Introduction
The ear canal, middle ear and temporal bone are rare
sites of malignancies among which squamous cell carcinoma is the
most commonly occurring cancer type (1). The incidence of this tumor in the US
is estimated to be only 0.1–0.6/100,000 population/year. However,
the challenging anatomical location and invasive nature makes this
type of cancer extremely difficult to treat, particularly in more
advanced stages (2). Although
several treatment modalities have been described in the literature,
there is a lack of consensus as to the best treatment, mainly due
to the absence of prospective randomized studies (3). The most frequently reported treatment
involves surgical resection with or without adjuvant radiotherapy.
Chemotherapy, brachytherapy or alternative treatment methods such
as superselective intra-arterial chemotherapy injection have been
described in the literature, however, their exact role remains to
be determined (4,5).
While there is a lack of data for optimal tumor
treatment, a convincing body of evidence has shown that early stage
cancer is associated with a higher treatment success and survival
rate, compared to late stage disease (3,6).
Therefore, the most important factors in treating patients with
this type of malignancy are early detection and diagnosis. However,
since many patients present with non-specific and unclear signs of
chronic inflammation and infection, detection and diagnosis of this
malignant type is difficult. Additionally, chronic and recurring
infections, thought to often precede tumor development, can lead to
decreased follow-up motivation, resulting in a delay in
diagnosis.
In light of these diagnostic and therapeutic
challenges, the present report described a case of advanced
squamous cell carcinoma of the external auditory canal in a patient
whose cancer was initially diagnosed and treated as osteomyelitis,
in the setting of chronic ear infections, at a non-US
institution.
Case report
A 73-year-old Hispanic female with a past medical
history of diabetes and chronic left-sided suppurative otitis media
that resulted in mastoidectomy in her mid-thirties, was admitted to
our institution with left-sided otalgia. The pain was associated
with a serosanguineous ear discharge, dizziness, headache, fever,
sore throat, generalized weakness and a twenty-pound unintentional
weight loss. Previously, the patient had been diagnosed and treated
for chronic mastoiditis and later for temporomandibular joint
osteomyelitits that extended to the temporal bone. She received
several courses of antibiotics, without relief. At the time,
cultures of the ear grew staphylococcus epidermidis and diphteroid
species. Left ear canal biopsy revealed a small number of
keratinizing atypical squamous cells and chronic inflammation,
suspicious for neoplasia.
On admission to our institution, physical
examination revealed serosanguineous discharge from the left
external ear canal as well as tenderness of the left mastoid
process, the temporomandibular joint and the submandibular region.
The patient’s symptoms were associated with left-sided diffuse
facial swelling and signs consistent with ipsilateral facial nerve
palsy. Basic laboratory work-up revealed a slightly elevated white
blood cell count of 12.2×106/μl, but otherwise
normal laboratory parameters. Cultures of the blood and ear
discharge were both negative. The chest roentgenogram was within
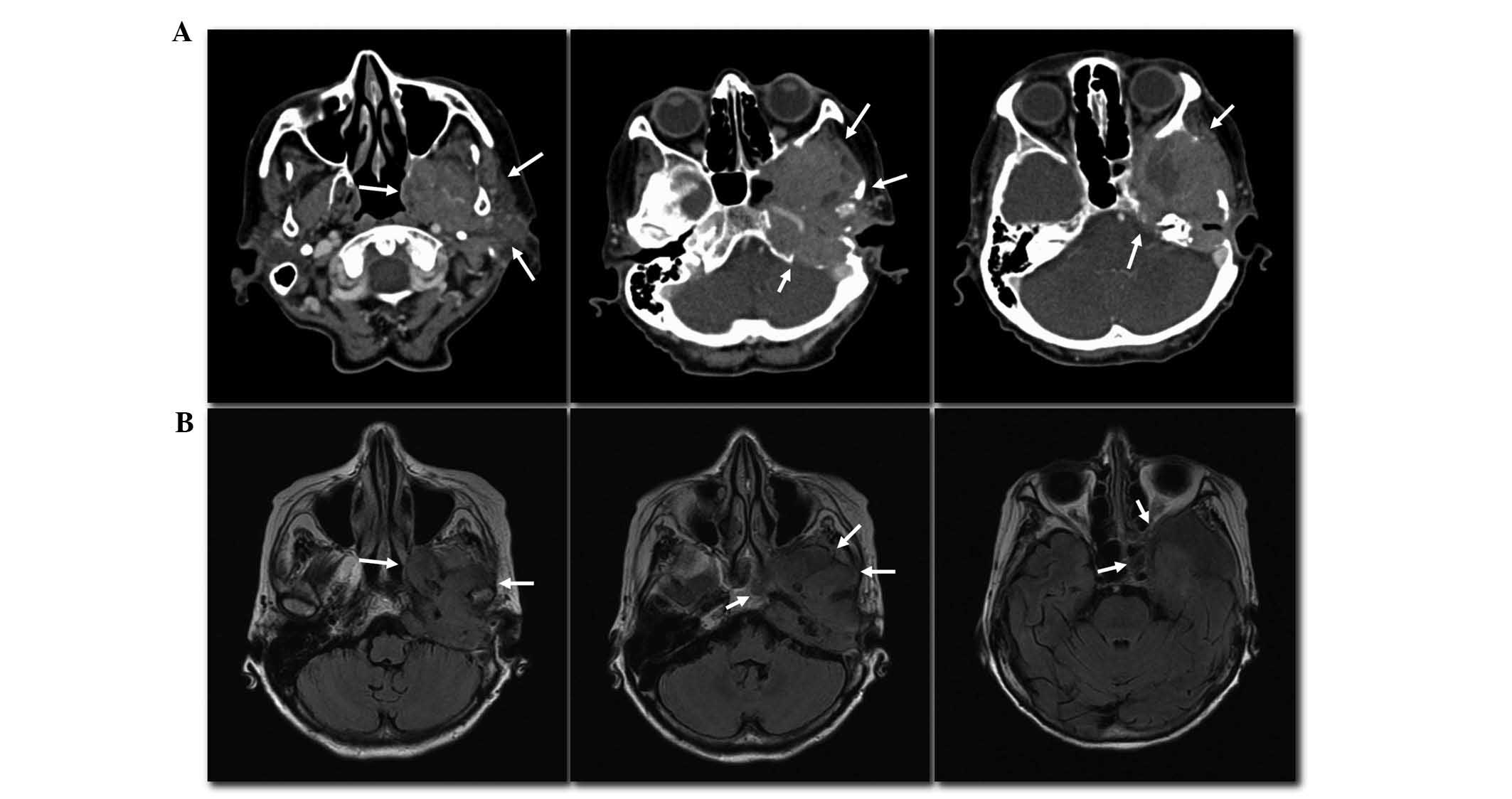
normal limits. Computed tomography (CT) of the head with and
without contrast, revealed a soft tissue mass invading the left
middle cranial fossa with destruction of the adjacent sphenoid and
temporal bones (Fig. 1A). Magnetic
resonance imaging (MRI) of the brain with and without contrast,
revealed an enhancing, expansive and erosive lesion in the same
area with invasion of the left cavernous sinus (Fig. 1B). Fine needle aspiration of the
mass in left middle cranial fossa identified well-differentiated
squamous cell carcinoma. CT of the chest, abdomen and pelvis were
negative for metastatic disease.
Based on the Pittsburgh staging system, the
diagnosis of a stage IV squamous cell carcinoma was made (7). Considering the advanced stage, the
patient was deemed not to be a surgical candidate. She received a
course of specific palliative radio-therapy for advanced head and
neck cancer (Quad shot) (8), with
concurrent carboplatin radiosensitization. This treatment consisted
of intensity-modulated radiation treatment administered twice
daily, 2 days per week. Over an 8-week period, the left external
auditory canal was exposed to a total dose of 29.6 Gy, given in 8
fractions, followed by radiation to the left middle ear with a
total of 14.8 Gy, given in 4 fractions. Minimal improvement was
noted in the patient’s symptoms over a short period of time, prior
to return of a steady decline that eventually led to the patient
succumbing to the disease.
Discussion
Squamous cell carcinoma of the external auditory
meatus, middle ear and temporal bone is an unusual and rare
malignancy, which may explain the fact that there is no American
Joint Committee on Cancer (AJCC) or Union for International Cancer
Control (UICC) staging system for this type of neoplasm. Arriaga
et al(7) suggested a staging
system in 1990, which has since entered the literature as the
Pittsburgh staging system, allowing for a more accurate comparison
of treatment and outcomes in patients with this disease. This
system underwent minor revision by Moody et al(9) in 2000 (Table I).
 | Table IThe Pittsburgh classification system
for external auditory meatus carcinoma. |
Table I
The Pittsburgh classification system
for external auditory meatus carcinoma.
| Stage | Status |
|---|
| T1 | Tumor limited to EAM
without bony erosion or evidence of soft tissue extension |
| T2 | Limited EAM erosion
(not full thickness), or radiographic findings consistent with
limited (<5 mm) soft tissue involvement |
| T3 | Erosion into the EAM
(full thickness) with limited (<5 mm) soft tissue involvement,
or tumor involving the middle ear and/or mastoid, or presence of
facial paralysis |
| T4 | Tumor eroding the
cochlea, petrous apex, medial wall of middle ear, carotid canal,
jugular foramen or dura, or with extensive (>5 mm) soft tissue
involvement |
| N | As described by the
American Joint Committee for classifying lymph node involvement in
head and neck neoplasms. However, any node involvement is
considered to be advanced disease: stage III, T1, N1; stage IV, T2,
T3, T4, N1 |
| M | Any metastasis is
considered to be advanced disease: stage IV, M1 |
Although the lack of a unifying classification,
along with the rarity of the disease have made the development of
clear treatment guidelines difficult, there have been uniform
observations in the literature, that may help us outline the most
beneficial treatment strategies for this patient population.
Surgical resection is crucial as a treatment
modality, and early surgical intervention is associated with
increased survival (9–11). Additionally, different stages of the
disease may require a different level of surgical resection.
Tumors that are limited to the external auditory
canal with or without limited bone erosion and soft tissue
involvement are classified as Pittsburgh stages T1 and T2 (Table I). In these stages, local resection
of the external auditory canal does not seem to be sufficient
(12). Mastoidectomy, lateral
temporal bone resection (TBR) and subtotal TBR are more appropriate
and these techniques showed similar survival in a retrospective
review including 144 patients, with a five-year survival of 50,
48.6 and 50%, respectively (13).
The same study did not find evidence of improved survival with the
addition of radiation therapy (RT) to TBR (with 48 vs. 44.4% 5-year
survival for TBR + RT vs. TBR alone, respectively) (13). In a retrospective analysis of 21
patients, Kollert et al(12)
found that stage-dependent lateral or subtotal TBR combined with
parotidectomy as well as a neck dissection was the most beneficial
approach. However, the role of chemotherapy remains to be
determined. Ogawa et al(14)
suggest that it does not affect disease-free survival (DFS).
Authors of that study found the 5-year DFS rate in T1, T2 and T3
patients to be 83, 45 and 0% in the RT group (P<0.0001) and 75,
75 and 46% in the group that underwent surgery with RT (P=0.13).
Based on those results, they recommend radical radiotherapy alone
as the treatment of choice for early-stage (T1) disease and surgery
with radiotherapy for more advanced (T2-3) disease (14).
In Pittsburgh stage T3 disease, i.e., with middle
ear extension, Kollert et al(12) again recommend stage-dependent
lateral or subtotal TBR combined with parotidectomy and neck
dissection (12). Prasad et
al(13) noted that subtotal TBR
appears to be more beneficial than lateral TBR or mastoidectomy,
with 42 vs. 29 vs. 17% 5-year survival. The same study showed clear
survival benefits from additional RT only in patients who underwent
mastoidectomy (20 vs. 0% 5-year survival). However, the benefits of
RT could not be estimated in patients with lateral or total TBR due
to lack of data (13). While some
investigators suggest RT for recurrent cases, questionable free
margins and/or lymph node metastases (12), other authors recommend surgery with
RT as the standard of care in general for all advanced disease
(T2-3) (14).
Involvement of the petrous apex, cochlea, carotid,
jugular foramen, dura, temporomandibular joint or the styloid
process as well as the presence of facial paresis signal Pittsburgh
stage T4 disease (Table I). In case
of dura mater involvement, resection of the affected dura does not
appear to improve survival. Furthermore, whether surgical resection
of the involved petrous apex, brain parenchyma or internal carotid
artery is of any survival benefit remains unclear (13). However, surgery remains important in
advanced disease. In cases where T4 lesions did not involve the
pyramidal apex, carotid canal, dura or any lymph nodes, surgical
intervention was found to improve the estimated survival rate to a
level as good as that of T3 lesions (15). Similarly, in a retrospective case
review of 12 patients, the 5-year estimated survival improved up to
75% for T4 tumors after surgery versus 16% for patients who did not
undergo surgery, (15). In T4
disease, carotid and middle- or posterior fossa invasion are
considered to be unresectable (1).
Irrespective of stage of the disease, Moffat et
al(11) emphasized the
importance of early referral and aggressive primary surgical
treatment with post-operative radiotherapy, in a retrospective
analysis of 39 patients. Another important factor is complete
resection with clear surgical margins. Several retrospective
analyses showed increased survival rates with tumor-free resection
margins, in all stages of disease (12,14–17).
However, our patient did not qualify as a surgical candidate due to
her advanced stage at presentation.
There is conflicting data in the literature
regarding the benefits of chemotherapy with or without radiation.
While Ogawa et al(14) did
not find chemotherapy to increase DFS in any stage of the disease,
a multi-institutional review by Yin et al(17) has suggested increased survival with
chemotherapy in stage 3 and 4 disease, if combined with surgery and
radiation (28.7 vs. 52.5%; surgery + radiation vs. surgery +
radiation + chemotherapy).
In a small study (18) that evaluated six patients who
underwent radiation with total doses ranging from 30 to 88 Gy, two
patients who received doses over 60 Gy survived for >5 years,
compared to a mean survival of 3 years and 11 months. The authors
of that study concluded that tumor doses of at least 70 Gy may be
necessary for local control of advanced disease (18). While Quad shot therapy was validated
in a phase II trial as a palliative approach for advanced head and
neck cancers, it has not been specifically studied in external
auditory canal carcinomas (8).
However, this approach has been shown to have a response rate in
>50% of patients with advanced head and neck cancers. This
treatment can be delivered with minimal toxicity and has been shown
to significantly improve the quality of life (8). While our patient had minimal benefits
from Quad shot therapy, larger scale studies are necessary to
define the exact role of this and alternative radiation regiments
with or without chemotherapy.
Predictors of poor survival in this patient
population include extensive tumor involvement, neck node
metastasis, facial nerve paralysis, pain, middle ear involvement,
cervical or periparotid lymphadenopathy and concomitant chronic
otitis media (1,7,15,19).
Advanced stage disease, node-positive disease, positive surgical
margins, tumor recurrence, poorly differentiated squamous cell
histological findings, brain involvement and salvage surgery were
also associated with a poorer outcome (11,17).
Possible predisposing factors for the disease are preceding head
and neck radiation for nasopharyngeal and skin neoplasms (1).
In conclusion, in this report, we describe a case of
a rare and aggressive tumor type for which the most beneficial
therapeutic approach remains to be determined. It is clear however,
that, if diagnosed late, this disease exhibits poor outcomes, while
it is associated with higher response rates and increased survival
at early stages.
Thus, emphasis should be placed on the importance of
early detection, diagnosis and treatment of squamous cell carcinoma
of the temporal bone and middle ear as the simplest and most
effective measure to increase patient survival. We also urge the
medical community for prompt diagnostic work-up in patients with
chronic and treatment-resistant ear infections.
References
|
1
|
Lobo D, Llorente JL and Suarez C: Squamous
cell carcinoma of the external auditory canal. Skull Base.
18:167–172. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kuhel WI, Hume CR and Selesnick SH: Cancer
of the external auditory canal and temporal bone. Otolaryngol Clin
North Am. 29:827–852. 1996.PubMed/NCBI
|
|
3
|
Gidley PW: Managing malignancies of the
external auditory canal. Expert Rev Anticancer Ther. 9:1277–1282.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ueda Y, Kurita T, Matsuda Y, et al:
Superselective, intra-arterial, rapid infusion chemotherapy for
external auditory canal carcinoma. J Laryngol Otol. 123(Suppl 31):
75–80. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Budrukkar A, Bahl G, Bhalavat R, et al:
High-dose-rate brachytherapy boost for carcinoma of external
auditory canal. Brachytherapy. 8:392–395. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Prabhu R, Hinerman RW, Indelicato DJ, et
al: Squamous cell carcinoma of the external auditory canal:
long-term clinical outcomes using surgery and external-beam
radiotherapy. Am J Clin Oncol. 32:401–404. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Arriaga M, Curtin H, Takahashi H, et al:
Staging proposal for external auditory meatus carcinoma based on
preoperative clinical examination and computed tomography findings.
Ann Otol Rhinol Laryngol. 99:714–721. 1990. View Article : Google Scholar
|
|
8
|
Corry J, Peters LJ, Costa ID, et al: The
‘QUAD SHOT’ - a phase II study of palliative radiotherapy for
incurable head and neck cancer. Radiother Oncol. 77:137–142.
2005.
|
|
9
|
Moody SA, Hirsch BE and Myers EN: Squamous
cell carcinoma of the external auditory canal: an evaluation of a
staging system. Am J Otol. 21:582–588. 2000.PubMed/NCBI
|
|
10
|
Austin JR, Stewart KL and Fawzi N:
Squamous cell carcinoma of the external auditory canal. Therapeutic
prognosis based on a proposed staging system. Arch Otolaryngol Head
Neck Surg. 120:1228–1232. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Moffat DA, Wagstaff SA and Hardy DG: The
outcome of radical surgery and postoperative radiotherapy for
squamous carcinoma of the temporal bone. Laryngoscope. 115:341–347.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kollert M, Draf W, Minovi A, et al:
[Carcinoma of the external auditory canal and middle ear:
therapeutic strategy and follow up]. Laryngorhinootologie.
83:818–823. 2004.(In German).
|
|
13
|
Prasad S and Janecka IP: Efficacy of
surgical treatments for squamous cell carcinoma of the temporal
bone: a literature review. Otolaryngol Head Neck Surg. 110:270–280.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ogawa K, Nakamura K, Hatano K, et al:
Treatment and prognosis of squamous cell carcinoma of the external
auditory canal and middle ear: a multi-institutional retrospective
review of 87 patients. Int J Radiat Oncol Biol Phys. 68:1326–1334.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Nakagawa T, Kumamoto Y, Natori Y, et al:
Squamous cell carcinoma of the external auditory canal and middle
ear: an operation combined with preoperative chemoradiotherapy and
a free surgical margin. Otol Neurotol. 27:242–248. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Pfreundner L, Schwager K, Willner J, et
al: Carcinoma of the external auditory canal and middle ear. Int J
Radiat Oncol Biol Phys. 44:777–788. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yin M, Ishikawa K, Honda K, et al:
Analysis of 95 cases of squamous cell carcinoma of the external and
middle ear. Auris Nasus Larynx. 33:251–257. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Shimatani Y, Kodani K, Mishima K, et al:
Evaluation of the results of radiotherapy for carcinoma involving
the external auditory canal or middle ear. Nihon Igaku Hoshasen
Gakkai Zasshi. 62:739–743. 2002.(In Japanese).
|
|
19
|
Moffat DA and Wagstaff SA: Squamous cell
carcinoma of the temporal bone. Curr Opin Otolaryngol Head Neck
Surg. 11:107–111. 2003. View Article : Google Scholar : PubMed/NCBI
|