Introduction
Teratomas are germ cell tumors commonly composed of
multiple cell types derived from one or more of the three germ
layers. Pathologically, teratomas are classified into three groups:
mature (cystic/solid, benign), immature (malignant) and monodermal
(highly specialized, e.g., struma ovarii, carcinoid tumors, neural
tumors). Teratomas most commonly arise in the gonads but have also
been found in the anterior mediastinum, retroperitoneum and
gastrointestinal tract (1). Several
studies have reported that laparoscopic approaches are generally
accepted in normal cases for their minimal invasiveness, fewer
complications and quicker recovery (2–4). The
evident cosmetic advantage of this technique for young women is
also noted. However, it is debatable whether this technique may be
applied to giant ovarian teratomas. Therefore, a study to evaluate
the intraperitoneal spillage and oncological safety of laparascopic
and laparotomic procedures for giant ovarian teratomas is
essential.
In the present study, we report a young woman (20
years old) with a massive ovarian neoplasm, histopathologically
diagnosed as a mature teratoma derived from three germ layers which
was successfully removed by laparotomy, and review 329 giant
ovarian teratomas treated at our hospital.
Materials and methods
Identification of patients with giant
teratoma
A total of 329 cases of giant ovarian teratoma
(tumor diameter over 15 cm) were admitted to the Second Affiliated
Hospital of Zhejiang University School of Medicine (Zhejiang,
China) between January 1st 2000 and December 31st 2010. The
diagnosis of giant ovarian teratoma was based on clinical
examination, imaging evaluation and finally confirmed by
pathological results. The patients were divided into two groups
according to whether laparoscopic (group 1) or laparotomic (group
2) surgery was employed. The data were analyzed using the Student’s
t-test and Fisher’s exact test. Statistical analyses were performed
using SPSS version 15.0 (SPSS, Chicago, IL, USA).
Case report
Local ethical committee approval was received and
the informed consent of the patients was obtained.
A 20-year-old female presented with a complaint of
irregular menstruations with an abdominal mass of increasing size,
denying any severe abdominal pain, vomiting, constipation or
melena. The woman was otherwise healthy and denied any previous
medical problems. Physical examination at admission demonstrated a
bulged belly with a huge convex deformation approximately 30×20×30
cm in size in the periumbilical region (Fig. 1). On palpation, the mass was hard
with mild tenderness, smooth on its surface and not fixed. No other
abnormalities were noted during the physical examination. Serum
tumor markers showed high levels of CA199 and CA125. α-fetoprotein
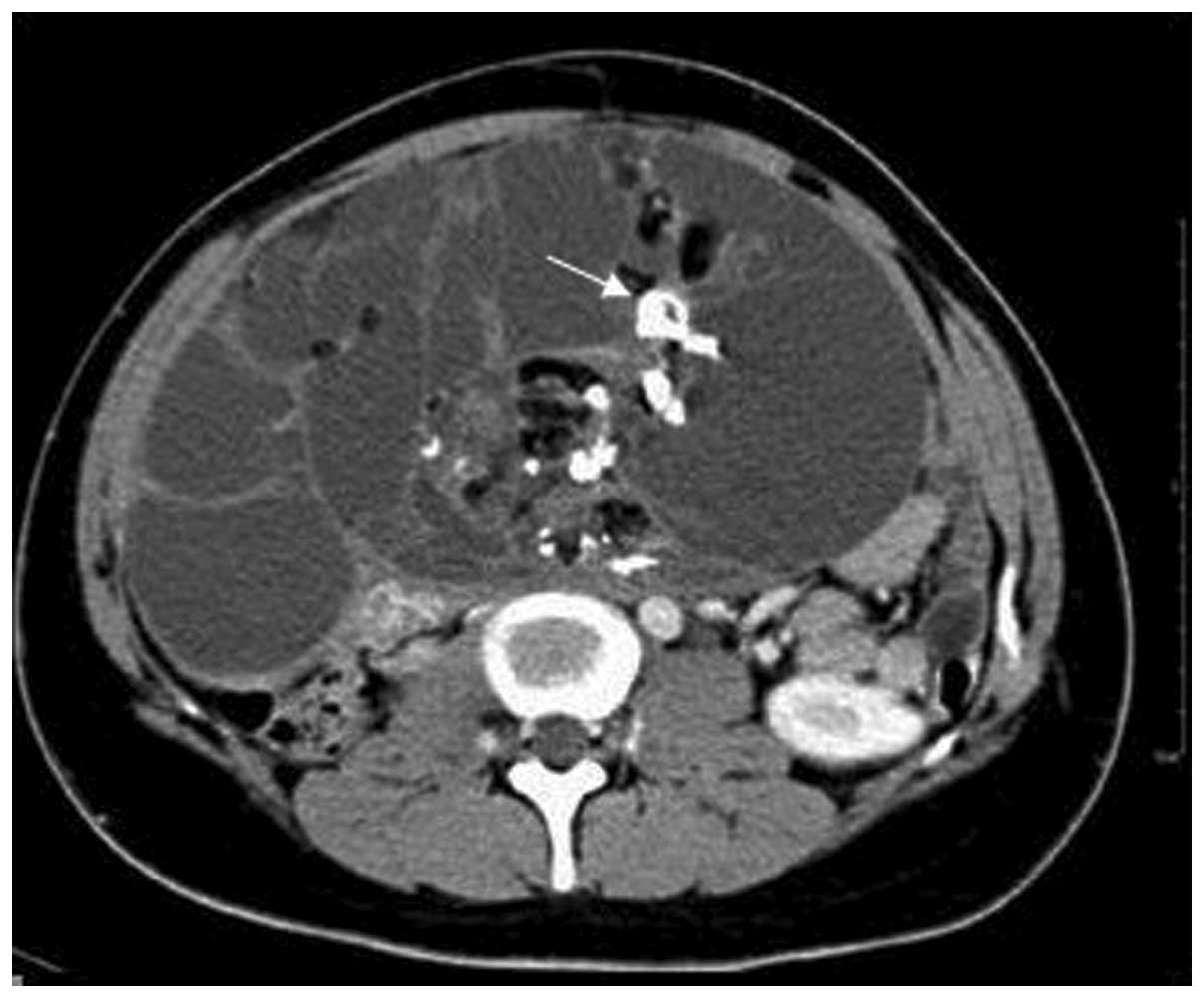
(AFP) and β-hCG levels were normal. Abdominal contrast CT revealed
a multilocular cystic mass containing tissues of different
densities, including bone and fat with calcified nuclei, and an
area of heterogeneous enhancement, located from the lower edge of
the liver to the pelvis (Fig. 2).
The patient was primarily diagnosed with teratoma and underwent a
median incisional exploratory laparotomy. We closely inspected the
pelvic and abdominal organs and found that no organ was infiltrated
and that the mass originated from the right ovary. The Fallopian
tube was elongated by traction of the tumor. In view of the
patient’s reproductive requirement and the results of the frozen
section analysis, we dissected the neoplasm entirely and ovary was
spared. The patient recovered without complications and was
discharged 6 days after surgery.
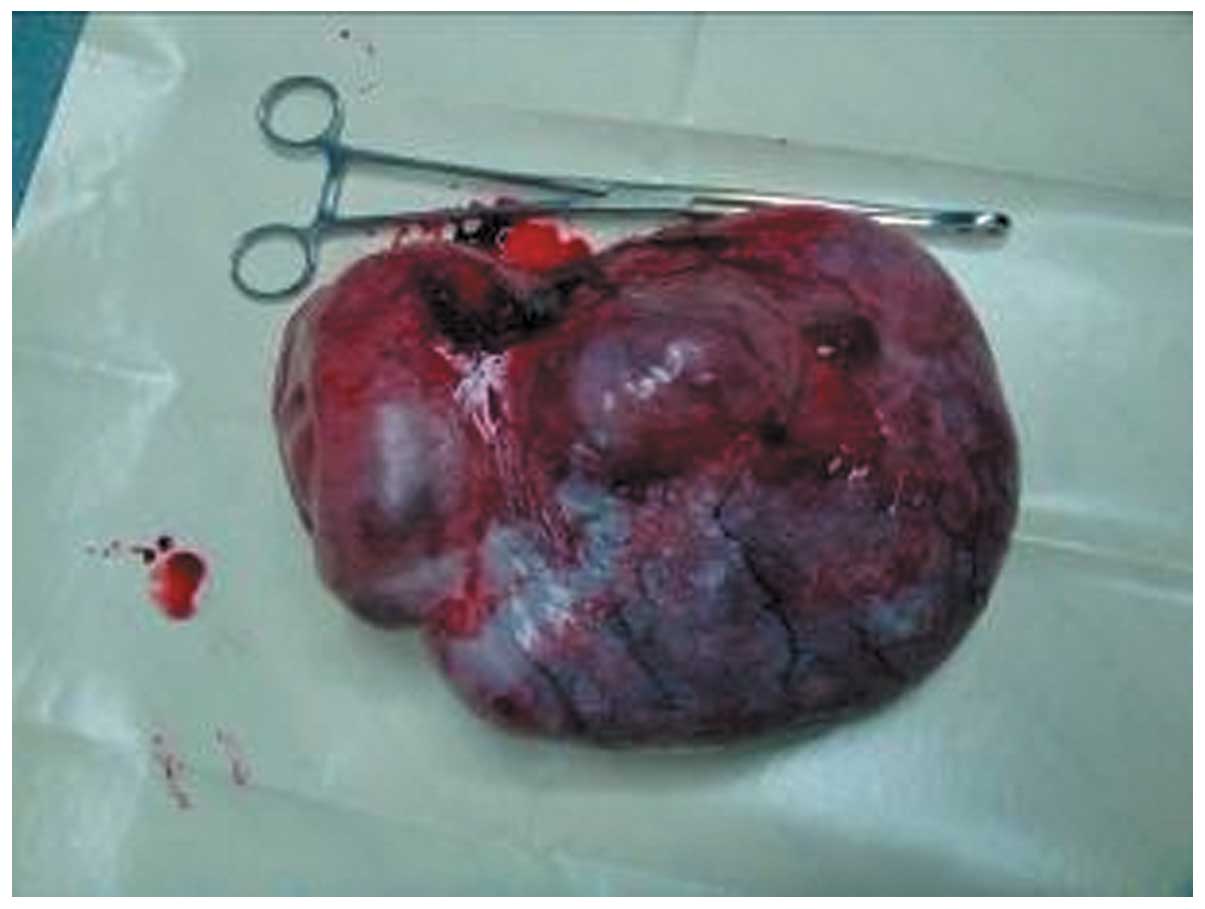
Pathological examination confirmed that the mass was
a benign teratoma coated with a smooth grey membrane and was
30×20×30 cm in size (Fig. 3). It
was a multilocular cystic mass with hypertension, containing some
transparent sticky liquid and lots of yellowish pasty sebaceous
material. Areas of calcifications compatible with bone were noted.
Brain tissue was also present microscopically. A 12-month follow-up
was conducted and no evidence of recurrence was found.
Results
Presentation
The median age of the 330 cases at presentation was
26 years, with a range from 6 to 83 years (Table I). The mean tumor size was 24.9±7.1
cm. The largest tumor was a 45×25-cm teratoma removed from a
74-year-old woman. A total of 228 (69.1%) patients reported
symptoms. The chief presenting complaint was abdominal distention
in 104 women (31.5%), abdominal pain in 103 (31.2%) and other
symptoms, including menoxenia and progressive dyspnea, in 21
(6.36%). Of the 330 patients, 102 were asymptomatic (30.9%) and had
their cysts discovered incidentally either on ultrasound or at the
time of surgery for another indication.
 | Table I.Clinical data of the 330 giant
teratoma cases. |
Table I.
Clinical data of the 330 giant
teratoma cases.
| Characteristic | Group 1
(n=111) | Group 2
(n=219)a | P-value |
|---|
| Age (years), mean ±
SD | 20.5±6.4 | 27.7±11.2 | 0.819 |
| Diameter of tumor
(cm), mean ± SD | 19.7±3.8 | 24.5±9.5 | 0.789 |
| Symptoms,
positive/negative | 78/33 | 150/69 | 0.741 |
| Abdominal
distention, positive/negative | 36/75 | 68/151 | 0.798 |
| Abdominal pain,
positive/negative | 38/73 | 65/154 | 0.399 |
| Menoxenia,
positive/negative | 3/108 | 12/207 | 0.253 |
| Dyspnea,
positive/negative | 1/110 | 5/214 | 0.375 |
| Asymptomatic,
positive/negative | 33/78 | 69/150 | 0.741 |
| Bilateral,
positive/negative | 9/102 | 20/199 | 0.756 |
| Pregnancy,
positive/negative | 5/106 | 13/206 | 0.588 |
| Emergency surgery,
positive/negative | 0/111 | 12/207 | 0.028b |
| Surgical approach,
positive/negative | | | |
| Cystectomy | 45/66 | 96/123 | 0.568 |
| Adnexectomy | 66/45 | 114/105 | 0.235 |
| Radical pelvic
dissectionc | 0/111 | 3/216 | 0.554 |
| Spillage,
positive/negative | 35/76 | 43/176 | 0.016b |
| Malignancy,
positive/negative | 0/111 | 5/214 | 0.172 |
| Chemotherapy,
positive/negative | 0/111 | 5/214 | 0.172 |
A total of 29 patients (8.8%) had teratomas present
in both ovaries and 18 (5.5%) were diagnosed during pregnancy [of
whom 2 (11.1%, 2/18) had obstructive dystocia and 6 (33.3%, 6/18)
had dyspnea]. Clinical data revealed no difference between the
laparoscopy and laparotomy groups (Table I).
Treatment
There was no difference in surgical procedures,
occurrence of malignancy or chemotherapy treatment between the two
groups. There were more emergency cases due to ovarian torsion in
group 2 compared with group 1 (5.5 vs. 0%, P<0.05). The overall
spillage rate was 23.6% (78/330) and was significantly lower in
group 2 compared with group 1 (19.6 vs. 31.5%, P<0.05),
reflecting the greater use of laparotomy in group 2.
Malignancy was found in 5 patients (1.52%). Two
patients with stage I immature teratoma had unilateral adnexectomy
and received three BEP cycles (bleomycin, etoposide and cisplatin)
following surgery. Malignant transformation was found in three
patients who underwent a total abdominal hysterectomy with
bilateral adnexectomy, including one case of melanoma in an
83-year-old woman and two cases of squamous cell carcinoma. The
three patients received a cisplatin/5-FU chemotherapy regimen.
Follow-up
There was no difference in the follow-up data
between the two groups. One case of recurrence occurred in melanoma
arising from mature teratoma. Granulomatous peritonitis was not
observed (Table II).
 | Table II.Follow-up data of the 330 giant
teratoma cases. |
Table II.
Follow-up data of the 330 giant
teratoma cases.
| Characteristic | Group 1 (n=111)
positive/negative | Group 2 (n=219)
positive/negative | P-value |
|---|
| Recurrence | 0/111 | 1/218 | 1.000 |
| Granulomatous
peritonitis | 0/111 | 0/219 | 1.000 |
| Surgical site
hematoma | 3/108 | 3/216 | 0.674 |
| Surgical site
infection | 0/111 | 3/216 | 0.532 |
Survival data were collected from 5 patients with
malignant teratomas who underwent open surgery. Two patients with
immature teratomas who received chemotherapy for between 3 months
and 2 years following surgery were disease-free after a period of 3
to 5 years without recurrence or metastasis. The 83-year-old woman
with melanoma arising from mature teratoma succumbed to multiple
organ failure 7 months after bilateral adnexectomy and
hysterectomy. The other two patients with squamous cell carcinoma
were well during the 1- to 2-year follow-up.
Discussion
Cystic ovarian teratomas, especially mature cases
(dermoid cysts), constitute 10–13% of all ovarian tumors and are
the most common benign ovarian germ cell tumors (5). They typically occur during
reproductive age (mean age, 27 years) (6). Ovarian cysts are traditionally labeled
as large when they are over 5 cm in diameter and giant or
voluminous when they are over 15 cm; a more suitable designation
for giant cysts may, however, relate the size of the cyst to the
size of the peritoneal cavity in these growing young patients
(7). The majority of teratomas may
be symptom free. With the tolerance of the abdomen, there is no
clear symptom at the early stage of ovary teratomas. The tumors
tend to enlarge until specific organs are functionally influenced
or incidental discovery by ultrasound. Mature cystic teratomas grow
slowly at an average rate of 1.8 mm each year, prompting
conservative management of smaller (diameter less than 6 cm) tumors
(8).
Giant ovarian teratomas commonly present with acute
abdominal pain caused by adnexal torsion (9) and abdominal distention due to the
rapid growth of a large, unilateral tumor undergoing capsular
distention, hemorrhage or necrosis (10). The patients may also have certain
non-specific abdominal complaints indicating mass effect, including
menoxenia, dyspnea and the symptoms of other organs becoming
influenced by the tumor. However, in the present study, the tumors
were so voluminous that they tended to be symptomatic. The rate of
symptomatic teratomas (69.1%, 228/330) was higher than reported
previously (29.4%) (2). Therefore,
the aim of treatment is to reduce the severity of teratoma-related
symptoms, especially to reduce the mass effect due to the raised
abdominal pressure, and to prevent the potential malignancy.
Following the primary assessment of the clinical
presentation, CA125, or other tumor markers as clinically
indicated, and imaging evaluation are recommended. At ultrasound,
mature teratomas are characterized by echogenic sebaceous material
and calcification (11). At CT, fat
attenuation within a cyst is diagnostic. CT and MRI are
straightforward as these modalities are more sensitive for fat
within the cyst, which is diagnostic for mature cystic teratomas
(12). Immature teratomas,
consisting of elements with only partial somatic differentiation,
usually have a large, irregular solid component containing coarse
calcifications and small foci of fat apparant on CT and MRI scans
(13). However, the appearance of
the tumor at ultrasound is non-specific. In certain instances, it
is difficult to differentiate other germ cell tumors of ovarian
origin, including dysgerminoma and yolk sac tumors, from teratomas.
Compared with these other germ cell tumors, teratomas tend to
exhibit a more heterogeneous appearance with a mixture of fluid,
fat and calcifications, as observed in our patient.
Surgical options to treat teratomas are
individualized by the possibility of chemical peritonitis and
malignancy (3). The existence of
giant mature ovarian teratomas, as suggested by the preoperative
examination and operative inspection, advises the excision of the
tumor. The decision as to whether the whole ovary or only the cyst
was to be removed was made according to the desire to retain
fertility. Shalev et al (2)
suggested that taking a close inspection of pelvic and abdominal
organs with cytological sampling on entering the abdomen aimed at
ruling out possible malignancy. Hysterectomy and bilateral
adnexectomy should be performed with every effort made to keep an
encapsulated mass intact during removal. Adnexectomy was also
performed in patients with adnexal torsion during emergengy surgery
(group 1 vs. group 2, 0 vs. 5.5%, P<0.05), which mostly ocurred
in young females lacking routine gynecological examination.
Although laparoscopic surgery has replaced
laparotomy as the preferred surgical approach for teratomas of
normal size, Teng (14) et
al reported spillage rates of 44–100% during laparoscopic
management and 0–13% during laparotomy. For the laparoscopic
techniques applied to the management of cystic giant teratomas,
prelaparoscopic decompression is necessary to allow for room to
establish pneumoperitoneum and manipulate the tumors, which is not
possible in solid teratomas. Salem (15) reported 15 cases of large ovarian
cysts removed following puncture of their walls. Dolan et al
presented a patient with a giant ovarian cyst, over 40 cm in
diameter, who underwent minilaparotomy drainage followed by
complete laparoscopic extirpation (7). Despite drainage of these cystic tumors
via a minilaparotomy or percutaneous techniques, inadvertent
perforation and spillage must be prevented. In our experience, few
studies concerning the spillage of giant ovarian teratomas over 15
cm in diameter have been published. The spillage rate in the
laparoscopic group was higher than that of the laparotomic group in
the present study (31.5 vs. 19.6%, P<0.05). Inadvertent rupture
may result in granulomatous peritonitis. A retrospective study
covering 20 years and including 26 cases of intraperitoneal
spillage in 314 patients identified 2 patients with postoperative
granulomatous peritonitis, giving an incidence of chemical
peritonitis of 8% in this group of patients (4). However, the data from another
retrospective study of 324 patients who underwent laparoscopic
cystectomy and suffered spillage with irrigation of the abdominal
cavity document a lower incidence (0.3%) (11). Although irrigation of the peritoneal
cavity was also performed in both studies, the difference in
incidence of granulomatous peritonitis may be due to the greater
volumes of irrigant required to render the washings clear as
suggested by Teng et al (14).
A detailed review of previous studies has revealed
that the laparoscopic procedure has rarely been performed on masses
with a diameter larger than 10 cm (2). Howard, in 1995, suggested that it
should not be performed on tumors with a diameter greater than 15
cm (16). By contrast, Shalev and
Peleg (17) recommended
laparoscopic surgery as a routine treatment for the ovarian
teratomas as large as 15 cm in diameter. Decompression of the cyst
followed by laparoscopy may cause rupture in certain conditions. On
the other hand, the variability of manifestations means that giant
ovarian teratomas are easily misdiagnosed as giant abdominal
leiomyosarcoma or liposarcoma. Therefore 219 (66.4%) cases chose
the median laparotomic exploratory incision in the present study
and intraoperative frozen section examination of integrated tumor
delivery has become routine. Suspicion of malignancy based on
preoperative imaging and inspection should preclude the
laparoscopic approach.
The pathological appearance of mature cystic
teratomas is characteristic. Squamous epithelium lines the wall of
the cyst and mesodermal (fat, bone, cartilage, muscle) and
endodermal tissues (e.g., gastrointestinal and bronchial
epithelium, thyroid tissue) are present in the cyst cavity in the
majority of cases (18). The tumors
are unilocular in 88% of cases and filled with sebaceous material,
although the patient had a multilocular tumor in our case.
Immature teratomas differ from mature tumors in that
they demonstrate malignant biological behavior, are much less
common (1% of ovarian teratomas) and affect a younger age group
(usually during the first 2 decades of life) (18). The malignant transformation of
mature cystic teratomas consists of differentiated tissues giving
rise to carcinoma or sarcoma, which is characterized by the
malignant transformation of the squamous epithelium in less than 1%
of cases (19). Sarcomas,
carcinoids and adenocarcinomas have also been reported (20). Slow-growing cysts that reach this
giant size are almost always benign. Therefore, the malignancy rate
was lower in this series, with two (0.61%, 2/330) squamous
malignant transformation histopathologically diagnosed.
Gobel et al (21) wrote in 1998 that surgical therapy
alone is an adequate treatment for patients affected by a mature
teratoma. The risk of recurrence of immature teratomas is strictly
correlated with the histological grading based on the amount of
embryo tissue present, according to WHO’s classification (22). A follow-up strategy is suggested for
immature teratomas at stage I, but is not sufficient for those at
stages II and III with malignant foci (23). Chemotherapy may increase the
disease-free rate of these patients and cause the maturation of
immature tissues. These retroconverted masses may remain stable for
a long period of time (24). The
essential regimen has been BEP for immature teratomas from three to
four cycles following surgery. However, the treatment for the
malignant transformation of mature teratomas is controversial.
Platinum-based chemotherapy may be a reasonable adjuvant therapy
for squamous cell carcinoma arising from mature teratomas (20).
In conclusion, the cornerstone of the study of giant
ovarian teratomas is that the evaluation of possible malignancy,
accidental rupture, rapid growth, doubtful infiltration, large
size, origin and adjacent structures is based on detailed
preparation. We found the prevalence rates of symptomatic tumors,
ovarian torsion and accidental rupture to be higher than those
previously reported in giant ovarian teratomas. Laparotomic
resection may be considered a necessary alternative to laparoscopy
in the management of the giant ovarian teratoma.
However, we cannot confirm that laparotomy could
replace laparoscopy in all instances. With the development of
complicated surgical techniques to meet the avoidance of spillage
and oncological safety, giant ovarian teratomas may be managed
laparoscopically regardless of the size of the tumor.
References
|
1.
|
DJ ChoiEC WallaceAE FraireD BaiyeeBest
cases from the AFIP: intrarenal
teratomaRadiographics25481485200510.1148/rg.25204515315798064
|
|
2.
|
JT Comerci JrF LicciardiPA BerghC
GregoriJL BreenMature cystic teratoma: a clinicopathologic
evaluation of 517 cases and review of the literatureObstet
Gynecol84222819948008317
|
|
3.
|
E ShalevM BustanS RomanoY GoldbergI
Ben-ShlomoLaparoscopic resection of ovarian benign cystic
teratomas: experience with 84 casesHum
Reprod1318101812199810.1093/humrep/13.7.18109740429
|
|
4.
|
W KondoN BourdelB CotteX TranR
BotchorishviliK JardonB RabischongJL PoulyG MageM CanisDoes
prevention of intraperitoneal spillage when removing a dermoid cyst
prevent granulomatous
peritonitis?BJOG11710271030201010.1111/j.1471-0528.2010.02580.x20465557
|
|
5.
|
PP KooningsK CampbellDR Mishell JrDA
GrimesRelative frequency of primary ovarian neoplasms: a 10-year
reviewObstet Gynecol7492192619892685680
|
|
6.
|
F StellaF DavoliGiant mediastinal mature
teratoma with increased exocrine pancreatic activity presenting in
a young woman: a case reportJ Med Case
Reports5238201110.1186/1752-1947-5-23821703035
|
|
7.
|
MS DolanSC BoulangerJR SalamehLaparoscopic
management of giant ovarian cystJSLS10254256200616882432
|
|
8.
|
B CaspiZ AppelmanD RabinersonY ZalelT
TulandiZ ShohamThe growth pattern of ovarian dermoid cysts: a
prospective study in premenopausal and postmenopausal womenFertil
Steril68501505199710.1016/S0015-0282(97)00228-89314922
|
|
9.
|
L HibbardAdnexal torsionAm J Obstet
Gynecol152456461198510.1016/S0002-9378(85)80157-54014339
|
|
10.
|
F GhaemmaghamiF AbbasiAG AbadiA favorable
maternal and neonatal outcome following chemotherapy with
etoposide, bleomycin, and cisplatin for management of grade 3
immature teratoma of the ovaryJ Gynecol
Oncol20257259200910.3802/jgo.2009.20.4.25720041106
|
|
11.
|
C CaldasJ SitzmannCL TrimbleWP McGuire
IIISynchronous mature teratomas of the ovary and liver: a case
presenting 11 years following chemotherapy for immature
teratomaGynecol Oncol4738539019921473754
|
|
12.
|
S GuerrieroG MallariniS AjossaA RisalvatoR
SattaV MaisM AngiolucciGB MelisTransvaginal ultrasound and computed
tomography combined with clinical parameters and CA-125
determinations in the differential diagnosis of persistent ovarian
cysts in premenopausal womenUltrasound Obstet
Gynecol9339343199710.1046/j.1469-0705.1997.09050339.x
|
|
13.
|
JN BuyMA GhossainAA MossM BazotM DoucetD
HugolJB TrucP PoitoutJ EcoiffierCystic teratoma of the ovary: CT
detectionRadiology171697701198910.1148/radiology.171.3.27177412717741
|
|
14.
|
FY TengD MuzsnaiR PerezF MazdisnianA
RossJW SayreA comparative study of laparoscopy and colpotomy for
the removal of ovarian dermoid cystsObstet
Gynecol8710091013199610.1016/0029-7844(96)00061-08649681
|
|
15.
|
HA SalemLaparoscopic excision of large
ovarian cystsJ Obstet Gynecol
Res28290294200210.1046/j.1341-8076.2002.00057.x12512924
|
|
16.
|
FM HowardSurgical management of benign
cystic teratoma. Laparoscopy vs. laparotomyJ Reprod
Med4049549919957473436
|
|
17.
|
E ShalevD PelegLaparoscopic treatment of
adnexal torsionSurg Gynecol Obstet17644845019938480267
|
|
18.
|
EK OutwaterES SiegelmanJL HuntOvarian
teratomas: tumor types and imaging
characteristicsRadiographics21475490200110.1148/radiographics.21.2.g01mr0947511259710
|
|
19.
|
EM DulmetP MacchiariniB SucJM VerleyGerm
cell tumors of the mediastinum. A 30-year
experienceCancer721894190119937689921
|
|
20.
|
L Dos SantosE MokA IasonosK ParkRA SoslowC
AghajanianK AlektiarRR BarakatNR Abu-RustumSquamous cell carcinoma
arising in mature cystic teratoma of the ovary: a case series and
review of the literatureGynecol Oncol105321324200717240432
|
|
21.
|
U GöbelG CalaminusJ EngertTeratomas in
infancy and childhoodMed Pediatr Oncol318151998
|
|
22.
|
G CandelaL Di LiberoS VarrialeF ManettaS
NapolitanoG ScettaD EspositoV SciasciaL SantiniHemoperitoneum
caused by the rupture of a giant ovarian teratoma in a 9-year-old
female. Case report and literature reviewAnn Ital
Chir80141144200919681297
|
|
23.
|
M Lo CurtoP D’AngeloG CecchettoMature and
immature teratomas: results of the first paediatric Italian
studyPediatr Surg Int23315322200717333214
|
|
24.
|
E MoskovicT JoblingC FisherE WiltshawC
ParsonsRetroconversion of immature teratoma of the ovary: CT
appearancesClin
Radiol43402408199110.1016/S0009-9260(05)80570-72070582
|