Introduction
Patients with small cell lung cancer (SCLC) are
surviving for longer with the aid of more effective contemporary
anticancer treatments (1,2). For this reason, metastases of the
central nervous system (CNS) are becoming increasingly common.
Prophylactic cranial irradiation (PCI) significantly reduces the
rate of brain metastases and improves survival in both limited
disease (LD)- and extensive disease (ED)-SCLC patients who respond
to first-line treatment, and should therefore be part of the
standard treatment for responders with both disease types (4,5).
Carcinomatous meningitis is clinically less common than brain
metastasis, but has a poor outcome in terms of both quality of life
and overall survival (6). We report
a case of carcinomatous meningitis despite PCI during treatment
with amrubicin (AMR).
Case report
A 47-year-old man was admitted to our hospital with
a cough and hoarseness in September 2009. Chest roentgenography and
computed tomography (CT) revealed a tumor in the right upper lobe
extending to the mediastinum, from which CT-guided biopsy
identified SCLC. No metastases were detected in any other organs
and thus a diagnosis of LD was made. Treatment was initiated with 4
courses of carboplatin (CBDCA; AUC 6 on day 1) and etoposide
(VP-16, 100 mg/m2 on days 1–3) with 54 Gy of concurrent
radiotherapy, achieving partial response (PR). Levels of the tumor
marker pro-gastrin-releasing peptide (ProGRP) decreased to within
the normal range following chemoradiotherapy. We then administered
25 Gy of PCI in January 2010. In October 2010, enlargement of the
mediastinal lymph nodes was detected on the chest CT. This was
considered to represent sensitive relapse; thus, retreatment with 4
courses of CBDCA and VP-16 was performed, and again PR was
achieved.
In July 2011, enlargement of the mediastinal lymph
nodes was detected on chest CT. As AMR has recently been shown to
exhibit significant activity against SCLC as a second-line
treatment, with predictable and manageable toxicities (2), we used AMR (40 mg/m2 on
days 1–3) as a second-line treatment. After two courses of AMR,
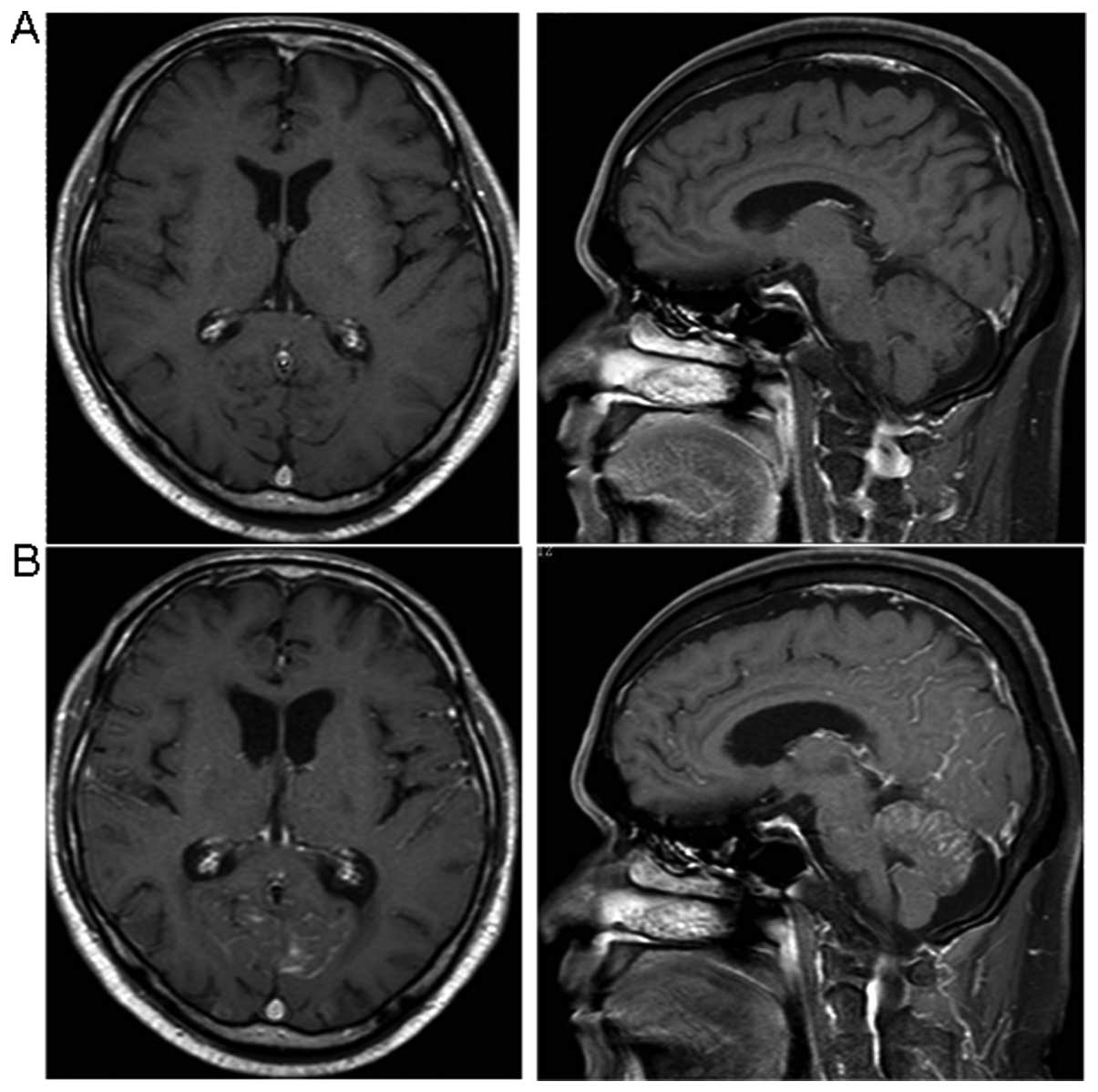
chest CT revealed stable disease. Follow-up of brain metastasis
with magnetic resonance imaging (MRI) revealed no significant
lesions on August 16 (Fig. 1A),
therefore the administration of the third course was commenced on
September 21.
On October 3, the patient was urgently hospitalized
suffering from a headache and disturbance of consciousness with
neck stiffness. As blood testing revealed grade 3 neutropenia, yet
ProGRP remained within the normal range, we first suspected septic
meningitis. Cytological examination of the cerebrospinal fluid
revealed SCLC cells, and abnormal leptomeningeal enhancement
(cerebral cortex, cerebral ventricles and cerebellum) was detected
on gadolinium-enhanced MRI (Fig.
1B). Carcinomatous meningitis without brain metastasis was
therefore diagnosed. As the symptoms progressed rapidly, supportive
care was selected. The patient succumbed 3 weeks after the
diagnosis of carcinomatous meningitis.
Discussion
Despite the development of systemic treatment, the
majority of patients with SCLC relapse, and CNS is a frequent site
of relapse. Approximately 10% of patients with SCLC initially
present with brain metastases. The 2-year cumulative risk rises to
≥50% (6). As a result, the role of
PCI has been studied in several trials. A published meta-analysis
of PCI for SCLC in patients with complete remission following
chemotherapy analyzed data from 7 randomized studies (3). The relative risk of mortality in the
treatment group was significantly lower than that in the control
group. PCI also decreased the cumulative incidence of brain
metastases. Furthermore, ED-SCLC patients with response to
first-line chemotherapy in the irradiation group exhibited a lower
risk of symptomatic brain metastases and an increase in median
survival from 5.4 to 6.7 months (4). These results suggest that PCI reduces
the incidence of symptomatic brain metastases and prolongs survival
in SCLC patients. However, whether PCI reduces the incidence of
carcinomatous meningitis remains unclear. In many cases of SCLC,
carcinomatous meningitis develops with brain metastasis (5). Further study is required to clarify
whether SCLC cases demonstrating carcinomatous meningitis without
brain metastasis also show an increased frequency of relapse
involving the CNS following PCI.
Due to the lack of randomized studies, in particular
studies referring to one specific primary tumor, no standard
treatment for carcinomatous meningitis can yet be recommended.
However, it is clear that treatment provides effective palliation
and in certain cases achieves longer survival (7). Intrathecal chemotherapy may be
administered either by lumbar puncture or intraventricularly
through an Ommaya reservoir. Radiotherapy is also used in the
treatment of carcinomatous meningitis for palliation of symptoms
(8). Since our patient received 25
Gy of PCI as the standard dose for SCLC (9), the addition of sufficient whole-brain
irradiation was difficult. In addition, the rapid progression of
symptoms meant that our patient was unable to receive intrathecal
chemotherapy.
This case demonstrated the difficulty of treating
carcinomatous meningitis, particularly in treatment following PCI
for SCLC.
References
|
1
|
Noda K, Nishiwaki Y, Kawahara M, et al:
Irinotecan plus cisplatin compared with etoposide plus cisplatin
for extensive small-cell lung cancer. N Engl J Med. 346:85–91.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Onoda S, Masuda N, Seto T, et al: Phase II
trial of amrubicin for treatment of refractory or relapsed
small-cell lung cancer: Thoracic Oncology Research Group Study
0301. J Clin Oncol. 24:5448–5453. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Aupérin A, Arriagada R, Pignon JP, et al:
Prophylactic cranial irradiation for patients with small-cell lung
cancer in complete remission. N Engl J Med. 341:476–484. 1999.
|
|
4
|
Slotman B, Faivre-Finn C, Kramer G, et al:
Prophylactic cranial irradiation in extensive small-cell lung
cancer. N Engl J Med. 357:664–672. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sculier JP, Feld R, Evans WK, et al:
Neurologic disorders in patients with small cell lung cancer.
Cancer. 60:2275–2283. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Komaki R, Cox JD and Whitson W: Risk of
brain metastases from small-cell carcinoma of the lung related to
the length of survival and prophylactic irradiation. Cancer Treat
Rep. 65:811–814. 1981.PubMed/NCBI
|
|
7
|
Strady C, Ricciarelli A, Nasca S, et al:
Carcinomatous meningitis and solid tumours. Oncol Rep. 7:203–207.
2000.PubMed/NCBI
|
|
8
|
Chamberlain MC: Neoplastic meningitis.
Oncologist. 13:967–977. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Le Péchoux C, Dunant A, Senan S, et al:
Standard-dose versus higher-dose prophylactic cranial irradiation
(PCI) in patients with limited-stage small-cell lung cancer in
complete remission after chemotherapy and thoracic radiotherapy
(PCI 99-01, EORTC 22003-08004, RTOG 0212, and IFCT 99-01): a
randomised clinical trial. Lancet Oncol. 10:467–474. 2009.
|