Introduction
Thyroid surgery, in particular to treat giant
thyroid gland tumor, is a potentially dangerous operation due to
the long course of disease and the surrounding anatomical changes,
meaning that the incidence of intra- and postoperative
complications is likely to be higher than in cases with normal
thyroid nodules. Thyroidectomy is one of the most frequent
surgeries performed in patients with giant thyroid gland tumors,
especially those with thyroid cancer (1). Improvements in anesthesia and
antisepsis, as well as better surgical instrumentation and
improvements in surgical technique, have rendered thyroidectomy an
efficacious and safe treatment modality with acceptable morbidity
and even unrecorded mortality. However, the optimal extent of
thyroid resection and lymph node dissection remain controversial.
Central compartment node dissection (CCND) is usually performed
with near-total thyroidectomy (NTT) for prophylactic purposes.
while lateral neck dissection (LND) is performed only when thyroid
carcinoma is pathologically confirmed according to the National
Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in
Oncology. (http://www.nccn.org/professionals/physician_gls/f_guidelines.asp#thyroid)
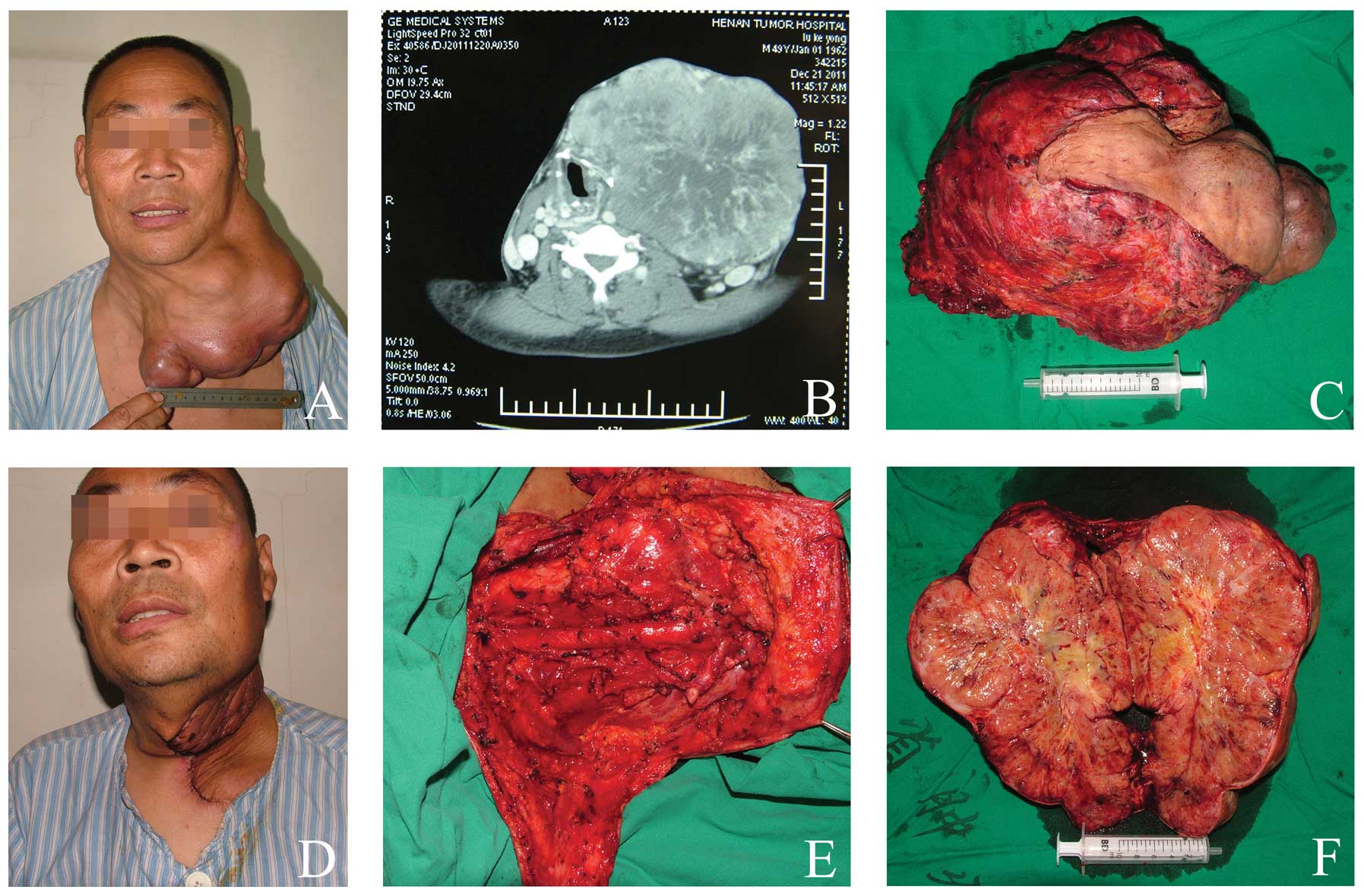
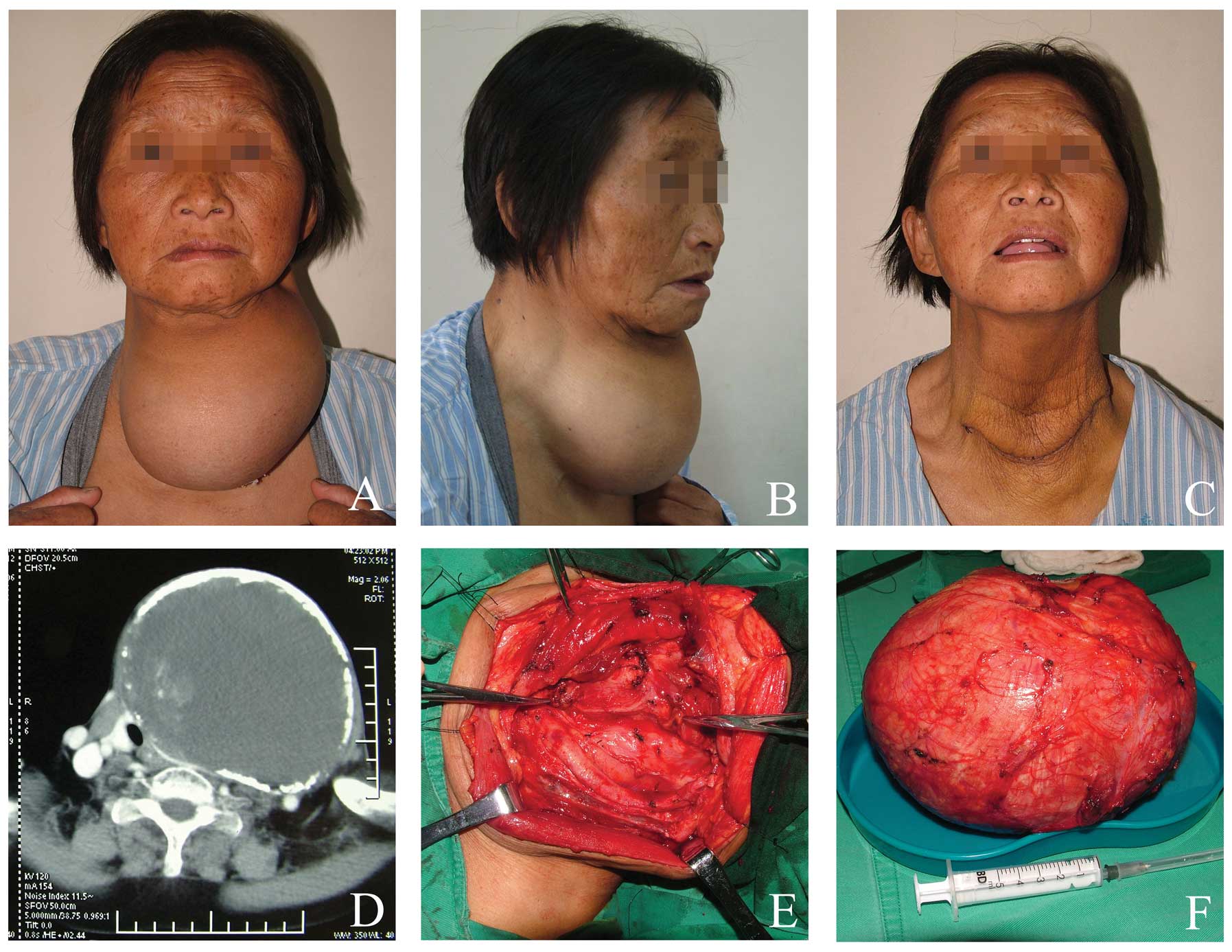
A giant thyroid gland tumor (Figs. 1 and 2) is defined as any thyroid with an
average weight greater than 500 g, a diameter greater than 10 cm,
extending up to the mandibular angle, a lower level extended to the
sternum and in which both sides of the posterior border are
normally sternocleidomastoid muscle. The main concern is the
potentially high rate of complications, including hematoma,
permanent recurrent laryngeal nerve (RLN) paralysis and
hypoparathyroidism (2,3). In this study, we present our
experience with several complications of surgical treatment of
giant thyroid gland tumors to increase the awareness and aid the
prevention of these complications.
Patients and methods
Patients
A total of 137 patients who underwent giant thyroid
gland tumor surgery at the Thyroid Disease Diagnosis and Treatment
Center (Department of Head and Neck, Henan Tumor Hospital,
Zhengzhou University, Henan, China) between January 2001 and
December 2010 approved a retrospective review of the images and
medical records.
According to the retrospective review of the images
and medical records of patients over 10 years, all patients
underwent routine measurements of serum calcium, phosphorus, WBC,
and parathyroid hormone levels pre-postoperative and examination of
vocal cord movement by direct laryngoscopy Complication rates were
assessed according to the extent of surgery, which was classified
as follows: NTT (group I, n=71); total thyroidectomy (TT; group II,
n=24); NTT-CCND (group III, n=11); TT-CCND (group IV, n=19); TT-LND
(group V, n=12).
Patients’ charts were reviewed for patient
demographics and clinicopathological characteristics, inlcuding
age, gender, history, the length of hospitalization, tumor size,
comorbid disease (including hypertension, cardiac disease and
diabetes mellitus) and pathological diagnosis. Complication rates
according to the extent of thyroid surgery included RLN injury
(permanent or transient), symptomatic hypoparathyroidism (permanent
or transient), incision site infections, bleeding, chyle fistula
and Horner’s syndrome. All patients with intra- or postoperative
complications attended our endocrine outpatient clinic at regular
intervals until 5 years after the surgery. During follow-up visits,
a complete patient evaluation was performed, including medication,
physical examination and blood sampling for serum calcium levels.
Patients who developed a postoperative complication and were unable
to attend the outpatient clinic were consulted by telephone. Local
Ethical Committee approval was granted for the use of surgical
trimming and informed consent was also obtained from the patients
prior to surgery.
Statistical analysis
The intra- and postoperative complications and their
rates were assessed for each of the five patient groups and
comparisons among groups were made using Fisher’s exact test; when
necessary, data were transformed to obtain results distributed with
equal variance. Pearson’s Chi-square test was used to assess the
correlations among the groups. P<0.05 was considered to indicate
a statistically significant result. All analyses were performed
using statistical package for social science (SPSS), version 13.0
(SPSS Inc., Chicago, IL, USA).
Results
Patient characteristics
From a review of medical records, 137
thyroidectomies were identified. Of the patients, 121 (88%) were
operated on for the first time and there were 16 (12%)
reoperations. There were 26 males and 111 females, with a mean age
of 47.8 years (Table I). The mean
history period was 4.9 years and the mean duration of
hospitalization was 8.2 days. The 137 cases evaluated were split
into two groups according to pathological diagnosis: i) 98 (72%)
patients who had benign pathology, including 71 thyroid adenoma
(52%) patients and 27 (20%) patients with nodular goiters (Fig. 2); and ii) 39 (28%) patients with a
malignant pathology (Fig. 1). The
latter malignant pathologies were differentiated in 36 (26.3%)
cases, medullary in 2 (1.5%) and undifferentiated in 1 (0.7%), 39
totally (28.5%). Patients’ data on the indications for surgery,
operative time, length of hospital stay, age and gender are listed
in Table I.
 | Table IDemographic and clinicopathological
characteristics of patients. |
Table I
Demographic and clinicopathological
characteristics of patients.
| Parameters | Total (n=137) | Group I (n=71) | Group II
(n=24) | Group III
(n=11) | Group IV
(n=19) | Group V (n=12) |
|---|
| Age (mean,
years) | 47.8 | 48.6 | 47.4 | 46.9 | 45.5 | 49.3 |
| Gender
(male:female) | 26:111 | 12:59 | 4:20 | 3:8 | 4:15 | 3:9 |
| History (mean,
years) | 4.9 | 5.1 | 4.6 | 3.9 | 4.3 | 6.7 |
| Tumor size (mean,
cm) | 13.1 | 11.6 | 15.1 | 13.0 | 14.3 | 16.2 |
| Comorbid
diease | | | | | | |
| Hypertension
(n) | 19 | 10 | 3 | 2 | 3 | 1 |
| Diabetes mellitus
(n) | 12 | 6 | 2 | - | 2 | 2 |
| Cardiac disease
(n) | 13 | 5 | 4 | 1 | 1 | 2 |
| Capsular invasion
(%) | 54.5 | 31.4 | 55.8 | 72.6 | 73.2 | 78.9 |
| Pathological
diagnosis | | | | | | |
| Thyroid
adenoma | 71 | 54 | 17 | - | - | - |
| Nodular
goiter | 27 | 15 | 12 | - | - | - |
| Thyroid
carcinoma | 39 | - | 7 | 9 | 21 | 2 |
| Hospital stay
(mean, days) | 8.2 | 6.9 | 8.2 | 9.3 | 10.5 | 11.2a |
| Surgery time (mean,
minutes) | 126.3 | 107.2 | 115.1 | 140.7 | 155.9 | 201.6 |
Complications
In the present study, permanent RLN injury was found
in 2.9% of cases (Table II). A
total of 54% of surgeons individuated the RLN, 42% uncovered it
anatomically and 4% did not search for it. However, the temporary
RLN injury incidence rates increased with increasing extent of
surgery, with incidences of 1.4, 8.4, 9.1, 10.5 and 16.7% in groups
I, II, III, IV and V, respectively (Table II). All the surgeons noted care was
taken not to injure the external branch of the laryngeal superior
nerve (LSN). LSN injury was diagnosed by an otolaryngologist
following indirect laryngoscopy or videolaryngostroboscopy of the
patients with difficulty in producing a high-pitched voice.
 | Table IIIntra- and postoperative rates
according to the extent of thyroid surgery. |
Table II
Intra- and postoperative rates
according to the extent of thyroid surgery.
| Percentage of cases
(n)
|
|---|
| Parameters | Total (n=137) | Group I (n=71) | Group II
(n=24) | Group III
(n=11) | Group IV
(n=19) | Group V (n=12) |
|---|
|
Hypoparathyroidism | | | | | | |
| Transient | 16.8 (23) | 5.6 (4) | 20.8 (5) | 27.3 (3) | 31.6 (6) | 41.7 (5) |
| Permanent | 2.9 (4) | 1.4 (1) | - | 9.1 (1) | 5.3 (1) | 8.3 (1) |
| EB-LSN lesions | | | | | | |
| Transient | 5.1 (7) | 2.8 (2) | 4.2 (1) | 9.1 (1) | 10.5 (2) | 8.3 (1) |
| Permanent | 2.1 (3) | - | 4.2 (1) | - | 5.3 (1) | 8.3 (1) |
| RLN lesions | | | | | | |
| Transient | 5.8 (8) | 1.4 (1) | 8.4 (2) | 9.1 (1) | 10.5 (2) | 16.7 (2) |
| Permanent | 2.9 (4) | - | 4.2 (1) | 9.1 (1) | 5.3 (1) | 8.3 (1) |
| Wound
infection | 3.6 (5) | 1.4 (1) | 4.2 (1) | 9.1 (1) | 5.3 (1) | 8.3 (1) |
| Flap edema | 5.1 (6) | 1.4 (1) | - | 9.1 (1) | 10.5 (2) | 16.7 (2) |
| Hematoma | 2.9 (4) | 1.4 (1) | 4.2 (1) | - | 5.3 (1) | 8.3 (1) |
| Chyle
fistula | 2.9 (4) | 1.4 (1) | - | 9.1 (1) | 5.3 (1) | 8.3 (1) |
| Horner’s
syndrome | 2.2 (3) | - | - | 9.1 (1) | 5.3 (1) | 8.3 (1) |
Symptomatic hypocalcemia, which was observed in 27
(19.7%) patients (16.8% transient), accounted for 37.5% of all
complications. The incidence of transient hypoparathyroidism was
5.6, 20.8, 27.3, 31.6 and 41.7% in groups I, II, III, IV and V,
respectively. Definitive permanent hypocalcemia following surgical
interventions for thyroid cancer was higher, particularly with the
extent of surgery.
Transient or permanent LSN injury was observed in 10
patients (7.3%; statistically significant). Hemorrhage accounted
for 2.9% (4/137) of the total complications and was not
statistically significant in groups I–V or associated with the
extent of surgery.
Discussion
Due to new monitoring technology, the incidence rate
of thyroid gland tumor has been increasing over recent years
(4) with no change in mortality
rates. Of these tumors, 50% have a diameter less than 2 cm and the
incidence rate of giant thyroid gland tumors, especially those with
a diameter greater than 10 cm, is lower.
Thyroid surgery takes place in an area of
complicated anatomy in which a number of vital physiological
functions and senses are controlled. Improved knowledge of the
surgical anatomy of the neck, thyroid pathology and required
surgical treatment is essential to keep complications within
reasonable limits (5).
Complications are often dependent on physical factors, including a
large or intrathoracic goiter, extensive malignancy and whether the
surgery is a primary or secondary procedure (6). The three main complications following
thyroid surgery are RLN palsy, hypoparathyroidism and postoperative
hemorrhage (7). In the present
study, we found that intra- and postoperative complications
following thyroid surgery may include transient or permanent
hypoparathyroidism, transient or permanent EB-SLN lesions,
transient or permanent RLN lesions, wound infection, hematoma,
chyle fistula, Horner’s syndrome and injury to motor nerves in the
neck.
Hyperparathyroidism is a major concern leading to
prolonged hospitalization and increased cost. In several studies
(1,6,8), the
incidence of transient hypocalcemia varied from 6.9 to 46%, while a
rate of 0.4 to 33% has been reported for permanent
hypoparathyroidism. In the present study, transient
hypoparathyroidism occurred in 16.8% of cases. Patients with
permanent hypoparathyroidism require life-long treatment with
calcium and vitamin D, so this complication is considered serious.
Certain authors (2,9) believe that a single functioning gland
is sufficient to restore normal parathyroid activity, whereas
others suggest that the integrity of at least three glands is
necessary (10). Transient
hypoparathyroidism, however, rarely affects quality of life. In our
series, the incidence rates of transient and permanent
hypoparathyroidism increased significantly with increasing extent
of surgery. Therefore it is necessary to take certain technical
precautions to reduce as much as possible the incidence of
persistent hypocalcemic complications.
Transient or definitive injuries to the RLN are the
most serious complications as they influence the patient’s quality
of life, similar to permanent hypoparathyroidism. The incidence of
permanent RLN injury has been reported to range between 0 and 4%
(11,12), similar to that found in the present
study. The permanent RLN lesions occurred less often in group I.
However, there was a mild increase in transient monoplegia and a
similar incidence of diplegia in this group. Although prevention of
injury can never be absolute, careful observation during every
operative step to monitor the wide range of possible variations in
the course of the nerve should substantially reduce the risk
(13). Certain studies compared the
complication rates associated with total and subtotal thyroidectomy
in benign nodular disease and did not identify any significant
difference between the two procedures (2,6,13). In
the present study, the preferred surgical technique did not
influence postoperative complication rates. Dralle et al
(14) concluded that routine visual
nerve identification and preservation should be the gold standard
in thyroid surgery. In our institution, intra-operative nerve
identification is the standard practice and thus was not analyzed
as an independent risk factor. In fact, certain surgeons believe
that it is important to save some thyroid tissue around the nerve
junction to the larynx, and some skilled, experienced surgeons have
obtained a low nerve injury rate without deliberate routine nerve
exposure. When cord paralysis with dysphonia occurs days or weeks
following surgery, the surgeon should consider that the symptom is
associated with RLN injury. It is important to start logopedic
rehabilitation early (within 2–3 weeks) in all cases of vocal cord
paralysis. Patients with vocal cord palsy should start logopedic
rehabilitation as early as possible.
Although innervating only one muscle, the
cricothyroideus, the LSN is important in providing a normal voice.
The role of this nerve and its muscle is to tense the vocal cords,
providing timbre to the voice. LSN transient or permanent injuries
are relatively frequent and are often underestimated. Although
certain surgeons insist on direct visualization of the external
branch of the superior laryngeal nerves in all cases, most surgeons
do not, considering it unnecessary in most cases as the nerve is
not thought to be at risk (2,3,12). It
is rarely possible to individuate the external branch of the LSN
easily and immediately as it is extremely thin or incorporated in
the lower pharyngeal constrictor muscle sheath. An obstinate
anatomical search may cause nerve damage. It should be noted that
approximately 20% of patients are at risk of injury to the external
branch of the LSN when the superior thyroid vessels are clamped,
divided and ligated en masse, a technique that was commonly used
prior to the anatomy of the external branch with its variations
being well described.
Hematoma following thyroidectomy is a life-threating
early complication of thyroid surgery in various series and its
incidence rate is reported to be 0.3–1.5% (15). In the present study, hematoma was a
complication in 2.9% of cases and reoperation was undertaken in 9
due to ongoing hemorrhage and airway obstruction. None required
reopening of the wound.
Chyle fistula and Horner’s syndrome are rare and
troublesome complications. Chyle fistula is usually identified upon
postoperative commencement of an oral diet and is indicated by
milky drainage, a sudden increase in drainage volume, bulging
supraclavicular fossa and induration or erythema of the skin
(1,3,16,17).
Horner’s syndrome is usually associated with unique clinical
features based on the anatomical location of the underlying
pathological process. Careful dissection around the prevertebral
fascia and the carotid sheath is necessary to avoid injury to the
sympathetic chains when performing a radical neck dissection.
Flap edema (Figs. 1
and 2) rates were higher in
patients who had a large gland size and were operated on by the
resident surgeon. The incidence of flap edema varied in total from
0.3 to 7% (1,15). Flap edema may be due to inadequate
surgical technique with damage of the lymphatic vessels and results
in poor venous circulation due to hemostasis over the ligation.
At the beginning of the 20th century, postoperative
infection was a major complication of thyroidectomy. At present,
with the benefit of antisepsis and the constant progress of
surgical techniques, the overall risk of postoperative wound
infection is substantially decreased. In our series, infection
occurred in 5 cases (3.6%), all of which were successfully managed
with wound debridement and antibiotics. We did not identify any
association between wound infection and extent of thyroid
resection. No differences were noted among patients administered an
antibiotic as prophylaxis, therapy or not at all.
In conclusion, these complications of thyroidectomy
may cause significant difficulty for patients and a significant
sense of discomfort for the surgeon. The results of our study
suggest that most giant thyroid gland tumor surgeries are safe and
may be performed with minimal morbidity, but an increased risk of
surgical complications, particularly hypoparathyroidism, remains a
problem that needs be solved in patients who require more extensive
surgery. Low complications rates may be achieved with more detailed
knowledge of the surgical anatomy, skilled surgical treatment and
experience. It is clear that to achieve low complication rates,
surgeons should be appropriately trained, follow best practice and
maintain their level of commitment and good communication until the
outcome is ensured.
Acknowledgements
We gratefully acknowledge members of
the Department of Medical Records Room and Data Center, Henan Tumor
Hospital, Zhengzhou University, for their excellent technical
assistance.
References
|
1.
|
R Moulton-BarrettR CrumleyS JalilieD
SeginaG AllisonD MarshakE ChanComplications of thyroid surgeryInt
Surg8263661997
|
|
2.
|
C DenerComplications rates after
operations for benign thyroid diseaseActa
Otolaryngol122679683200210.1080/00016480232039639412403134
|
|
3.
|
SE OlsonJ StarlingH ChenSymptomatic benign
multi-nodular goiter: unilateral or bilateral
thyroidectomy?Surgery142458462200710.1016/j.surg.2007.07.00317950336
|
|
4.
|
A Rego-IraetaLF Pérez-MéndezB MantinanRV
Garcia-MayorTime trends for thyroid cancer in northwestern Spain:
true rise in the incidence of micro and larger forms of papillary
thyroid
carcinomaThyroid19333340200910.1089/thy.2008.021019355823
|
|
5.
|
RD BlissPG GaugerLW DelbridgeSurgeon’s
approach to the thyroid gland: surgical anatomy and the importance
of techniqueWorld J Surg248918972000
|
|
6.
|
NN al-SulimanNF RyttovN QvistM
Blichert-ToftHP GraversenExperience in a specialist thyroid surgery
unit: a demographic study, surgical complications, and outcomeEur J
Surg163132019979116105
|
|
7.
|
S OzbasS KocakS AydintugA CakmakMA
DemirkiranGC WishartComparison of the complications of subtotal,
near total and total thyroidectomy in the surgical management of
multinodular goitreEndocr
J52199205200510.1507/endocrj.52.19915863948
|
|
8.
|
RC PercivalAW HargreavesJA KanisThe
mechanism of hypocalcemia following thyroidectomyActa Endocrinol
(Copenh)10922022619854013612
|
|
9.
|
AR SassonJF Pingpank JrRW WetheringtonAL
HanlonJA RidgeIncidental parathyroidectomy during thyroid surgery
does not cause transient symptomatic hypocalcaemiaArch Otolaryngol
Head Neck Surg127304308200110.1001/archotol.127.3.304
|
|
10.
|
F PattouF CombemaleS FabreB CarnailleM
DecoulxJL WemeauA RacadotC ProyeHypocalcemia following thyroid
surgery: incidence and prediction of outcomeWorld J
Surg22718724199810.1007/s0026899004599606288
|
|
11.
|
NG IyerAR ShahaManagement of thyroid
nodules and surgery for differentiated thyroid cancerClin
Oncol22405412201010.1016/j.clon.2010.03.00920381323
|
|
12.
|
SS AbadinEL KaplanP AngelosMalpractice
litigation after thyroid surgery: the role of recurrent laryngeal
nerve injuries, 1989–2009Surgery148718722201020709343
|
|
13.
|
PS HuntM PooleTS ReeveA reappraisal of the
surgical anatomy of the thyroid and parathyroid glandsBr J
Surg556366196810.1002/bjs.18005501195635426
|
|
14.
|
H DralleC SekullaJ HaertingW TimmermannHJ
NeumannE KruseS GrondHP MühligC RichterJ VossRisk factors of
paralysis and functional outcome after recurrent laryngeal nerve
monitoring in thyroid
surgerySurgery13613101322200410.1016/j.surg.2004.07.01815657592
|
|
15.
|
F TaneriO KurukahveciogluB EgeU YilmazE
TekinC CifterE OnukProspective analysis of 518 cases with
thyroidectomy in TurkeyEndocr Regul398590200516468230
|
|
16.
|
RT GregorManagement of chyle fistulization
in association with neck dissectionOtolaryngol Head Neck
Surg122434439200010699823
|
|
17.
|
GK RodgersJT JohnsonGJ PetruzzelliVS
WartyRL WagnerLipid and volume analysis of neck drainage in
patients undergoing neck dissectionAm J
Otolaryngol1330630919921285563
|