Introduction
According to WHO classification, gastric cancer
(GCA) can be divided into two major categories, intestinal and
diffuse types (1). Lymph node
metastasis of GCA decides the tumor-node-metastasis (TNM) stage.
Lymph node micrometastasis (MM) in GCA is also a significant
prognostic factor and influences the therapeutic regimen (2–5), while
isolated tumor cell (ITC) is a type of MM. In routine pathology
practice, ×40 microscopy of hematoxylin and eosin (HE) staining is
commonly used to detect lymph node metastasis. However,
misdetection often occurs with this method.
In clinical practice, we also find that lymph node
metastasis of intestinal type GCA is glandular-like and little
misdetection occurs in HE staining; however, diffuse type GCA is
the opposite. Cancer cells are isolated in the primary tumor and
lymph node metastases, especially in MM/ITC. Misdetection occurs
more often in conventional HE staining.
Certain studies have claimed that regular HE
staining supplemented with immunohistochemistry [IHC; cytokeratin
(CK) or epithelial membrane antigen (EMA)] may increase the
detection rate of lymph node metastasis of GCA (6–8) by
providing more accurate pathological information so as to guide
treatment and prognosis prediction (9). However, of these studies, some used
pan-CK as an independent indicator, some EMA and others a
combination to detect the metastasis. We find that some
non-epithelial cells, such as plasma cells, are positive, while
some cancer cells are negative in EMA staining in our routine work.
Therefore, the questions of which is the best marker for detecting
the lymph node metastasis of GCA and whether the combination of CK
and EMA increases the metastasis detection rate remain
unsettled.
Patients and methods
Patients and specimens
Among the patients who underwent radical gastrectomy
at the Department of Surgery at Hua Shan Hospital (tertiary
referral center in China) between 2007 and 2009, 50 patients with
intestinal type GCA and 50 with diffuse type GCA were reviewed. We
collected 700 lymph nodes dissected from patients with intestinal
type GCA and 722 from patients with the diffuse type. The mean age
of this series of patients was 57.88±13.53 years (range, 28–81),
while that of the intestinal type patients was 59.88±13.48 years
and for the diffuse type was 55.45±13.32 years. The study was
approved by the Ethics Committee of Huashan Hospital, Fudan
University, Shanghai, China. Informed patient consent was obtained
from all the patients.
IHC staining
A total of 1,422 lymph nodes were resected from the
100 patients and a single pathologist reexamined all lymph node
slides to confirm the absence of lymph node metastasis. IHC
staining for CK and EMA was performed using the ABC IHC staining
method. From paraffin blocks, the widest area that represented the
condition of the corresponding lymph node was sectioned at 4-mm
thickness, and the tissue sections were deparaffinized by immersion
in xylene and rehydration in a series of alcohol. To augment the
expression of antigen in tissues, citrate buffer solution was added
to the samples which were then boiled in a microwave oven. To
suppress the endogenous peroxidase activity, the samples were
treated with 3% hydrogen peroxide solution for 15 min and rinsed
with phosphate-buffered saline (PBS). To prevent non-specific
immune reactions, the samples were reacted with normal horse serum
for 20 min. The slides were shaken lightly and then reacted with
primary antibody at 37°C for 90 min. A 1:100 dilution of
mouse-anti-human broad-spectrum CK antibody AE1/AE3 (M-0349 200912)
or a 1:200 dilution of mouse-anti-human EMA monoclonal antibody
(M-0236 200912) was used as the primary antibody. After rinsing the
slides with PBS, a 1:200 dilution of secondary antibody (VECTOR
peroxidase mouse IgG PK-4002) was added and the mixture were
reacted at 37°C for 60 min and then rinsed with PBS. Subsequently,
ABC solution was added, reacted for 30 min and the samples were
rinsed with PBS. DAB was then added, reacted for 5 min and the
samples were rinsed with the buffer solution, counter-stained with
Mayer’s hematoxylin and sealed with resin mount (060440303018 Leica
LV Ultra). The negative control was prepared by the same procedure
with lymphoid follicles of the amygdala and tonsil epithelia were
used as the positive control.
Evaluation of staining results
CK is located in the cytoplasm (10) and EMA on the cell membrane (11,12).
Positive staining cells are brown-yellow, while the negative cells
are unstained. Positive staining lymph nodes were confirmed by
examination of the structure and morphology of the cells.
If IHC-positive cancer cells were detected in the
lymph node as a single cell or a small nest of cancer cells <0.2
mm in size, it was defined as ITC. If the size of the cell nest was
>0.2 mm but <2 mm, it was defined as MM. However, MM and ITC
were combined into one group in the subsequent statistical analysis
as there were few cases of ITC in our study (13). Two senior pathologists independently
observed the HE, CK and EMA staining slides under a microscope to
determine the results. For the HE-, CK- and EMA-positive staining
slides, ×100 microscopy of the HE sections was used to determine
whether the positive IHC results were tumor metastasis. A single
pathologist reexamined all slides to confirm the absence of lymph
node metastasis.
Statistical analysis
For comparison of the detection rate of CK and EMA
staining method, we calculated the detection, true-positive,
true-negative and false-positive rates. Statistical comparisons
were performed using a four-fold table and a paired marginal
χ2 test, Fisher’s exact probability and Student’s
t-test. P<0.05 was considered to indicate a statistically
significant result. The statistical analysis software SPSS 15.0 was
used (SPSS, Inc., Chicago, IL, USA).
Results
Detection rate of lymph node
metastasis
A total of 1,422 lymph nodes were resected from the
100 patients (50 intestinal GCA and 50 diffuse GCA). Of those lymph
nodes, 700 were dissected from intestinal type GCA and 722 from
diffuse type. Of the patients with intestinal type GCA, 222/700
were node-positive, with a detection rate of 31.71%, while in the
diffuse type, 200/722 were node-positive, with a detection rate of
27.70%, by conventional HE staining. Following examination by both
HE and IHC staining, 250/700 (35.71%) intestinal cases and 260/722
(36.01%) diffuse cases were node-positive. A total of 28 intestinal
type and 60 diffuse type lymph nodes were found to be positive by
IHC staining which were missed by HE staining. All these foci were
found to be MM/ITC.
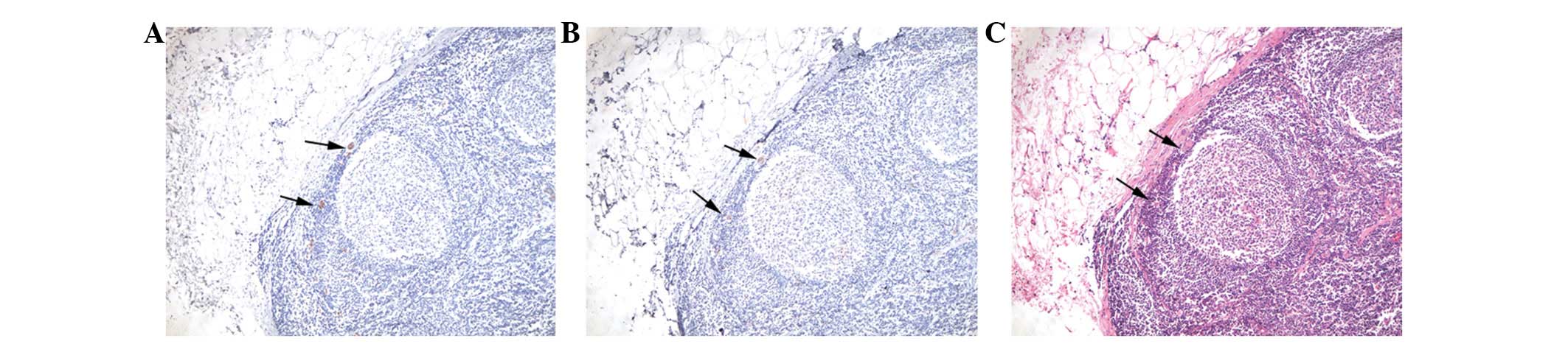
CK IHC staining
In intestinal and diffuse type GCA, 250 and 260
lymph nodes were positive for metastasis by CK staining and the
detection rate increased from 31.71% to 35.71% (P<0.01) and from
27.70% to 36.01% (P<0.01), respectively (Table I). Therefore, there was misdetection
by HE staining (Fig. 1).
 | Table IChi-square analysis of detection rate
of pan-CK, EMA and HE (×40). |
Table I
Chi-square analysis of detection rate
of pan-CK, EMA and HE (×40).
| HE (×40)
| | | |
|---|
| Sample | (+) | (−) | Total | Chi-square | P-value |
|---|
| Intestinal | | | | | |
| pan-CK | | | | | |
| (+) | 222 | 28 | 250 | 28.00 | <0.01 |
| (−) | 0 | 450 | 450 | | |
| Total | 222 | 478 | 700 | | |
| EMA | | | | | |
| (+) | 221 | 85 | 306 | 82.05 | <0.01 |
| (−) | 1 | 393 | 394 | | |
| Total | 222 | 478 | 700 | | |
| Diffuse | | | | | |
| pan-CK | | | | | |
| (+) | 200 | 60 | 260 | 600.00 | <0.01 |
| (−) | 0 | 462 | 462 | | |
| Total | 200 | 522 | 722 | | |
| EMA | | | | | |
| (+) | 193 | 95 | 288 | 75.92 | <0.01 |
| (−) | 7 | 427 | 434 | | |
| Total | 200 | 522 | 722 | | |
There was no false-positive or false-negative case
of CK staining in the two types of GCA following confirmation under
×100 microscopy (Table II).
 | Table IIComparison of true-positive and
true-negative rates of CK and EMA. |
Table II
Comparison of true-positive and
true-negative rates of CK and EMA.
| Sample | HE ×100 (+) | HE ×100 (−) | True-positive rate
(%) | True-negative rate
(%) |
|---|
| Intestinal | | | | |
| pan-CK (+) | 250 | 0 | 100 | 100 |
| pan-CK (−) | 0 | 450 | | |
| EMA (+) | 249 | 57 | 99.60 | 87.33 |
| EMA (−) | 1 | 393 | | |
| Diffuse | | | | |
| pan-CK (+) | 260 | 0 | 100 | 100 |
| pan-CK (−) | 0 | 462 | | |
| EMA (+) | 253 | 35 | 97.31 | 92.42 |
| EMA (−) | 7 | 427 | | |
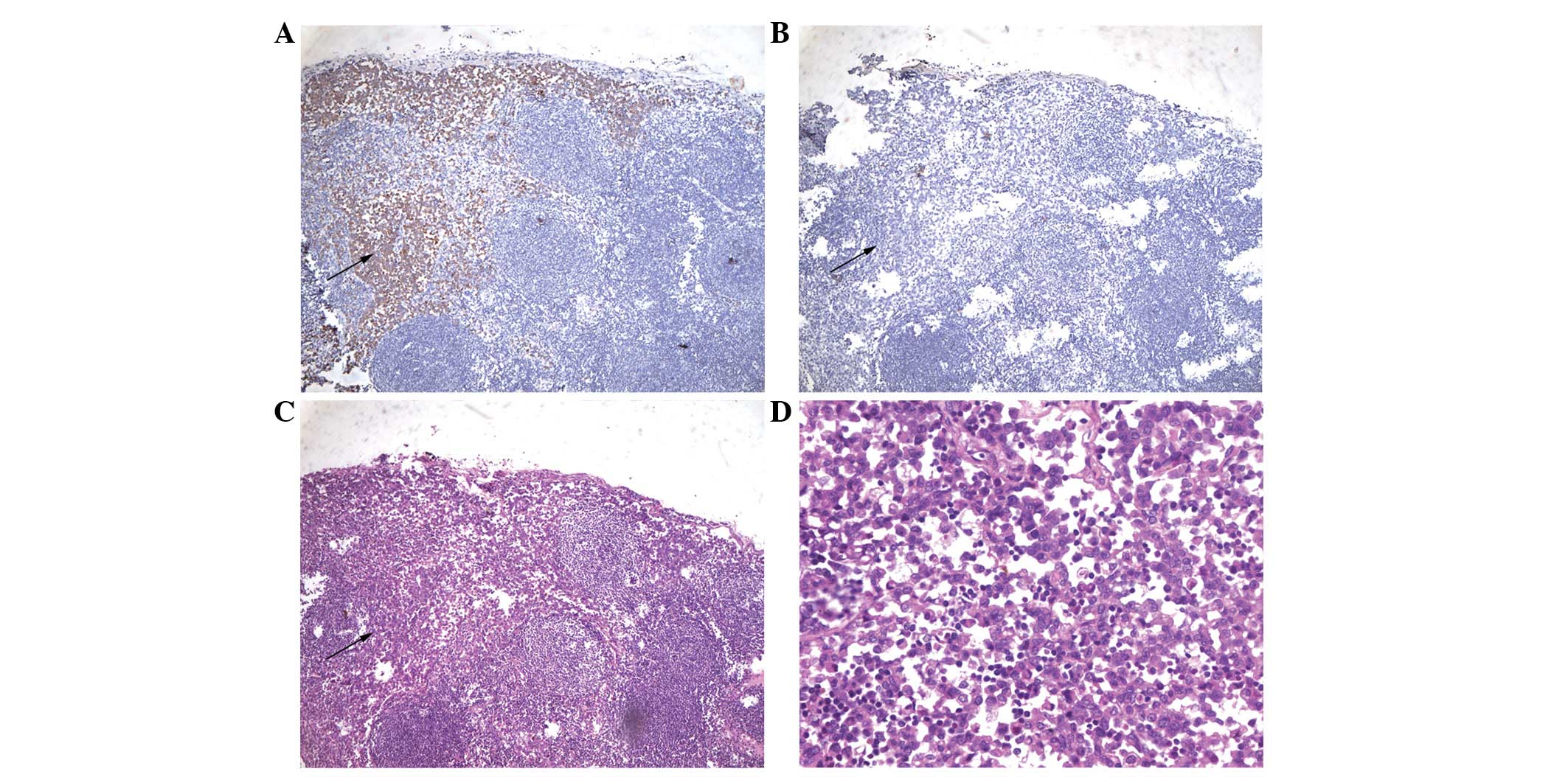
Among EMA-negative lymph nodes, one intestinal type
and seven diffuse type lymph nodes were positive by both CK and HE
staining. However, there were no cases of EMA-positive tumor cells
which were negative by CK staining (Table II; Fig.
2).
EMA IHC staining
In intestinal type and diffuse type, 306 and 288
lymph nodes were positive for metastasis by EMA staining, while the
detection rate increased by 37.84% and 44.00%, respectively
(P<0.01; Table I).
One of the 250 intestinal type lymph nodes was
negative by EMA staining but contained cancer cells when viewed
under ×100 microscopy. Of the diffuse type cases, seven out of 260
lymph nodes were negative. The false-negative rates were 0.40% and
2.69%, respectively (Table II).
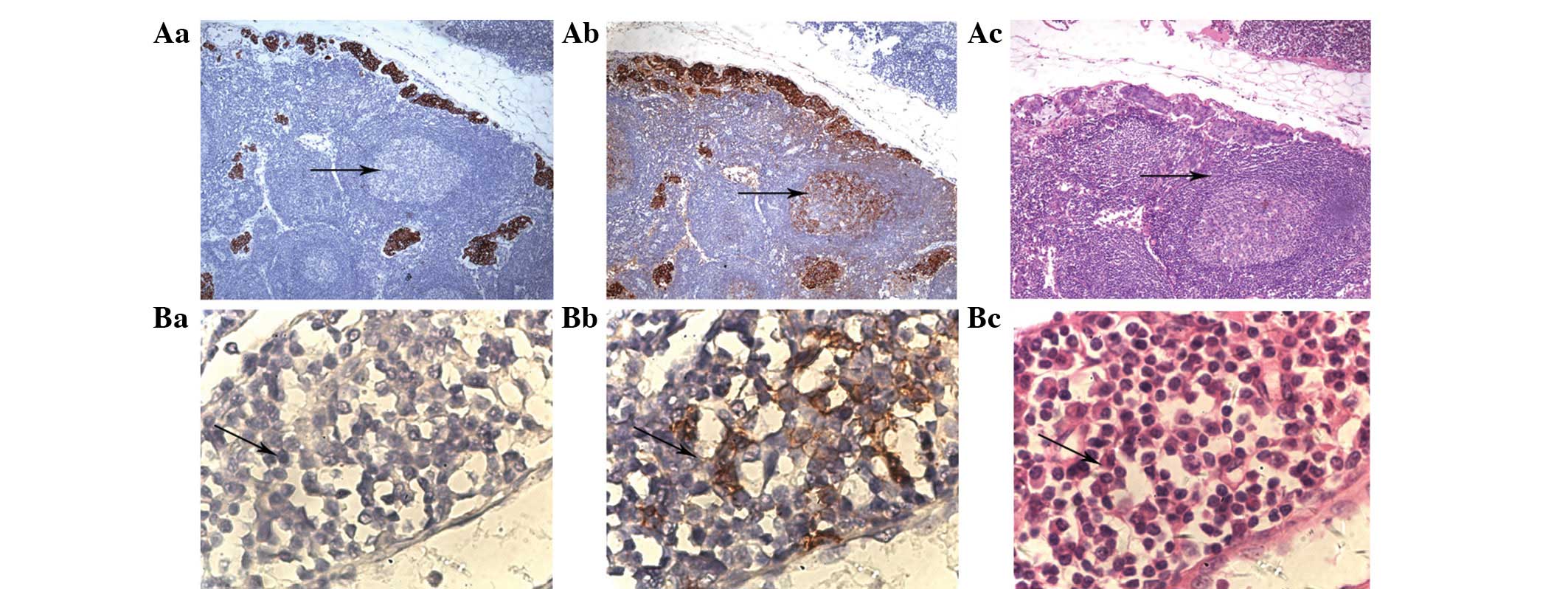
In certain cases, normal cells were positive by EMA
staining. A total of 57 out of 450 intestinal type and 35 of 462
diffuse type lymph nodes were false-positive. These false-positive
foci were mostly germinal centers and plasma cells (Fig. 3).
Combination of CK and EMA IHC
staining
In the two types of GCA, the combined use of HE and
IHC staining did not increase the detection rate of lymph node
metastasis and increased the false-positive rate.
Among the intestinal type cases, the true-positive
rate of CK staining was higher than that of EMA staining (100 and
99.60%, respectively), as was the true-negative rate (100 and
97.31%, respectively; Table
II).
Among the diffuse type cases, the true-positive rate
of CK staining was also higher than that of EMA staining (100 and
97.31%, respectively), as was the true-negative rate (100 and
92.42%, respectively; Table
II).
Discussion
Lymph node metastasis can be divided into three
types, including macrometastasis, MM and ITC. Presently, GCA is one
of the most malignant tumors while lymph node MM/ITC always occurs
in the early stage. Lymph node MM plays a main role in stage
confirmation, prognosis and the selection of clinical therapeutic
regimen. MM/ITC exists in up to 30% of HE-negative lymph nodes
(13,14). There have been several studies
evaluating the correlation between MM/ITC and prognosis in GCA
(2,15–17).
Most studies reported that MM/ITC affected the prognosis of GCA,
but the degree of influence was variable according to the groups of
patients. One study reported that both CK and EMA staining
increased the sensitivity and specificity of the detection rate of
lymph node MM/ITC and decreased the rate of misdetection. pan-CK
(AE1/AE3) and EMA are epithelium-specific antibodies. As the basic
component of cellular structure of normal epithelial cells and
epithelial cancer cells, they are often used to differentiate
tumors according to whether they originate from the epithelium or
not. However, no study has confirmed which of CK and EMA is the
better method for raising the detection rate of lymph node MM/ITC,
and whether it is necessary to perform combined CK and EMA
examinations. Our study demonstrates that IHC staining increases
the detection rate of lymph node metastasis. All the misdetected
foci of metastasis were confirmed to be MM/ITC.
CK staining is valuable in assisting diagnosis and
selecting a suitable clinical treatment. Some HE-negative slides
were CK-positive due to MM/ITC. There were significant differences
between HE and CK staining when the cases were checked under ×40
light microscopy. There was no false-positive or false-negative
case of CK staining in either type of GCA, as confirmed under ×100
microscopy.
Although there are differences between the results
of EMA and HE staining, false-positive and false-negative rates of
EMA staining are much higher. The reasons for this are as follows.
Firstly, some HE-positive slides were EMA-negative and MM/ITC is
more easily missed in EMA staining. Secondly, HE-negative slides
were EMA-positive. The visual field of EMA staining is not as
clear-cut as in CK staining (18,19).
Inexperienced pathologists may falsely regard this non-specific
staining as positive and make a false diagnosis. Thirdly, the
germinal centers of lymph nodes appear to be positive. Certain
studies have reported that germinal centers may be false-positive
under EMA staining in patients with T lymph cell lymphoma.
Fourthly, plasma cells may also be stained. Some authors also
report that plasma cells may be false-positive in EMA staining,
characterized as the focus of MM/ITC of the diffuse type GCA, which
may lead to misdiagnosis (20,21).
It is unnecessary to perform combined CK and EMA
examinations to detect the lymph node metastasis of GCA. It may
increase the false-positive rate, but is unlikely to improve the
detection rate.
The present study has certain limitations. Although
CK staining increases the detection rate of lymph node metastasis
of GCA, MM/ITC appears as only a single cell or a small nest of
cancer cells. This means that the focus will not occur in all the
slides of one paraffin block, which may cause misdetection in IHC
or HE staining.
There is no need to perform EMA examination, due to
the false-positive and false-negative situation. For the two types
of GCA, CK should be used to confirm whether MM/ITC exists if
conventional pathology is negative. Since the focus of lymph node
MM/ITC appears as isolated cells or a small nest of cancer cells,
it may be easily missed in HE staining only. However, HE staining
is sufficient if the lymph node is positive under routine
pathological examination.
Our research compares the methods of HE, CK and EMA
staining, aiming to demonstrate the work process of diagnosing
lymph node metastasis, especially MM/ITC, of GCA.
Acknowledgements
Dr Tengfang Zhu assisted with
pathological examination. Supported by Chinese National Basic
Science Funding, No. J0730860.
References
|
1
|
Catalano V, Labianca R, Beretta GD, Gatta
G, de Braud F and Van Cutsem E: Gastric cancer. Crit Rev Oncol
Hematol. 71:127–164. 2009. View Article : Google Scholar
|
|
2
|
Morgagni P, Saragoni L, Scarpi E, et al:
Lymph node micrometastases in early gastric cancer and their impact
on prognosis. World J Surg. 27:558–561. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ishigami S, Natsugoe S, Tokuda K, et al:
Clinical impact of micrometastasis of the lymph node in gastric
cancer. Am Surg. 69:573–577. 2003.PubMed/NCBI
|
|
4
|
Natsugoe S, Nakashima S, Matsumoto M, et
al: Paraaortic lymph node micrometastasis and tumor cell
microinvolvement in advanced gastric carcinoma. Gastric Cancer.
2:179–185. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
de Manzoni G, Verlato G, Guglielmi A,
Laterza E, Genna M and Cordiano C: Prognostic significance of lymph
node dissection in gastric cancer. Br J Surg. 83:1604–1607.
1996.PubMed/NCBI
|
|
6
|
Miyake K, Seshimo A and Kameoka S:
Assessment of lymph node micrometastasis in early gastric cancer in
relation to sentinel nodes. Gastric Cancer. 9:197–202. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ishida K, Katsuyama T, Sugiyama A and
Kawasaki S: Immunohistochemical evaluation of lymph node
micrometastases from gastric carcinomas. Cancer. 79:1069–1076.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Bower M, Newlands ES, Holden L, et al:
EMA/CO for high-risk gestational trophoblastic tumors: results from
a cohort of 272 patients. J Clin Oncol. 15:2636–2643.
1997.PubMed/NCBI
|
|
9
|
Yasuda K, Adachi Y, Shiraishi N, Inomata
M, Takeuchi H and Kitano S: Prognostic effect of lymph node
micrometastasis in patients with histologically node-negative
gastric cancer. Ann Surg Oncol. 9:771–774. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Jain R, Fischer S, Serra S and Chetty R:
The use of Cytokeratin 19 (CK19) immunohistochemistry in lesions of
the pancreas, gastrointestinal tract, and liver. Appl
Immunohistochem Mol Morphol. 18:9–15. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhang J, Shen KW, Liu G, et al: Antigenic
profiles of disseminated breast tumour cells and microenvironment
in bone marrow. Eur J Surg Oncol. 29:121–126. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Heyderman E, Strudley I, Powell G,
Richardson TC, Cordell JL and Mason DY: A new monoclonal antibody
to epithelial membrane antigen (EMA)-E29. A comparison of its
immunocytochemical reactivity with polyclonal anti-EMA antibodies
and with another monoclonal antibody, HMFG-2. Br J Cancer.
52:355–361. 1985. View Article : Google Scholar
|
|
13
|
Kim JJ, Song KY, Hur H, Hur JI, Park SM
and Park CH: Lymph node micrometastasis in node negative early
gastric cancer. Eur J Surg Oncol. 35:409–414. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Cai J, Ikeguchi M, Maeta M and Kaibara N:
Micrometastasis in lymph nodes and microinvasion of the muscularis
propria in primary lesions of submucosal gastric cancer. Surgery.
127:32–39. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Harrison LE, Choe JK, Goldstein M,
Meridian A, Kim SH and Clarke K: Prognostic significance of
immunohistochemical micrometastases in node negative gastric cancer
patients. J Surg Oncol. 73:153–157. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lee E, Chae Y, Kim I, Choi J, Yeom B and
Leong AS: Prognostic relevance of immunohistochemically detected
lymph node micrometastasis in patients with gastric carcinoma.
Cancer. 94:2867–2873. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Maehara Y, Oshiro T, Endo K, et al:
Clinical significance of occult micrometastasis lymph nodes from
patients with early gastric cancer who died of recurrence. Surgery.
119:397–402. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ferry JA, Sohani AR, Longtine JA, Schwartz
RA and Harris NL: HHV8-positive, EBV-positive Hodgkin lymphoma-like
large B-cell lymphoma and HHV8-positive intravascular large B-cell
lymphoma. Mod Pathol. 22:618–626. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Delsol G, Gatter KC, Stein H, et al: Human
lymphoid cells express epithelial membrane antigen. Implications
for diagnosis of human neoplasms. Lancet. 2:1124–1129. 1984.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Baldus SE, Palmen C and Thiele J: MUC1
(EMA) expressing plasma cells in bone marrow infiltrated by plasma
cell myeloma. Histol Histopathol. 22:889–893. 2007.PubMed/NCBI
|
|
21
|
Leong CF, Raudhawati O, Cheong SK,
Sivagengei K and Noor Hamidah H: Epithelial membrane antigen (EMA)
or MUC1 expression in monocytes and monoblasts. Pathology.
35:422–427. 2003. View Article : Google Scholar : PubMed/NCBI
|