Introduction
The occurrence of an accessory spleen is not rare;
it affects approximately 10% of the general population, and 16% of
all cases are intrapancreatic (1),
However, the development of an epidermoid cyst of intrapancreatic
accessory spleen (IPAS) is not common, with 30 cases (2–29)
described in the literature since Davidson et al(2) described the first case of epidermoid
cyst of IPAS. Due to the difficulty in differentiating the lesion
from a cystic neoplasm of the pancreas by an imaging study
(4), the majority have been
diagnosed following surgical resection, with the exception of one
case by Itano et al(5).
Pre-operative diagnosis was mainly cystic neoplasm of the pancreas.
Herein, we report a case of 54-year-old female with an epidermoid
cyst of an IPAS and review the literature.
The study was approved by the ethics committee of
Chosun University Hospital, Gwangju, Korea (IRB No.: CHOSUN
2012-10-007). The committee approved the waiver of patient consent
for these cases.
Case report
A 54-year-old female with iron deficiency anemia was
admitted to hospital complaining of dizziness and abdominal
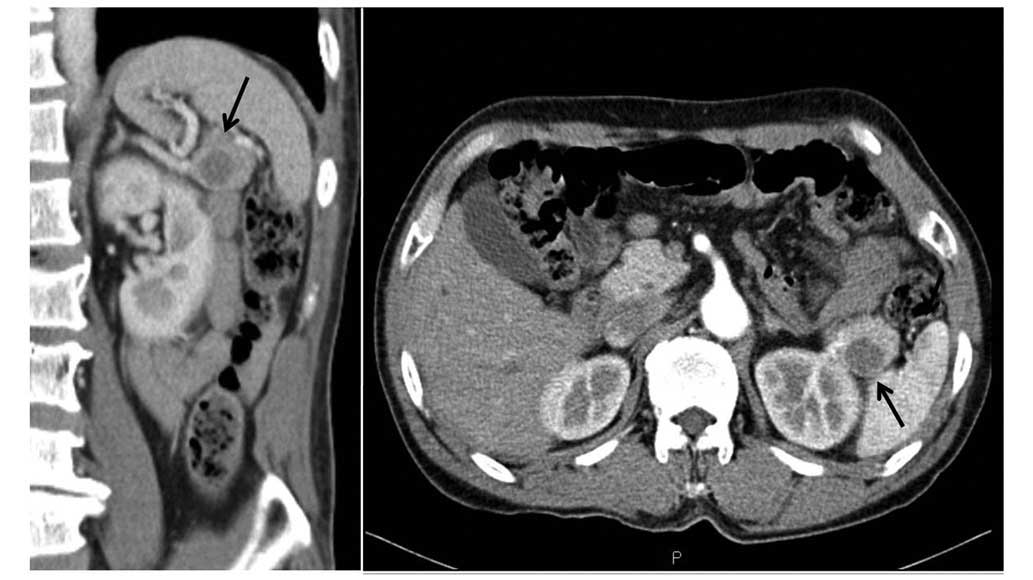
discomfort. During the clinical workup, a 2.3 cm-radiological-sized
cystic mass was detected in the tail of the pancreas by abdominal
computed tomography (CT; Fig. 1).
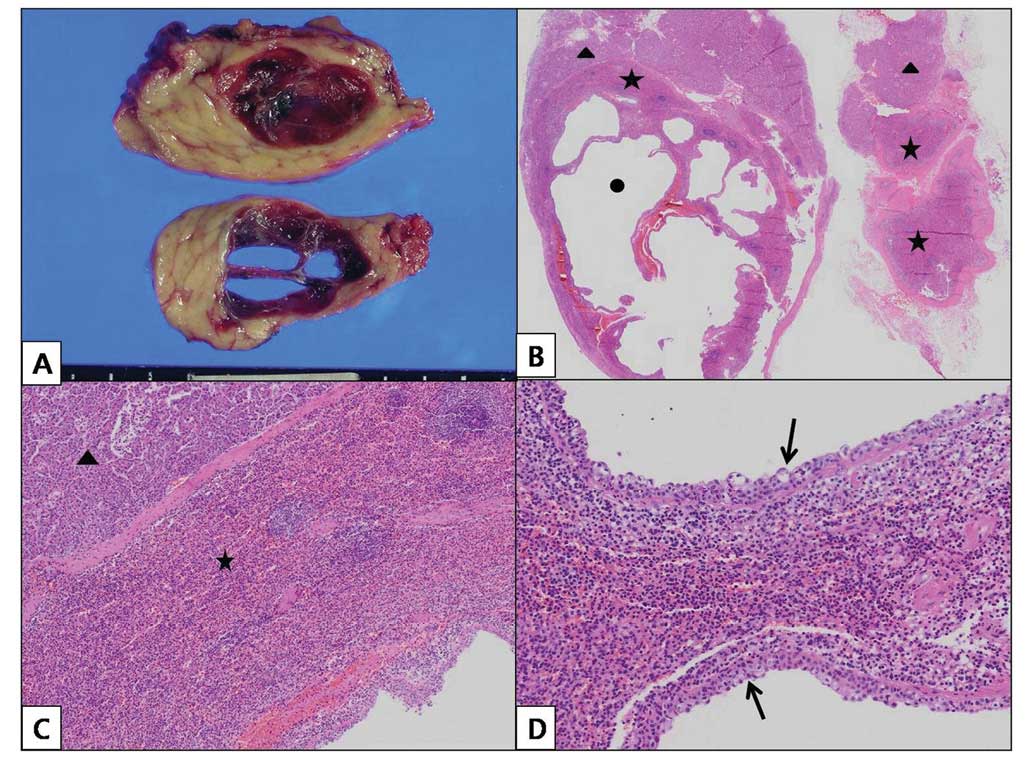
Distal pancreatectomy was performed upon clinical diagnosis of
pancreatic cancer. Grossly, the surgical specimen showed a
well-demarcated multilocular cystic mass within the pancreatic
parenchyma, measuring 2.0×1.5 cm (histoligcal size) and containing
dark serosanginous fluid. Microscopic investigation revealed that
the majority of the epithelial lining was comprised of multilayered
cuboidal epithelium with focal denudation. However, no atypical or
malignant changes were observed (Fig.
2). Immunohistochemical staining demonstrated that the
epithelial lining was reactive for cytokeratin (CK) and CK7. The
cystic wall demonstrated histologically normal splenic pulp tissue,
which was surrounded by a hyalinized fibrous band. The final
pathologic diagnosis was an epidermoid cyst arising from an IPAS.
The six-month post-operative course was uneventful.
Discussion
Approximately 16% of accessory spleens occur in or
around the tail of the pancreas (1). An epidermoid cyst in an IPAS is
extremely rare and was first described in 1980 by Davidson et
al(2). Following this, 30 cases
of epidermoid cyst of IPAS have been described in the literature.
Table I summarizes the 31 cases of
epidermoid cyst in an IPAS, including the case we describe here.
The cases involved 15 males and 16 females, with ages ranging from
12–70 years (mean, 46 years). All cysts were located in the
pancreatic tail. While 16 patients were asymptomatic, various
symptoms were observed in 14 patients, including weight loss,
nausea, vomiting, abdominal pain and discomfort, back pain,
epigastric pain and fever. Histological analysis revealed that the
cysts were solitary or multilocular, lined with keratinized or
non-keratinized stratified squamous epithelium or cuboidal
epithelium, and in some cases exhibiting mixed-form epithelium.
 | Table I.Summary of the 31 cases of epidermoid
cyst arising in intrapancreatic accessory spleen (IPAS), including
the present case. |
Table I.
Summary of the 31 cases of epidermoid
cyst arising in intrapancreatic accessory spleen (IPAS), including
the present case.
| No | First author
(Ref.) | Year | Age/Gender | Site | Symptoms | CA 19-9 | Size (cm) | Surgery | Epi. lining |
|---|
| 1 | Davidson (2) | 1980 | 40/M | Tail | WL, N | NR | 5.5 | DP&S | - |
| 2 | Hanada (3) | 1981 | 51/M | Tail | AP | NR | - | DP | - |
| 3 | Jibu (4) | 1987 | 37/M | Tail | - | - | 4.0 | - | - |
| 4 | Morohoshi (5) | 1991 | 32/M | Tail | AP | WNL | 6.0×5.0 | RC | SSE |
| 5 | Nakae(6) | 1991 | 37/F | Tail | AP | NR | | SPDP | |
| 6 | Tang (7) | 1994 | 38/M | Tail | ASx. | NR | 1.4 | DP | SSE |
| 7 | Furukawa (8) | 1998 | 45/M | Tail | ASx. | WNL | 2.0 | DP | SSE |
| 8 | Higaki (9) | 1998 | 46/F | Tail | Back pain | 201 | 3.0×3.0 | DP&S | SSE |
| 9 | Tateyama (10) | 1998 | 67/F | Tail | AP | 201 | 3.0 | DP | SSE |
| 10 | Sasou (11) | 1999 | 49/F | Tail | ASx. | WNL | 4.3×2.6 | DP | NSSE |
| 11 | Tsutsumi (12) | 2000 | 51/M | Tail | ASx. | WNL | 2.5 | DP | NSSE |
| 12 | Choi (13) | 2000 | 54/F | Tail | EP, N, V, WL | NR | 15.0×11.0 | E&S | KSSE |
| 13 | Horibe (14) | 2001 | 48/M | Tail | ASx. | 53 | 2.0×1.0 | DP | SSE |
| 14 | Sonomura (15) | 2002 | 45/F | Tail | EP | 159 | 3.5 | DP | SSE |
| 15 | Yokomizo (16) | 2002 | 38/M | Tail | ASx. | 410 | 2.7 | DP | NSSE |
| 16 | Fink (17) | 2002 | 12/F | Tail | Fever | NR | 10.0 | RC | NSSE |
| 17 | Kanazawa (18) | 2004 | 58/F | Tail | ASx. | 62 | 2.5 | SPDP | SSE |
| 18 | Ru (19) | 2007 | 41/M | Tail | ASx. | NR | 2,5 | DP | NSSE |
| 19 | Itano (20) | 2008 | 40/M | Tail | ASx. | WNL | 3.0 | DP | SSE |
| 20 | Servais (21) | 2008 | 52/F | Tail | ASx. | NR | 11.5×10.5×8.5 | DP | CCE |
| 21 | Gleeson (22) | 2008 | 32/F | Tail | AP | NR | 1.5×1.2 | DP&S | SSE |
| 22 | Kadota (23) | 2009 | 57/F | Tail | ASx. | WNL | 6.0×5.0×4.0 | DP | NSSE, CE |
| 23 | Kadota (23) | 2009 | 70/F | Tail | ASx. | 48 | 1.7×1.0×0.8 | DP | NSSE, CE |
| 24 | Kadota (23) | 2009 | 37/M | Tail | ASx. | 647 | 10×7.0×7.0 | SPDP | KSSE, CE |
| 25 | Zhang (24) | 2009 | 26/F | Tail | ASx. | WN | 2.5×2.5 | SPDP | SSE |
| 26 | Itano (25) | 2010 | 67/M | Tail | EP, WL | WNL | 3.0 | LADP | SSE |
| 27 | Yamanishi (26) | 2011 | 55/F | Tail | ASx. | 90 | 2.5×1.5 | DP | SSE |
| 28 | Iwasaki (27) | 2011 | 36/F | Tail | EP, WL | 79 | 3.4×1.9 | LDP | SSE |
| 29 | Horn (28) | 2011 | 62/M | Tail | AP | NR | 4.8×3.7×1.9 | CR | KSSE |
| 30 | Khashab (29) | 2011 | 49/F | Tail | AP | NR | 2.3 | LADP | SSE |
| 31 | Present case | 2012 | 56/M | Tail | AP. | WNL | 2.0×1.5 | SPDP | CE |
An elevation of serum CA 19-9 level was observed in
10 cases, hence the difficulty in pre-operatively differentiating
between an epidermoid cyst in an IPAS and pancreatic malignancy
during clinical analysis. Higaki et al(9) revealed that the serum CA 19-9 level
markedly decreased to within the normal range following surgery in
a patient diagnosed with an epidermoid cyst in an IPAS, suggesting
that the serum CA 19-9 originated in the epidermoid cyst in an
IPAS.
The histogenesis of an epidermoid cyst in an IPAS
may be identical to that of a splenic epidermoid cyst (23). There are three hypotheses concerning
the histogenesis of an epidermoid cyst in an IPAS (10). Firstly, the cyst may originate from
mesothelial inclusion with subsequent squamous metaplasa (30). Secondly, teratomatous derivation or
an inclusion of fetal squamous epithelium may cause cystic change
(31). Thirdly, a derivation from
the pancreatic duct may protrude into the accessory spleen
(10). In a case described by
Kadota et al(23), there
were pancreatic ducts in the fibrous tissue surrounding the
accessory spleen tissue, and the squamous and cuboidal epithelia
indicated a transitional appearance from one form to the other.
Additionally, immunohistochemical analysis demonstrated that the
staining results of the cystic epithelial lining were identical to
those of the pancreatic duct. These results support the third
hypothesis.
A pre-operative imaging diagnosis of an epidermoid
cyst in an IPAS is extremely difficult. Notably, a diagnosis of
abdominal CT in the present case was also pancreatic tail cancer.
As there are no characteristic features to define the lesion on
radiology, it is not possible to entirely differentiate the cystic
pancreatic malignancy prior to surgery and histopathological
examination (28).
In conclusion, an epidermoid cyst in an IPAS is an
extremely rare disease entity, and radiographic and clinical
results (including CA 19-9 elevation) are similar to those of other
cystic pancreatic neoplasms. As a result, the possibilty of such a
cystic lesion should be considered in the differential diagnosis of
a pancreatic cystic lesion.
Acknowledgements
This study was supported by research
funds from Chosun University, 2010.
References
|
1.
|
Halpert B and Alden ZA: Accessory spleens
in or at the tail of the pancreas. A survey of 2700 additional
necropsies. Arch Pathol. 77:652–654. 1964.PubMed/NCBI
|
|
2.
|
Davidson ED, Campbell WG and Hersh T:
Epidermoid splenic cyst occurring in an intrapancreatic accessory
spleen. Dig Dis Sci. 25:964–967. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Hanada M, Kimura M, Kitada M, et al:
Epidermoid cyst of accessory spleen. Acta Pathol Jpn. 31:863–871.
1981.PubMed/NCBI
|
|
4.
|
Jibu T, Nagai H, Senba D, Wada Y, Kuroda
A, Morioka Y, et al: A case of epidermoid cyst occurring in an
intrapancreatic accessory spleen. Nihon Shokakibyo Gakkai Zasshi.
84:1859–1862. 1987.(In Japanese).
|
|
5.
|
Morohoshi T, Hamamoto T, Kunimura T, et
al: Epidermoid cyst derived from an accessory spleen in the
pancreas. A case report with literature survey. Acta Pathol Jpn.
41:916–921. 1991.PubMed/NCBI
|
|
6.
|
Nakae Y, Hayakawa T, Kondo T, et al:
Epidermoid cyst occurring in a pancreatic accessory spleen. J Clin
Gastroenterol. 13:362–364. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Tang X, Tanaka Y and Tsutsumi Y:
Epithelial inclusion cysts in an intrapancreatic accessory spleen.
Pathol Int. 44:652–654. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Furukawa H, Kosuge T, Kanai Y, et al:
Epidermoid cyst in an intrapancreatic accessory spleen: CT and
pathologic findings. Am J Roentgenol. 171:2711998. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Higaki K, Jimi A, Watanabe J, et al:
Epidermoid cyst of the spleen with CA19-9 or carcinoembryonic
antigen productions: report of three cases. Am J Surg Pathol.
22:704–708. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Tateyama H, Tada T, Murase T, et al:
Lymphoepithelial cyst and epidermoid cyst of the accessory spleen
in the pancreas. Mod Pathol. 11:1171–1177. 1998.PubMed/NCBI
|
|
11.
|
Sasou S, Nakamura S and Inomata M:
Epithelial splenic cysts in an intrapancreatic accessory spleen and
spleen. Pathol Int. 49:1078–1083. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Tsutsumi S, Kojima T, Fukai Y, et al:
Epidermoid cyst of an intrapancreatic accessory spleen: a case
report. Hepatogastroenterology. 47:1462–1464. 2000.PubMed/NCBI
|
|
13.
|
Choi SK, Ahn SI, Hong KC, Kim SJ, Kim TS,
Woo ZH, et al: A case of epidermoid cyst of the intrapancreatic
accessory spleen. J Korean Med Sci. 15:589–592. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Horibe Y, Murakami M, Yamao K, et al:
Epithelial inclusion cyst (epidermoid cyst) formation with
epithelioid cell granuloma in an intrapancreatic accessory spleen.
Pathol Int. 51:50–54. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Sonomura T, Kataoka T, Chikugo T, et al:
Epidermoid cyst originating from an intrapancreatic accessory
spleen. Abdom Imaging. 27:560–562. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Yokomizo H, Hifumi M, Yamane T, et al:
Epidermoid cyst of an accessory spleen at the pancreatic tail:
diagnostic value of MRI. Abdom Imaging. 27:557–559. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Fink AM, Kulkarni S, Crowley P, et al:
Epidermoid cyst in a pancreatic accessory spleen mimicking an
infected abdominal cyst in a child. Am J Roentgenol. 179:206–208.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Kanazawa H, Kamiya J, Nagino M, et al:
Epidermoid cyst in an intrapancreatic accessory spleen: a case
report. J Hepatobiliary Pancreat Surg. 11:61–63. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Ru K, Kalra A and Ucci A: Epidermoid cyst
of intrapancreatic accessory spleen. Dig Dis Sci. 52:1229–1232.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Itano O, Shiraga N, Kouta E, et al:
Epidermoid cyst originating from an intrapancreatic accessory
spleen. J Hepatobiliary Pancreat Surg. 15:436–439. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Servais EL, Sarkaria IS, Solomon GJ, et
al: Giant epidermoid cyst within an intrapancreatic accessory
spleen mimicking a cystic neoplasm of the pancreas: case report and
review of the literature. Pancreas. 36:98–100. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Gleeson FC, Kendrick ML, Chari ST, et al:
Epidermoid accessory splenic cyst masquerading as a pancreatic
mucinous cystic neoplasm. Endoscopy. 40:E141–E142. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Kadota K, Kushida Y, Miyai Y, et al:
Epidermoid cyst in an intrapancreatic accessory spleen: three case
reports and review of the literatures. Pathol Oncol Res.
16:435–442. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Zhang Z and Wang JC: An epithelial splenic
cyst in an intrapancreatic accessory spleen. A case report. JOP.
10:664–666. 2009.PubMed/NCBI
|
|
25.
|
Itano O, Chiba N, Wada T, et al:
Laparoscopic resection of an epidermoid cyst originating from an
intrapancreatic accessory spleen: report of a case. Surg Today.
40:72–75. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Iwasaki Y, Tagaya N, Nakagawa A, Kita J,
Imura J, Fujimori T, et al: Laparoscopic resection of epidermoid
cyst arising from an intrapancreatic accessory spleen: a case
report with a review of the literature. Surg Laparosc Endosc
Percutan Tech. 21:e275–279. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27.
|
Yamanishi H, Kumagi T, Yokota T, Koizumi
M, Azemoto N, Watanabe J, et al: Epithelial cyst arising in an
intrapancreatic accessory spleen: a diagnostic dilemma. Intern Med.
50:1947–1952. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28.
|
Horn AJ and Lele SM: Epidermoid cyst
occurring within an intrapancreatic accessory spleen. A case report
and review of the literature. JOP. 12:279–282. 2011.PubMed/NCBI
|
|
29.
|
Khashab MA, Canto MI, Singh VK, Hruban RH,
Makary MA and Giday S: Endosonographic and elastographic features
of a rare epidermoid cyst of an intrapancreatic accessory spleen.
Endoscopy. 43:e193–194. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30.
|
Ough YD, Nash HR and Wood DA: Mesothelial
cysts of the spleen with squamous metaplasia. AM J Clin Pathol.
76:666–669. 1981.PubMed/NCBI
|
|
31.
|
Lifschitz-Mercer B, Open M, Kushnir I and
Czernobilsky B: Epidermpid cyst of the spleen:a cytokeratin profile
with comparison to other squamous epithelia. Virchows Arch.
424:213–216. 1994. View Article : Google Scholar : PubMed/NCBI
|