Introduction
Hypopharyngeal carcinoma is a difficult carcinoma to
treat due to the fact that it is often diagnosed at a late stage
and that it has an aggressive natural history. The standard
operation is a total pharyngolaryngectomy. This procedure can have
a negative impact on the well-being of patients as it involves
tracheotomy and loss of natural voice, which may lead to social
isolation, loss of employment and depression. Chemoradiotherapy
(radiotherapy plus concurrent chemotherapy) has become the standard
of care for patients with unresectable squamous cell carcinoma of
the head and neck (1) and for organ
preservation (2,3).
The repair of various types of DNA damage is
critical for cell survival. Of these, DNA double-strand break (DSB)
is understood to be one of the most serious forms of damage induced
by DNA-damaging agents such as ionizing irradiation (4). Non-homologous end-joining (NHEJ) is a
key mechanism of DNA DSB repair (5). In the NHEJ pathway, DSBs are rejoined
at an appropriate chromosomal end, either directly or following DNA
end processing, and DNA-dependent protein kinase (DNA-PK) is
important in DNA DSB repair by NHEJ throughout the cell cycle
(6). DNA-PK is a serine/threonine
kinase, which is composed of the DNA-PK catalytic subunit
(DNA-PKcs) and the heterodimer of Ku70 and Ku86. DNA-PK binds DSBs
in DNA, and phosphorylates and activates DNA-binding protein,
including XRCC4 and DNA ligase IV, p53 and several transcription
factors. Subsequently, ligase IV repairs DNA DSB (7). Therefore, DNA-dependent protein kinase
(DNA-PK) is important in DNA DSB repair. The immunohistochemical
analysis of proteins involved in DNA DSB repair such as Ku70, Ku86
and XRCC4 may have potential as a predictive assay for tumor
radiosensitivity (8,9).
In this study, we investigated the correlation
between the expression of proteins involved in DNA DSB and the
results of chemoradiotherapy for hypopharyngeal cancers in patients
admitted to the Sapporo Medical University. We also examined the
expression of Ki-67, a nuclear protein that is expressed in cycling
cells.
Patients and methods
Patients
Fifty-seven Japanese patients with previously
untreated squamous cell carcinoma of the hypopharynx were treated
at the Sapporo Medical University between March 2002 and December
2009.
The patient population consisted of 48 men and 9
women. The mean age was 63 years (range, 33–82). The distribution
according to the subsites of the hypopharynx was 48 piriform sinus,
7 postcricoid area and 2 posterior pharyngeal wall. With regard to
TNM stage (7th edition), 4 patients had stage I disease, 10 had
stage II, 8 had stage III and 35 had stage IV disease (Table I). Most patients (75%) had stage III
or IV disease.
 | Table IThe treatment results according to
stage. |
Table I
The treatment results according to
stage.
| Stage | Number of
patients | Locoregional
recurrence alone | Locoregional
recurrence and distant metastasis | Distant metastasis
alone |
|---|
| I | 4 | 0 | 0 | 0 |
| II | 10 | 1 | 0 | 0 |
| III | 8 | 0 | 1 | 1 |
| IV | 35 | 10 | 6 | 1 |
Patients with distant metastasis at the first
admission were excluded from this study.
This study was approved by the ethics committee of
Sapporo University. Patient consent was obtained either from the
patient or the patient’s family.
Treatments
In 51 of the 57 patients, chemotherapy was
administered concurrently with radiotherapy. Six patients were
treated with radiotherapy alone. The chemotherapy consisted of FP
(cisplatin plus 5FU) or S-1. FP was used in 39 patients and S-1 in
12 patients. FP consisted of cisplatin 40–60 mg/m2
intravenously and 5FU 400–700 mg/body/day for 4 days by continuous
venous infusion. S-1 (50–80 mg/body) was orally administered during
periods of radiotherapy.
Radiation was administered using a 4 MV photon
linear accelerator. The primary tumor, jugular and retropharyngeal
nodes were treated with lateral parallel-opposed photon fields. An
appositional anterior field was used to irradiate the
supraclavicular and paratracheal nodes. A tumor dose of 50 Gy (25
fractions/5 weeks) was administered to the primary tumor and
regional lymph nodes. Doses of 10–20 Gy were usually added to the
primary tumor with reduced fields after 50 Gy.
Immunohistochemical staining of various
proteins in hypopharyngeal cancer tissues
Formalin-fixed, paraffin-embedded specimens from
biopsy were used. Immunohistochemical staining was carried out
using methods described in a previous study (10). Anti-Ku70, Ku86 or XRCC4 rabbit
polyclonal antisera, which have been described previously (10,11),
were used. Ki-67 staining was performed with MIB-1 monoclonal
rabbit antibody (Dako, Copenhagen, Denmark) using methods described
previously (12). The number of
cells that stained positive for Ku70, Ku86, XRCC4 and Ki-67 were
determined by scoring 3 microscopic fields of 300 tumor cells each,
without prior knowledge of radiosensitivity or treatment outcome,
and determining the percentages of cells that were positive for the
expression of Ku70, Ku86, XRCC4 and Ki-67.
Statistical analysis
The median follow-up time to the last contact or
mortality was 30 months, with a range of 0 to 93 months. The
cut-off for analysis was November 2011. Patients alive at the
cut-off date had a median follow-up time of 45 months. Overall and
disease-free survival were calculated by the Kaplan-Meier method.
Differences were analyzed by the log-rank test. A significance
level of 0.05 was used throughout. Locoregional recurrence refers
to recurrence in the hypopharynx and/or regional lymph nodes.
Results
Overall and disease-free survival
rates
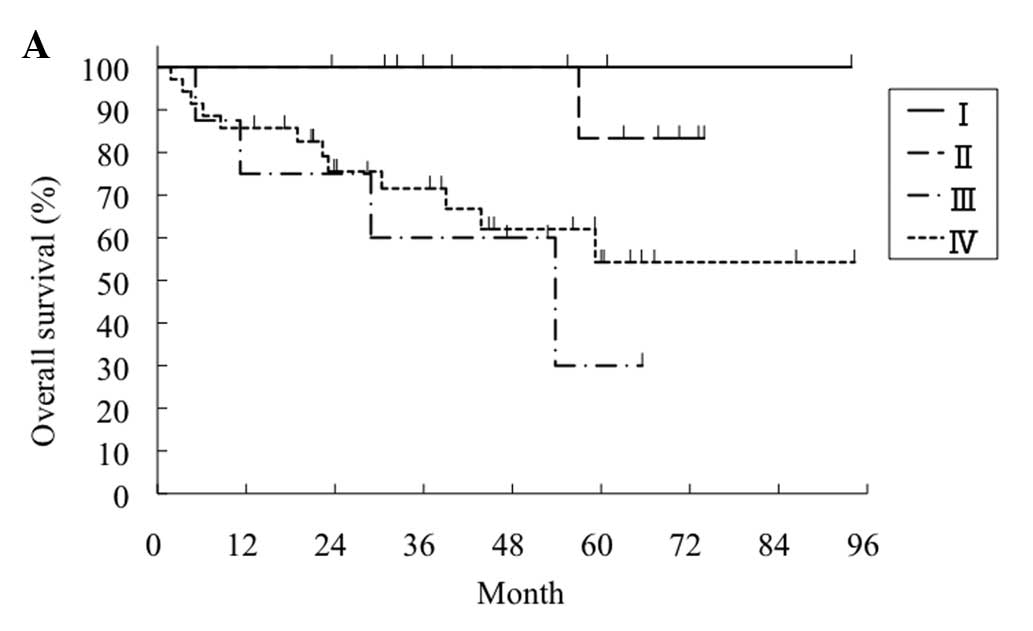
The overall 5-year survival rate in patients treated
with chemoradiotherapy was 100% in stage I, 83% in stage II, 30% in
stage III and 50% in stage IV (Fig.
1A). The difference in the overall 5-year survival between
stages I-II and stages III-IV was significant (P=0.02). The 5-year
disease-free survival rate in patients treated with
chemoradiotherapy was 100% in stage I, 90% in stage II, 64% in
stage III, and 50% in stage IV (Fig.
1B). The difference in disease-free survival between stages
I-II and stages III-IV was significant (P=0.02).
Treatment results according to stage
Table I shows the
treatment results according to stage. Only 3 of 22 patients
experienced locoregional recurrence and/or distant metastasis in
stages I-III compared to 17 of 35 patients in stage IV. Most
patients with distant metastasis also experienced locoregional
recurrence, although two patients had distant metastasis alone.
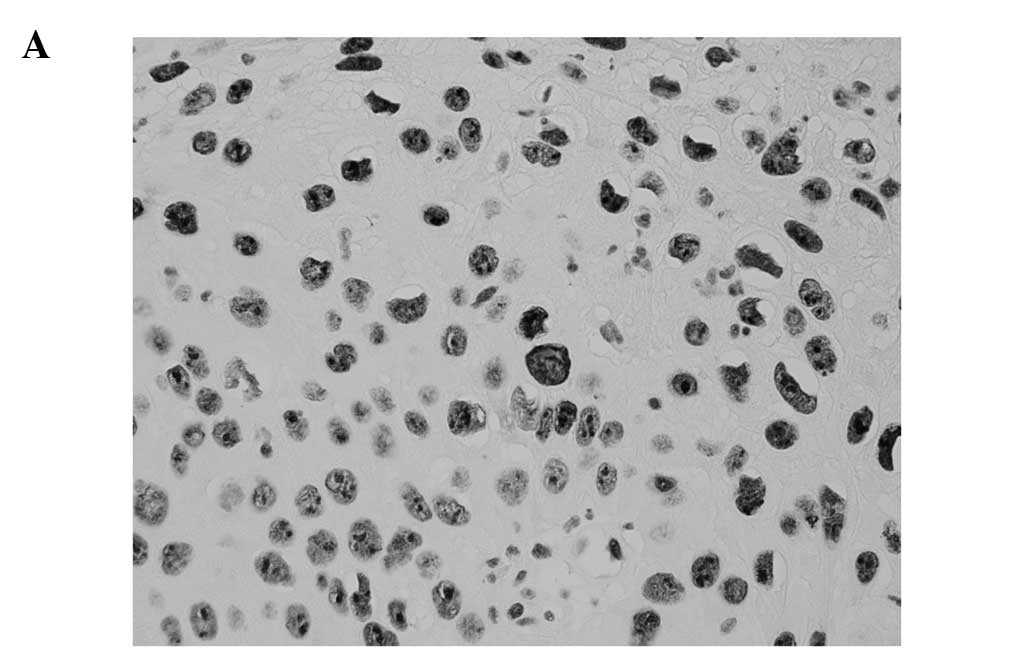
Immunohistochemical staining
The staining of Ku70, Ku86, XRCC4 and Ki-67 was
nuclear with none of the normal epithelial cells or malignant cells
exhibiting cytoplasmic or membrane immunoreactivity. The staining
was diffuse throughout the cell nucleus (Fig. 2).
Analysis of results of immunohistology
and survival
The percentage of cells that expressed Ku70, Ku86,
XRCC4 and Ki-67 in different tumors was analyzed (Table II).
 | Table IIThe percentage of cells that expressed
Ku70, Ku86, XRCC4 and Ki-67. |
Table II
The percentage of cells that expressed
Ku70, Ku86, XRCC4 and Ki-67.
| Expression | Mean ± SD (%) | Median (%) | Range (%) |
|---|
| Ku70 | 52±30 | 50 | 0–98 |
| Ku86 | 37±31 | 29 | 0–98 |
| XRCC4 | 77±23 | 86 | 33–98 |
| Ki-67 | 37±23 | 31 | 1.4–97 |
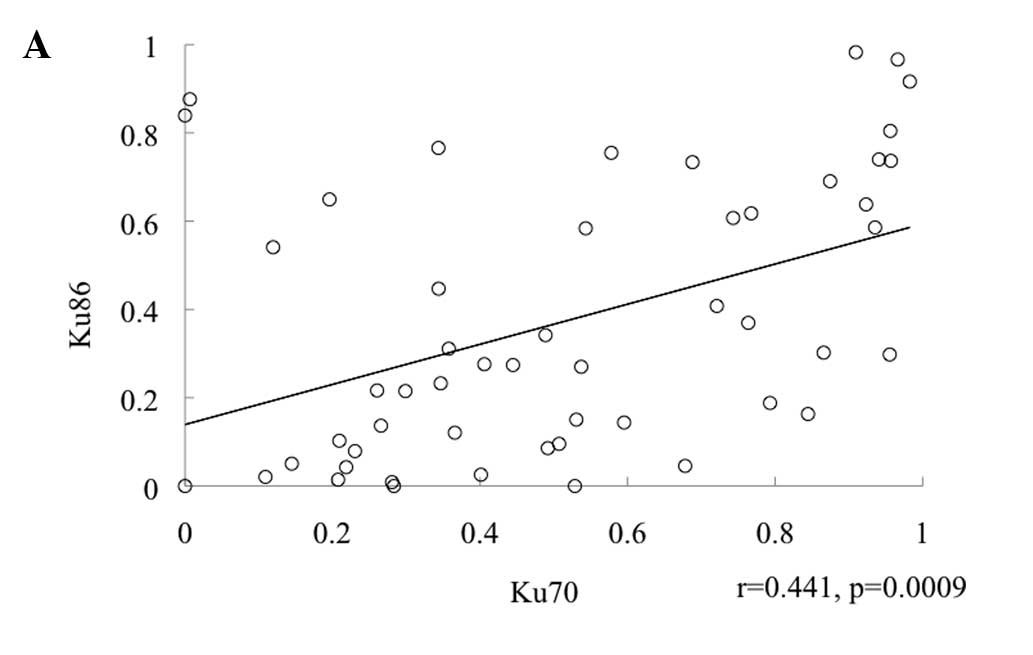
We examined whether there was a correlation between
the expression levels of proteins involved in NHEJ. A significant
correlation was found between the percentage of cells expressing
Ku70 and Ku86 (r=0.44; P=0.009; Fig.
3A), Ku70 and XRCC4 (r=0.39; P=0.004; Fig. 3B), and Ku86 and XRCC4 (r=0.54;
P<0.0001; Fig. 3C).
The mean percentage of cells expressing Ku70 in the
local control group was 49% and that in the local failure group was
57%. The mean percentage of cells expressing Ku86 in the local
control group was 39% and that in the local failure group was 34%.
The mean percentage of cells expressing XRCC4 in the local control
group was 76% and that in the local failure group was 79%. The mean
percentage of cells expressing Ki-67 in the local control group was
35% and that in the local failure group was 41%.
An analysis of the correlation between the
expression of these proteins and locoregional control was performed
according to stage. In stages I-III, patients with a lower
expression of Ku70 (<35%) tended to have better locoregional
control (Table III). In stages
I-III, patients with a lower expression of XRCC4 (<78%) tended
to have better locoregional control (Table IV). However, this tendency in Ku70
and XRCC4 was not significant due to the small numbers. There was
no such tendency in patients with stage IV (Tables III and IV).
 | Table IIIThe correlation between the expression
of Ku70 and locoregional control according to stage. |
Table III
The correlation between the expression
of Ku70 and locoregional control according to stage.
| A, Stages I, II and
III |
|---|
|
|---|
| Percentage of Ku70
positivity | Number of
patients | Number of
recurrences | Recurrence rate
(%) |
|---|
| <35% | 10 | 0 | 0 |
| >35% | 9 | 2 | 22 |
|
| B, Stage IV |
|
| Percentage of Ku70
positivity | Number of
patients | Number of
recurrences | Recurrence rate
(%) |
|
| <35% | 9 | 3 | 33 |
| >35% | 23 | 11 | 48 |
 | Table IVThe correlation between the expression
of XRCC4 and locoregional control according to stage. |
Table IV
The correlation between the expression
of XRCC4 and locoregional control according to stage.
| A, Stages I, II and
III |
|---|
|
|---|
| Percentage of XRCC4
positivity | Number of
patients | Number of
recurrences | Recurrence rate
(%) |
|---|
| <78% | 7 | 0 | 0 |
| >78% | 11 | 2 | 18 |
|
| B, Stage IV |
|
| Percentage of XRCC4
positivity | Number of
patients | Number of
recurrences | Recurrence rate
(%) |
|
| <78% | 9 | 5 | 56 |
| >78% | 23 | 10 | 43 |
We also analyzed the correlation between the
expression of Ku70, Ku86, XRCC4 and Ki-67 and distant metastasis.
Nine patients experienced distant metastasis. In seven patients the
distant metastasis was accompanied by locoregional recurrence but
two patients had distant metastasis alone (Table I). In patients with both distant
metastasis and locoregional recurrence, there was no apparent
correlation between the expression of these proteins and distant
metastasis. By contrast, in two patients with distant metastasis
alone, one patient had 0% expression of Ku70 and the other had 0%
expression of Ku86 (Fig. 3A). There
were four patients with 0% expression of Ku70 or Ku86. None of the
four patients experienced locoregional recurrence. Two patients
developed distant metastasis.
Discussion
The estimates of overall and disease-free survival
at 3 years in all patients were 78 and 63%, respectively (Fig. 1A and B). These treatment results
were comparable with other studies using chemoradiotherapy
(13,14).
We examined whether there was a correlation between
the expressions of proteins involved in NHEJ. A significant
correlation was found between the percentage of cells expressing
Ku70 and Ku86 (Fig. 3A), Ku70 and
XRCC4 (Fig. 3B), and Ku86 and XRCC4
(Fig. 3C). The results of Ku70 and
Ku86 were in agreement with our previous results, demonstrating
that the expression of Ku70 and Ku86 paralleled each other in
breast cancer tissues (15). These
results indicated that there was a concerted expression of Ku70 and
Ku86 in breast cancer tissues. Hosoi et al reported that
Ku70 and Ku86 have consensus Sp1 recognition elements in their
promoter region and that Sp1 may influence the concerted expression
of Ku70 and Ku86 (16). To the best
of our knowledge, the correlation of the expression of XRCC4 with
that of Ku70 or Ku86 is a new finding. However, the mechanism of
the concerted expression of these proteins remains to be
determined.
Patients with a lower expression of Ku70 or XRCC4
tended to have better locoregional control in stages I-III
(Table III). Komuro et al
reported results of 96 patients with advanced rectal carcinoma
treated with preoperative radiotherapy (8). The lower expression of Ku70 or Ku86 in
preradiation biopsy specimens of tumor samples was correlated with
better objective responses, suggesting that low expression of Ku70
or Ku86 may be correlated with high radiosensitivity.
There was no such correlation between the expression
of Ku70 or XRCC4 and locoregional control in patients with stage IV
(Tables II and III). Patients with stage IV had a large
primary tumor and/or large lymph node metastases. In such a
situation, the large number of tumor cells and hypoxic tumor cells
may affect radiocurability and obscure the effect of Ku70 or XRCC4
expression.
Ki-67 is a nuclear protein that is expressed in
cycling cells. For patients treated with radiotherapy, the tumors
with a high Ki-67 labeling index demonstrated good local control in
squamous cell carcinomas of the head and neck (17), esophageal cancer (18) and uterine cervical cancer (19). However, no such correlation was
found between the Ki-67 labeling index and locoregional control of
hypopharyngeal cancer treated with chemoradiotherapy in our
results. This observation indicated that chemoradiotherapy may be
effective for tumors that included non-cycling cells.
There were two patients with distant metastasis
alone, one of whom had 0% expression of Ku70 and the other a 0%
expression of Ku86. There were four patients with 0% expression of
Ku70 or Ku86 (Fig. 2A). None of the
four patients experienced locoregional recurrence but two developed
distant metastasis alone. These results may be associated with our
previous results which demonstrated that breast cancer cells with a
lower expression of Ku70 or Ku86 had aggressive cancer phenotypes
such as a higher nuclear grade and positive axillary lymph node
metastasis (15). Genes involved in
DNA DSB repair are involved in the maintenance of genomic stability
(20). We previously demonstrated
that DNA-PK activity is associated with chromosomal instability
(21). An absence of Ku70 or Ku86
expression indicates low DNA-PK activity. Such low DNA-PK activity
resulted in the genetic alteration of cancer cells, leading to
higher tendency of distant metastasis.
In conclusion, patients with a lower expression of
Ku70 or XRCC4 tended to have better locoregional control in stages
I-III, but there was no such tendency in patients with stage IV. In
two patients with distant metastasis alone, one patient had 0%
expression of Ku70 and the other had 0% expression of Ku86. This
finding suggests that proteins involved in NHEJ may have an impact
on the treatment results of chemoradiotherapy in hypopharyngeal
cancer.
Acknowledgements
The study was supported in part by a Grant-in-Aid
for Scientific Research from the Ministry of Education, Culture,
Sports, Science and Technology, Japan and by a grant from the
Program for Developing the Supporting System for Upgrading
Education and Research in Sapporo Medical University.
References
|
1
|
Adelstein DJ, Li Y, Adams GL, et al: An
intergroup study phase III comparison of standard radiation therapy
and two schedules of concurrent chemoradiotherapy in patients with
unresectable squamous cell head and neck cancer. J Clin Oncol.
21:92–98. 2003. View Article : Google Scholar
|
|
2
|
Denis F, Garaud P, Bardet E, et al: Final
results of the 94-01 French Head and Neck Oncology and Radiotherapy
Group randomized trial comparing radiotherapy alone with
concomitant radiochemotherapy in advanced-stage oropharynx
carcinoma. J Clin Oncol. 22:69–76. 2004. View Article : Google Scholar
|
|
3
|
Forastiere AA, Goepfert H, Maor M, et al:
Concurrent chemotherapy and radiotherapy for organ preservation in
advanced laryngeal cancer. N Engl J Med. 349:2091–2098. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hall EJ: DNA strand breaks and chromosomal
aberrations. Radiobiology for the Radiologist. Hall EJ and Giaccia
AM: 6th edition. Lippincott Williams & Wilkins; Philadelphia:
pp. 16–29. 2006
|
|
5
|
Polo SE and Jackson SP: Dynamics of DNA
damage response proteins at DNA breaks: a focus on protein
modification. Gene Dev. 25:409–433. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lees-Miller SP: The DNA-dependent protein
kinase, DNA-PK: 10 years and no ends in sight. Biochem Cell Biol.
74:503–512. 1996.PubMed/NCBI
|
|
7
|
Jeggo PA: Identification of genes involved
in repair of DNA double-strand breaks in mammalian cells. Radiat
Res. 150:S80–S91. 1998. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Komuro Y, Watanabe T, Hosoi Y, et al: The
expression pattern of Ku correlates with tumor radiosensitivity and
disease free survival in patients with rectal carcinoma. Cancer.
95:1199–1205. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhao HJ, Hosoi Y, Miyachi H, et al:
DNA-dependent protein kinase activity correlates with Ku70
expression and radiation sensitivity in esophageal cancer cell
lines. Clin Cancer Res. 6:1073–1078. 2000.PubMed/NCBI
|
|
10
|
Sakata K, Matsumoto Y, Tauchi H, et al:
Expression of genes involved in repair of DNA double-strand breaks
in normal and tumor tissues. Int J Radiat Oncol Biol Phys.
49:161–167. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kamdar RP and Matsumoto Y:
Radiation-induced XRCC4 association with chromatin DNA analyzed by
biochemical fractionation. J Radiat Res. 51:303–313. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sakata K, Someya M, Nagakura H, et al:
Brachytherapy for oral tongue cancer: an analysis of treatment
results with various biological markers. Jpn J Clin Oncol.
38:402–407. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pointreau Y, Garaud P, Chapet S, et al:
Randomized trial of induction chemotherapy with cisplatin and
5-fluorouracil with or without docetaxel for larynx preservation. J
Natl Cancer Inst. 101:498–506. 2009. View Article : Google Scholar
|
|
14
|
Posner MR, Hershock DM, Blajman CR, et al:
Cisplatin and fluorouracil alone or with docetaxel in head and neck
cancer. New Engl J Med. 25:1705–1715. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Someya M, Sakata K, Matsumoto Y, Satoh M,
Narimatsu H and Hareyama M: Immunohistochemical analysis of Ku70/86
expression of breast cancer tissues. Oncol Rep. 18:1483–1487.
2007.PubMed/NCBI
|
|
16
|
Hosoi Y, Watanabe T, Nakagawa K, et al:
Up-regulation of DNA-dependent protein kinase activity and Sp1 in
colorectal cancer. Int J Oncol. 25:461–468. 2004.PubMed/NCBI
|
|
17
|
Raybaud-Diogene H, Fortin A, Morency R,
Roy J, Monteil RA and Tetu B: Markers of radioresistance in
squamous cell carcinomas of the head and neck: a clinicopathologic
and immunohistochemical study. J Clin Oncol. 15:1030–1038.
1997.PubMed/NCBI
|
|
18
|
Okuno Y, Nishimura Y, Kashu I, Ono K and
Hiraoka M: Prognostic values of proliferating cell nuclear antigen
(PCNA) and Ki-67 for radiotherapy of oesophageal squamous cell
carcinomas. Br J Cancer. 80:387–395. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Nakano T and Oka K: Differential values of
Ki-67 index and mitotic index of proliferating cell population. An
assessment of cell cycle and prognosis in radiation therapy for
cervical cancer. Cancer. 72:2401–2408. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Burma S, Chen BPC and Chen DJ: Role of
non-homologous end joining (NHEJ) in maintaining genomic integrity.
DNA Repair. 5:1042–1048. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Someya M, Sakata K, Matsumoto Y, et al:
The association of DNA-dependent protein kinase activity with
chromosomal instability and risk of cancer. Carcinogenesis.
27:117–122. 2006. View Article : Google Scholar : PubMed/NCBI
|