-rich variants and the cortical differentiation of
thymoma with complications from myasthenia gravis. The quantity and
strong intensity of fascin+ epithelium were associated
with cluster-forming infiltrating fascin+ DCs and
favorable prognosis, as assessed by the Masaoka staging system,
thus fascin+ epithelium may promote tumor immunity.
Acknowledgements
This study was partly supported by the Tokyo Medical
University Cancer Research Foundation.
References
|
1
|
Kurup A and Loehrer PJ Sr: Thymoma and
thymic carcinoma: therapeutic approaches. Clin Lung Cancer.
6:28–32. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Duwe BV, Sterman DH and Musani AI: Tumors
of the mediastinum. Chest. 128:2893–2909. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Marx A, Ströbel P, Zettl A, Chan JKC,
Müller-Hermelink HK, Harris NL, Kuo TT, Shimosato Y and Engel P:
Thymomas. Pathology and Genetics of Tumours of the Lung, Pleura,
Thymus and Heart (WHO classification of tumors series). Travis WD,
Brambilla E, Müller-Helmelink HK and Harris CC: IARC Press; Lyon,
France: pp. 152–171. 2004
|
|
4
|
Margaritora S, Cesario A, Cusumano G,
Meacci E, D’Angelillo R, Bonassi S, Carnassale G, Porziella V,
Tessitore A, Vita ML, Lauriola L, Evoli A and Granone P:
Thirty-five-year follow-up analysis of clinical and pathologic
outcomes of thymoma surgery. Ann Thorac Surg. 89:245–252.
2010.PubMed/NCBI
|
|
5
|
Masaoka A, Monden Y, Nakahara K and
Tanioka T: Follow-up study of thymomas with special reference to
their clinical stages. Cancer. 48:2485–2492. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Okumura M, Miyoshi S, Takeuchi Y, Yoon HE,
Minami M, Takeda SI, Fujii Y, Nakahara K and Matsuda H: Results of
surgical treatment of thymomas with special reference to the
involved organs. J Thorac Cardiovasc Surg. 117:605–613. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gerner MY and Mescher MF: Antigen
processing and MHC-II presentation by dermal and tumor-infiltrating
dendritic cells. J Immunol. 182:2726–2737. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kornstein MJ, Hoxie JA, Levinson AI and
Brooks JJ: Immunohistology of human thymomas. Arch Pathol Lab Med.
109:460–463. 1985.
|
|
9
|
Pomplun S, Wotherspoon AC, Shah G,
Goldstraw P, Ladas G and Nicholson AG: Immunohistochemical markers
in the differentiation of thymic and pulmonary neoplasms.
Histopathology. 40:152–158. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lee D and Wright DH: Immunohistochemical
study of 22 cases of thymoma. J Clin Pathol. 41:1297–1304. 1988.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pinkus GS, Pinkus JL, Langhoff E,
Matsumura F, Yamashiro S, Mosialos G and Said JW: Fascin, a
sensitive new marker for Reed-Sternberg cells of hodgkin’s disease.
Evidence for a dendritic or B cell derivation? Am J Pathol.
150:543–562. 1997.PubMed/NCBI
|
|
12
|
Kurata A, Terado Y, Schulz A, Fujioka Y
and Franke FE: Inflammatory cells in the formation of tumor-related
sarcoid reactions. Hum Pathol. 36:546–554. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Machesky LM and Li A: Fascin: invasive
filopodia promoting metastasis. Commun Integr Biol. 3:263–270.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Darnel AD, Behmoaram E, Vollmer RT, Corcos
J, Bijian K, Sircar K, Su J, Jiao J, Alaoui-Jamali MA and Bismar
TA: Fascin regulates prostate cancer cell invasion and is
associated with metastasis and biochemical failure in prostate
cancer. Clin Cancer Res. 15:1376–1383. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Iguchi T, Aishima S, Umeda K, Sanefuji K,
Fujita N, Sugimachi K, Gion T, Taketomi A, Maehara Y and Tsuneyoshi
M: zFascin expression in progression and prognosis of
hepatocellular carcinoma. J Surg Oncol. 100:575–579. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yildiz L, Kefeli M, Aydin O and Kandemir
B: Fascin expression in melanocytic lesions of the skin. Eur J
Dermatol. 19:445–450. 2009.PubMed/NCBI
|
|
17
|
Zhang FR, Tao LH, Shen ZY, Lv Z, Xu LY and
Li EM: Fascin expression in human embryonic, fetal, and normal
adult tissue. J Histochem Cytochem. 56:193–199. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Brunhuber T, Haybaeck J, Schäfer G, Mikuz
G, Langhoff E, Saeland S, Lebecque S, Romani N and Obrist P:
Immunohistochemical tracking of an immune response in mammary
Paget’s disease. Cancer Lett. 272:206–220. 2008.PubMed/NCBI
|
|
19
|
Ozerhan IH, Ersoz N, Onguru O, Ozturk M,
Kurt B and Cetiner S: Fascin expression in colorectal carcinomas.
Clinics. 65:157–164. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Onodera M, Zen Y, Harada K, Sato Y, Ikeda
H, Itatsu K, Sato H, Ohta T, Asaka M and Nakanuma Y: Fascin is
involved in tumor necrosis factor-alpha-dependent production of
MMP9 in cholangiocarcinoma. Lab Invest. 89:1261–1274. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Xie JJ, Xu LY, Wu JY, Shen ZY, Zhao Q, Du
ZP, Lv Z, Gu W, Pan F, Xu XE, Xie D and Li EM: Involvement of CYR61
and CTGF in the fascin-mediated proliferation and invasiveness of
esophageal squamous cell carcinomas cells. Am J Pathol.
176:939–951. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kefeli M, Yildiz L, Kaya FC, Aydin O and
Kandemir B: Fascin expression in uterine smooth muscle tumors. Int
J Gynecol Pathol. 28:328–333. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Durmaz A, Kurt B, Ongoru O, Karahatay S,
Gerek M and Yalcin S: Significance of fascin expression in
laryngeal squamous cell carcinoma. J Laryngol Otol. 124:194–198.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Marchevsky AM, Gupta R, McKenna RJ, Wick
M, Moran C, Zakowski MF and Suster S: Evidence-based pathology and
the pathologic evaluation of thymomas: the World Health
Organization classification can be simplified into only 3
categories other than thymic carcinoma. Cancer. 112:2780–2788.
2008. View Article : Google Scholar
|
|
25
|
Kondo K, Mukai K, Sato Y, Matsuno Y,
Shimosato Y and Monden Y: An immunohistochemical study of thymic
epithelial tumors. III. The distribution of interdigitating
reticulum cells and S-100 beta-positive small lymphocytes. Am J
Surg Pathol. 14:1139–1147. 1990. View Article : Google Scholar
|
|
26
|
Rouse RV and Weiss LM: Human thymomas:
evidence of immunohistologically defined normal and abnormal
microenvironmental differentiation. Cell Immunol. 111:94–106. 1988.
View Article : Google Scholar
|
|
27
|
Kurata A, Terado Y, Izumi M, Fujioka Y and
Franke FE: Where does the antigen of cutaneous sarcoidosis come
from? J Cutan Pathol. 37:211–221. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Wakimoto T, Tomisaka R, Nishikawa Y, Sato
H, Yoshino T and Takahashi K: Identification and characterization
of human thymic cortical dendritic macrophages that may act as
professional scavengers of apoptotic thymocytes. Immunobiology.
213:837–847. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ambe K, Mori M and Enjoji M: S-100
protein-positive dendritic cells in colorectal adenocarcinomas.
Distribution and relation to the clinical prognosis. Cancer.
63:496–503. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Becker Y: Anticancer role of dendritic
cells (DC) in human and experimental cancers – a review. Anticancer
Res. 12:511–520. 1992.
|
|
31
|
Müller-Hermelink HK, Möller P, Engel P,
Menestrina F, Kuo TT, Shimosato Y, Ströbel PH, Asamura H, Marx A,
Masaoka A, Harris NL and Sobin LH: Tumours of the thymus. Pathology
and Genetics of Tumours of the Lung, Pleura, Thymus and Heart (WHO
classification of tumors series). Travis WD, Brambilla E,
Müller-Helmelink HK and Harris CC: IARC Press; Lyon, France: pp.
145–151. 2004
|
|
32
|
Vignjevic D, Schoumacher M, Gavert N,
Janssen KP, Jih G, Laé M, Louvard D, Ben-Ze’ev A and Robine S:
Fascin, a novel target of beta-catenin-TCF signaling, is expressed
at the invasive front of human colon cancer. Cancer Res.
67:6844–6853. 2007. View Article : Google Scholar : PubMed/NCBI
|