Introduction
Lung cancer is one of the most common types of
malignant types of cancer worldwide, accounting for 14% of all
malignant tumors. The morbidity and mortality rates of lung cancer
are ranked the highest among various malignant tumors. Lung cancer
may be divided into two categories by histopathology: non-small
cell lung cancer (NSCLC) and small cell lung cancer (SCLC). NSCLC
accounts for 80 to 85% of all histological types of lung cancer.
Although great progress has been made in the treatment of lung
cancer in recent years, the five-year survival rate remains less
than 15% (1). Postoperative,
recurrent metastasis is a significant factor affecting prognosis.
As such, a correct assessment of postoperative recurrent metastasis
and appropriate standard adjuvant therapy following surgery are
essential to improve the prognosis. At present, the main indicator
that identifies and guides prognosis is TMN staging (1), but this approach is limited. Using TMN
staging, many patients with stage I lung cancer (20–30%) fail to
survive more than five years, while certain patients with more
advanced stages (III or IV) live longer than expected. Therefore,
the TMN staging assessment of prognosis cannot be broadly and
accurately applied, and other prognostic markers are required.
Currently, the majority of tumor markers used for clinical
diagnosis are proteins or other biological macromolecules secreted
into the extracellular portions by tumor cells; these markers
usually appear in the advanced stages of cancer. However, the time
of occurrence and the macromolecular level usually have no close
association with the prognosis of NSCLC. Therefore, these tumor
markers have limited importance or significance for early NSCLC
prognosis.
In recent years, the emergence of epigenetics has
defined another essential research direction. Modern tumor theory
(2–5) considers that there are two types of
mechanisms in tumor formation: i) genetic-level mutations or
changes in the DNA nucleotide sequence, and ii) epigenetic
mechanisms, in which the DNA nucleotide sequence is unchanged but
the gene expression is affected at a transcriptional level through
DNA chemical modification. Epigenetic change can be achieved by
meiosis heredity. Epigenetic modifications include phenomena such
as chromatin remodeling, DNA methylation, histone modifications and
non-coding RNA regulation. Abnormalities in any of these four steps
affect chromatin structure and gene expression and may lead to
complex syndromes, such as multifactorial diseases and cancer. DNA
methylation is one of the most common forms of DNA modification and
is the most widely studied. Unlike DNA sequence changes, many
epigenetic changes are reversible; this provides optimism for the
treatment of disease through epigenetic modification.
The RUNX gene family has three members in mammals,
RUNX1, RUNX2 and RUNX3 (6). The
products of RUNX are essential for regulating growth signal
transduction and gene expression and play significant roles in
normal cell development and tumor formation. The RUNX3 gene was
identified in 1994 by Levanon et al (7). It was originally termed acute myeloid
leukemia gene 2 and was later known as core-binding factor α 3 gene
(8) and polyomavirus enhancement
factor- binding protein gene 2 (9).
The RUNX3 gene is located at 1p36.1 of the short arm chromosome 1
in humans and chromosome 4 in mice. The gene length is
approximately 67 kb and it contains two promoters, P1 and P2, and
six exons. The RUNX3 protein is a crucial regulatory factor in the
TGF-β signaling pathway. RUNX3 deletion results in the limited
function of Smad proteins and the promotion of TGF-β signaling,
which leads to tumor development (10).
Decreased RUNX3 expression or deletion are mainly
due to methylation or allelic loss. For example, the high
methylation of the RUNX3 CpG island is closely correlated with
cancer incidence and may be a useful diagnostic biomarker (11). On the other hand, a decreased RUNX3
expression or deletion is correlated to the prognosis of breast
cancer (12), bladder cancer
(13), pancreatic cancer (14) and other types of cancer. Currently,
the association of RUNX3 gene promoter methylation in lung cancer
and its clinical features is unknown. In this study, the
methylation-specific polymerase chain reaction (MSP) method was
used to detect RUNX3 gene promoter methylation in NSCLC and healthy
adjacent tissues. In addition, we analyzed its association with
clinical and pathological features of lung cancer to reveal the
potential clinical significance of RUNX3 gene promoter methylation
in the diagnosis of NSCLC.
Materials and methods
Clinical data
Specimens were collected from 58 patients with NSCLC
by surgical resection between January 2008 and December 2010 at The
Affiliated Jangyin People’s Hospital of Southeast University
Medical College, China. All specimens were pathologically diagnosed
as NSCLC by biopsy, and none of the subjects received pre-operative
radiotherapy, chemotherapy or other cancer treatments. The subjects
comprised 36 males and 22 females, aged 38–72 years, with a median
age of 57 years and a mean age of 56.6 (±8.7) years. Other
characteristics included: squamous cell carcinoma (n=26),
adenocarcinoma (n=32); clinical stages I and II (n=25), clinical
stages III and IV (n=33); lymph node metastasis (n=34), no lymph
node metastasis (n=24); highly differentiated tumor (n=35), poorly
differentiated tumor (n=23); smoking history (n=42), and no smoking
history (n=16). Each subject specimen contained distinct NSCLC
tissue and corresponding normal adjacent tissue. The specimens were
frozen and stored in liquid nitrogen immediately after
sampling.
Experimental methods
Reagents and primers
DNA extraction kits were purchased from Beijing
Tiangen Biochemistry Technology Limited Company (Beijing, China),
and the methylation kits were purchased from Zymo Research
Corporation (Irvine, California, USA). Primers were synthetized by
Takara Biotech Co. (Dalian, China).
RUNX3 gene promoter methylation
analysis
Genomic DNA was extracted from fresh tissue
according to kit instructions. Genomic DNA was modified with
sulfite. The methylation modification was performed for the genomic
DNA according to kit instructions, and the modified genomic DNA was
stored at −20°C until further use. DNA was purified and recovered
for MSP analysis. The primers for RUNX3 gene promoter methylation
and demethylation are available in the literature (15). The methylated primer sequence was:
forward: 5′-ATAATAGCGGTCGTTAGGGCGTCG-3′; and reverse:
5′-GCTTCTACTTTCCCACTTCTCACA-3′. The non-methylated primer sequence
was: forward: 5′-ATAATAGTTGTT GTTAGGGTGTTG-3′; and reverse:
5′-ACTTCTACTTTC CCACTTCTCACA-3′. The PCR reaction system was 25 μl,
including 10X PCR buffer, 1.5 mmol/l MgCl2, 10 mmol/l
dNTP, 0.5 mmol/l forward and reverse primers and 1 unit Taq DNA
polymerase. PCR conditions were as follows: denaturation at 94°C
for 3 min, then at 94°C for 30 sec, at 55°C (methylated) or 56°C
(non-methylated) for 90 sec, and at 72°C for 60 sec, 35 cycles in
total, and finally at 72°C for 10 min. PCR products were analyzed
by agarose electrophoresis (1.0%) and visualized with
ImageMaster® VDS.
Statistical methods
SPSS 13.0 software was used to process the data. The
four-cell table χ2 test was used to compare the
methylation differences between the RUNX3 gene promoter groups. The
above hypothesis test was two-sided with a test level (α) of 0.05;
p<0.05 was considered to be statistically significant.
Results
Test results of RUNX3 gene promoter
methylation
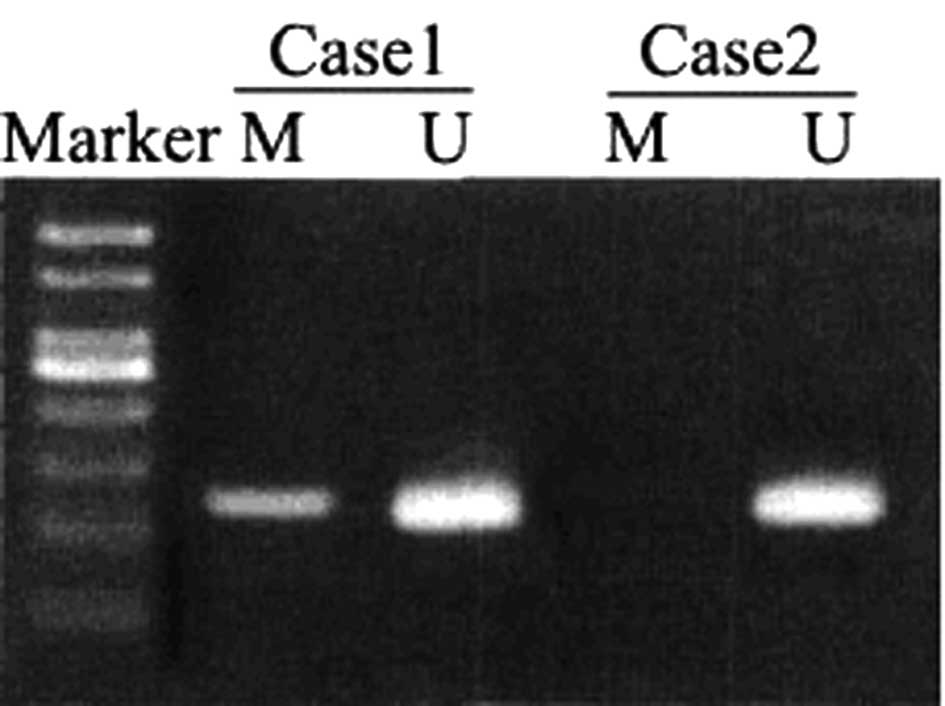
Among the 58 cases of NSCLC, 26 had RUNX3 gene
promoter methylation, giving a relevance ratio of 44.8%; whereas 10
samples from the normal adjacent tissues had RUNX3 gene promoter
methylation, giving a relevance ratio of 17.2%. The methylation
rate of RUNX3 gene promoter in the NSCLC tissue was significantly
higher than that in the normal adjacent tissue
(χ2=10.311, p=0.001). The PCR electrophoresis results
are shown in Fig. 1; Case 1 is
methylated RUNX3 and Case 2 is non-methylated RUNX3.
The correlation between RUNX3 gene
promoter methylation and clinicopathological characteristics
Table I shows that
RUNX3 gene promoter methylation was correlated to the clinical
stage, lymph node metastasis and degree of differentiation.
Patients in clinical stages III and IV had a significantly higher
methylation relevance ratio (57.6%) than patients in clinical
stages I and II (28.0%, p=0.025). Patients with lymph node
metastasis had a significantly higher methylation relevance ratio
(55.9%) than those without lymph node metastasis (29.2%, p=0.044).
Patients with poorly differentiated tumors also had a significantly
higher methylation relevance ratio (69.6%) than those with
moderately- or highly-differentiated tumors (28.6%, p=0.002).
However, the RUNX3 gene promoter methylation relevance ratio was
not significantly different by gender, age, pathological type and
smoking history (p>0.05).
 | Table ICorrelation between methylation of
RUNX3 gene promoter and clinicopathological characteristics [n
(%)]. |
Table I
Correlation between methylation of
RUNX3 gene promoter and clinicopathological characteristics [n
(%)].
| Clinical data | N | Methylation | Non-methylation | χ2 | P-value |
|---|
| Gender |
| Male | 36 | 14 (38.9) | 22 (61.1) | | |
| Female | 22 | 12 (54.5) | 10 (45.5) | 1.353 | 0.245 |
| Age |
| <60 years | 34 | 15 (41.1) | 18 (55.9) | | |
| ≥60 years | 24 | 11 (45.8) | 14 (54.2) | 0.017 | 0.897 |
| Pathological
type |
| Squamous cell
carcinoma | 26 | 13 (50.0) | 13 (50.0) | | |
| Adenocarcinoma | 32 | 13 (40.6) | 19 (59.4) | 0.510 | 0.475 |
| Clinical staging |
| Stage I+II | 25 | 7 (28.0) | 18 (72.0) | | |
| Stage III+IV | 33 | 19 (57.6) | 14 (42.4) | 5.031 | 0.025 |
| Lymph node
metastasis |
| No | 34 | 7 (29.2) | 17 (70.8) | | |
| Yes | 24 | 19 (55.9) | 15 (44.1) | 4.060 | 0.044 |
| Differentiation
degree |
| Poorly
differentiated | 23 | 16 (69.6) | 7 (30.4) | | |
| Moderately and
highly differentiated | 35 | 10 (28.6) | 25 (71.4) | 9.431 | 0.002 |
| Smoking history |
| No | 16 | 10 (62.5) | 6 (37.5) | | |
| Yes | 42 | 16 (38.1) | 26 (61.9) | 2.790 | 0.095 |
Discussion
The RUNX3 gene is a recently discovered tumor
suppressor gene that regulates cell growth and apoptosis and plays
a significant regulatory role in transcription and cell signal
transduction. RUNX3 functions impact both normal physiological
development and tumor development, and a reduced function of RUNX3
plays a role in the development of various human malignancies
(16). Numerous studies have shown
that a decreased RUNX3 expression, RUNX3 deletion, or high
methylation of the RUNX3 CpG island are common in gastric, liver,
lung, breast, pancreatic and colorectal cancer. It has also been
confirmed that RUNX3 methylation is tumor-specific. Tan et
al (17) examined the presence
of methylated RUNX3, p16, RASSF1A and CDH1 in serum from 70 cases
of cancer (metastatic breast cancer, NSCLC, gastric cancer,
pancreatic cancer, colorectal cancer and hepatocellular carcinoma).
Serum specimens from 10 healthy volunteers were used as controls.
RUNX3 methylation was present in 44 patients. Of the four genes
screened, at least one methylated gene was present in 62 patients,
while a 3-gene combined detection (without RUNX3) was present in 50
cases. No methylation was detected in serum specimens from the 10
healthy volunteers. Therefore, as serum test markers, methylation
of RUNX3 is more sensitive, and the combined detection approach of
multiple genes (including the RUNX3 gene) can improve cancer
diagnosis. The results from the current study demonstrated that the
methylation rate of the RUNX3 gene promoter in NSCLC tissues was
significantly higher than that in the normal adjacent lung tissues
(44.8 versus 17.2%), indicating that RUNX3 promoter methylation was
common in NSCLC.
The study performed by Sato et al (18) indicated that the RUNX3 methylation
rate in NSCLC patients without a smoking history was significantly
higher than that in patients with a smoking history, and that the
RUNX3 methylation rate in adenocarcinoma patients was higher than
that in squamous cell carcinoma patients. For adenocarcinoma,
abnormal RUNX3 methylation was the essential mechanism for the
inactivation of RUNX3 expression, and gene silencing was essential
for the occurrence of lung cancer. Yanagawa et al (19)demonstrated that RUNX3 methylation in
NSCLC tissues was not significantly different between groups by age
(<69 versus >70 years), gender, smoking history or presence
of pleural invasion (19,20). RUNX3 methylation was higher in
patients in stage I as compared to stages II to III, but the
difference was not statistically significant. The RUNX3 methylation
rate in adenocarcinoma was significantly higher than that in
squamous cell carcinoma. We speculated that RUNX3 methylation has a
greater impact on NSCLC progression during earlier stages by
exhibiting distant metastasis beyond stage H/III. Li et al
(21) demonstrated that a decreased
RUNX3 mRNA expression correlated with abnormal methylation status.
The detected methylation rate of the RUNX3 gene promoter was 28% in
adenocarcinoma, 12% in squamous cell carcinoma and 58% in large
cell carcinoma. No methylation was detected in normal lung tissues,
and RUNX3 methylation increased with increasing clinical stage.
The results of the current study have shown that
RUNX3 gene promoter methylation was correlated to clinical stage,
lymph node metastasis and degree of differentiation. Patients in
clinical stages III and IV had a significantly higher methylation
relevance ratio (57.6%) than patients in stages I and II (28.0%),
and patients with lymph node metastasis had a significantly higher
methylation relevance ratio (62.5%) than those without lymph node
metastasis (32.4%). Patients with poorly-differentiated tumors also
had a significantly higher methylation relevance ratio (65.2%) than
those who with moderately- or highly-differentiated tumors (31.4%).
However, the RUNX3 methylation relevance ratio was not
significantly different by gender, age, pathological type and
smoking history. Therefore, this study demonstrated that RUNX3
methylation had no significant correlation with pathological type
or smoking history. The results may have been affected by study
factors such as sample size and geographic and population
differences. Further research on these associations is
required.
In conclusion, RUNX3 methylation plays a significant
role in the occurrence, development and postoperative recurrent
metastasis of NSCLC. RUNX3 methylation may be an essential
postoperative prognostic biomarker for NSCLC. Since changes in
methylation epigenetic inheritance are reversible, clinical
treatment through demethylation (22,23)
may be useful to delay recurrent metastasis and improve prognosis.
This approach brings new direction and hope for cancer treatment
through gene-targeted therapy.
References
|
1
|
Kim JS, Kim JW, Han J, Shim YM, Park J and
Kim DH: Cohypermethylation of p16 and FHIT promoters as a
prognostic factor of recurrence in surgically resected stage I
non-small cell lung cancer. Cancer Res. 66:4049–4054. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Esteller M: Epigenetics provides a new
generation of oncogenes and tumour-suppressor genes. Br J Cancer.
94:179–183. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yamada Y, Jackson-Grusby L, Linhart H,
Meissner A, Eden A, Lin H and Jaenisch R: Opposing effects of DNA
hypomethylation on intestinal and liver carcinogenesis. Proc Natl
Acad Sci USA. 102:13580–13585. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Carraway H and Herman J: Montoring
methylation changes in caner. Methods Mol Biol. 383:187–202.
2007.
|
|
5
|
Chim CS, Liang R, Leung MH and Kwong YL:
Aberrant gene methylation implicated in the progression of
monoclonal gammopathy of undetermined significance to multiple
myeloma. J Clin Pathol. 60:104–106. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Durst KL and Hiebert SW: Role of RUNX
family members in transcriptional repression and gene silencing.
Oncogene. 23:4220–4224. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Levanon D, Negreanu V, Bernstein Y, Bar-Am
I, Avivi L and Groner Y: AML1, AML2, and AML3, the human members of
the runt domain gene-family: cDNA structure, expression, and
chromosomal localization. Genomics. 23:425–432. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ito Y: Molecular basis of tissue-specific
gene expression mediated by the runt domain transcription factor
PEBP2/CBF. Genes Cells. 4:685–696. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bae SC and Choi JK: Tumor suppressor
activity of RUNX3. Oncogene. 23:4336–4340. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Miyazono K, Suzuki H and Imamura T:
Regulation of TGF-beta signaling and its roles in progression of
tumors. Cancer Sci. 94:230–234. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Blyth K, Cameron ER and Neil JC: The RUNX
genes: gain or loss of function in cancer. Nat Rev Cancer.
5:376–387. 2005. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jiang Y, Tong D, Lou G, Zhang Y and Geng
J: Expression of RUNX3 gene, methylation status and
clinicopathological significance in breast cancer and breast cancer
cell lines. Pathobiology. 75:244–251. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kim EJ, Kim YJ, Jeong P, Ha YS, Bae SC and
Kim WJ: Methylation of the RUNX3 promoter as a potential prognostic
marker for bladder tumor. J Urol. 180:1141–1145. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Nomoto S, Kinoshita T, Mori T, Kato K,
Sugimoto H, Kanazumi N, Takeda S and Nakao A: Adverse prognosis of
epigenetic inactivation in RUNX3 gene at 1p36 in human pancreatic
cancer. Br J Cancer. 98:1690–1695. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Waki T, Tamura G, Sato M, Terashima M,
Nishizuka S and Motoyama T: Promoter methylation status of
DAP-kinase and RUNX3 genes in neoplastic and non-neoplastic gastric
epithelia. Cancer Sci. 94:360–364. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Friedrich MJ, Rad R, Langer R, Voland P,
Hoefler H, Schmid RM, Prinz C and Gerhard M: Lack of RUNX3
regulation in human gastric cancer. J Pathol. 210:141–146. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tan SH, Ida H, Lau QC, Goh BC, Chieng WS,
Loh M and Ito Y: Detection of promoter hypermethylation in serum
samples of cancer patients by methylation-specific polymerase chain
reaction for tumour suppressor genes including RUNX3. Oncol
Rep. 18:1225–1230. 2007.
|
|
18
|
Sato K, Tomizawa Y, Iijima H, Saito R,
Ishizuka T, Nakajima T and Mori M: Epigenetic inactivation of the
RUNX3 gene in lung cancer. Oncol Rep. 15:129–135. 2006.
|
|
19
|
Yanagawa N, Tamura G, Oizumi H, Kanauchi
N, Endoh M, Sadahiro M and Motoyama T: Promoter hypermethylation of
RASSF1A and RUNX3 genes as an independent prognostic prediction
marker in surgically resected non-small cell lung cancers. Lung
Cancer. 5:131–138. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yanagawa N, Tamura G, Oizumi H, et al:
Promoter hypermethylation of tumor suppressor and tumor-related
genes in non-small cell lung cancers. Cancer Sci. 94:589–592. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Li QL, Kim HR, Kim WJ, Choi JK, Lee YH,
Kim HM, Li LS, Kim H, Chang J, Ito Y, Youl Lee K and Bae SC:
Transcriptional silencing of the RUNX3 gene by CpG hypermethylation
is associated with lung cancer. Biochem Biophys Res Commun.
314:223–228. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Herranz M and Esteller M: DNA methylation
and histone modifications in patients with cancer: potential
prognostic and therapeutic targets. Methods Mol Biol. 361:25–62.
2007.PubMed/NCBI
|
|
23
|
Fojtova M, Piskala A, Votruba I, Otmar M,
Bartova E and Kovarik A: Efficacy of DNA hypomethylating capacities
of 5-aza-2′-deoxycytidine and its alpha anomer. Pharmacol Res.
55:16–22. 2007.PubMed/NCBI
|