Introduction
Giant cell tumor (GCT) of the bone is a relatively
common primary bone tumor, accounting for 5% of all invasive
primary bone tumors. Treatment with simple curettage often results
in a high local recurrence rate. Tumor resection and reconstruction
with prosthesis or a large segment allograft has a low rate of
local recurrence; however, the patient’s native joint function
becomes significantly impaired. With the development of surgical
techniques and an increased understanding of the biological
behaviour of GCT, curettage has gradually been replaced by
aggressive curettage (1). This
implies using high-speed burr to grind the paratumorous bone,
expanding the range of curettage and using chemical agents (phenol,
alcohol and bone cement) to process the bone cavity, to finally
achieve marginal excision. We followed up 16 patients with GCT of
the bone who had been treated in the Orthopedic Department of the
General Hospital of Jinan Military Commanding Region, China, from
January 2008 to June 2011. These patients had received aggressive
curettage, bone cement filling, internal fixation and oral
administration of bisphosphonates. In the follow-up, tumor
recurrence and joint function were observed in order to evaluate
the clinical outcomes.
Patients and methods
Patients
Among the 16 patients with GCT in the distal femur
that were treated in our hospital from January 2008 to June 2011,
there were seven males and nine females, aged 27–78 years (mean, 38
years). There were 12 cases of primary GCT and four cases of
recurrent GCT. This study was approved by the ethics committee of
the Orthopedic Department, The General Hospital of Jinan Militray
Commanding Region, Jinan, Shandong, China. Informed consent was
obtained from the patients.
Clinical diagnosis and
classification
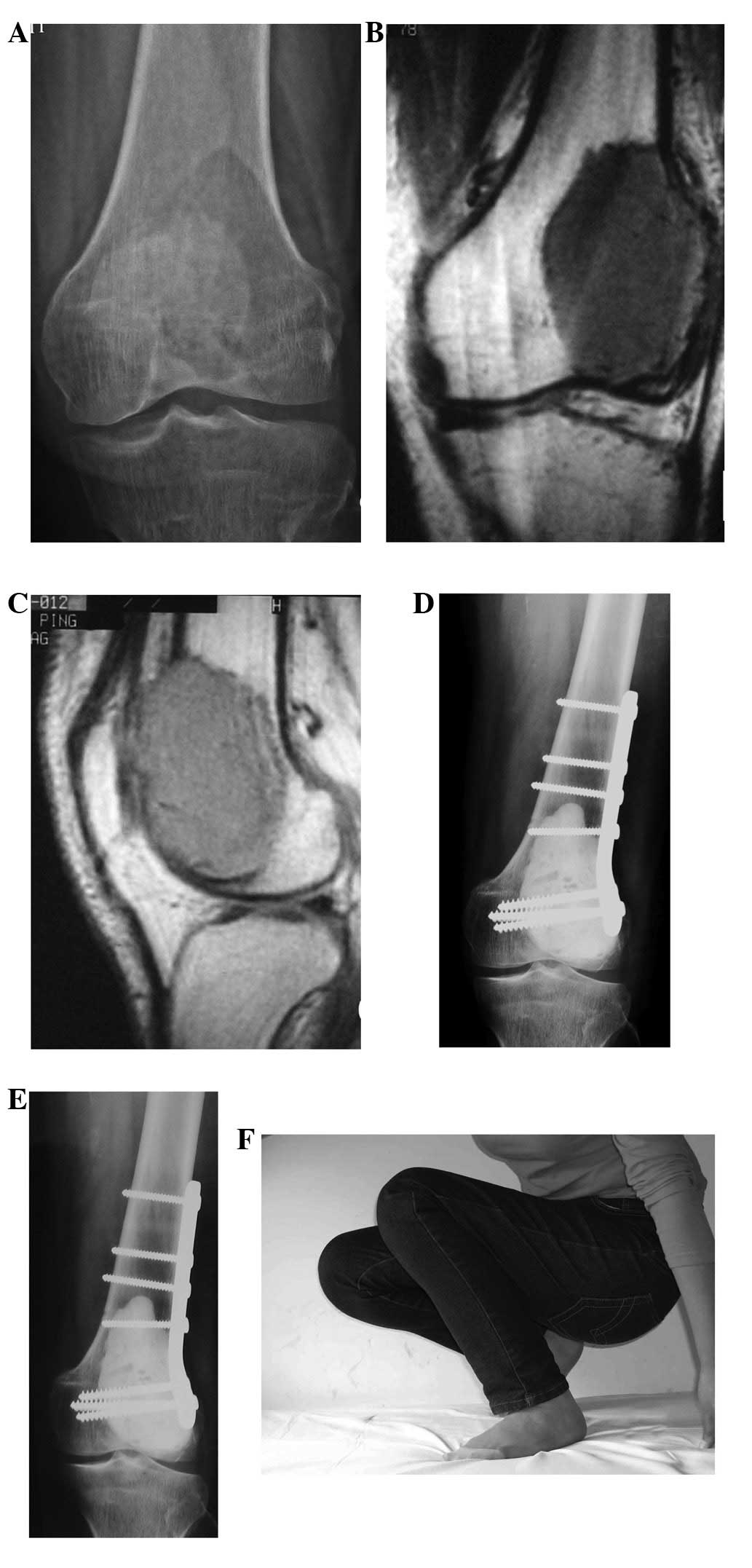
Patients were evaluated with clinical and imaging
data following examination with X-ray, CT and MRI. Preoperative
biopsy was conducted on the 12 patients with primary GCT, in order
to confirm the diagnosis. According to the Campanacci grading
system (2); two cases of grade I,
11 cases of grade II and three cases of grade III were present in
this group.
Surgical technique and adjuvant
therapy
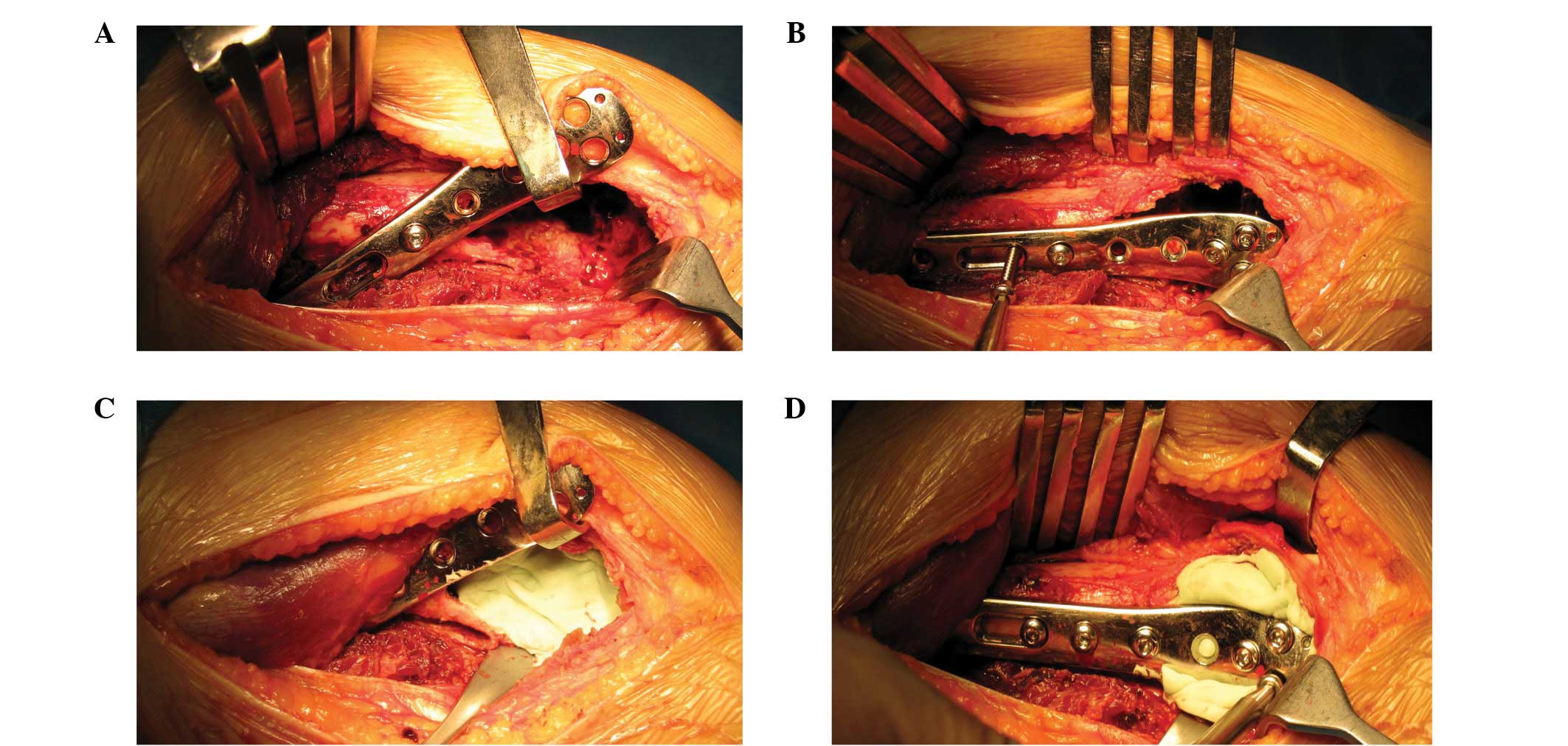
The surgical approach was determined based on the
location of the lesion. The tumor was exposed completely to
separate the normal adjacent soft tissues. While protecting the
adjacent soft tissues, a bone window was opened as wide as possible
from the lesion edge. The tumor was then removed with a scraper,
the curettage was further expanded with a high-speed burr and the
paratumorous cortical bone was ground to form smooth surface. The
spongy bone was ground 0.5–1.0 cm and the surface of exposed
cortical bone was burned using an electric knife. The lesion was
then washed with a large volume of distilled water under pulse
pressure. An appropriate anatomical steel plate was selected and
the healthy diaphysis, as well as the ground paratumorous cortical
bone, were drilled and tapped. Screws of the appropriate length
were selected and screwed in at the correct entry angle. All screws
were then removed, apart from one screw that served to temporarily
fix the steel plate, which was then lifted to fill the bone with
cement. After bone cement filling, all screws were immediately
tightened along the original threads (Fig. 1).
All patients were administered postoperative, oral
alendronate sodium tablets (10 mg/day); drug administration was
pulsed for one month every two months, and this continued for two
years.
Follow-up
Following surgery, all patients were followed up
regularly. The follow-up time was 23–53 months (median, 28 months).
The follow-up review included the following: Lung CT scan once
every six months and X-ray examination once every three months for
two years, and then every six months after the first two years.
Limb function was simultaneously evaluated by Enneking limb
reconstruction scores (3).
Results
Oncology results
All patients were followed up. The median follow-up
time was 28 months (23–53 months) and no local recurrence or
metastasis was observed.
Limb function
All incisions healed well. The postoperative
training of the knee joint was initiated three to five days after
surgery and the weight-bearing exercise began 14 days after
surgery. Limb function had essentially recovered after one month.
Only one patient suffered from pain when bending the knee, as a
screw was too long. Repeat surgery was carried out to remove the
screw, and the postoperative knee function returned to normal.
Enneking limb function scores of this group of patients ranged from
24–29 (average, 26.7) (Fig. 2).
Imaging results
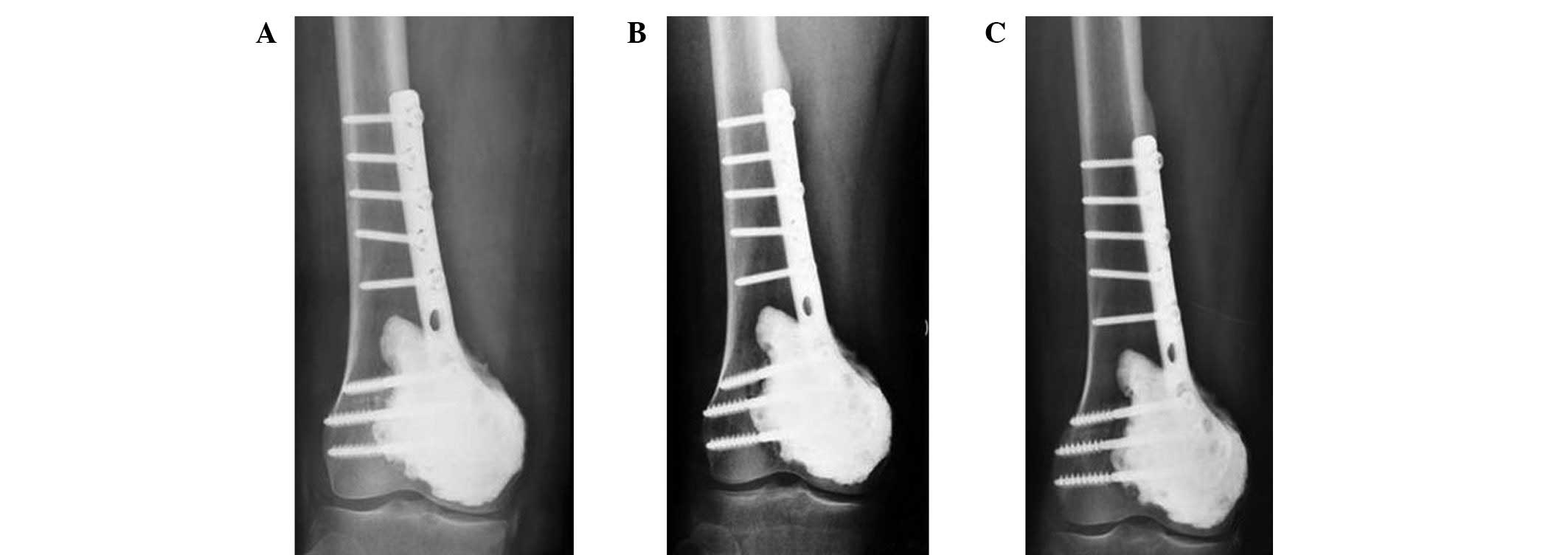
All patients received X-ray examination once every
three months within the first two years after surgery, and then
once every six months after two years. All internal fixations
remained in place in this group of patients and no subchondral bone
fracture was identified. Four patients were observed to have lucent
zones evenly distributed around the bone cement during 4–13 months
(average, 8 months) of follow-up (Fig.
3). However, these lucent zones demonstrated no further
progression in further follow-up.
Adverse drug reaction
Two patients suffered from acid reflux, heartburn
and other mild gastrointestinal symptoms after oral alendronate,
which disappeared following treatment of these symptoms.
Discussion
GCT is a relatively common primary bone tumor.
Although GCT is benign, it is typically clinically treated with
intralesional curettage and en bloc resection, due to its strong
local invasion and high postoperative recurrence rate. Simple
intralesional surgery has a relatively high recurrence rate. As
studies have demonstrated, the recurrence rate for GCT treated by
intralesional curettage plus bone grafting was 29–75% (4). Although en bloc resection has a lower
recurrence rate, it damages the patient’s joint function and
requires reconstruction with a large segment allograft or
prosthesis. In the case of long-term survival, the emergence of
various complications becomes inevitable; therefore, the long-term
outcomes of en bloc resection are poor.
With the gradually increasing awareness of the local
invasion of GCT and the development of surgical techniques, the
concept of aggressive curettage has arisen. This implies that the
affected bone and wall are ground intralesionally with a high-speed
burr, washed under pulse pressure and treated with chemical agents
(including phenol, alcohol and bone cement) to achieve marginal
excision. Algawahmed et al(5) used meta-analysis to analyze 13
articles regarding the intralesional application of a high-speed
burr in GCT, with or without auxiliary treatments, and identified:
i) 66 recurrences (20%) out of 323 cases that had received
treatment with both a high-speed burr and another auxiliary method,
and ii) 15 recurrences (23%) out of 64 patients who had received
simple treatment with a high-speed burr only. The authors proposed
that using a high-speed burr is the most effective way to reduce
the local recurrence rate. Treatment of GCT with aggressive
curettage retains the limb function and reduces the recurrence rate
to a minimum. However, there remains a lack of uniform surgical
recommendation regarding aggressive curettage. We propose that a
comprehensive preoperative assessment of the biological behavior of
GCT, including tumor growth, clinical progression, as well as
pathological and imaging manifestations, should be conducted.
Aggressive curettage may be performed in limb GCT cases without
pathological fracture, with limited tumor location and extent. It
is not necessarily a contraindication to use intralesional
curettage for patients with Campanacci grade III tumors.
Limb GCT often occurs around the knee, and most
patients have a long-term survival, which results in a reasonably
high demand on the limb function. Intralesional curettage with bone
grafting may require a large amount of bone graft, and it is
difficult to differentiate the bone graft absorption from
recurrence. Moreover, the required protective weight-bearing before
bone healing interferes with the recovery of joint function. Bone
cement as a filler material has long been used in GCT lesion
filling and exhibits numerous advantages. It reconstructs bone
defects immediately, restores bone continuity and facilitates early
postoperative weight-bearing. In a biomechanical study by Frassica
et al(6), with the
application of bone cement reconstruction, the mechanical strength
of bone defects was demonstrated to be restored to 98%.
Additionally, the heat released by bone cement polymerization
exerts a high-temperature inactivation effect on the lesion edge
and further reduces the recurrence rate. In a follow-up study by
Kivioja et al(7), the
recurrence rate of 147 patients with intra-lesional curettage and
bone cement filling was 22%, while that of 47 cases receiving
curettage and bone grafting was 52%. Moreover, Kafchitsas et
al(8) performed curettage on 38
GCT patients, among which 21 patients who had received bone cement
filling demonstrated a recurrence rate of 23.8%, while the other 17
patients who had received bone grafting displayed a postoperative
recurrence rate of 52.9%. Bone cement filling is also beneficial as
it enables tumor recurrence to be detected early-on in X-ray film.
Kafchitsas et al(8) followed
up 21 patients with bone cement filling by imaging, and revealed
that a gradually progressive lucent zone between the bone and bone
cement was present in four out of the five recurrent cases. The
authors propose that this phenomenon may be used as a reliable
indicator of tumor recurrence. During the follow-up, they also
observed that patients who had received bone cement filling
demonstrated a 1.4 mm (average) lucent zone with a hardened edge
between the bone and bone cement in the first six months after
surgery. However, the lucent zones typically did not progress and
affect the fixation. Furthermore, the width of the lucent zone was
related to the volume of bone cement; the authors hypothesized that
the thermal burns by the bone cement and the micromovement cause
the appearance of these lucent zones, and that the gradually
progressing lucent zones initiate tumor recurrence. Four patients
in the present study exhibited evenly distributed lucent zones,
with hardened edges, around the bone cement during the first 4–13
months (mean, 8 months) of follow-up. These zones were speculated
to be related to the thermal burns of bone cement; however, further
follow-up indicated that these lucent zones demonstrated no further
progression.
GCT often involves the subchondral bone and is
sometimes situated near to the articular cartilage. Treatment with
bone cement, thermal burns or micromovement theoretically causes
cartilage degeneration and fracture, leading to the occurrence of
osteoarthritis. Fraquet et al(9) treated 30 patients with long bone GCT
by tumor curettage and bone cement filling, 73% of which exhibited
GTC close to the articular cartilage. Following an average of 6.4
years’ follow-up, only two patients manifested mild joint
degeneration. von Steyern et al(11) treated nine patients with GCT that
were close to the knee joint with tumor curettage and bone cement
filling. The distances between bone cement and articular cartilage
were 0–3.5 mm (mean, 1.0 mm), of which three were 0 mm. During the
6–16 years of follow-up, only one case exhibited narrowness of the
medial joint space in the postoperative weight-bearing X-ray.
Although MR confirmed the existence of articular cartilage, delayed
gadolinium-enhanced MR scan indicated articular cartilage injury.
The authors stressed that the preoperative articular cartilage must
be continuous, and noted that the hardness of subchondral filler is
an important factor affecting the degeneration of articular
cartilage. Previous animal experiments have confirmed that
replacement of subchondral bone with bone cement does not reduce
its strength (10). In addition,
the nutrition of articular cartilage mainly depends on synovium and
is less dependent on blood supply; therefore, the effect of bone
cement filling on articular cartilage is not as serious as
theoretically predicted. In this study, none of the 16 patients
manifested clinical symptoms of osteoarthritis; however, due to the
relatively short follow-up time, further follow-up observations are
required.
Although there are few studies regarding the
necessity and timing of internal fixation after bone cement
filling, we propose that the internal fixation is necessary.
Fraquet et al(9) indicated
that without internal fixation, the stress-induced bone cement
loosening would cause further resorption of the surrounding bone
and pathologic fractures of the subchondral bone, leading to the
bead effect of bone cement. Fixation is capable of locking the bone
cement and bone cladding into one, hence preventing the occurrence
of loosening. The authors treated 16 out of 30 cases of GCT of the
long bone with internal fixation, and there was no bead effect
observed with the bone cement. The current, commonly used internal
fixation methods include fixations with steel plate or medullary
cavity-implanted multiple Steinmann pins or cross screws. Toy et
al(12) conducted in
vitro biomechanical studies and revealed that bone cement
filling of the distal femoral bone defect, accompanied by internal
fixation using cross screws, generated significantly better
biomechanical strength than that of simple bone cement filling, or
bone cement filling in combination with fixation using
intramedullary Steinmann pins. Uglialoro et al(13) demonstrated that the biomechanical
strength of bone cement filling of the distal femoral defect,
accompanied by internal steel plate fixation, is superior to that
of bone cement filling in combination with fixations using
intramedullary Steinmann pins or cross screws.
Bisphosphonate drugs have significant therapeutic
effects on bone-metastasized tumors and osteoclast-mediated bone
destructions, such as in GCT of the bone. Clinical studies have
been conducted with regard to treating GCT with bisphosphonates as
an adjuvant therapy. Tse et al(15) performed a retrospective controlled
study of 44 cases of GCT patients. Of the 44 cases, 24 patients
received two courses of preoperative and three courses of
postoperative intravenous infusions of pamidronate disodium or
zoledronic acid, followed by three months of oral administration of
clodronate disodium. In the follow-up of 48–115 months, the
recurrence rates in drug treatment and control groups were 4.2%
(1/24) and 30% (6/20), respectively. However, due to the small
experimental sample size and the fact that the follow-up was
short-term (as well as many other influential factors), the ability
of bisphosphonates to reduce the recurrence rate of GCT remains
inconclusive. In this study, all patients received oral alendronate
sodium tablets (10 mg/day) for two years with a one month interval
between each two months of oral administration. The main side
effects of alendronate sodium are acid reflux, heartburn and
abdominal pain, among other gastrointestinal symptoms. The patients
in this study manifested only low fever, acid reflux, heartburn and
other mild adverse reactions, which disappeared after symptomatic
treatment, suggesting a good safety of the drug.
In summary, we have applied intralesional aggressive
curettage, bone cement filling and plate internal fixation in 16
GCT cases. This was followed by postoperative oral administration
of bisphosphonate drugs (alendronate sodium), and no recurrence has
been observed since. For clinical practice, our method has
advantages including being easy to perform, ideal recovery of the
limb function, low rate of short-term recurrence and acceptance by
patients. The median follow-up time of this study was 28 months;
therefore, a greater number of cases and longer follow-up times
need to be investigated in the future.
References
|
1.
|
Errani C, Ruggieri P, Asenzio MA, Toscano
A, Colangeli S, Rimondi E, Rossi G, Longhi A and Mercuri M: Giant
cell tumor of the extremity: A review of 349 cases from a single
institution. Cancer Treat Rev. 36:1–7. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Campanacci M, Baldin N, Boriani S and
Sudanese A: Giant cell tumour of bone. J Bone Joint Surg Am.
69:106–114. 1987.
|
|
3.
|
Enneking WF, Dunham W, Gebhardt MC,
Malawar M and Pritchard DJ: A system for the functional evaluation
of reconstructive procedures after surgical treatment of tumors of
the musculoskeletal system. Clin Orthop Relat Res. 286:241–246.
1993.PubMed/NCBI
|
|
4.
|
Klenke FM, Wenger DE, Inwards CY, Rose PS
and Sim FH: Recurrent giant cell tumor of long bones: analysis of
surgical management. Clin Orthop Relat Res. 469:1181–1187. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Algawahmed H, Turcotte R, Farrokhyar F and
Ghert M: High-speed burring with and without the use of surgical
adjuvants in the intralesional management of giant cell tumor of
bone: A systematic review and meta-analysis. Sarcoma. 2010:1–5.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Frassica FJ, Sim FH, Pritchard DJ and Chao
EY: Subchondral replacement: a comparative analysis of
reconstruction with methyl methacrylate or autogenous bone graft.
Chir Organi Mov. 75:189–190. 1990.PubMed/NCBI
|
|
7.
|
Kivioja AH, Blomqvist C, Hietaniemi K,
Trovik C, Walloe A, Bauer HC, Jorgensen PH, Bergh P and Follerås G:
Cement is recommended in intralesional surgery of giant cell
tumors: a Scandinavian Sarcoma Group study of 294 patients followed
for a median time of 5 years. Acta Orthop. 79:86–93.
2008.PubMed/NCBI
|
|
8.
|
Kafchitsas K, Habermann B, Proschek D,
Kurth A and Eberhardt C: Functional results after giant cell tumor
operation near knee joint and the cement radiolucent zone as
indicator of recurrence. Anticancer Res. 30:3795–3799.
2010.PubMed/NCBI
|
|
9.
|
Fraquet N, Faizon G, Rosset P, Phillipeau
JM, Waast D and Gouin F: Long bones giant cells tumors: treatment
by curretage and cavity filling cementation. Orthop Traumatol Surg
Res. 95:402–406. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Frassica FJ, Gorski JP, Pritchard DJ, Sim
FH and Chao EY: A comparative analysis of subchondral replacement
with polymethylmethacrylate or autogenous bone grafts in dogs. Clin
Orthop. 293:378–379. 1993.PubMed/NCBI
|
|
11.
|
von Steyern FV, Kristiansson I, Jonsson K,
Mannfolk P, Heinegård D and Rydholm A: Giant-cell tumour of the
knee: the condition of the cartilage after treatment by curettage
and cementing. J Bone Joint Surg Br. 89:361–365. 2007.PubMed/NCBI
|
|
12.
|
Toy PC, France J, Randall RL, Neel MD,
Shorr RI and Heck RK: Reconstruction of noncontained distal femoral
defects with polymethylmethacrylate and crossed-screw augmentation:
a biomechanical study. J Bone Joint Surg Am. 88:171–178. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Uglialoro AD, Maceroli M, Beebe KS,
Benevenia J and Patterson FR: Distal femur defects reconstructed
with polymethylmethacrylate and internal fixation devices: a
biomechanical study. Orthopedics. 32:5612009. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Yang ZM, Tao HM, Yang DS, Ye ZM and Li WX:
The choice strategy of surgical treatment for giant cell tumor
close to the knee. Chin J Surg. 44:1693–1698. 2006.(In
Chinese).
|
|
15.
|
Tse LF, Wong KC, Kumta SM, Huang L, Chow
TC and Griffith JF: Bisphosphonates reduce local recurrence in
extremity giant cell tumor of bone: a case-control study. Bone.
42:68–73. 2008. View Article : Google Scholar : PubMed/NCBI
|