Introduction
Adenoid cystic carcinoma (ACC) of the breast is a
type of malignant tumor with very low incidence, constituting only
0.1% of all breast carcinomas (1).
In contrast to extra-mammary ACC, which commonly encroaches the
salivary glands, the prognosis of ACC arising in the breast is
excellent. This is due to its slower progressive biological course,
lower metastases of lymph nodes and uncommon distant metastases
(2,3). Generally, it presents with negative
estrogen receptors (ER) and progesterone receptors (PR) in
immunohistochemical testing. With respect to histologic pathology,
its cellular composition comprises ductal epithelioid cells and
basaloid myoepithelial cells (4),
although there is no commonly accepted origination. Leeming et
al showed evidence that ACC originates from the ductal
epithelium and myoepithelium (5).
Due to its favorable prognosis, accurate clinical diagnosis and
differential diagnosis are of significant importance.
The study was approved by the ethics committee of
Nanjing University, Nanjing, China. Informed consent was obtained
from each patient prior to the study.
Case reports
Case 1
A 45-year-old female was admitted to Nanjing Jinling
Hospital, China, complaining of a lump in the right breast which
had appeared 9 months earlier and had been increasing in tenderness
for a week. In the physical examination, the patient’s breasts were
found to be bilaterally symmetrical, without any skin retraction.
Both of the nipples were on the same horizontal line without
discharge or retraction. A mass was palpable in the lower-outer
quadrant 3 cm away from the right nipple, with an approximate size
of 3×5 cm. The mass was tough in texture, irregular in shape,
unclear in boundary and slightly adhesive to surrounding tissues.
There were no positive findings in the left breast. The superficial
lymph nodes were not palpable in the bilateral axillary and
clavicular fossa. The patient had no history of smoking or alcohol
consumption and there was no family history of any types of
tumor.
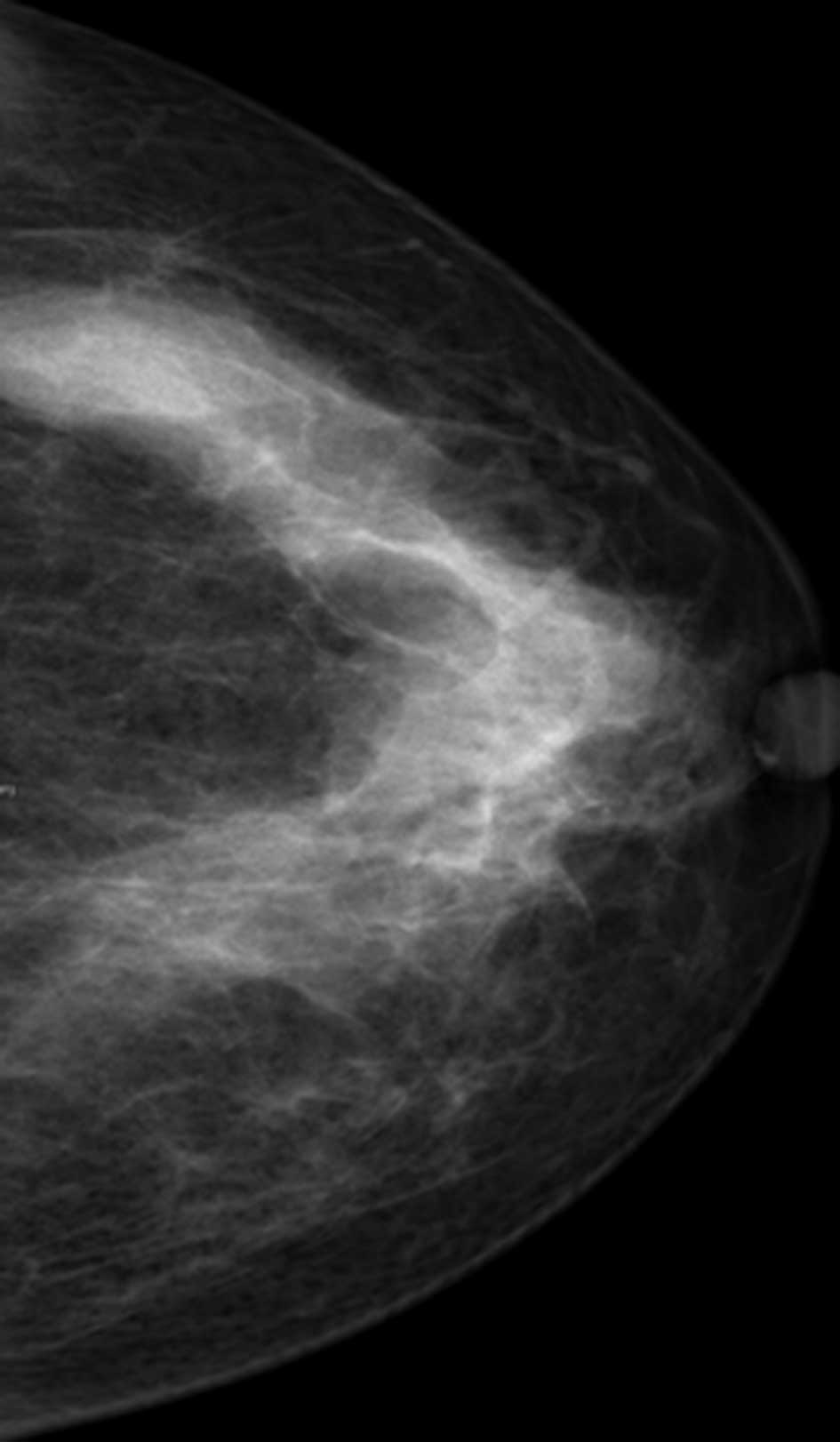
Ultrasonography revealed an ill-defined mass in the
right breast, and its internal echo was non-homogenous. Mammography
revealed a large irregular dense shadow behind the right nipple
which was slightly retracted (Fig.
1). The boundary of the shadow was unclear and the glands
around were gathered without obvious internal calcification.
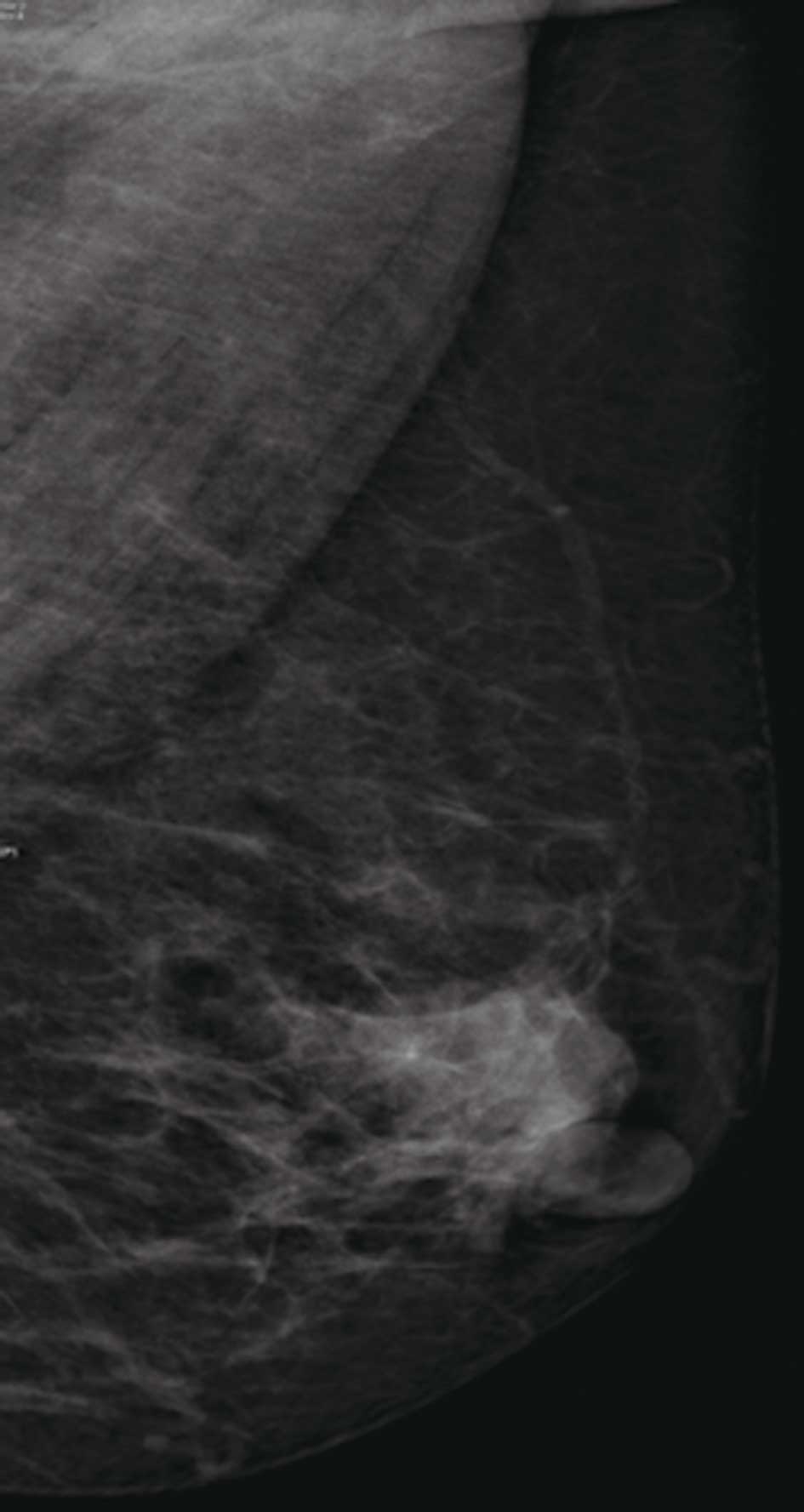
Additionally, mammography revealed shadows of several hollow
swollen lymph nodes in the soft tissue in the anterior of the
ipsilateral axilla (Fig. 2). The
emission computed tomography (ECT) of whole-body bone imaging
showed no signs of tumor metastasis.
The detection of tumor markers showed that serum
carbohydrate antigen (CA) 125 was 96.7 IU/ml and CA 15-3 was 12.4
IU/ml. Other tumor markers were within normal ranges.
Sonographically guided fine-needle aspiration cytology (FNAC) of
the mass was performed in another hospital. The pathology of FNAC
confirmed a myoepithelial derived tumor, the cells of which were
arranged into glandular, cribriform and cord-like patterns. A
simple lumpectomy was also performed in the same hospital. The
pathology of the specimen identified the tumor as ACC of the
breast. Immunohistochemistry of the tumor cells derived from the
myoepithelium revealed ER, PR, calponin and smooth muscle actin
(SMA) to be positive and P63 to be strongly positive. The patient
subsequently underwent a modified radical mastectomy and the
pathology which followed showed adenosis of the breast with
granulomatous inflammation and a foreign-body giant cell reaction.
The margins, basement membrane and nipple were all free of
carcinoma. The lymph nodes were also negative for tumor
metastasis.
We performed the modified radical mastectomy
according to the pathology results, the patient’s economic
situation and with the patient’s consent. One week after surgery,
the patient was given a course of chemotherapy, a combination of
cyclophosphamide, pirarubicin and 5-fluorouracil (CEF), by
intravenous drip before hospital discharge. The patient
subsequently continued her chemotherapy every 3 weeks and is in a
good condition to date.
Case 2
A 39-year-old woman was admitted to our hospital due
to a tender lump in her left breast which had been present for
approximately 3 months. The breast examination revealed a lump
under the nipple, approximately 1.5 cm in diameter. It was tough in
texture and immobile; however, there was no erythema, ecchymosis,
skin ulceration or dimpling. No axillary lymphadenopathy was
detected and there were no positive findings in the laboratory
examinations. The family history was negative for breast cancer and
the patient was not a smoker or alcohol-consumer.
The patient was given a successful lumpectomy and
modified radical mastectomy, and the pathology following surgery
showed ACC of the breast. There were no lymph nodes involved.
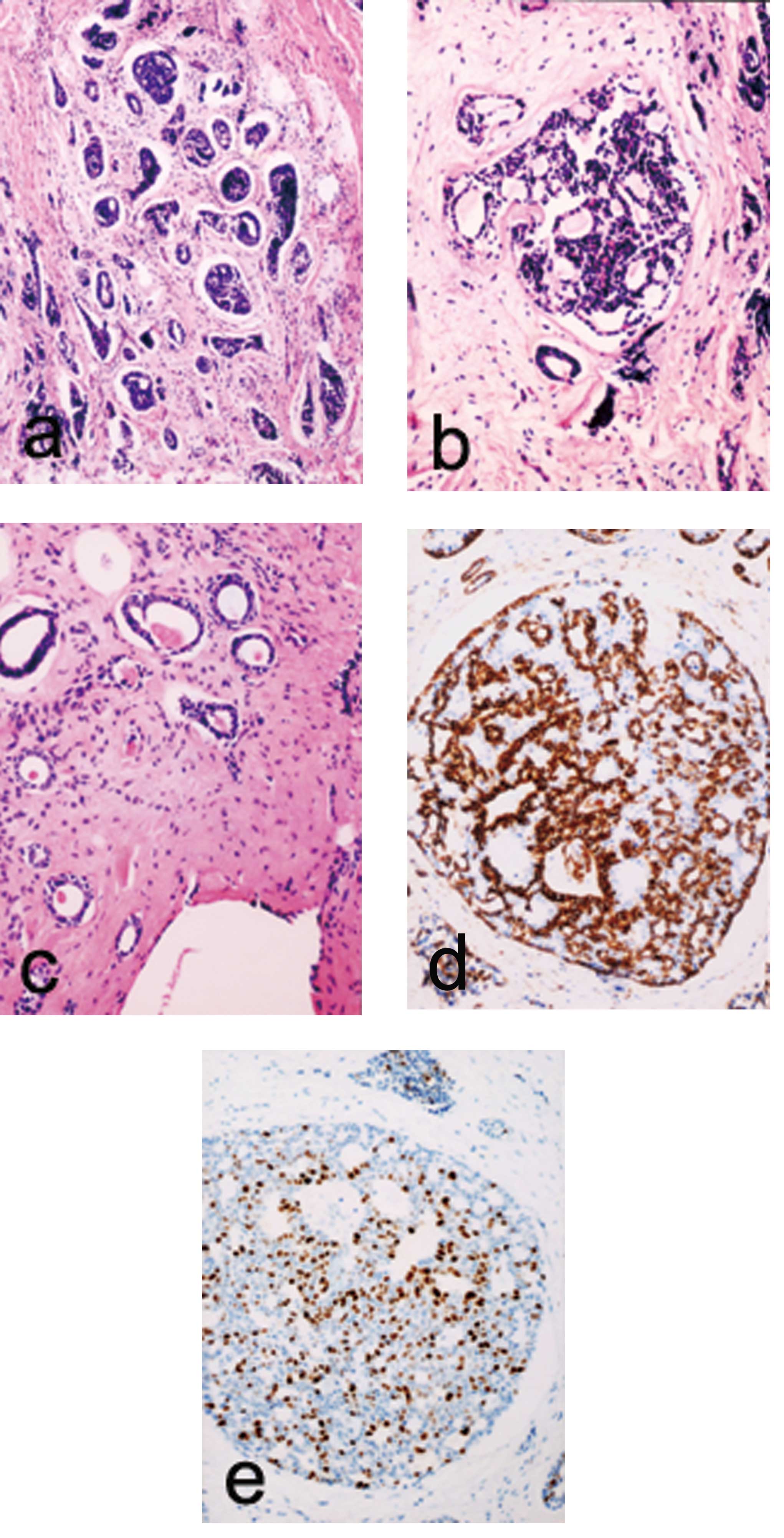
Microscopic examination showed that the tumor cells with different
shapes and less cytoplasm formed typical cribriform islands
(Fig. 3a), inside of which there
was an acidophilic or basopholous mucinous substance (Fig. 3b). Some ducts were scattered and
located around the cribriform structure (Fig. 3c). Immunohistochemistry of the tumor
cells derived from the glandular epithelium showed that ER, PR and
SMA were negative and epithelial membrane antigen (EMA) was
positive. Tumor cells derived from the myoepithelium showed that
SMA was positive and EMA was negative (Fig. 3d). The tumor cell proliferation
marker Ki67 was highly expressed (Fig.
3e). The patient received two courses of chemotherapy (CEF),
and remained in a good condition throughout the 28-month follow-up
period.
Discussion
ACC of the breast is a rare and slowly progressive
carcinoma accounting for 0.1% of all breast carcinomas. It is of
note due to its favorable prognosis and distinctive histological
appearance, since lymph node involvement and distant metastases are
very uncommon. Predominantly, the neoplasm affects women at a mean
age of 50–65 years (1). According
to existing literature, it mainly occurs unilaterally without
predilection for laterality (1).
The most common clinical manifestation of ACC of the
breast is a tender mass, commonly located in the area of the
areola, as was demonstrated in our patients. The nipple is seldom
involved and nipple discharge is uncommon. Spontaneous pain in a
patient may be attributable to the perineural invasion of the
tumor; however, this symptom is uncommon. McClenathan et al
retrospectively analyzed 22 cases and discovered that 10 patients
primarily complained of pain (6).
Several of them felt extreme pain while others complained of local
pain at least one year before an abnormality was found using
medical imaging. Notably, perineural invasion of the tumor was not
evident among the patients experiencing spontaneous pain. In our
second case, the patient complained of tenderness of the lump,
which had been found in the right breast several months
previously.
A review of the existing literature revealed that
the imaging features of ACC of the breast were not as typical and
symptomatic as the clinical manifestation. X-ray radiological
imaging may present ACC as a benign tumor, with a smooth and clear
boundary and regular density, or with a lobulated density and
uneven density shadow. Santamaría et al, combining imaging
appearances with pathological characteristics, discovered that the
majority of carcinomas were located in the upper quadrant of the
breast or in the area of the areola (7). In mammography, ACC may present as a
circumscribed lobulated nodule. When the boundaries of the nodular
shadow were unclear or partially unclear, microscopic invasion was
usually found (7). Inside the tumor
lesion there may be calcifications, which are generally observed in
histology but infrequently detected in mammography. Saqi et
al noted that it was significant to make full use of FNAC for
the early diagnosis of ACC of the breast (8).
Lymph node metastases as well as distant metastases
of ACC in the breast are rare. Sumpio et al reviewed 120
cases from the literature and showed lymph node metastases in only
4 cases, and distant metastases in only 8 cases, the majority of
which occurred in the lung (9). In
another series of 182 cases, Arpino et al noted fewer than
10 cases with lymph node metastases and only 14 cases with distant
metastases in the 10 years following surgery (10). However, distant metastases may
occur, most frequently in the lung, without sentinel lymph node
involvement. In the present case reports, all the lymph nodes sent
for pathological biopsy were negative for tumor cells.
With regard to pathology, ACC of the breast is
mainly composed of two types of cells; ductal epithelioid cells and
basaloid myoepithelial cells, which form circumscribed clusters of
cells arranged in solid, cribriform, tubular and trabecular
arrangements, although one pattern may predominate (4). According to its various growth
patterns, ACC of the breast may be classified as cribriform,
tubular or solid types. The cribriform type is the most symptomatic
and most frequently presented, while the solid type occurs
comparatively seldom (11). The
differential diagnosis of the carcinoma includes cribriform ductal
carcinoma in situ, invasive cribriform carcinoma, invasive
ductal carcinoma and benign tumors such as collagenous spherulosis.
The negative expression of ER and PR helps to distinguish ACC from
cribriform ductal carcinoma in situ, which lacks the
basement membrane-like material found in the lumens of ACC.
Invasive cribriform carcinomas and ductal carcinomas in situ
also present ER and PR; however, the invasive cribriform carcinoma
lacks myoepithelial cells related to its invasive characteristics.
The collagenous spherulosis has acidophilic spherules rich in
collagen, which have positive PAS (Periodic Acid-Schiff) staining
and accompany usual type epithelial hyperplasia. ACC of the solid
type is similar to ordinary ductal carcinoma. Acs et al
reported 17 cases of ACC coexisting with microglandular adenosis
(MGA) and suggested that ACC may develop in the background of and
in continuity with MGA (12).
As the prognosis of ACC is related to the
histological grade, Ro et al (13) suggested that ACC of the breast may
be classified into three grades according to the proportion of
solid growth elements of the tumor. Tumors of grade I are made up
of glandular and ductal structures without any solid elements.
Tumors of grade II include less than 30% solid elements and grade
III tumors include more than 30%. This grading was found to be of
great significance in treatment and prognosis. As the percentage of
solid elements increases, so does the risk of tumor development and
postoperative recurrence (3,7)
Arpino et al (10) reviewed the molecular markers,
treatment and clinical outcomes of 28 cases of ACC of the breast.
Having analyzed the DNA of the tumors, they found that 92% of the
patients were DNA diploid, whereas the frequency of DNA aneuploidy
in invasive breast carcinomas was approximately 60–65%. AAC of the
breast also showed lower proliferative activity with PR and ER
usually negative. Leeming et al (5) reviewed 140 cases and found only one
case positive in ER. However, in a different group, which consisted
of 14 cases, there were 4 positive in ER and in a separate group of
13, there were 3 positive in PR (6). Similarly, Kleer et al (14) analyzed 19 cases and found 5 positive
in ER. In this case, both ER and PR were positive in the tumor
cells. Based on the above, ACC of the breast may not be completely
distinguished from other invasive breast carcinomas according to ER
and PR expression alone.
The optimal treatment of ACC of the breast has not
yet been determined due to its low incidence. The reviewed
literature shows several surgical treatment modalities ranging from
a simple lumpectomy without radiotherapy to a radical mastectomy.
The radical mastectomy is not advised due to the high risk of
physical and psychological damage to patients and the low incidence
of nodal metastasis of the tumor. McClenathan et al
(6) suggested that even limited
lymph node dissection was unwarranted. Instead, the simple
mastectomy has widely been used and is preferred by many surgeons.
The simple lumpectomy has the advantages of lower operative damage,
less postoperative discomfort and faster recovery; however, it is
associated with unacceptably high rates of local recurrence. As a
result, it is necessary to combine the lumpectomy with adjuvant
systemic chemotherapy or local radiotherapy with discretion.
According to the pathological grading suggested by Ro et al
(13), the proposed treatment is
simple lumpectomy for grade I tumors, simple mastectomy for grade
II tumors and mastectomy with axillary clearance for grade III
tumors. With respect to adjuvant chemotherapy, hormonal
manipulation and bio-immunotherapy treatments of ACC of the breast,
there are still few studies to date. To find the optimum treatment,
prospective clinical trials need to compare the different
treatments, which may prove difficult to conduct in such a rare
neoplasm.
There are several studies which have investigated
the postoperative recurrence rates of ACC of the breast. Literature
overviews revealed higher rates of local recurrence following
simple lumpectomy. Santamaría et al (7) reviewed 182 cases following surgery and
found 14 cases of local recurrence, of which 11 recurred after
simple lumpectomy, one after simple mastectomy and 2 after radical
or modifed mastectomy. Sumpio et al (9) reported 6 cases of local recurrence
following simple lumpectomy, out of a total of 8 cases. Leeming
et al (5) noted that 9 out
of 24 patients suffered from local recurrence following simple
lumpectomy, a recurrence rate of 37%. Youk et al (15) described a case of local recurrence
following successful treatment by lumpectomy and systemic
chemotherapy and radiotherapy.
ACC of the breast is a type of rare carcinoma with
relatively typical clinical presentation. The diagnosis may be made
by the combination of imaging and pathology; however, there is
still no consensus on the standard treatment. Despite the favorable
prognosis, there are reports of local recurrences and distant
metastases following treatment. As a result, it is necessary for
the patients to be closely followed-up and periodically examined
following treatment.
References
|
1.
|
YM LawST QuekPH TanSL WongAdenoid cystic
carcinoma of the breastSingapore Med J50e8e11200919224074
|
|
2.
|
FJ CavanzoHB TaylorAdenoid cystic
carcinoma of the breast: an analysis of 21
casesCancer2474074519694309694
|
|
3.
|
GN PetersM WolffAdenoid cystic carcinoma
of the breast. Report of 11 new cases: Review of the literature and
discussion of biological behaviorCancer5268068619836305483
|
|
4.
|
S AzoulayM LaéP FréneauxS MerleKIT is
highly expressed in adenoid cystic carcinoma of the breast, a
basal-like carcinoma associated with a favorable outcomeMod
Pathol1816231631200516258515
|
|
5.
|
R LeemingM JenkinsG MendelsonAdenoid
cystic carcinoma of the breastArch
Surg127233235199210.1001/archsurg.1992.014200201270191311551
|
|
6.
|
JH McClenathanG de la RozaAdenoid cystic
breast cancerAm J
Surg183646649200210.1016/S0002-9610(02)00858-912095593
|
|
7.
|
G SantamaríaM VelascoG ZanónB
FarrúsAdenoid cystic carcinoma of the breast: mammographic
appearance and pathologic correlationAm J
Roentgenol1711679168319989843312
|
|
8.
|
A SaqiCL MercadoD Hamele-BenaAdenoid
cystic carcinoma of the breast diagnosed by fine-needle
aspirationDiagn Cytopathol30271274200415048965
|
|
9.
|
BE SumpioTA JenningsMJ MerinoPD
SullivanAdenoid cystic carcinoma of the breast. Data from the
Connecticut Tumor Registry and a review of the literatureAnn
Surg205295301198710.1097/00000658-198703000-000133030200
|
|
10.
|
G ArpinoGM ClarkS MohsinVJ BardouAdenoid
cystic carcinoma of the breast: molecular markers, treatment and
clinical outcomeCancer9421192127200210.1002/cncr.1045512001107
|
|
11.
|
WT YangTQ ZhangMC ShenAdenoid cystic
carcinoma of the breast: report of four cases and review of the
literatureJ Clin Exp Pathol2110132005
|
|
12.
|
G AcsJF SimpsonIJ BleiweissJ
HughMicroglandular adenosis with transition into adenoid cystic
carcinoma of the breastAm J Surg
Pathol2710521060200310.1097/00000478-200308000-0000212883237
|
|
13.
|
JY RoEG SilvaHS GallagerAdenoid cystic
carcinoma of the breastHum
Pathol1812761281198710.1016/S0046-8177(87)80413-62824330
|
|
14.
|
CG KleerHA ObermanAdenoid cystic carcinoma
of the breast: value of histologic grading and proliferative
activityAm J Surg
Pathol22569575199810.1097/00000478-199805000-000089591727
|
|
15.
|
JH YoukMJ KimEK KimJY LeeRecurrence of
adenoid cystic carcinoma in the breast after lumpectomy and
adjuvant therapyJ Ultrasound Med25921924200616798905
|