Introduction
Female urethral carcinoma is rare and accounts for
approximately 0.02% of all female cancers and less than 1% of
cancers in the female genitourinary tract (1). In females, squamous cell carcinoma is
the most common histological type, accounting for 70% of all cases.
Transitional cell carcinoma (20%) and adenocarcinomas (8–10%) are
the next most common cell types (2). Most patients are symptomatic at
presentation. Certain patients may present with obstructive
symptoms, dysuria, urethral bleeding, urinary frequency and often a
palpable urethral mass or induration. The evaluation of females
with suspected urethral carcinoma includes cystourethroscopy,
physical examination, CT and MRI of the abdomen and pelvis and
chest radiography. The prognosis is determined largely by the
clinical stage and the location of the lesions. Tumors in the
distal urethra tend to have a better outcome (3).
Primary adenocarcinoma of the female urethra is
extremely rare with only a few retrospective cases published. We
report two cases of female urethral adenocarcinoma, including a
rare case of mucinous adenocarcinoma. The study was approved by the
ethics committee of Zhongshan Hospital, Xiamen University, China.
Informed consent was obtained from each patient.
Case 1
A 44-year-old female patient complained of painless
occasional urethral bleeding over the previous 2 months. Physical
examination revealed a reddish hemispheroid mass measuring 15 mm in
diameter without bleeding or tenderness at the posterior lip of the
urethral meatus. No enlarged inguinal lymph nodes were identified.
Serum studies were normal and urinalysis revealed numerous red
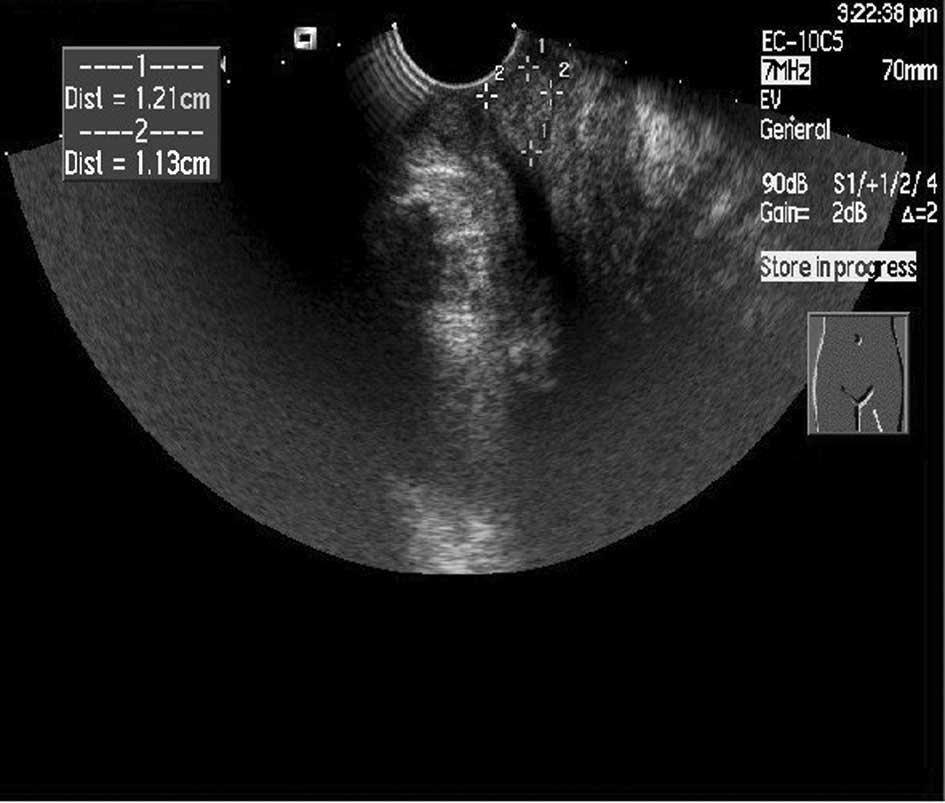
blood cells per high power field. Transvaginal ultrasonography of
the urethra revealed a well-defined hyperechoic mass with abundant
blood flow, with approximate dimensions of 12x11x10 mm (Fig. 1). Abdominal and pelvic CT scan with
contrast and chest rediology was unremarkable. Biopsy of the mass
revealed adenocarcinoma of the urethra. The patient underwent
partial urethectomy and frozen-section pathology was performed to
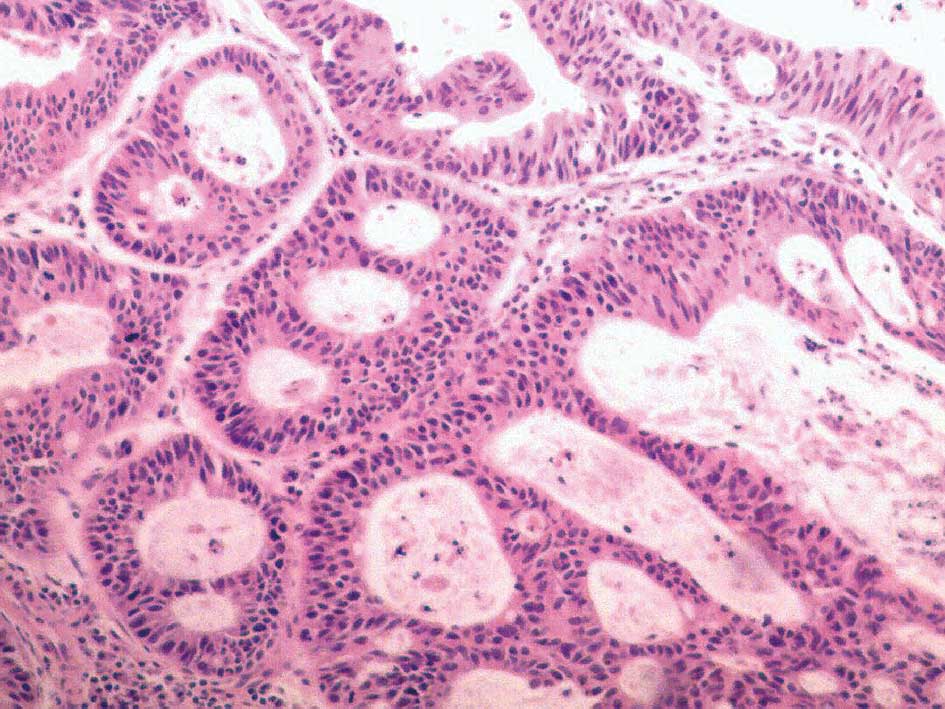
ensure an adequate margin. Subsequent routine pathology reported
adenocarcinoma of the urethra with a free margin consistent with
the previous pathology report (Fig.
2). The patient recovered without complication and retained
normal void function. The patient was followed up for more than 5
years and remained free of local recurrence and distant
metastasis.
Case 2
A 52-year-old female patient was admitted for a
gradually enlarging urethral mass with itching over the past 3
years. The patient developed acute urinary retention 10 days before
admission, therefore a 16-French urinary catheter was inserted in a
local hospital. The patient had undergone tubal lignations 20 years
earlier. Vaginal examination revealed a fixed hard mass measuring
approximately 3x2x3 cm beneath the anterior vaginal wall, without
tenderness and bleeding. Two enlarged lymph nodes 2.5 cm in
diameter were felt in the bilateral inguinal regions, which were
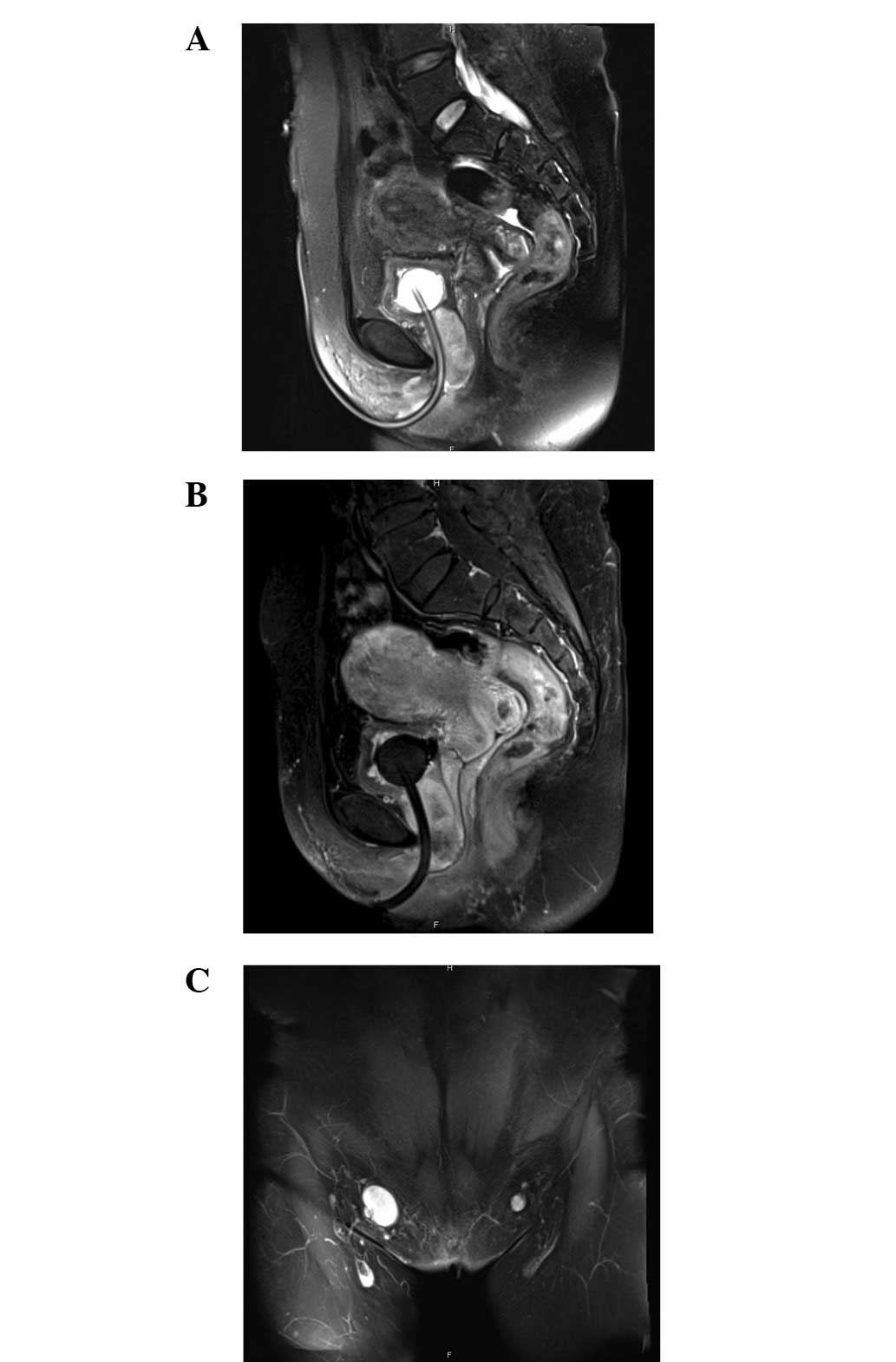
hard and mobilized but free of tenderness. Pelvic MRI with contrast
revealed a 5x2.9x3.6-cm tumor surrounding the urethra, with
slightly higher signal in T1- and T2-weighted images and uneven
enhancement after contrast administration (Fig. 3A and B). Enlarged lymph nodes with
even enhancement measuring approximately 1.8x2.6 cm were observed
in the bilateral inguinal region (Fig.
3C). The results of routine hematology studies and chemistry
blood tests were in the normal range. Tumor serum markers,
including carcinoembryonic antigen, α-fetoprotein and
prostate-specific antigen (PSA), were all in the normal range.
Cystourethroscopy revealed normal urethral and bladder mucous
membrane with some urethral hyperemia. Biopsy of the urethral
membrane revealed chronic inflammation of the urethra. A puncture
biopsy later revealed mucinous adenocarcinoma of the tissues
between the urethra and anterior vaginal wall with a possibility of
a metastatic lesion from the intestinal tract or ovaries. However,
the clinical data did not support the hypothesis that the lesion
was metastatic, as pelvic MRI revealed normal ovaries and
metastatic screening, including chest radiology, ultrasonography of
the abdomen and nuclide bone scan, and serum tumor markers were
unremarkable.
After careful preoperative preparation, the patient
underwent anterior pelvic exenteration, including anterior vaginal
wall, urethra, bladder and uterus, with pelvic and bilateral lymph
node dissection and ileum conduit. Postoperative pathology reported
moderately differentiated mucinous adenocarcinoma of the posterior
urethra, including bladder neck, internal urethral orifice and
external urethral orifice. The tumor had invaded the superficial
muscular layer of the anterior vaginal wall, but the vaginal mucosa
was not affected (Fig. 4).
Metastases were present in the right pelvic lymph nodes (1/3), left
inguinal lymph nodes (1/9) and the right inguinal lymph nodes
(2/9). The patient recovered gradually in 4 weeks and healed
satisfactorily. The patient was then transferred to the Department
of Oncology, Zhongshan Hospital, Xiamen University, Fujian, China,
and accepted two courses of chemotherapy regimen of gemcitabine
plus cisplatin. The patient was followed up for 12 months without
local recurrence or distant metastasis. Lymphedema in the left
lower extremity was present 2 months postoperatively and resolved
after medical management and using elastic socks. The ileum conduit
functioned well.
Discussion
Female urethral carcinoma is among the rarest types
of neoplasia of the genitourinary tract and corresponds to 0.003%
of all malignant neoplasias occurring in the female urogenital
tract (4). Although it was once
believed that urethral cancer was four times more common in females
than males, more recent literature suggests that primary urethral
cancer is nearly three times more common in males: a Surveillance,
Epidemiology and End Results (SEER) study reported an incidence of
4.3 per million in males and 1.5 per million in females (5).
In females, squamous cell carcinoma is the most
common histological type of urethral carcinoma, accounting for 70%
of all cases. Transitional cell carcinoma (20%) and adenocarcinomas
(8–10%) are the next most common cell types. Other rarer cell types
include lymphoma, neuroendocrine carcinoma, sarcomas,
paragangliomas, melanoma and metastasis (2).
Mucinous adenocarcinoma is most often composed of
colonic-type glandular epithelium and may contain abundant
extracellular mucin; it resembles mucinous carcinoma of the colon
and rectum, although it may occur at other sites, including the
pancreas, stomach, prostate and breast (6). Mucinous adenocarcinoma of the female
urethra is rare, with 25 cases reported in the English literature
(7–9) and one case report in the Japanese
literature (10).
Etiological factors associated with the development
of urethral carcinoma in females include leukoplakia, chronic
irritation, caruncles, polyps, parturition and human papillomavirus
infection or other viral infections. Female urethral diverticula
may also predispose the patient to malignant change and
adenocarcinoma accounts for more than 60% of female urethral
carcinomas arising within a diverticulum (11).
The origin of urethral adenocarcinomas remains
unclear. Certain authors have suggested that urethral
adenocarcinomas in females originate at the periurethral Skene’s
glands, which is a homolog of the prostate. PSA positivity is
considered to be evidence for an origin from the Skene’s glands
(12). Reis et al reported
that the macroscopic and microscopic examination of two
PSA-negative adenocarcinomas, including cytochemical and
immunohistochemical studies, favored an origin from Skene’s glands
due to similarities to findings in normal Skene’s glands (3,13).
Chan et al reported a case suggesting that mucinous urethral
adenocarcinoma may arise from the malignant transformation of
urethritis glandularis (13).
Most patients with urethral carcinoma are
symptomatic at presentation. A number of patients present with
obstructive symptoms, dysuria, urethral bleeding, urinary frequency
and often a palpable urethral mass or induration. A suspicion of a
urethral tumor should be raised in any otherwise healthy
middle-aged female without prior urological history who presents
with urinary retention. Patients may also present with a small
lesion prolapsing through the urethral meatus or with a small
submucosal lesion on the anterior wall of the vagina. Tumors spread
typically by local extension and may ulcerate as the tumor
progresses to the skin and vulvar region. Proximal lesions may
extend posteriorly into the vagina or proximally into the bladder.
Lymphatic spread is uncommon at early stages, but clinically
palpable nodes may be present in up to one-third of patients at
presentation and half of patients with advanced and proximal
tumors. Hematogenous spread may occur to the lung, liver, bone and
brain, in order of frequency (14).
The evaluation of females with suspected urethral
carcinoma includes cystourethroscopy, physical examination under
anesthesia, computed tomography of the abdomen and pelvis and chest
radiography. MRI has been used to evaluate pelvic lesions and may
aid the determination of local extension. MRI has been reported to
be accurate for evaluating local urethral tumors in 90% of
patients. Urethral tumors typically appear hypointense on
T1-weighted images and relatively hyperintense on T2-weighted
images. Tumor extent is best evaluated on sagittal T2-weighted
images. Tumors in the distal urethra may extend into the adjacent
perineum and the target-like appearance of the normal urethra on
axial T2-weighted images may be disrupted (15). CT may reveal a urethral mass with
soft-tissue attenuation (16).
Transvaginal ultrasonograpy may also provide clues for diagnosis.
Biopsy for suspected tumor is essential for establishing the
diagnosis. For the diagnosis of primary urethral mucinous
adenocarcinoma, exclusion of metastatic lesion originating from the
intestinal tract or ovaries is essential.
Due to the rarity of this type of tumor and
heterogeneity of the disease, most studies report similar prognoses
in different histological subtypes (17,18).
Certain studies have suggested that squamous cell carcinoma tends
to have a lower recurrence rate compared with adenocarcinoma and
transitional cell carcinoma, but the case series are too small to
have any statistical significance (17,18).
The prognosis is determined largely by the clinical stages and the
location of the lesions. Tumors in the distal urethra tend to have
a better outcome (3).
Options for treatment of female urethral carcinoma
include surgery, radiation therapy and chemotherapy, alone or in
combination. Treatment has tended toward a multimodality approach
in recent years. Local excision, which should lead to excellent
functional results, may be sufficient for the relatively uncommon
small, superficial, distal urethral tumors. Proximal female
urethral carcinomas are more likely to be high stage and may extend
into the bladder and vagina, as in the second case described in the
present study. For advanced female urethral cancer, a combination
of chemotherapy, radiation therapy and surgery has been recommended
for optimal local and distant disease control (19). Due to the high morbidity associated
with inguinal dissection and lack of improved survival, inguinal
dissection is not routinely performed and is only for patients who
present with positive inguinal or pelvic lymphadenopathy without
distant metastasis or those who develop regional lymphadenopathy
during surveillance (14).
Primary adenocarcinoma of female urethra is rare. A
biopsy is necessary for any suspicious urethral lesions. MRI is
recommended for tumor staging. Small, superficial, distal urethral
tumors may be treated with excision of the distal urethra. For
advanced female urethral cancer, a combination of chemotherapy,
radiation therapy and surgery is recommended for optimal local and
distant disease control. Regular follow-up is required in these
patients.
References
|
1.
|
V SrinivasSA KhanFemale urethral cancer -
an overviewInt Urol Nephrol19423427198710.1007/BF02550360
|
|
2.
|
I OuzaidJF HermieuS DominiqueP FernandezL
ChoudatV RaveryManagement of adenocarcinoma of the female urethra:
case report and brief reviewCan J Urol1754045407201020974039
|
|
3.
|
EL GheilerMV TefilliR TiguertJG de
OliveiraJE PontesDP Wood JrManagement of primary urethral
cancerUrology52487493199810.1016/S0090-4295(98)00199-X
|
|
4.
|
LO ReisA BillisFT FerreiraLY IkariRF
StelliniU FerreiraFemale urethral carcinoma: evidences to origin
from Skene’s glandsUrol Oncol29218223201119450996
|
|
5.
|
MA SwartzMP PorterDW LinNS WeissIncidence
of primary urethral carcinoma in the United
StatesUrology6811641168200610.1016/j.urology.2006.08.105717141838
|
|
6.
|
YB ChenJI EpsteinPrimary carcinoid tumors
of the urinary bladder and prostatic urethra: a clinicopathologic
study of 6 casesAm J Surg Pathol35442446201121317716
|
|
7.
|
C NeyHL MillerD OchsAdenocarcinoma in a
diverticulum of the female urethra: a case report of mucous
adenocarcinoma with a summary of the literatureJ
Urol10687487719714330018
|
|
8.
|
JM MeisAG AyalaDE JohnsonAdenocarcinoma of
the urethra in women. A clinicopathologic
studyCancer6010381052198710.1002/1097-0142(19870901)60:5%3C1038::AID-CNCR2820600519%3E3.0.CO;2-%233038294
|
|
9.
|
DP MurphyAJ PantuckPS AmentaFemale
urethral adenocarcinoma: immunohistochemical evidence of more than
1 tissue of originJ
Urol16118811884199910.1016/S0022-5347(05)68833-710332458
|
|
10.
|
H TanakaH MasudaY KomaiPrimary
adenocarcinoma of the female urethra treated by multimodal
therapyHinyokika Kiyo5543462009(In Japanese)
|
|
11.
|
Y AwakuraM NonomuraN ItohA MaenoT
FukuyamaAdenocarcinoma of the female urethral diverticulum treated
by multimodality therapyInt J
Urol10281283200310.1046/j.1442-2042.2003.00613.x12694472
|
|
12.
|
MK DodsonWA ClibyGL KeeneyMF PetersonKC
PodratzSkene’s gland adenocarcinoma with increased serum level of
prostate-specific antigenGynecol Oncol553043071994
|
|
13.
|
YM ChanD Ka-Leung ChengA Nga-Yin CheungH
Yuen-Sheung NganLC WongFemale urethral adenocarcinoma arising from
urethritis glandularisGynecol
Oncol79511514200010.1006/gyno.2000.596811104631
|
|
14.
|
RJ KarnesRH BreauDJ LightnerSurgery for
urethral cancerUrol Clin North
Am37445457201010.1016/j.ucl.2010.04.011
|
|
15.
|
S GourtsoyianniT HudolinE SalaD GoldmanBH
BochnerH HricakMRI at the completion of chemoradiotherapy can
accurately evaluate the extent of disease in women with advanced
urethral carcinoma undergoing anterior pelvic exenterationClin
Radiol6610721078201110.1016/j.crad.2011.07.039
|
|
16.
|
A KawashimaCM SandlerNF WassermanAJ
LeRoyBF King JrSM GoldmanImaging of urethral disease: a pictorial
reviewRadiographics24Suppl
1S195S216200410.1148/rg.24si04550415486241
|
|
17.
|
DS DimarcoCS DimarcoH ZinckeSurgical
treatment for local control of female urethral carcinomaUrol
Oncol22404409200410.1016/S1078-1439(03)00174-115464921
|
|
18.
|
CS FoensDH HusseyJJ StaplesJF DoornbosBC
WenAP VigliottiA comparison of the roles of surgery and radiation
therapy in the management of carcinoma of the female urethraInt J
Radiat Oncol Biol
Phys21961968199110.1016/0360-3016(91)90736-N1917626
|
|
19.
|
AJ KL WeinAC NovickAW PartinCA
PetersCampbell-Walsh Urology Vol 4 10th edition
SaundersElsevierPhiladelphia, PA2011
|