Introduction
Appendiceal cystadenoma has unique clinical
characteristics. It is a rare disease, accounting for 0.6% of
appendectomy specimens (1), with an
appendiceal carcinoid detection rate of 0.3–0.5%. A quarter of
patients have no significant clinical manifestations (2). Appendiceal mucocele (AM) and
appendiceal cystadenoma are distinct entities; the former is not a
specific diagnosis, but a descriptive term for the dilation of the
lumen of the vermiform appendix by an abnormal accumulation of
mucous. These histopathologic lesions and mucoceles are defined as
three types. One type is appendiceal cystadenoma. This is difficult
to clinically identify and a surgical pathological diagnosis is
required. The nosogenesis, pathology, biological activity, disease
evolution, treatment points and prognosis (3) are different for each case. Due to the
pressure retention and atypical cells, an appendix cystadenoma is
often deformed and flat, resulting in a missed diagnosis.
Pathologists are more likely to lean toward a diagnosis of
appendiceal cystadenoma as opposed to appendiceal cyst. The
appendiceal mucosa originates from the colon epithelium, so the
lower gastrointestinal tract is vulnerable to the impact of the
same tumor. It is reported that 20% of appendiceal cystadenomas are
accompanied by a synchronous or metachronous colon tumor (5). Appendiceal cystadenoma is the required
accurate preoperative diagnosis needed to prevent intraoperative
rupture and predict malignant transformation (1,6)
Appendix cystadenoma patients all have a different length of
hospitalization, quality of life and prognosis due to the different
timings of medical intervention and whether the cystadenoma is
removed in its entirety. It’s prognosis as appendicitis requires a
timely and complete resection, otherwise it will relapse into
cystadenocarcinoma (4). Another
possibility is a spontaneous rupture or an intraoperative rupture
resulting in secondary pseudomyxoma peritonei (PMP), which has a
clinical surgical detection rate of only 2/10,000 and a poorer
prognosis (2). As a result, the
prognosis of appendiceal cystadenoma relies upon the speed of
treatment. This report of three cases of appendiceal cystadenoma
seriously considers the timing of clinical intervention and the
prognosis, as experienced in the primary hospital. This study was
approved by the ethics committee of Beilun District People’s
Hospital, the First Affiliated Hospital, Beilun Branch of Zhejiang
University, Ningbo, China.
Case report
Case 1
A 79-year-old man with no notable medical or
surgical history presented with a four-day-long history of
distending pain in the right side of the abdomen. There was no
palpable mass and no guarding or rebound tenderness was observed.
Ultrasound showed a pathologic mass, 4 cm in diameter in the right
side of the abdomen and the echo of the normal appendix was not
displayed. Biochemistry laboratory results were within normal
range. At surgery, a smooth mass was noted at the base of the
appendix that continued into the cecum at the ileocecal junction.
The tumor was not observed to be involved with the appendix, which,
up to the base, was hard and encapsulated with no adhesions to the
surrounding tissue. The frozen section of the mass was consistent
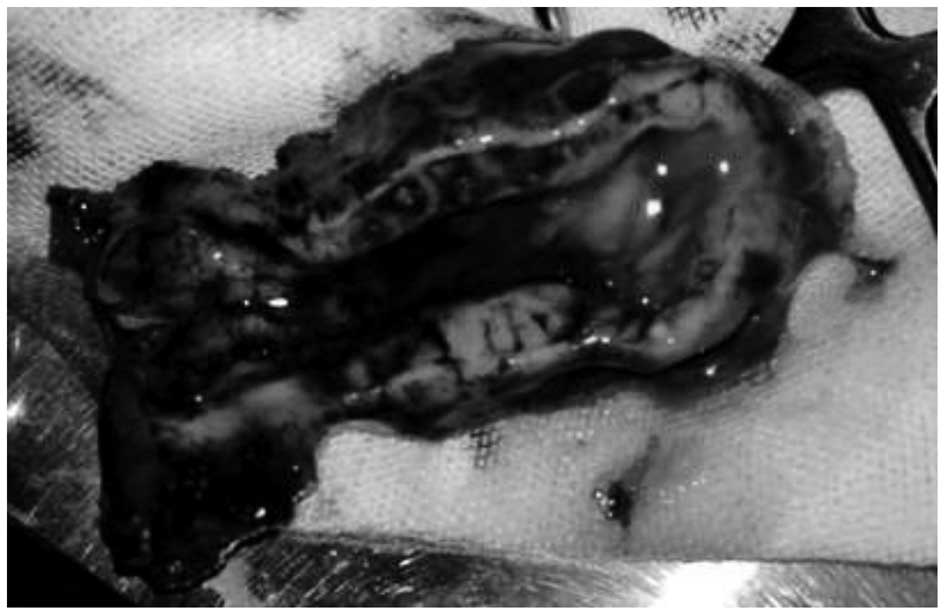
with appendiceal cystadenoma. An appendectomy was performed. When
the specimens were cut yellowish jelly-like mucinous material was
observed (Fig. 1). The patient was
discharged 7 days after surgery without discomfort and was followed
up at 4 months. The patient has had no recurrence so far.
Case 2
A 70-year-old woman was in good health until a large
abdominal mass was detected in her right lower quadrant upon
routine physical examination. Physical and laboratory examinations
were within the normal range, but the patient had a raised
carcinoembryonic antigen (CEA) level of 6.64 ng/ml. Ultrasound
found a pathologic mass, which was consistent with appendiceal
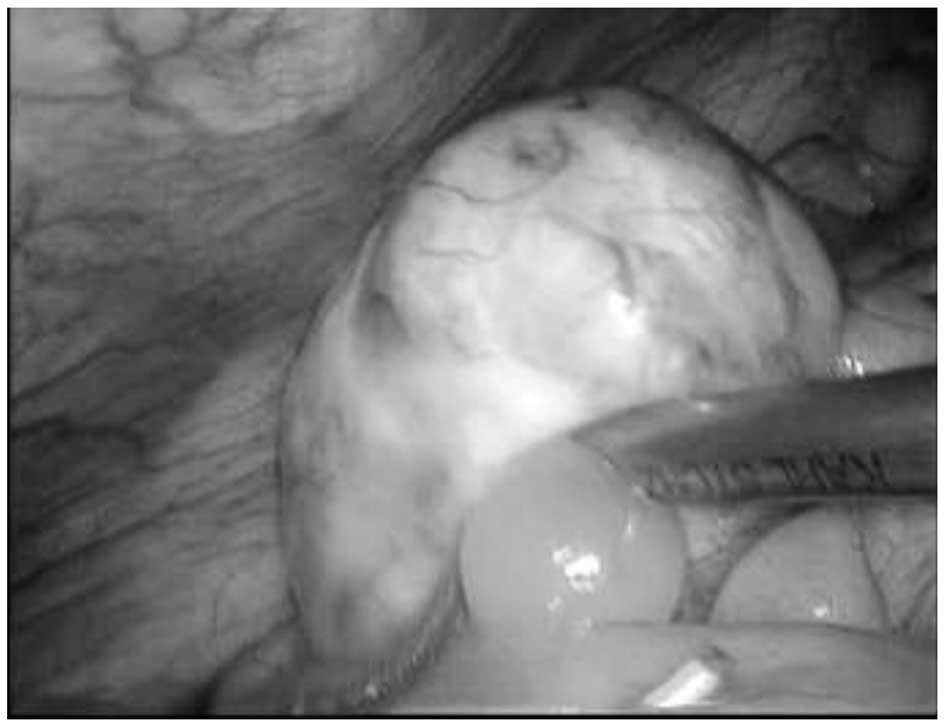
mucocele. The patient underwent a diagnostic laparoscopy.
Intraoperatively, dense adhesions were not encountered in the right
lower quadrant, but the capsule wall ruptured with an outflow of
yellowish jelly-like mucus (Fig.
2). The patient received an irrigation of the peritoneal cavity
instead of chemotherapy or hyperthermic chemotherapy. Ascites were
observed in the abdominal drainage following surgery. The volume of
drainage was assessed. There was 10 ml of yellowish mucus on day 5
after surgery, which increased to 15 ml on day 7. It was clean on
day 18 after surgery and the patient was discharged. Sonography
revealed seroperitoneum with maximum depth of ∼31 mm liquid
anechoic area during the patient’s hospitalization. Few
mucin-producing epithelial cells were found in the ascites on
cytology. Biochemistry laboratory results of ascites revealed that
Rivalta’s test was positive and a clinical diagnosis of PMP ascites
type was made (5). At the last
clinic visit, the patient reported with the chief complaint of
abdominal distension. The patient’s abdomen was again enlarged and
seroperitoneum was obtained again on sonographic studies. The
patients refused to receive an ultraphonic guided puncture and was
discharged after certain symptomatic approaches were performed.
Case 3
A 73-year-old female presented with a 1-month
history of a distended abdomen, without nausea and vomiting. A
computed tomography (CT) scan was obtained and revealed abnormal
appendix enhancement, which was partially thickened at the surface
of the liver and peritoneum. At this point, surgical options were
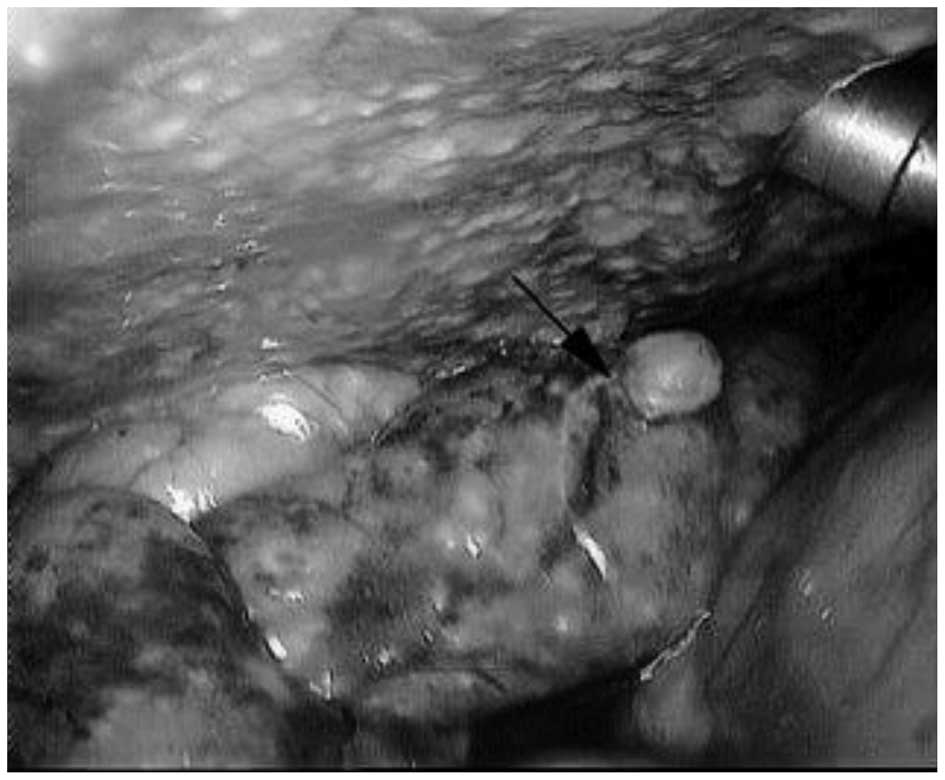
discussed and the patient underwent diagnostic laparoscopy.
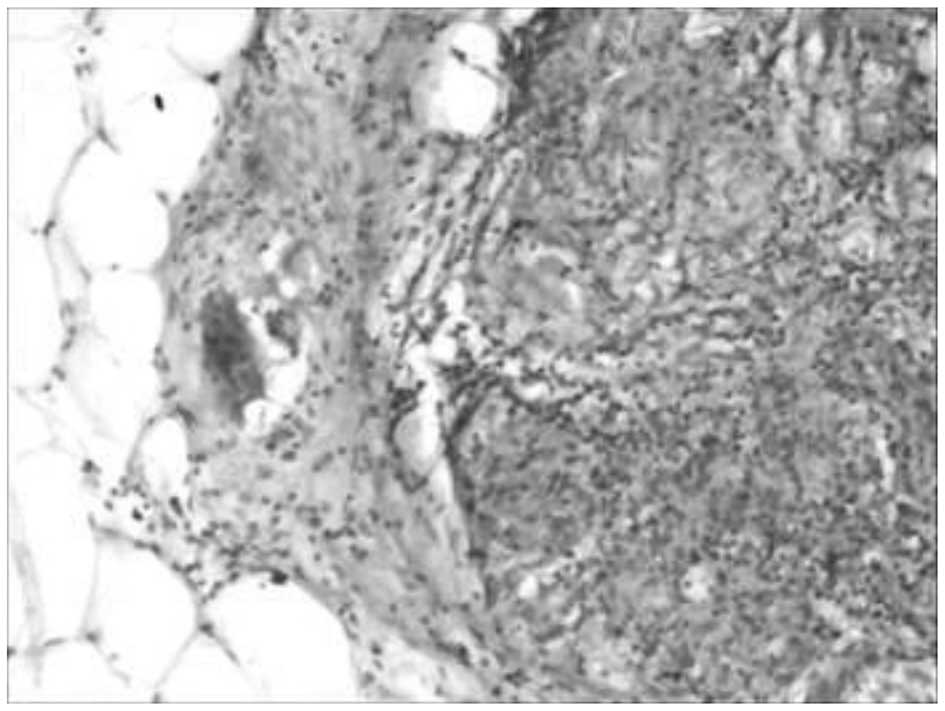
Operative findings included diffusely light yellow nodules located
at the surface of the liver and peritoneum without ascites
(Fig. 3). There was a firm and
irregular suspicious looking tumor measuring ∼2×2 cm at the end of
appendix (Fig. 4), suspected to be
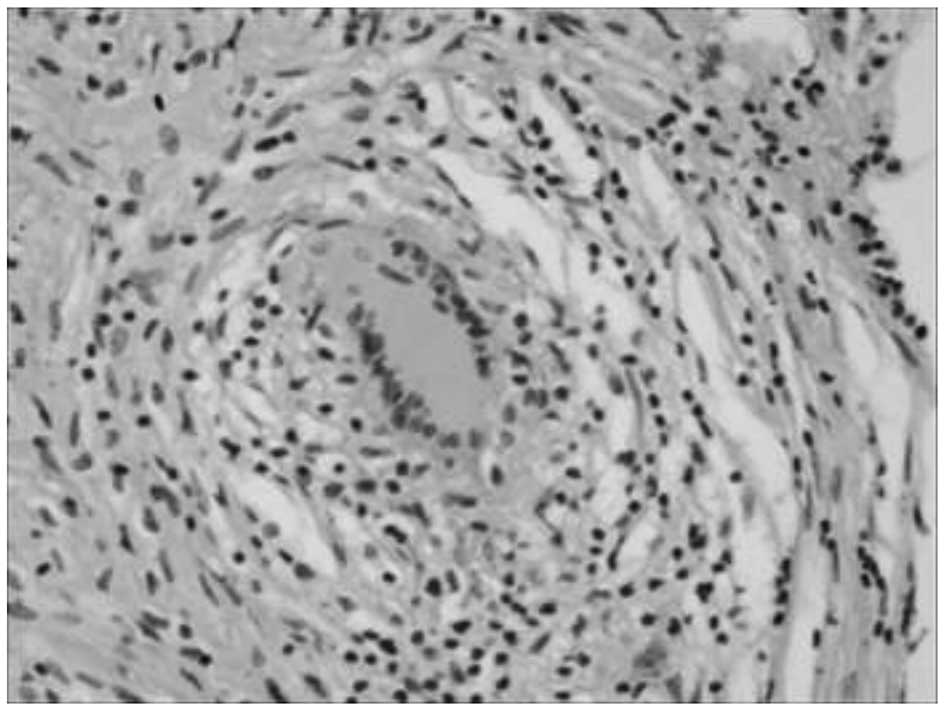
an appendiceal cystadenoma after man-made rupture. A section of the
epiploic appendices with nodules located was cut and intraoperative
histopathologic examination was performed. This demonstrated
non-necrotizing granuloma which was considered to be the same as
the diffusely light yellow nodules located at the surface of the
liver and peritoneum. There was little mucous membrane epithelium
in the nodule on histopathologic examination, thus
immunohistochemical methods were impossible. (Figs. 5 and 6). The medical team considered that a
diagnosis of intestinal tuberculosis could not be eliminated,
requiring medical therapy rather than surgery. In accordance with
the wishes of the patient’s family, an appendectomy was not
performed, even though a test for acid-fast bacilli was negative. A
PPD skin test was inconclusive. After further investigation of the
patient’s history, an ultrasound demonstrated a dilated and fluid
filled appendix. The clinical diagnosis was ascites and low-grade
appendiceal mucinous neoplasm. After 3 days of symptomatic
approaches the patient improved and symptoms disappeared. The
patient and her family refused to accept further checks and left
the hospital. The patient remained healthy for 7 months with no
treatment, but then had signs of bloating again. According to the
history and clinical presentation, this case matched the diagnosis
of PMP. The symptoms persisted but the patient’s family did not
consent to further surgery due to her age and general condition.
She was discharged for follow-up.
Discussion
In China, appendiceal cystadenoma has its own
characteristics (1). Located in an
unremarkable organ, appendiceal cystadenoma is not considered to be
serious. In large developing countries, such as China, community
physicians often treat it as appendicitis. Diagnosis will occur in
the first instance in community hospitals (2). Although the Chinese scientific
community are willing to research tumor oncology to improve the
survival time of months, they are yet to establish a set a
countermeasures for appendiceal cystadenoma, even though this would
be cost-effective and efficient (3). Chinese individuals often suffer from
right lower abdominal pain. Many grass-roots hospitals treat this
symptom collectively as ‘appendicitis’. If the pain is not severe
it may be treated with antibiotics, which are easily obtained. The
majority of sufferers of appendiceal cystadenoma are elderly
individuals, who are more willing to take antibiotics rather than
visit the Emergency Department (ED). These patients tend to only
visit the ED if they have experienced multiple bouts of pain or if
the pain becomes unbearable. This therapeutic strategy risks
spontaneous rupture or malignant transformation of the appendiceal
cystadenoma (4). In addition, the
majority of patients wish to continue to work and do not have the
time required to complete the follow-up treatment.
This study presents one case of a successful and
complete resection, one case of intraoperative rupture due to the
appearance of postoperative secondary PMP ascites, and one case of
PMP nodal type. Three types of PMP, namely PMP ascites type,
nodular type and mixed type (5–11) have
been reported in the literature. It appears that these three types
are part of a continuous process; the nodular type occurs late in
the process and evolves from PMP ascites. The second of our cases
did not receive cytoreductive surgery of hyperthermic chemotherapy
which consists of warmed saline solution containing 30 mg
mitomycin, 150 mg etoposide and 300 mg cisplatin, which is
introduced into the peritoneal cavity for 60 min to maintain the
abdominal temperature at 42–43°C. The patient also refused
intraperitoneal chemotherapy and experienced postoperative
secondary ascites at 2 weeks. Case 2 will be followed up to assess
whether their progress follows the path of case 3. The three
patients had very different costs of investments of medical
resources (Table I).
 | Table IDetails of three cases of appendiceal
cystadenoma. |
Table I
Details of three cases of appendiceal
cystadenoma.
| Case | Differential
prognosis | Responsibility | Treatment
observations | Spending on medical
resources |
|---|
| 1 | Recovery | - | Timely
Complete | Cost of surgery |
| 2 | Longer duration of
hospitalization
Follow-up care | Surgeon | Man-made
rupture
Non-effective remedial measures | Cost of
surgery
Longer duration of hospitalization
Follow-up care |
| 3 | Longer duration and
second hospitalization
Follow-up care | Physician | Misdiagnosis the
first time
The delay led to spontaneous rupture and PMP | Twice the
expenditure
Follow-up care |
Ultrasound is both pervasive and commonplace in
China. When finding the right lower quadrant filled with fluid,
ultrasound Doctors often consider appendix abscess rather than
appendiceal cystadenoma. At this time a personal medical history
should be taken to determine whether the patient has experienced
pain in the past and how severe the pain has become. Even if the
intraoperative pathological diagnosis is appendiceal cystadenoma,
clinicians still prefer to believe that it is an appendiceal cyst,
as this is more common. This results in: i) PMP: an appendix with
an abscess requires a few months of conservative treatment before
surgery. If the puncture fluid is mucus, the rupture caused by
intervention may lead to PMP. Delayed surgery causes it to develop
into secondary PMP. Case 3 presents a similar situation, since it
is difficult to eliminate the minimal residual disease by
chemotherapy and surgery. If the patient has a poorer prognosis,
this disease produces canceration, which is more common in younger
individuals and requires surgery as early as possible. ii) Rupture
of PMP: assumption that the cause is a small cyst may lead to
rupture of the PMP during surgery. Case 2 presents a similar
situation.
Health care reform in China has reached a critical
point. This economy has a large population and any small problem
will be multiplied by the sheer size of the population and become
exacerbated. Misunderstandings and treatment errors can result in a
different prognosis of the same disease, which may result in an
unreasonable allocation of medical resources.
With the global economy in distress, more direct and
convenient high economic cost measures should be taken. Healthcare
should be promoted in rural communities, particularly to the
elderly. The grassroots level hospital is the first step in
treating appendiceal disease and primary care doctors are a main
force. They must therefore deepen their knowledge and increase
their awareness of such presentations as described here. The
difficulty of surgery will not increase, in comparison to treating
appendicitis, if the treatment is not delayed. It may significantly
affect prevention, treatment and amelioration of prognosis; it is
therefore essential to understand the clinical manifestations of
appendiceal mucinous tumor and its comprehensive pathological
features, and to master the timely processing and proper disposal
of the tumor. Finally, early diagnosis has important clinical
significance as it can be complicated by malignant transformation,
volvulus, intestinal necrosis, obstruction, intussusception,
secondary infection, bleeding, PMP and even thrombosis of the iliac
vein (12–14). Doctors therefore need to increase
their understanding of recurrent right lower quadrant pain or mass,
recurrent episodes of chronic appendicitis, or a history of
appendiceal abscess.
Acknowledgements
The authors thank the patients for
providing written consent to publish this study. They also thank Dr
Weihuai Liu, Dr Mingfei Sun and Dr Pengfei Li, who have been a
source of encouragement and inspiration.
References
|
1
|
Marudanayagam R, Williams GT and Rees BI:
Review of the pathological results of 2660 appendicectomy
specimens. J Gastroenterol. 41:745–749. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rampone B, Roviello F, Marrelli D and
Pinto E: Giant appendiceal mucocele: Report of a case and brief
review. World J Gastroenterol. 11:4761–4763. 2005.PubMed/NCBI
|
|
3
|
Dhage-Ivatury S and Sugarbaker PH: Update
on the surgical approach to mucocele of the appendix. J Am Coll
Surgeons. 202:680–684. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Xiao S-Y: Mucinous neoplasms of the
vermiform appendix. Surgical Pathology Clinics. 3:395–409. 2010.
View Article : Google Scholar
|
|
5
|
Sugarbaker PH: New standard of care for
appendiceal epithelial neoplasms and pseudomyxoma peritonei
syndrome? Lancet Oncol. 7:69–76. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gillion JF, Franco D, Chapuis O, et al:
Appendiceal mucoceles, pseudomyxoma peritonei and appendiceal
mucinous neoplasms: Update on the contribution of imaging to choice
of the surgical approach. J Chir. 146:150–166. 2009.(In
French).
|
|
7
|
Moran BJ and Cecil TD: The etiology,
clinical presentation, and management of pseudomyxoma peritonei.
Surg Oncol Clin N Am. 12:585–603. 2003. View Article : Google Scholar
|
|
8
|
Carmignani CP, Sugarbaker TA, Bromley CM
and Sugarbaker PH: Intraperitoneal cancer dissemination: mechanisms
of the patterns of spread. Cancer Metastasis Rev. 22:465–472. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Smeenk RM, Verwaal VJ and Zoetmulder FA:
Pseudomyxoma peritonei. Cancer Treat Rev. 33:138–145. 2007.
View Article : Google Scholar
|
|
10
|
Smeenk RM, Bruin SC, van Velthuysen M-LF
and Verwaal VJ: Pseudomyxoma peritonei. Curr Probl Surg.
45:527–575. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Brueggen C, Baird G and Meisheid A:
Pseudomyxoma peritonei syndrome of appendiceal origin: an overview.
Clin J Oncol Nurs. 11:525–532. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ghidirim G, Gagauz I, Misin I, Canariov M,
Ionesii P and Zastavnitchi G: Mucinous cystadenocarcinoma of the
appendix complicated with spontaneous cutaneous fistula. Chirurgia
(Bucur). 102:231–235. 2007.(In Romanian).
|
|
13
|
Hamada T, Kosaka K, Shigeoka N, et al:
Torsion of the appendix secondary to appendiceal mucocele - gray
scale and contrast-enhanced sonographic findings. J Ultrasound Med.
26:111–115. 2007.PubMed/NCBI
|
|
14
|
Kelpis TG, Taliotis DM and Weerasena NA:
Rare association of a patient with Alagille syndrome and mitral
valve regurgitation. Thorac Cardiovasc Surg. 55:395–397. 2007.
View Article : Google Scholar : PubMed/NCBI
|