Introduction
Ganglioneuromas (GNs) are typically rare benign
tumors primarily arising from the central or peripheral autonomic
nervous system, particularly the sympathetic system. The most
affected anatomical sites are the posterior mediastinum,
retroperitoneum, adrenal gland and soft tissue of the head and
neck.
GNs rarely differentiate into malignant and
metastasic disease (1) and
differentiation into malignant peripheral nerve sheath tumors
(MPNST) is extremely rare and scarcely reported. To date, there are
less than 20 reported cases of MPNST worldwide in the
English-language literature (2).
MPNST is most frequently observed in adult life, and is slightly
more common in males compared with females.
The diagnosis of MPNST is difficult. Surgical
resection is the primary treatment of MPNST, which is usually
followed by a poor outcome. MPNST occurs most frequently in the
head and neck or the upper extremities and only 1% of cases have
been identified in the retroperitoneum (3). The clinical features of MPNST,
including the symptoms, diagnosis, pathway of malignancy
transformation and characteristics of metastasis, are largely
unknown and remain to be investigated. In the current study, we
present a case of a huge MPNST with hepatic metastasis originating
from retroperitoneal GN in a 43-year-old male, which was initially
diagnosed as hepatocellular carcinoma due to the tumor’s location
and unusual blood supply. The study was approved by the Ethics
Committee of China-Japan Union Hospital of Jilin University,
Changchun, China. Written informed consent was obtained from the
patient.
Case report
A 43-year-old man was admitted to The Third Hospital
(China-Japan Union Hospital) of Jilin University (Changchun, China)
due to complaints of upper abdominal pain. No other symptoms,
including fever, jaundice and weight loss, were noted, but
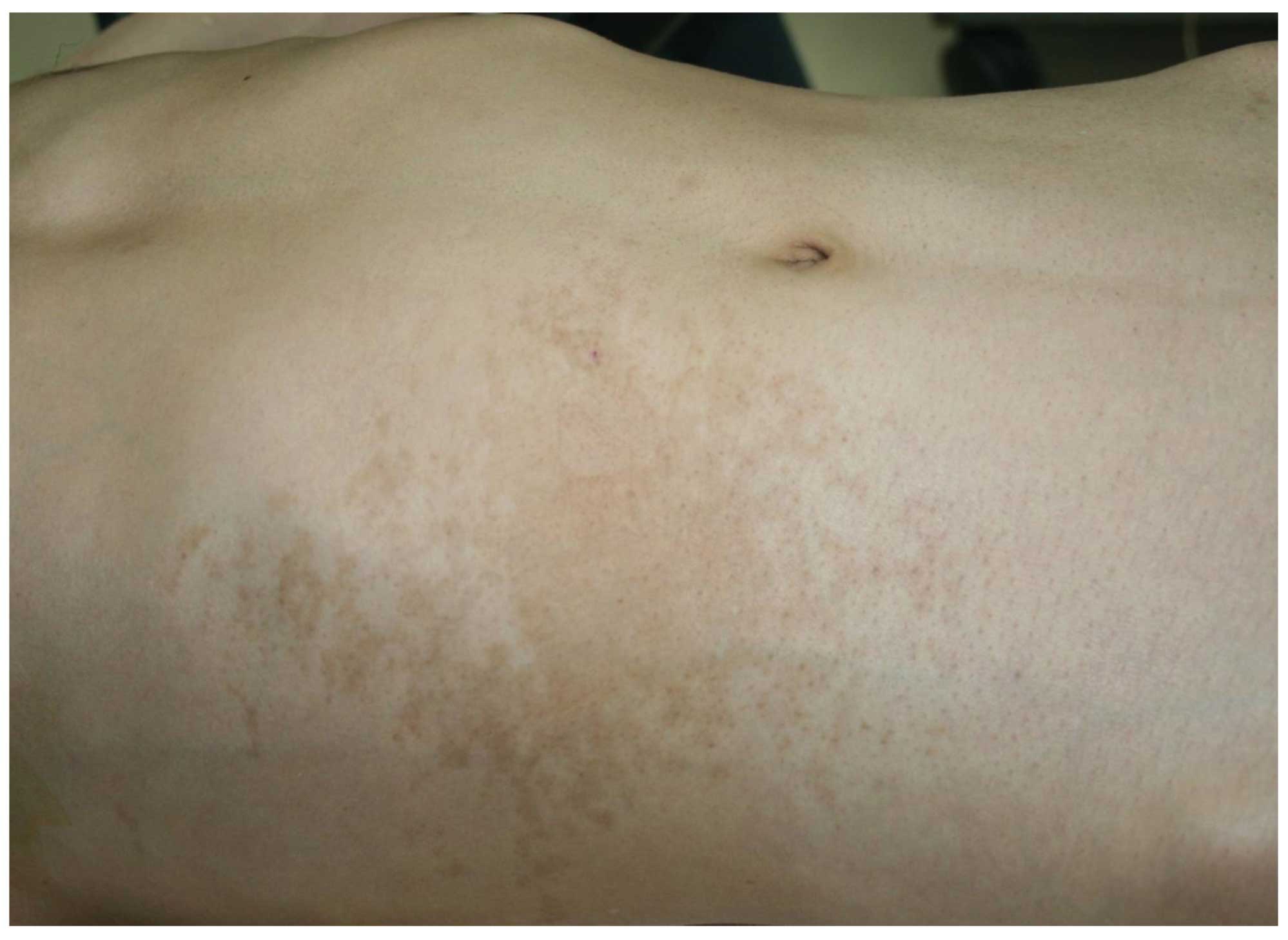
scattered brown pigments were observed on the right hypochondriac
region of the abdomen (Fig. 1).
Ultrasonography identified a giant ‘hepatic neoplasm’ ∼25×15×15 cm
in size that occupied the patient’s right liver lobe and contained
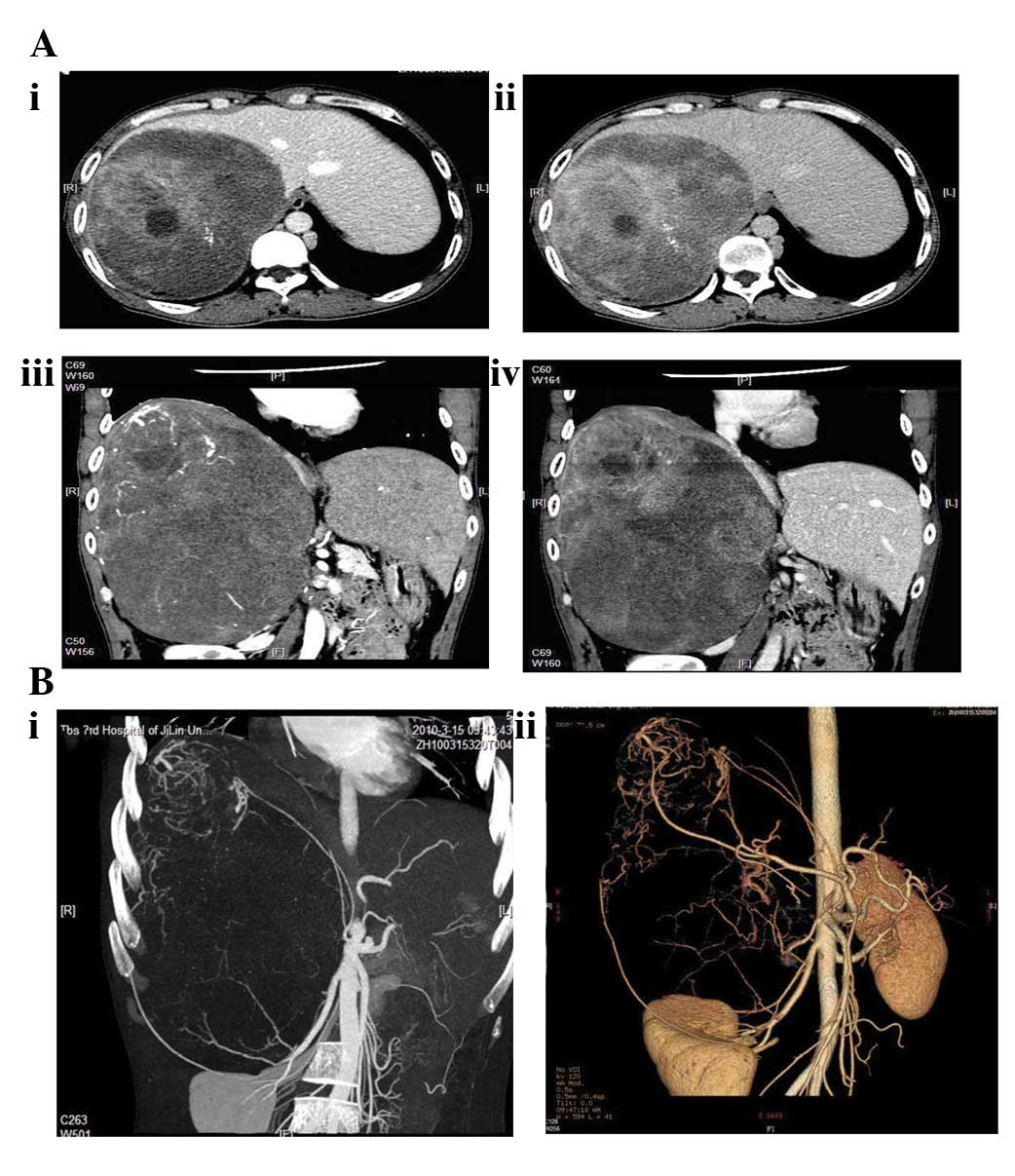
cystic and solid components. A contrast-enhanced computed
tomography (CT) scan revealed a huge non-homogeneous, oblong shaped
and relatively well-defined expansive mass occupying the right
posterior liver lobes. It was enhanced in arterial phases and
particularly enhanced in portal venous phases, but the inferior
hepatic vena cava was not clearly presented (Fig. 2A). The 3D CT vessel reconstruction
demonstrated that the majority of the tumor was nourished by the
renal artery and another vessel branching from the abdominal aorta,
while the top part of the tumor (4 cm in diameter) was nourished by
the right hepatic artery (Fig. 2B).
The serum tumor markers for α-fetoprotein (AFP), carcinoembryonic
antigen (CEA) and carbohydrate antigen 19-9 (CA19-9) were within
the normal ranges. Fine needle aspiration on the tumor revealed
spindle shaped cells and a few gangliocytes without any evidence of
malignancy, indicating that the tumor may be derived from
retroperitoneal neural crest cells.
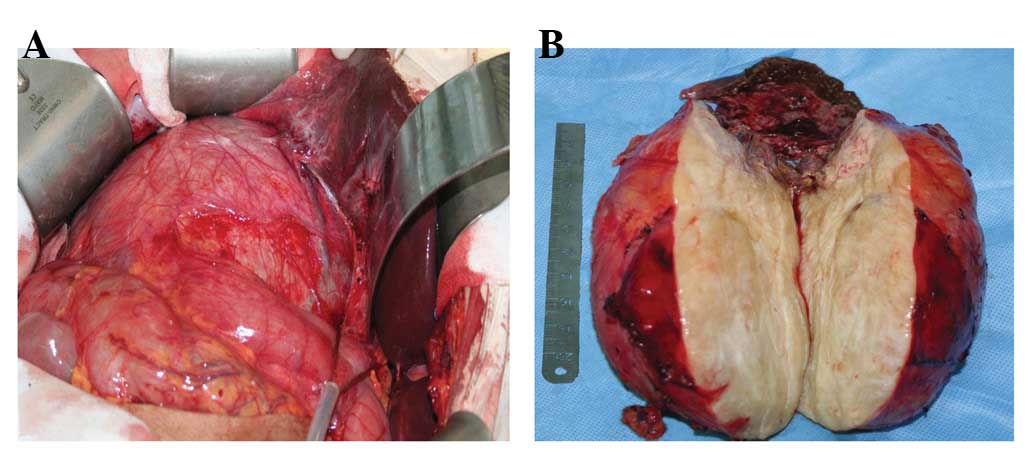
An exploratory laparotomy was conducted, which
demonstrated that the tumor originated from the retroperitoneal
area of the abdominal cavity. It squeezed and compressed the right
liver lobe (Fig. 3A) and a 1-cm
metastatic nodule was observed in the compressed right liver lobe
close to the tumor, which was separated with MPNST. The MPNST had a
loose adhesion to adjacent retroperitoneal tissues and was resected
completely with the partial right hepatic lobe (Fig. 3B).
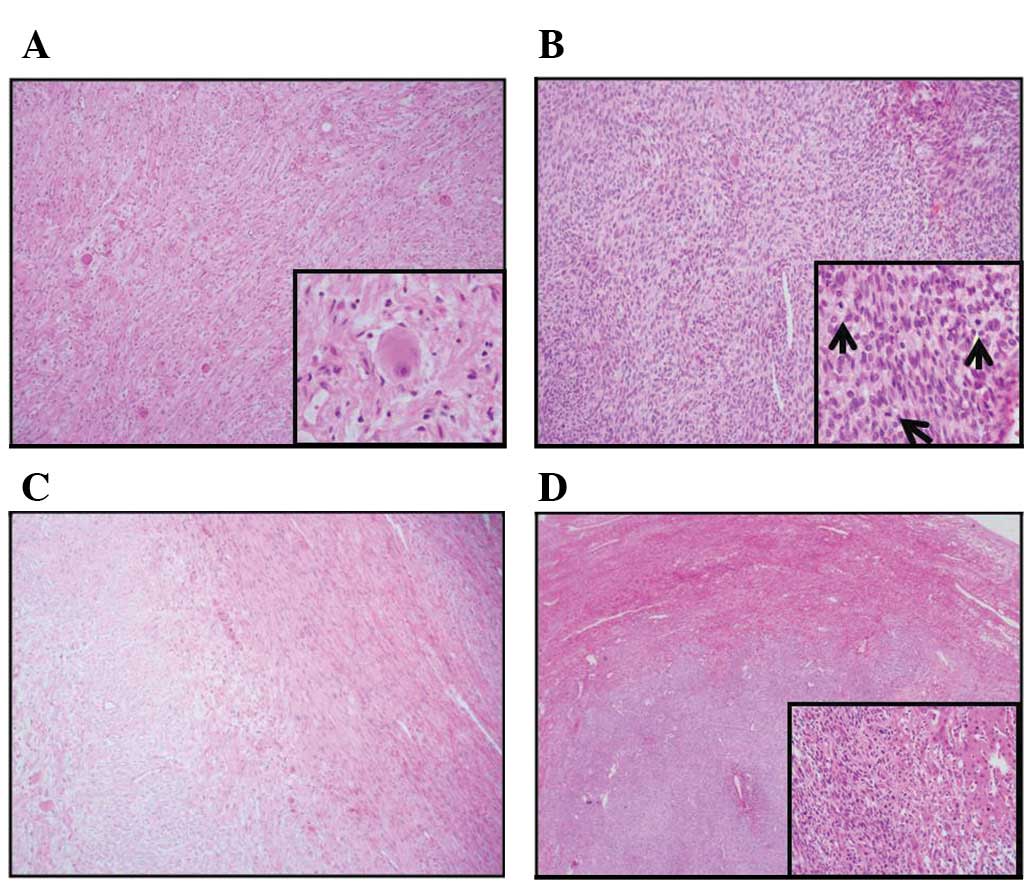
Histological examination revealed a GN malignant
transformation in which the tumor was composed of GN and MPNST.
There was a line of demarcation between the two components. The GN
region consisted of sparse spindle cells with scattered mature
ganglioneurocytes (Fig. 4A). In
addition, hyperchromatic spindle or short spindle cells intensively
ranged in the malignancy demonstrating a fasciculated growth
pattern in which 2–4 mitotic figures per high power field (hpf)
were observed. Hemorrhage and necrosis in the malignant area were
compatible with the hypodensity of the image (Fig. 4B). There was a distinct boundary
between the benign and malignant regions (Fig. 4C) and malignant tumor cells were
detected in the metastasized liver tissue (Fig. 4D).
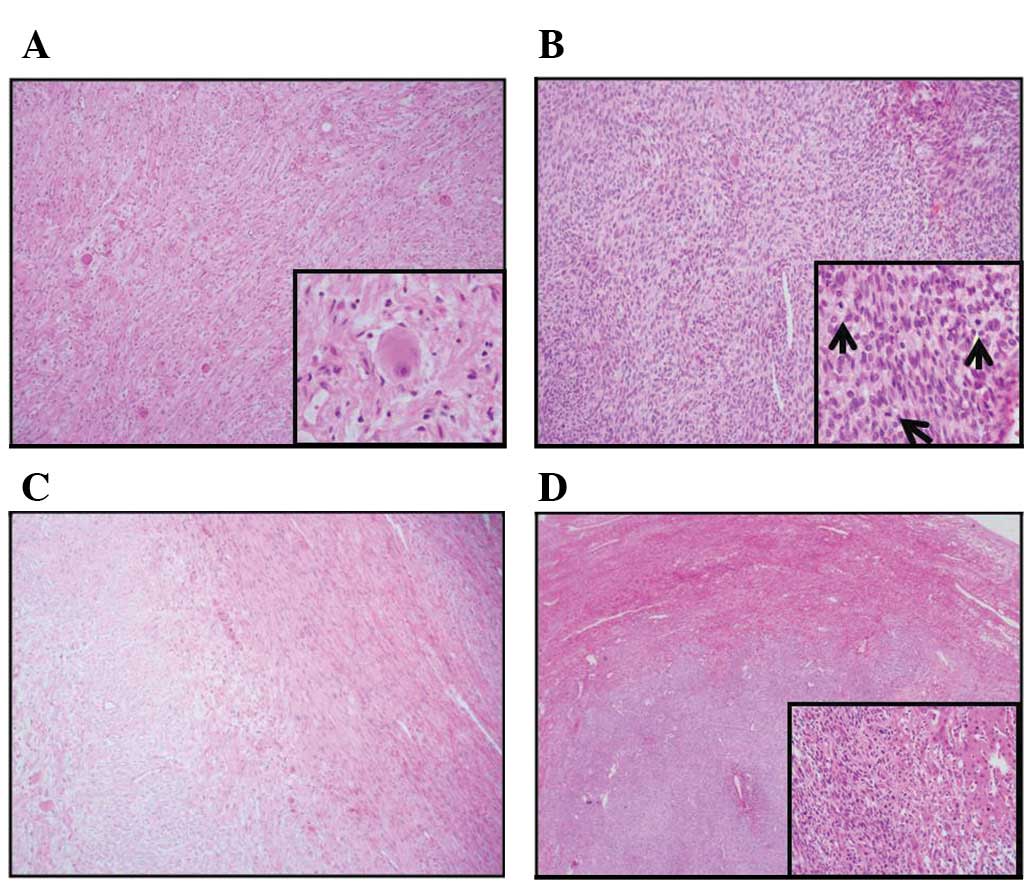 | Figure 4(A) The GN region consisted of sparse
spindle cells scattered with mature gangliocytes (magnification,
×200); insert showing an enlarged morphology of gangliocytes
(magnification, ×400). (B) Intensively arranged spindle cells with
mitotic figures (magnification, ×200); insert showing 2–4 mitotic
cells per hpf, as indicated by arrows (magnification, ×400). (C)
There was a distinct boundary between benign and malignant regions.
(magnification, ×200) (D) Liver membrane nodule of the right lobe
showing the liver metastasis (magnification, ×40); insert showing
malignant cells in the hepatic parenchyma (magnification, ×400).
GN, ganglioneuroma; hpf, high power field. |
Immunohistochemical staining revealed that the cells
of the GN stained positive for S100 protein and syn, and the MIB-1
proliferative index (labeled with immunohistochemical stain for the
Ki67 antigen) was <1%. In malignant tissue, CD56, GFAP, CD117,
CD34, BCL-2 and P53 were stained positive, while S100, SMA and
actin were stained negative. The MIB-1 proliferative index was
>40%.
The postoperative course was uneventful and no
additional therapy was administered. Since the procedure, the
patient has been followed up closely and has been recurrence free
for 4 months.
Discussion
GN is a rare, benign tumor arising from the neural
crest cells. It is composited with ganglion cells, Schwann cells
and a few neuroblasts. GN is most commonly located in the posterior
mediastinum followed by the retroperitoneum, and is most frequently
diagnosed between the ages of 10 and 40 years (4). Despite its extremely rare incidence,
malignant transformations may occur and the neoplasm may exist in
the form of an MPNST (5). The
majority of GNs manifest as an asymptomatic mass, which are
discovered on routine radiographic studies for other lesions. The
present case was symptomatically associated with pain of the
abdomen and metastasis to the liver. Using contrast-enhanced CT, we
have demonstrated that multiple blood supplies from the abdominal
aorta, renal artery and hepatic artery may be the cause of quick
tumor progression, malignant transformation and abdominal symptoms
of the tumor.
MPNST is rare, with an expected incidence of 0.001%
(6). It has been suggested that the
disease occurrence is usually associated with radiation or
neurofibromatosis type 1 (NF-1). However, how much of those factors
contribute to the occurrence of MPNST and whether the ethnicity and
region are involved are unknown. Li et al and Ye et
al reported that a few patients had a history of radiotherapy
or neurofibromatosis (7,8). Coffin and Dehner (9) have reported that retroperitoneal
malignant schwannoma in the absence of NF-1 is extremely rare. The
definite correlation of the regional diversity in the incidence of
MPNST remains uncertain. The present case has no evidence of NF-1
or radiation history, but regional skin brown pigmentation was
identified on the right hypochondric region of the abdomen. Over
the years, a universal notion has developed which suggests that GN
patients with NF-1 have a greater lifetime risk of developing MPNST
and tend to have a worse prognosis. de Chadarevian et
al(2) reviewed 12 fully
documented MPNST patients arising from GN of 139 MPNST cases.
Similar to the presentation of our patient, none of the cases had
NF, indicating that other factors may involved.
Our histological examination revealed that the tumor
included two distinct components: benign loose texture areas and
malignant compact texture areas with necrosis and hemorrhage. The
majority of the middle to bottom area of the tumor consisted of
benign, well-differentiated spindle cells with scattered mature
ganglion cells, while the malignant region located at the top part
of the tumor extruded into the hepatic parenchyma. The lesion
detected in the liver had its own boundary and ganglion cells were
revealed inside. Based on these histological results, the tumor was
composed of approximately 75% GN and 25% MPNST. Abrupt transition
of the two different components was observed. We concluded that
MPNST arose from the transformation of GN since ganglion cells were
identified in the malignant area. However, this does not preclude
the conceptual possibility that any type of nerve sheath cells are
able to turn into malignant neoplasms. Therefore, possible
initiators are either Schwann cells recruited by the GN or one of
the integral neoplastic constituents of the benign GN. Studies on
how MPNST may be derived from GN are required (10) as only limited data are available
regarding the research of this transformation.
MPNST is usually asymptomatic, however, symptoms may
occur in certain cases depending on the location of the tumor and
whether the hormones are being secreted or not. MPNSTs have few
laboratory characteristics and morphological features, making the
preoperative diagnosis difficult. In almost all cases, the
diagnosis depends on the pathology and immunohistochemistry
examinations. In our patient, there was an important physical sign
of abdominal café au lait macules (CALMs), which was nearly
overlooked. CALM belongs to the definition of neurocutaneous
syndrome. Skin lesions may occur sporadically in the general
population and are nearly universal findings in patients with NF-1.
However, there have been no publications reporting objective
quantification of CALM pigmentation (11).
Arteriography and 3D CT vascular reconstruction may
be useful to visualize the vascularization. Manifesting the artery
blood supply is generally the most reliable method for ruling out
the origin of the tumors. In our patient, the nutritious blood
originated from multiple arteries involving the branches of the
renal artery, right hepatic artery and abdominal aorta. The fact
that the blood supply by hepatic vessels to the top part of the
tumor may be a result from hepatic invasion, confirms the vascular
connection between the liver and the tumor. Rapid proliferation of
malignant cells usually occurs in a relatively ischemic situation,
which leads to the compensation of blood supply from the liver.
This phenomenon is pathophysiologically reasonable; however, there
are no previous studies on uncommon blood supplies in MPNST cases.
This has made it difficult to differentiate the tumor from HCC
until surgery.
The prognosis of MPNST has been poorly reported. Our
patient received a complete surgical excision and was recurrence
free for only 4 months. MPNST is not sensitive to radiation or
chemotherapy, so there are no effective therapeutic methods to be
used postoperatively (12). In the
perspective of our case and accumulated reports of GN malignant
transformations to MPNST, although extremely rare, further
systematic investigations are feasible and important to elucidate
the mechanisms of GN and MPNST.
References
|
1
|
Jung HR, Kang KJ, Kwon JH and Kang YN:
Adrenal ganglioneuroma with hepatic metastasis. J Korean Surg Soc.
80:297–300. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
de Chadarevian JP, Maepascasio J, Halligan
GE, Katz DA, Locono JA, Kimmel S and Katsetos CD: Malignant
peripheral nerve sheath tumor arising from an adrenal
ganglioneuroma in a 6-year-old boy. Pediatr Dev Pathol. 7:277–284.
2004.PubMed/NCBI
|
|
3
|
Okada K, Hasegawa T, Tajino T, et al:
Clinical relevance of pathological grades of malignant peripheral
nerve sheath tumor: a multi-institution TMTS study of 56 cases in
Northern Japan. Ann Surg Oncol. 14:597–604. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gary C, Robertson H, Ruiz B, Zuzukin V and
Walvekar RR: Retropharyngeal ganglioneuroma presenting with neck
stiffness: report of a case and review of literature. Skull Base.
20:371–374. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Acin-Gandara D, Carabias A, Bertomeu A,
Gimenez-Alvira L, Colao L and Limones M: Giant retroperitoneal
ganglioneuroma. Rev Esp Enferm Dig. 102:205–207. 2010.(In
Spanish).
|
|
6
|
Chhabra A, Soldatos T, Durand DJ, Carrino
JA, McCarthy EF and Belzberg AJ: The role of magnetic resonance
imaging in the diagnostic evaluation of malignant peripheral nerve
sheath tumors. Indian J Cancer. 48:328–334. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Li C, Shi Y, Luo H and Wang J: Giant
retroperitoneal malignant schwannoma: a case report and review of
literature. Chinese-German J Clinical Oncol. 9:180–182. 2010.
View Article : Google Scholar
|
|
8
|
Ye TS, Zhang XF, Wang Y, et al: Clinical
research of malignant peripheral nerve sheath tumor (36 cases
report). Med J Chin PLA. 8:717–718. 2003.(In Chinese).
|
|
9
|
Coffin CM and Dehner LP: Peripheral
neurogenic tumors of the soft tissues in children and adolescents:
a clinicopathologic study of 139 cases. Pediatr Pathol. 9:387–407.
1989. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mora J, Cheung NK, Juan G, et al:
Neuroblastic and Schwannian stromal cells of neuroblastoma are
derived from a tumoral progenitor cell. Cancer Res. 61:6892–6898.
2001.
|
|
11
|
Boyd KP, Gao L, Feng R, Beasley M,
Messiaen L, Korf BR and Theos A: Phenotypic variability among
café-au-lait macules in NF-1. J American Acad Dermatol. 63:440–447.
2010.PubMed/NCBI
|
|
12
|
Anghileri M, Miceli R, Fiore M, Mariani L,
Ferrari A, Mussi C, Lozza L, Collini P, Olmi P, Casali PG, Pilotti
S and Gronchi A: Malignant peripheral nerve sheath tumors:
prognostic factors and survival in a series of patients treated at
a single institution. Cancer. 107:1065–1074. 2006. View Article : Google Scholar : PubMed/NCBI
|