Introduction
Vertebral compression fractures (VCFs) are the most
common type of osteoporotic fracture (1) and affect over 200 million individuals
worldwide (2,3). Postmenopausal bone loss is one of the
leading causes of VCFs. However, a variety of primary malignant
conditions or secondary to non-skeletal primary neoplasms (multiple
myeloma, lymphoma and metastatic disease) may also be responsible.
Diagnosis of osteoporosis is based on clinical and radiological
imaging observations, including DEXA examination. However, these
processes often do not distinguish between neoplastic and
osteoporotic etiology (4).
In previous years, minimally invasive techniques,
including percutaneous vertebroplasty (PVP) and percutaneous
kyphoplasty (PKP), have been developed. PVP and PKP procedures have
been relatively effective in reducing fracture-related pain,
diminishing disability and accelerating complete recovery of
orthopedic injuries (5–8). Acquisition of a biopsy sample is
performed during PVP or PKP procedures. Biopsy samples are also
obtained from patients with normal laboratory reports. The outcome
of bone biopsies with unexpected malignancy in cases of vertebral
compression fracture treated with PVP or PKP have been previously
reported (9–12). The purpose of the present study was
to review the results of biopsies obtained during PVP or PKP.
Specifically, we aimed to determine the incidence of previously
undiagnosed malignancies in our own patient population. We also
wanted to determine the efficacy of obtaining biopsy during PVP or
PKP to estimate the effect of biopsy results on subsequent patient
care and management.
Patients and methods
Patients
Between January 2003 and December 2011, a total of
546 patients were treated with PVP or PKP at the Department of
Orthopedic Surgery of the First Affiliated Hospital of SooChow
University, Suzhou, China. This included 104 males (19%) and 442
females (81%), with a mean age of 75.3 years (range, 56–93 years).
In total, we treated 692 cases of VCFs. During PVP or PKP
procedures, 692 vertebral body biopsies were obtained; 427 level 1,
95 level 2, 21 level 3 and 3 level 4 biopsies were obtained in this
study. Biopsy levels included the following cases: T5 (3), T6 (8),
T7 (14), T8 (23), T9 (33), T10 (30), T11 (62), T12
(149), L1 (189), L2 (85), L3 (50), L4 (31) and L5 (15). Prior to surgery, 502 patients (92%)
had no history of malignancy and 44 patients (8%) had a history of
malignancy, which was considered to be the cause of their
compression fractures. The group of patients with known history of
malignancy was comprised of patients with carcinoma of the lung
(13), breast (7), multiple-myeloma (6), liver (5), bladder (4), prostate (4), pancreatic gland (2), chromatophoroma (2) and gastric cancer (1).
Obtainment of biopsies
During the PVP and PKP procedures, 122 and 570
biopsies were obtained, respectively. The patients were kept in the
prone position for every procedure. In all cases, the
transpedicular approach was used to access the collapsed vertebral
body. For this purpose, we used biplane fluoroscopy with two C-arms
statically placed in the posteroanterior and lateral positions. A
3-mm diameter trephine (Medtronic, Minneapolis, MN, USA) was passed
immediately into the vertebral body through the previously inserted
working cannula. The working cannula was inserted prior to infusion
of the biological cement or prior to insertion of the inflatable
bone tamp in the PVP and PKP procedures, respectively. Biopsies
were sent for pathological examination immediately following the
completion of the procedure and were fixed in 10% neutral-buffered
formalin. The decalcified biopsy material was embedded in paraffin,
sectioned and stained with hematoxylin and eosin. The stained
sections were examined by a pathologist under a light microscope.
If malignancy was identified, the biopsy was reviewed by a senior
pathologist.
The present study was approved by the institutional
review board (IRB) of The First Affiliated Hospital of SooChow
University, Suzhou, China and informed consent was obtained from
each patient or candidate.
Results
Following the surgical procedure, all patients
recovered from the VCF and reported rapid pain relief. Symptomatic
complications caused by PVP or PKP were not observed. All patient
charts were available for review and 89.9% of biopsies obtained
from 546 patients were suitable for histological evaluation. The
biopsy results of 448 patients were consistent with the diagnosis
of osteoporotic VCFs (OVCFs). In the majority of biopsy specimens,
trabecular bone with erratic levels of fibrosis and granulation
tissue reflected various stages of progressive fracture healing.
Among the 44 patients with an initial malignant condition,
malignancy was identified as the cause of compression fractures in
25 patients. In the remaining 19 patients with malignancy, the
suspected etiology behind the VCFs was not confirmed. In this case,
osteoporosis was identified in 16 patients, while the biopsies of
the remaining 3 patients were not suitable for pathological
examination. We observed 2 patients whose malignancy was not
suspected through pre-operative imaging or clinical symptoms. One
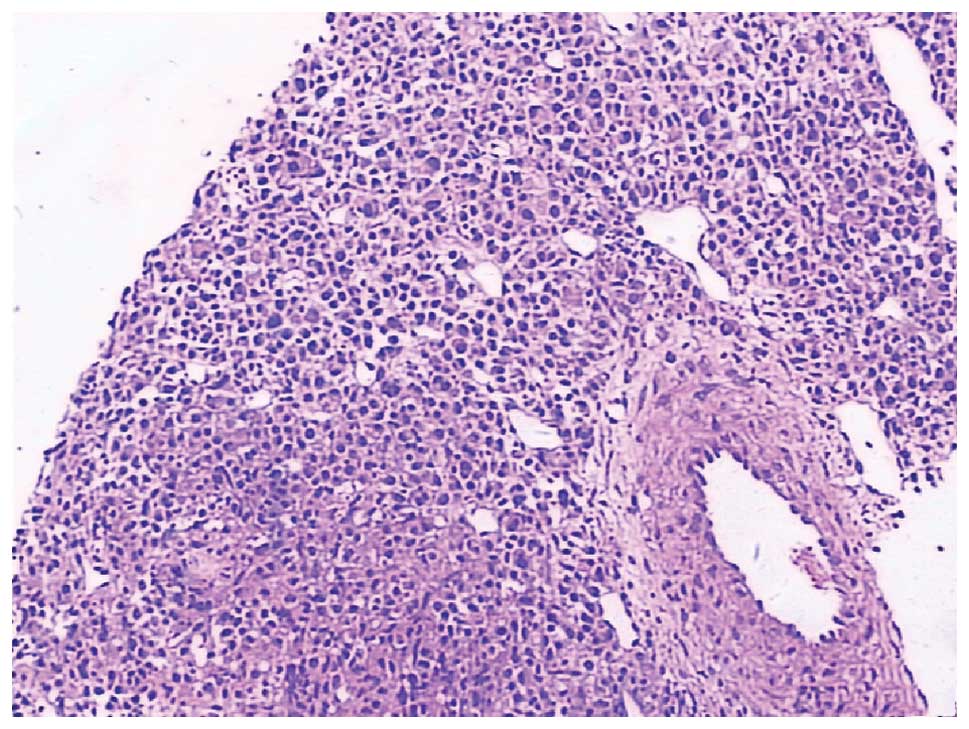
patient (male, 68 years old) suffered from multiple myeloma
(Fig. 1), while another patient
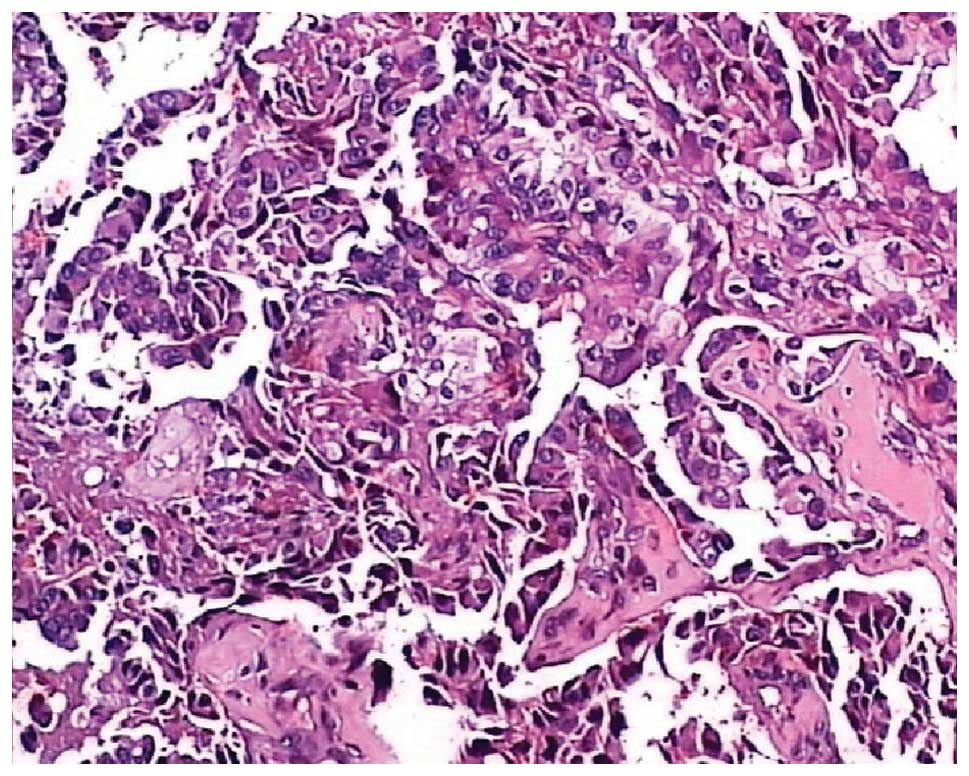
(female, 62 years old) suffered from metastatic carcinoma (Fig. 2). In the present study, the rate of
unsuspected malignancy was 0.4%. These two patients were
subsequently transferred to the oncology department for further
diagnostic tests and treatment.
Discussion
Prior to PVP or PKP procedures, diagnosis of OVCFs
was based on clinical and radiological observations, including
X-ray, CT, MRI, bone material density and ECT. However, in certain
cases these pre-operative investigations fail to provide correct
diagnosis of the condition (4,10,11).
It has been reported that the rate of distinguishing benign and
malignant compression fractures of the spine through MRI is between
55 and 94% (13–15). Therefore, patients with malignancy
require accurate pathological diagnosis to select the correct
program for further treatment of their condition. Following
administration of steroids, chemotherapeutic drugs or radiotherapy,
patients with lymphoma, multiple myeloma or metastatic carcinomas
are prone to VCFs owing to bone loss. In addition, the majority of
patients are elderly. However, osteoporosis is often assumed to be
the natural cause of VCFs and aging increases occurrence of OVCFs
(10). Malignancy and osteoporosis
was observed in the same patient. In the majority of cases,
osteoporosis is considered to be the correct assumption, however a
misdiagnosis may have a disastrous prognosis. The nature of the
underlying pathology associated with vertebral collapse is
important in correct prognosis. Moreover, it is also required for
assessing a patient’s response to therapy and long-term patient
care (10). The nature of the
underlying pathology associated with vertebral collapse is also
important for VCF patients with a medical history of malignancy,
wherein the primary tumor is not involved with the spine.
In the case of patients with a history of malignancy
or suspected malignancy, the outcomes of bone biopsies obtained
during PVP or PKP have been inconsistent, as the percentage of
malignancy diagnosis varies between 32.4 and 89% (16,17).
In the present study, 25 patients (56.8%) were diagnosed with
malignancy through biopsy samples obtained during PVP or PKP. These
patients had a history of malignancy or suspected malignancy and
were transferred to the oncology department for specialized
treatment. Medical history of malignancy was reported in 16
patients, however, their biopsy samples did not provide any
evidence of malignancy. Therefore, osteoporosis was the cause of
VCFs in these patients and the 16 patients underwent
anti-osteoporosis treatment.
There are instances where biopsy provides evidence
of malignancy when the patient has no clinical or imaging evidence
(9–12). Togawa et al(10) demonstrated that biopsy provided a
definitive diagnosis in one case of unsuspected multiple myeloma in
their population (0.7% of all biopsies). Muijs et
al(9) observed malignancy
evidence in the biopsies of 3 patients (3.8% of all biopsies),
whose malignancies were previously undiagnosed. This included 2
patients with multiple myeloma stage IIa and 1 patient with
chondrosarcoma grade I. These biopsy samples were obtained during
PVP, which were conducted to treat OVCFs in these patients. Shindle
et al(11) reported that
3/238 (1.3%) patients were diagnosed with unsuspected lymphoma
during PKP, through analysis of biopsy samples obtained during the
treatment. The authors obtained a total of 423 biopsy samples
during diagnosis of 238 patients. More recently, Schoenfeld et
al(12) reported that
malignancy was observed in 4 patients through analysis of biopsy
samples obtained during PVP or PKP. In this case, the malignancy
was detected in the previous diagnosis of 3 patients and 2 patients
(0.4%) were diagnosed with malignancy by biopsy during PKP. The
malignancy was not suspected in these cases, as these patients
revealed normal pre-operative imaging and did not exhibit any
clinical symptoms. In summary, vertebrae biopsy is highly
recommended in such cases and not only clarifies the nature of
disease but also contributes to treatment development in VCF
patients with a history of malignancy. For patients who do not
demonstrate clinical malignant evidence, vertebral biopsy is an
important method for confirmation of the malignancy diagnosis.
According to clinical and radiological observations
of VCFs, biopsy results were consistent with the diagnosis of OVCFs
in 398 patients included in the present study. In the majority of
biopsy specimens, trabecular bone with fibrosis and granulation
tissue reflected the various stages of progressive fracture
healing. Diamond et al(18)
characterized the histological process of fracture healing in
cancellous bone of vertebral body and divided this process into
four stages. Stage 1 included necrosis and granulation tissue;
stage 2 included chondrogenesis and bone matrix synthesis; stage 3
included endochondral ossification and woven bone formation; and
stage 4 included bone remodeling and modeling. The present findings
revealed that the majority of fractures were early stage and may be
attributed to the early procedure time and biopsy sample size.
The posterolateral approach is normally used for
obtaining biopsy under fluoroscopic or CT guidance in cases of
thoracic or lumbar spine (19–21).
However, the risk correlated with this process varies from 0 to 26%
and is associated with various complications, including
pneumothorax, hematoma, neurological lesions, root pain and
infective disorders. Posterolateral biopsy is also correlated with
the risk of tumor metastasis by needle sheath in malignancy
(22). In order to avoid these
complications, the biopsy was previously performed using a
transpedicular approach under CT or fluoroscopic guidance (22,23).
During PVP or PKP in the present study, a cannulated trocar was
inserted into the vertebral body through a transpedicular approach.
Following removal of the guide wire, a trephine was used to obtain
the biopsy sample of the vertebral body. The procedures provided a
definite path to acquire a biopsy sample and did not significantly
increase surgical time. In the case of malignant patients with
VCFs, we completed the diagnosis and surgery during PKP or PVP.
During PVP or PKP procedures, the time and frequency
of biopsy material acquisition remains debated. Togawa et al
and Schoenfeld et al(10,12)
advise that biopsy should be performed while conducting the first
vertebral augmentation procedure. However, Allen et
al(24) suggested that patients
undergoing first-time vertebral augmentation should be considered
for vertebral biopsy. The present study and additional studies
(4,10,12)
have confirmed malignant biopsy results in patients, who did not
exhibit any other clinical malignant evidence. However, the rate of
detection was low in such cases. Moreover, a biopsy obtained during
PVP or PKP does not increase morbidity in the patients and the
biopsy aids identification of the underlying pathology. Early
detection of malignant disease is more important than the risks
associated with biopsy as effective timely treatment for malignancy
is unlikely to be provided to patients who do not recieve early
diagnosis through this process. Considering the potential
advantages of biopsy during PVP or PKP, we suggest that biopsy of
every collapsed vertebra should be performed during every procedure
of PVP or PKP, even in patients with no history of malignancy or
suspected malignancy.
Previously, a meta-analysis of percutaneous spine
biopsy demonstrated that the rates of adequacy (92.6 vs. 90.1%) and
accuracy (90.2 vs. 88.1%) were slightly higher than those of
fluoroscopy. However, these increases were not significant
(25). A previous study reported
that diagnostic accuracy of percutaneous spine biopsy is more than
90% in cases of known or suspected malignancy (26). Therefore, researchers must focus on
improving the efficiency of needle aspiration biopsy to obtain
sufficient pathological cells. Kattapuram et al(27) reported that the accuracy achieved by
large needles was slightly higher than that of fine. It has been
suggested that needles with a diameter of at least 2 mm are
suitable for obtaining samples sufficient for histological
evaluation (20,28,29).
Ward et al(29) demonstrated
that 3.5 mm trephine were suitable for obtaining samples. Larger
diameter needles were more suitable for obtaining adequate bone
cores for histological evaluation. However, during PVP or PKP, the
diameter of biopsy needles is limited by the working cannula. The
biopsy and infusion of bone cement are performed under cannula,
which is first inserted into the pedicle. Therefore, the biopsy
procedure is not associated with the risks of inflicting injuries
to vital tissues, including major vessels and nerve roots of spinal
cord. While obtaining patient biopsies during PKP or PVP, we did
not observe any complications. Therefore, we recommend using biopsy
needles with maximal diameter in order to obtain more bone cores.
In the present study, a biopsy needle with a diameter of 3 mm was
utilized safely and effectively during the PVP or PKP
procedures.
In conclusion, PVP and PKP are effective treatments
for VCFs. If biopsy samples are obtained while performing these
procedures, no increase in morbidity or surgical duration is
observed. Biopsy aids identification of the underlying pathology.
In the present study, the rate of unsuspected malignance was 0.4%.
Obtaining a biopsy sample is relatively safe and easy, therefore we
recommend collapsed vertebral body biopsy during every PVP or PKP
procedure. In addition we recommend using a biopsy needle of
maximal diameter for under cannula. For effective VCF management,
it is important to obtain a biopsy sample during PVP or PKP
procedure.
References
|
1
|
Ross PD: Clinical consequences of
vertebral fractures. Am J Med. 103:30S–42S. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Garfin SR, Buckley RA and Ledlie J;
Balloon Kyphoplasty Outcomes Group: Balloon kyphoplasty for
symptomatic vertebral body compression fractures results in rapid,
significant and sustained improvements in back pain, function and
quality of life for elderly patients. Spine (Phila Pa 1976).
31:2213–2220. 2006. View Article : Google Scholar
|
|
3
|
van Schoor N, Smit J, Twisk JW and Lips P:
Impact of vertebral deformities, osteoarthritis and other chronic
diseases on quality of life: a population based study. Osteoporos
Int. 16:749–756. 2005.PubMed/NCBI
|
|
4
|
Ho CS, Choi WM, Chen CY, Chen WY and Chan
WP: Metastasis in vertebra mimicking acute compression fractures in
a patient with osteoporosis: MRI findings. Clin Imaging. 29:64–67.
2005.PubMed/NCBI
|
|
5
|
Ledlie JT and Renfro M: Balloon
kyphoplasty: one year outcomes in vertebral body height
restoration, chronic pain and activitiy levels. J Neurosurg.
98:36–42. 2003.PubMed/NCBI
|
|
6
|
Crandall D, Slaughter D, Hankins PJ, Moore
C and Jerman J: Acute versus chronic vertebral compression
fractures treated with kyphoplasty: early results. Spine J.
4:418–24. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Evans AJ, Jensen ME, Kip KE, et al:
Vertebral compression fractures: pain reduction and improvement in
functional mobility after percutaneous polymethylmethacrylate
vertebroplasty retrospective report of 245 cases. Radiology.
226:366–372. 2003. View Article : Google Scholar
|
|
8
|
Mathis JM, Ortiz AO and Zoarski GH:
Vertebroplasty versus kyphoplasty: a comparison and contrast. AJNR
Am J Neuroradiol. 25:840–845. 2004.PubMed/NCBI
|
|
9
|
Muijs SP, Akkermans PA, van Erkel AR and
Dijkstra SD: The value of routinely performing a bone biopsy during
percutaneous vertebroplasty in treatment of osteoporotic vertebral
compression fractures. Spine (Phila Pa 1976). 34:2395–2399. 2009.
View Article : Google Scholar
|
|
10
|
Togawa D, Lieberman IH, Bauer TW,
Reinhradt MK and Kayanja MM: Histological evaluation of biopsies
obtained from vertebral compression fractures: unsuspected myeloma
and osteomalacia. Spine (Phila Pa 1976). 30:781–786. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shindle MK, Tyler W, Edobor-Osula F,
Gradner MJ, Shindle L, Toro J and Lane JM: Unsuspected lymphoma
diagnosed with use of biopsy during kyphoplasty. J Bone Joint Surg
Am. 88:2721–2724. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Schoenfeld AJ, Dinicola NJ, Ehrler DM, et
al: Retrospective review of biopsy results following percutaneous
fixation of vertebral compression fractures. Injury. 39:327–333.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
An HS, Andreshak TG, Nguyen C, Williams A
and Daniels D: Can we distinguish between benign versus malignant
compression fractures of the spine by magnetic resonance imaging?
Spine (Phila Pa 1976). 20:1776–1782. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Rupp RE, Ebraheim NA and Coombs RJ:
Magnetic resonance imaging differentiation of compression spine
fractures or vertebral lesions caused by osteoporosis or tumor.
Spine (Phila Pa 1976). 20:2499–2504. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Moulopoulos LA, Yoshimitsu K, Johnston D,
Leeds NE and Libshitz HI: MR prediction of benign and malignant
vertebral compression fractures. J Magn Reson Imaging. 4:667–674.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Minart D, Vallee JN, Cormier E and Chiras
J: Percutaneous coaxial transpedicular biopsy of vertebral body
lesions during vertebroplasty. Neuroradiology. 43:409–412. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Erie L, Mark HB, Leszek P, et al:
Percutaneous CT-guided biopsy of osseous lesion of the spine in
patients with known or suspected malignancy. AJNR Am J Neuroradiol.
25:1583–1588. 2004.PubMed/NCBI
|
|
18
|
Diamond TH, Clark WA and Kumar SV:
Histomorphometric analysis of fracture healing cascade in acute
osteoporotic vertebral body fractures. Bone. 40:775–780. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bender CE, Berquist TH and Wold LE:
Imaging-assisted percutaneous biopsy of the thoracic spine. Mayo
Clin Proc. 61:942–950. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Fyfe IS, Henry AP and Mulholland RC:
Closed vertebral biopsy. J Bone Joint Surg Br. 65:140–143.
1983.
|
|
21
|
Laredo JD and Bard M: Thoracic spine:
percutaneous trephine biopsy. Radiology. 160:485–489. 1986.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Jelinek JS, Kransdorf MJ, Gray R,
Aboulafia AJ and Malawer MM: Percutaneous transpedicular biopsy of
vertebral body lesions. Spine (Phila Pa 1976). 21:2035–2040. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Pierot L and Boulin A: Percutaneous biopsy
of the thoracic and lumbar spine: transpedicular approach under
fluoroscopic guidance. AJNR Am J Neuroradiol. 20:23–25.
1999.PubMed/NCBI
|
|
24
|
Allen RT, Kum JB, Weidner N, Hulst JB and
Garfin SR: Biopsy of osteoporotic vertebral compression fractures
during kyphoplasty: unsuspected histologic findings of chronic
osteitis without clinical evidence of osteomyelitis. Spine (Phila
Pa 1976). 34:1486–1491. 2009. View Article : Google Scholar
|
|
25
|
Nourbakhsh A, Grady JJ and Garges KJ:
Percutaneous spine biopsy: a meta-analysis. J Bone Joint Surg Am.
90:1722–1725. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lis E, Bilsky MH, Pisinski L, Boland P,
Healy JH, O’malley B and Krol G: Percutaneous CT-guided biopsy of
osseous lesion of the spine in patients with known or suspected
malignancy. AJNR Am J Neuroradiol. 25:1583–1588. 2004.PubMed/NCBI
|
|
27
|
Kattapuram SV, Khurana JS and Rosenthal
DI: Percutaneous needle biopsy of the spine. Spine (Phila Pa 1976).
17:561–564. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Akerman M, Berg NO and Persson BM: Fine
needle aspiration biopsy in the evaluation of tumor-like lesions of
bone. Acta Orthop Scand. 47:129–136. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ward JC, Jeanneret B, Oehlsehlegel C and
Magerl F: The value of percutaneous transpedicular vertebral bone
biopsies for histologic examination. Results of an experimental
histopathologic study comparing two biopsy needles. Spine (Phila Pa
1976). 21:2484–2490. 1996. View Article : Google Scholar
|