Introduction
Lung cancer is the most common cause of
cancer-related mortality worldwide. Half of the patients affected
by lung cancer develop metastases, occurring more frequently in the
lymph nodes, liver, bone, brain and adrenal glands (1). Gastrointestinal (GI) lung cancer
metastases are extremely rare and the reported incidence is ∼0.5%,
depending on the evaluation methods used, which include endoscopy,
surgical specimens or autopsy (2).
Multidetector computed tomography (CT) with contrast
medium is the optimum imaging procedure along with positron
emission tomography (PET)/CT to detect colonic masses. The value of
CT for depicting structural anatomy is widely appreciated and
applied clinically to identify abnormalities in a non-invasive
manner.
The most frequent clinical presentations of GI are
abdominal pain and hemorrhage; however, other symptoms, including
fatigue and dyspnea, are possible.
In the present study, we report the case of a young
male who presented with weakness, dyspnea and headache prior to
developing abdominal pain. These symptoms occurred following five
lines of chemotherapy targeting the primary tumor. The clinical
presentation was correlated with severe hyponatremia, most likely
induced by the secretion of an ectopic antidiuretic hormone.
The main previously published studies reporting on
GI metastases from the lung tumor are also reviewed. Written
informed consent was obtained from the patient.
Case report
Clinical diagnosis and presentation
A 43-year-old male with a 25-year smoking history
(45 pack-years) was referred to the Cardiopulmonary Department in
Sant’Andrea Hospital, Rome, Italy, in October 2009, due to a
persistent cough and high temperature for several days. The
parental history was positive for chronic obstructive pulmonary
disease and cancer. The patient received antibiotic treatment
without benefit over two weeks. Further investigations demonstrated
mild anemia with a hemoglobin (Hb) concentration of 119 g/l and
normal leukocyte and platelet counts. The oxy-hemoglobin saturation
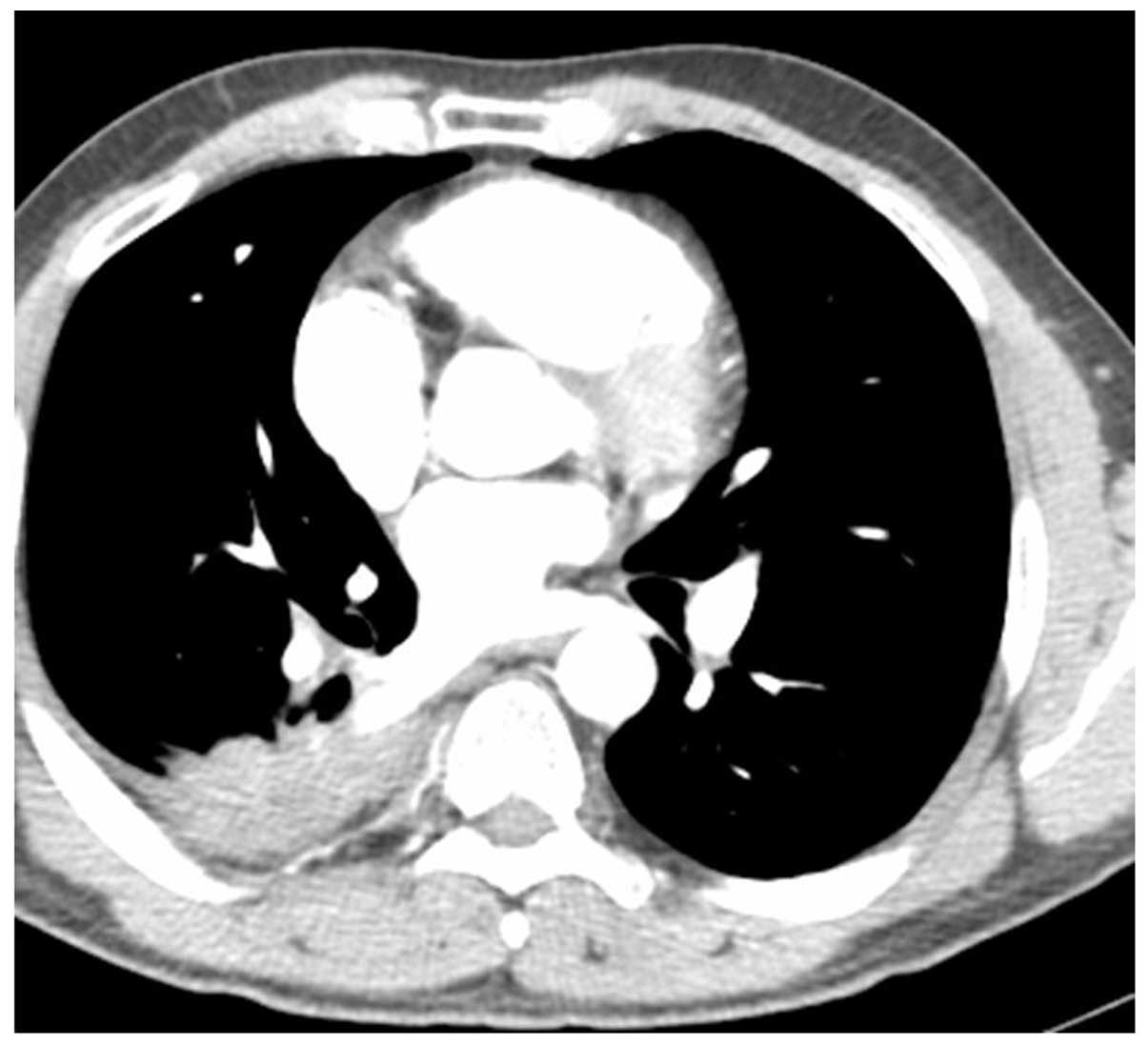
was also normal. A body CT scan revealed a lung mass measuring
nearly 5 cm (Fig. 1) in the lower
right lung and bronchoscopy with a bronchial lavage detected the
presence of lung cancer cells. The patient underwent thoracotomy;
however, it was not possible to remove the lesion due to
infiltration of the main pulmonary artery. A diagnosis of
adenocarcinoma involving vessels of the mediastinum was made, with
evidence of neither lymph node nor distant metastases (T4N0M0,
Stage IIIa). The patient underwent five lines of chemotherapy,
beginning in December 2009: cisplatin + vinorelbine, three cycles;
pemetrexed, six cycles; oral vinorelbine, three cycles; erlotinib
for only three months due to the occurrence of an early skin side
effect; gemcitabine, four cycles without significant changes in the
natural course of the disease. Two years after the diagnosis, the
patient was again admitted to our hospital as a result of fatigue,
dyspnea at rest, headache and neuralgia of the lower leg. The
hematological results were: Hb (11.0 g/l), platelet count
(105×109/l), white blood cells (12.1×109
g/l), the sodium serum level was extremely low (120 mEq/l) with
normal urinary and elevated D-dimer levels. The patient was
hypoxemic with a resting PaO2 of 59 mmHg.
A total body multidetected CT scan additionally
revealed a single brain metastasis located in the left parietal
lobe with concurrent GI involvement. A FDG-PET scan was also
performed demonstrating a tracer uptake with high intensity in two
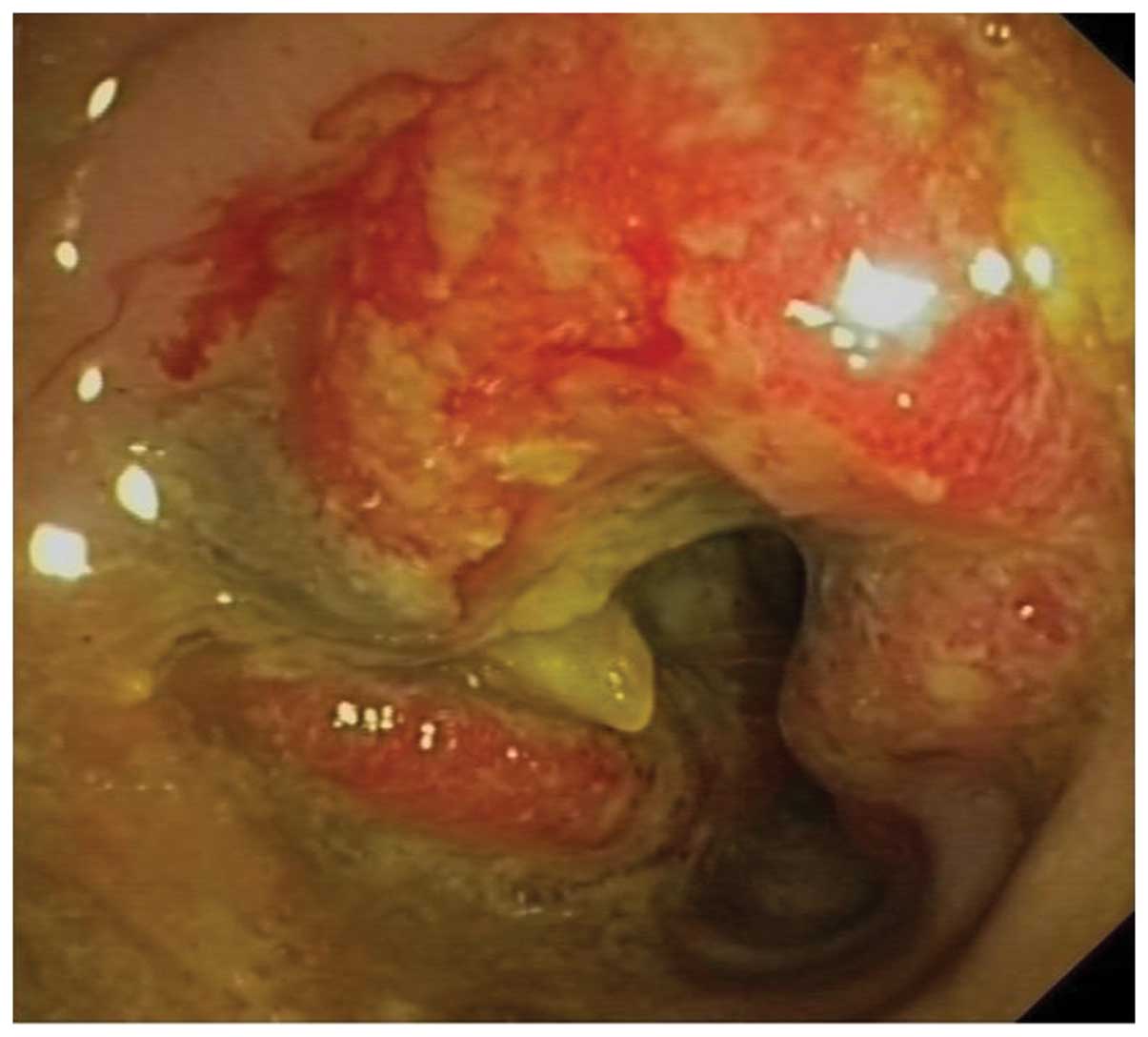
sites; the lung and sigmoid colon. A colonoscopy was also performed
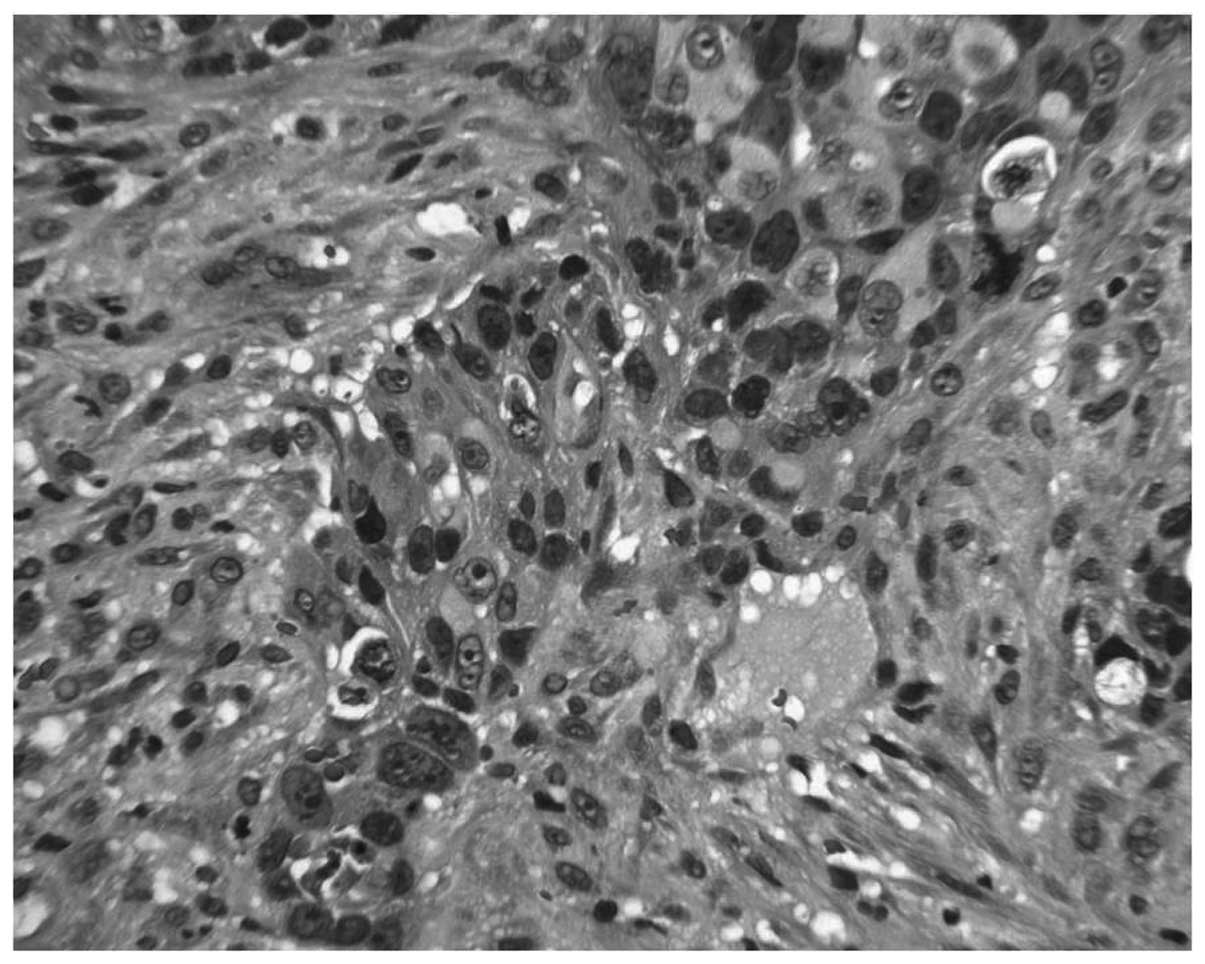
showing a colonic ulcerating lesion which bled on touch (Fig. 2) and an endoscopic biopsy revealed
neoplastic infiltration by a poorly differentiated adenocarcinoma
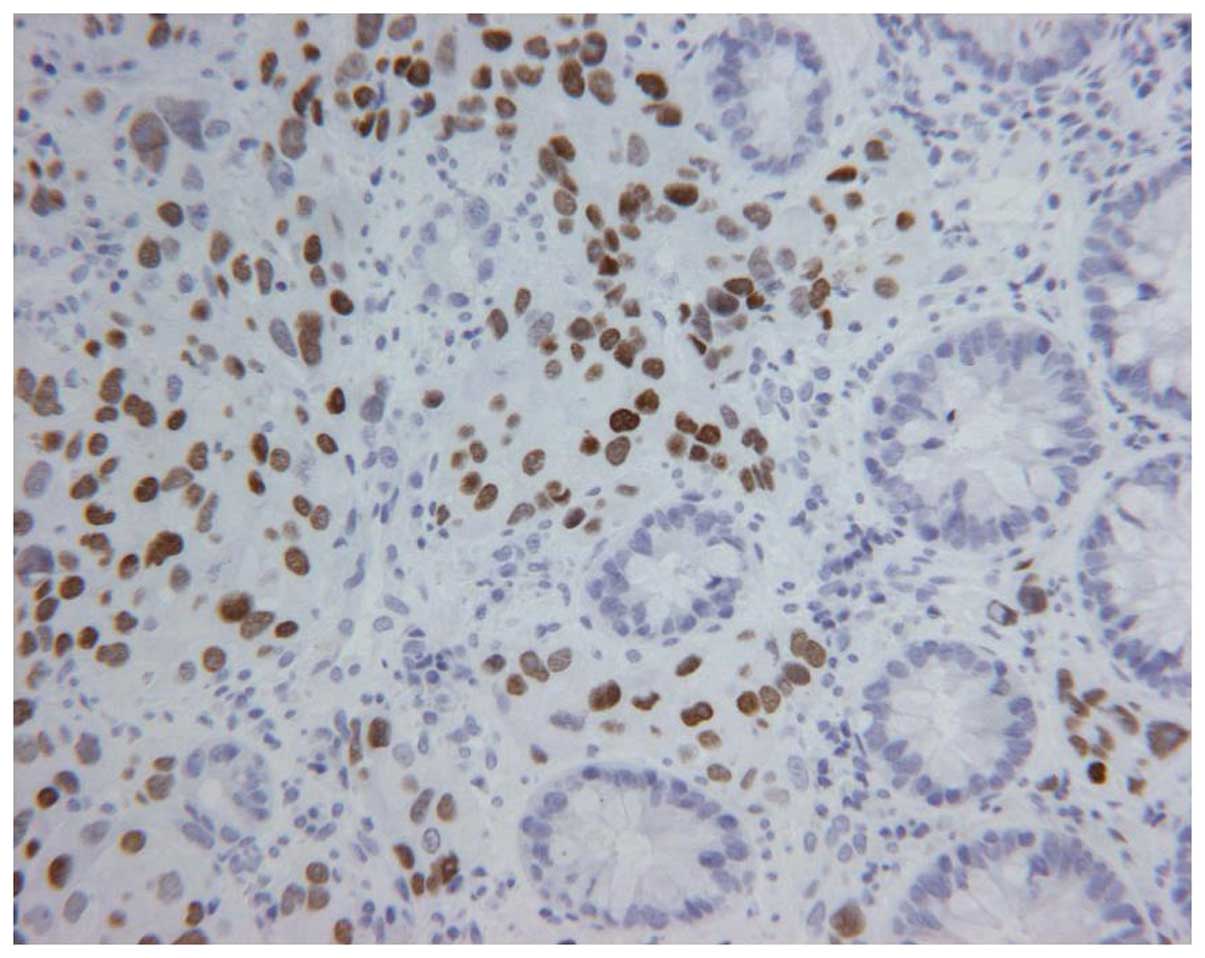
of lung origin. Immunostaining detected a positive correlation
between the neoplastic cells with thyroid transcription factor 1
(TTF-1) and cytokeratin 7 (CK7), with no evidence of CK20 and CDX2
expression (Figs. 3 and 4).
Treatment
The patient underwent brain radiotherapy and
treatment with dexamethasone, followed by moisturizing therapy.
Although no obstructive symptoms were evident, a surgical treatment
was recommended on the colonic lesion to avoid obstruction and
perforation, however; it was not performed due to worsening of the
patient’s general condition. One month later, the patient succumbed
to severe lung failure, dehydration and metabolic disorder.
Review of the literature
A search of the literature was conducted using
Medline and Scopus databases. The first study that we examined
identified 8,159 diagnosed cases of lung cancer collected between
1987 and 2008. The incidence of GI metastases in this study was
0.34%, 29 patients in absolute number. The specimens used to make
the pathological findings were obtained either on surgical
resection or on endoscopic biopsies (3). The data recorded included the stage of
lung cancer at initial diagnosis, and the interval between
diagnosis of lung cancer and the detection of GI metastasis. Only
two of the 29 patients with GI metastases were identified as having
colon metastatic presentation. In this study, all patients
underwent contrast-enhanced abdominal CT and the most common
clinical presentation was abdominal pain followed by anemia and
jaundice. The most common histological type was squamous cell
carcinoma, followed by adenocarcinoma. A perforation of the GI
tract occurred in 22% of the patients. There were six small bowel
metastases exhibiting either GI obstruction or perforation.
In the above-mentioned study, only 3 of the 21 lung
cancer patients were diagnosed with colonic metastases, consisting
of stomach or duodenal involvement. The most common symptoms were
bleeding, hemorrhage and abdominal pain. The prognosis was poor
upon the detection of metastases, particularly when they were
atypical in nature. As is evident from a study of 8,493 new cases
of lung cancer diagnosed between August 1998 and August 2007
(4), the incidence of GI
presentation was 0.34% and among these patients, 29 of the 31
patients had stomach and small bowel involvement and only 2
demonstrated colonic metastases. The majority of the patients had
synchronous metastases in other locations at the time of GI
metastasis discovery, mainly in the lymph nodes, liver, adrenal
glands, bone and brain. Another case of colonic metastasis from
primary carcinoma of the lung was described by Hirasaki et
al(5), who demonstrated a
positive fecal occult blood test. The histological type was
squamous (5).
Discussion
The case described in the present study is
characterized by an atypical location of metastasis from lung
cancer with an atypical course of disease and clinical
presentation. The management of metastasis from lung cancer with
atypical symptoms is the focus of this study. These symptoms are
mainly due to the ectopic production of antidiuretic hormones by
tumors. The observation of metastases in the large bowel, although
rare, have to be considered in cases where the lung cancer is not
well controlled and the patient does not exhibit a good response to
chemotherapy. The initial stage and smoking history of the patient
may affect the course of the disease.
The imaging techniques most commonly used for the
detection of primary and metastatic lesions are the multi-detecter
CT scan and PET-CT imaging, which are useful in the early detection
of tumor lesions. The typical clinical presentations of GI
metastases were variable; the majority of the patients with
symptomatic gastric and/or duodenal metastases demonstrated
abdominal pain (6,7), GI bleeding, obstruction and intestinal
perforation.
The circulating tumor cells are important in the
spread of neoplastic lesions to other organs (6), although metastases from primary lung
carcinoma in the small bowel are more frequently detected than
those in the large bowel. In this regard, Nishizawa et al
have recently described seven cases (0.17%) of symptomatic small
bowel metastases from 4,114 patients with lung cancer referred to
the author’s institution between 1995 and 2005 (8). The median life expectancy following
detection was 6 months, and the study revealed that a surgical
approach is not always feasible due to increased perioperative
risks. Large bowel metastasis was not described in this study.
The spread of tumor cells affects prognosis. The
diffusion of disease by the hematic or lymphatic routes causes a
worsening of clinical symptoms and survival rate (9). The direct invasion of the esophagus is
more likely than bowel metastasis via the hematic route as the
bowel is an organ which is distant from the bronchus (10,11).
We hypothesize that its rare presentation is due to arterial
perfusion of the left large bowel that is provided by the
mesenteric inferior artery. This artery originates from the
abdominal aorta at the level of the L3 vertebral body, and one of
its branches is the sigmoid artery which supplies the descending
colon, sigmoid colon and superior part of the rectum.
In the present study, we advance the hypothesis that
the burden of disease is due to the aggressiveness of the tumor,
and in addition, due to young age, the tumor cells propagate
extremely fast and reach the arterial system of the colon.
The patient initially presented with dyspnea at
rest, nausea and neuralgia of lower leg, most likely due to
compression of the femoral nerve roots and also fatigue. However,
neither rectal bleeding nor obstruction was observed.
An important consideration is that hyponatremia
syndrome has a wide range of symptoms from nausea and vomiting to
asthenia and edema of the brain, depending on the levels of sodium.
In the metastatic phase, these symptoms are caused by low serum
sodium levels, which form a metabolic condition in which there is
not enough sodium in the body fluids outside of the cells (12). It is a common electrolyte
abnormality observed frequently in cancer patients. It may be
caused by the inappropriate secretion of antidiuretic hormone
(13).
In this study, we identified that poorly
differentiated adenocarcinoma was also atypical. A study by Berger
et al(7) reported that
squamous cell lung carcinoma causes small bowel metastases more
frequently than other histotypes. An additional consideration is
that the choice of chemotherapy for first and second line treatment
is between classical and personalized treatment options, with human
epidermal growth factor receptor tyrosine-kinase inhibitors
(14). When the therapy is
ineffective and the disease continues to advance, only best
supportive care can be used.
References
|
1
|
Cheng L, Eng C, Nieman LZ, Kapadia AS and
Du XL: Trends in colorectal cancer incidence by anatomic site and
disease stage in the United States from 1976 to 2005. Am J Clin
Oncol. 34:573–580. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Grossmann I, Avenarius JK, Mastboom WJ and
Klaase JM: Preoperative staging with chest CT in patients with
colorectal carcinoma: not as a routine procedure. Ann Surg Oncol.
17:2045–2050. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kim SY, Ha HK, Park SW, Kang J, Kim KW,
Lee SS, Park SH and Kim AY: Gastrointestinal metastasis from
primary lung cancer: CT findings and clinicopathologic features.
AJR Am J Roentgenol. 193:W197–W201. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lee PC, Lo C, Lin MT, Liang JT and Lin BR:
Role of surgical intervention in managing gastrointestinal
metastases from lung cancer. World J Gastroenterol. 17:4314–4320.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hirasaki S, Suzuki S, Umemura S, Kamei H,
Okuda M and Kudo K: Asymptomatic colonic metastases from primary
squamous cell carcinoma of the lung with a positive fecal occult
blood test. World J Gastroenterol. 14:5481–5483. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
O’Flaherty JD, Gray S, Richard D, Fennell
D, O’Leary JJ, Blackhall FH and O’Byrne KJ: Circulating tumor
cells, their role in metastases and their clinical utility in lung
cancer. Lung Cancer. 76:19–25. 2012.PubMed/NCBI
|
|
7
|
Berger A, Cellier C, Daniel C, Kron C,
Riquet M, Barbier JP, Cugnenc PH and Landi B: Small bowel
metastases from primary carcinoma of the lung: clinical findings
and outcome. Am J Gastroenterol. 94:1884–1887. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nishizawa Y, Kobayashi A, Saito N, Nagai
K, Sugito M, Ito M and Nishizawa Y: Surgical management of small
bowel metastases from primary carcinoma of the lung. Surg Today.
42:233–237. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Fujiwara A, Okami J, Tokunaga T, Maeda J,
Higashiyama M and Kodama K: Surgical treatment for gastrointestinal
metastasis of non-small-cell lung cancer after pulmonary resection.
Gen Thorac Cardiovasc Surg. 59:748–752. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
McNeill PM, Wagman LD and Neifeld JP:
Small bowel metastases from primary carcinoma of the lung. Cancer.
59:1486–1489. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yang CJ, Hwang JJ, Kang WY, Chong IW, Wang
TH, Sheu CC, Tsai JR and Huang MS: Gastro-intestinal metastasis of
primary lung carcinoma: clinical presentations and outcome. Lung
Cancer. 54:319–323. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lien YH and Shapiro JI: Hyponatremia:
clinical diagnosis and management. Am J Med. 120:653–658. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Peri A and Combe C: Considerations
regarding the management of hyponatremia secondary to SIADH. Best
Pract Res Clin Endocrinol Metab. 26:S16–S26. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Shepherd FA, Rodrigues Pereira J, Ciuleanu
T, Tan EH, Hirsh V, Thongprasert S, Campos D, Maoleekoonpiroj S,
Smylie M, Martins R, van Kooten M, Dediu M, Findlay B, Tu D,
Johnston D, Bezjak A, Clark G, Santabárbara P and Seymour L;
National Cancer Institute of Canada Clinical Trials Group:
Erlotinib in previously treated non small cell lung cancer. N Engl
J Med. 353:123–132. 2005. View Article : Google Scholar : PubMed/NCBI
|