Introduction
Malignant lymphomas (ML) frequently involve
intrathoracic organs, but endobronchial involvement (EBI) is
relatively rare (1–3). The present study describes the case of
a patient with lymphoplasmacytic lymphoma (LPL) transforming to
large cell lymphoma, characterized by an endobronchial tumor of the
main carina. To the best of our knowledge, this type of progression
of LPL has not previously been reported. Notably, the present study
used an autofluorescence imaging (AFI) bronchovideoscope system to
evaluate the invasion of ML into the surrounding mucosa. The study
provides further insight into the clinical significance of the EBI
of ML and the utility of bronchoscopic examination in these
patients. Written informed consent was obtained from the
patient.
Case report
A 41-year-old male was referred to the Respiratory
Division of Nagoya City University Hospital subsequent to
experiencing a cough with bloody sputum for a few days. The patient
had a 4-year history of a low-grade non-Hodgkin’s lymphoma (NHL)
with IgM paraproteinemia, diagnosed as LPL. The primary LPL lesion
was in the bone marrow, with no lesions detected on computed
tomography (CT) or 18F-fluorodeoxyglucose-positron emission
tomography (FDG-PET). The patient had been treated with
chemotherapy, including 8 courses of R-COP therapy (rituximab,
cyclophosphamide, oncovin and prednisolone), 12 courses of
fludarabine and 5 courses of bendamustine, and had attained a good
partial response (PR). The cough with bloody sputum was first
noticed ∼1 month after the final dose of chemotherapy.
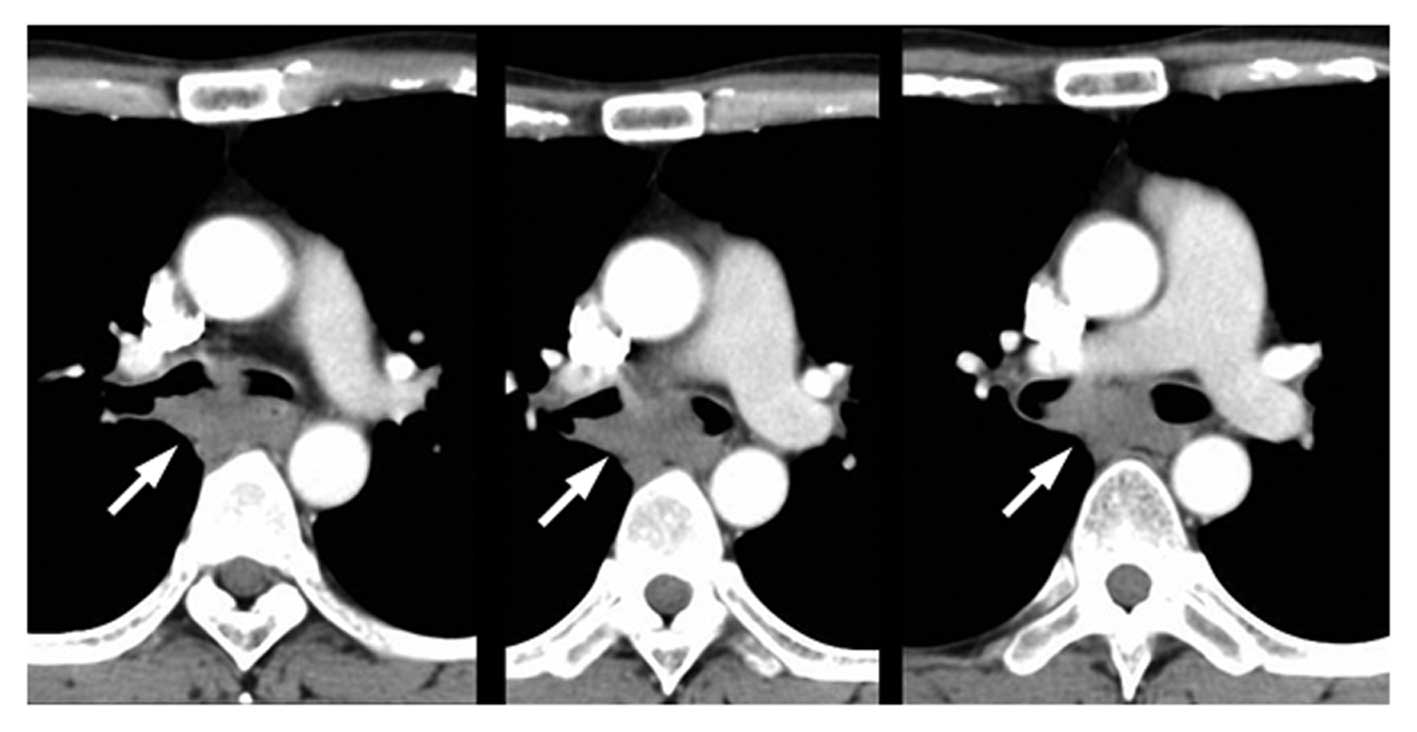
A physical examination revealed crackles in each
lung and a oxyhemoglobin saturation of 96% in normal room air. A CT
scan showed subcarinal lymphadenopathy and an endobronchial tumor
involving the main carina (Fig. 1).
The patient’s platelet count was low [63,000/μl (normal,
>148,000/μl)], and the concentration of circulating
interleukin-2 receptor (IL-2R) was slightly elevated [538 U/ml
(normal, <519 U/ml)]. The lactate dehydrogenase (LDH) level was
within the normal range. The IgG, IgA and IgM concentrations were
408 mg/dl (normal, 870–1700 mg/dl), 11 mg/dl (normal, 110–410
mg/dl) and 187 mg/dl (normal, 35–220 mg/dl), respectively. A
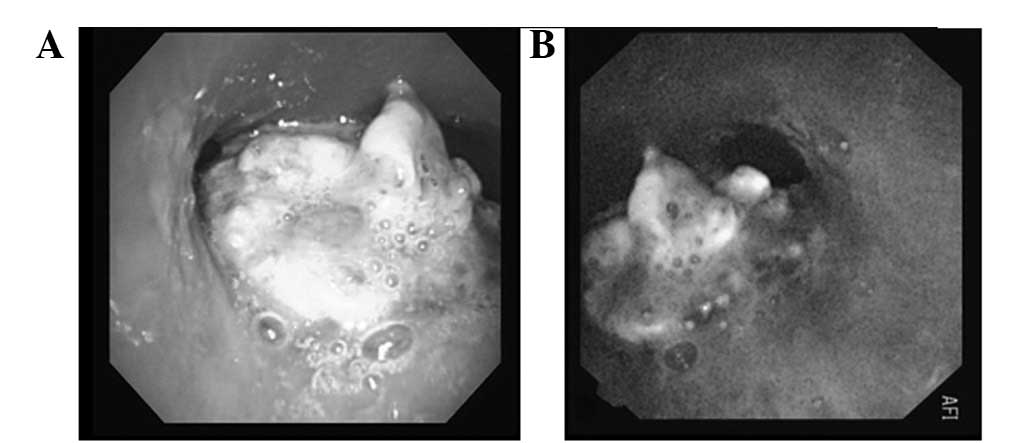
bronchoscopic examination showed an exophytic tumor with rough
surfaces and a white, moss-like appearance at the main carina
(Fig. 2). An autofluorescence
imaging (AFI) examination showed that the exophytic tumor and
surrounding area were magenta in color. A transbronchial biopsy
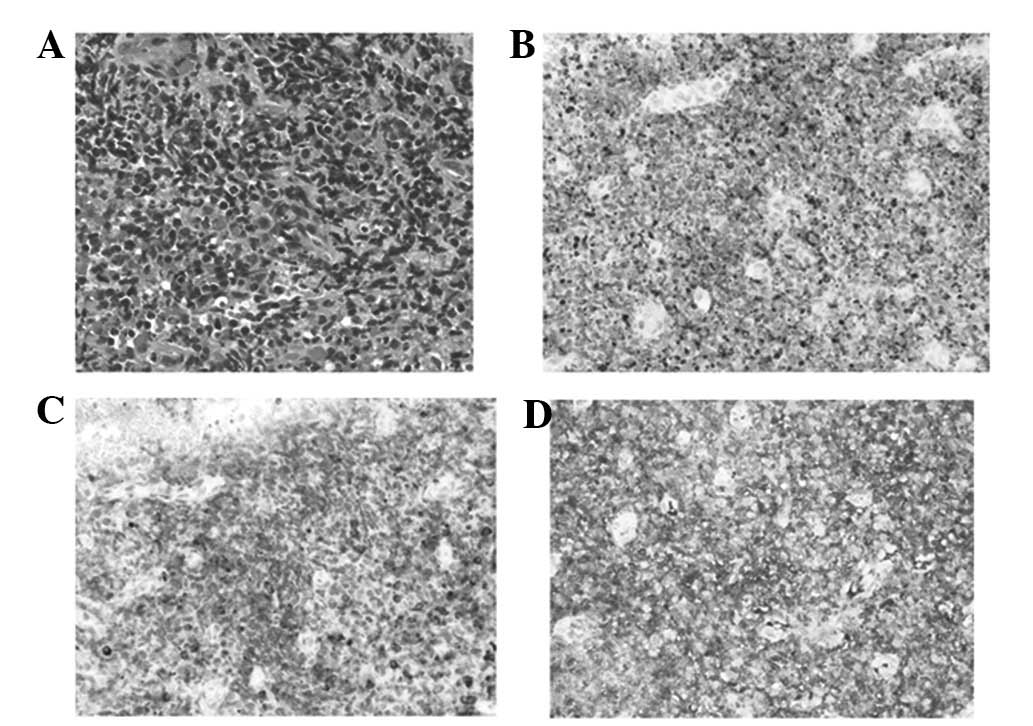
(TBB) specimen showed large atypical cells (Fig. 3). Immunohistochemical staining was
positive for CD20 and CD79a and negative for CD3 and CD10. The
cells were weakly positive for IgM and the κ/λ ratio was high. The
patient was diagnosed with a high-grade transformation of LPL
involving the main carina.
The patient was treated with 2 courses of DeVIC
therapy (dexamethasone, etoposide, ifosfamide and carboplatin), and
achieved a complete response (CR), as confirmed by FDG-PET.
Thereafter, the patient underwent an allogeneic stem cell
transplantation and is currently (15 months post-treatment) alive
without recurrence.
Discussion
The present study describes a rare case of
transformed LPL with carinal involvement. Although ML frequently
involves the intrathoracic organs, endobronchial involvement (EBI)
in NHL is rare, even in patients with advanced disease (3,4). To
the best of our knowledge, a high-grade transformation of LPL
detected as an endobronchial tumor has not previously been
reported.
LPL is classified as a low-grade lymphoma and
constitutes <5% of all NHLs. LPL occurs in older adults, usually
involving the bone marrow, lymph nodes and spleen, while extranodal
involvement and a leukemic phase are rare (5). LPL tumors consist of a diffuse
arrangement of small B lymphocytes with variable degrees of
plasmacytoid differentiation. The clinical presentation usually
consists of a disseminated disease, with >20% of patients having
monoclonal IgM paraproteinemia and hyperviscosity symptoms
(5). The median survival of
patients with LPL is 50–60 months due to the transformation to
large cell lymphoma. The primary LPL lesion in the present patient
was in the bone marrow, and IgM paraproteinemia was detected. The
transformation to large cell lymphoma occurred ∼48 months after the
initial diagnosis of LPL. With the exception of the age of onset of
the LPL and EBI, the patient had a typical clinical course.
Endobronchial lymphomas have been classified into 2
types; diffuse submucosal infiltrations in the presence of intra-
and extra-thoracic lymphoma (type I), and central airway
involvement due to a solitary mass in the absence of
clinically-apparent systemic lymphoma (type II) (6,7). In
Japan, however, endobronchial lymphomas have been classified into 3
types, characterized by a raised tumor mass (type I), multiple
submucosal nodules (type II) and diffuse submucosal infiltration
(type III) (2). The present patient
may be classified endoscopically as type II according to the former
classification system and as type I according to the latter.
Although the more common type of EBI accompanying NHL differs in
various studies (2,6,7), this
may be due to the varying characteristics of NHL.
Five mechanisms of endobronchial metastasis have
been proposed: i) direct bronchial invasion of a parenchymal mass;
ii) direct bronchial invasion of a mediastinal mass; iii) lymphatic
spread to peribronchial connective tissues; iv) transbronchial
aspiration of tumor emboli; and v) direct hematogenous metastasis
(8). The most common mechanisms
regarding endobronchial NHLs are mechanisms ii) and iii) (8). Chest CT scans in the present patient
showed that the endobronchial tumor was from mediastinal
lymphadenopathy, suggestive of mechanism ii).
The majority of EBIs occur in patients with systemic
or relapsed/refractory disease, and are more frequent in patients
with Hodgkin’s disease than in those with NHL (2,7).
Although the most frequent EBI loci observed in NHL patients
differ, the main and lobar bronchi are the most common sites
(2,4,7). The
most common histological subtypes of endobronchial lymphoma are
considered to be bronchus-associated lymphoid tissue lymphoma and
diffuse B-cell lymphoma (6,7,9),
although too few patients have been assessed to draw definitive
conclusions. Further investigations of EBI accompanying NHL are
warranted.
Autofluorescence bronchoscopy is an important tool
in the early detection of preinvasive bronchial lesions, including
squamous dysplasia, carcinoma in situ and early hilar lung
carcinoma (10). A new type of
autofluorescence bronchoscopy, AFI, has been revealed to more
precisely distinguish preinvasive bronchial lesions and bronchitis
(10). The AFI examination of the
present patient demonstrated that the exophytic tumor and its
surrounding areas were magenta in color. Since the mucosal surface
surrounding the tumor was endoscopically smooth, submucosal
invasion of the lymphoma was suspected. However, as only a few
studies to date have described the use of AFI in patients with
endobronchial lymphoma (11,12),
further studies are necessary to assess the usefulness of AFI in ML
patients with EBI.
In conclusion, the present study describes a rare
case of LPL involving the main carina. Bronchoscopic examinations
with TBB and AFI led to a diagnosis of a transformation to large
cell lymphoma. These findings may provide further insight into
endobronchial lymphoma and, particularly in patients with
refractory low-grade lymphoma, emphasize the importance of
histological examination of newly developed lesions.
References
|
1.
|
Banks DE, Castellan RM and Hendrick DJ:
Lymphocytic lymphoma recurring in multiple endobronchial sites.
Thorax. 35:796–797. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Tanigawa S, Hosokawa Y, Abe M, et al:
Classification and clinical features of endobronchial involvement
of non-Hodgkin’s lymphoma. JJSRE. 14:15–21. 1992.(In Japanese).
|
|
3.
|
Fujimoto Y, Nomura K, Shimizu D, et al:
Pulmonary relapse of non-Hodgkin’s lymphoma in bilateral upper
lobes. Intern Med. 45:971–973. 2006.
|
|
4.
|
Eng J and Sabanathan S: Endobronchial
non-Hodgkin’s lymphoma. J Cardiovasc Surg (Torino). 34:351–354.
1993.
|
|
5.
|
Vitolo U, Ferreri AJ and Montoto S:
Lymphoplasmacytic lymphoma-Waldenstrom’s macroglobulinemia. Crit
Rev Oncol Hematol. 67:172–185. 2008.
|
|
6.
|
Rose RM, Grigas D, Strattemeir E, Harris
NL and Linggood RM: Endobronchial involvement with non-Hodgkin's
lymphoma. A clinical-radiologic analysis. Cancer. 57:1750–1755.
1986.
|
|
7.
|
Solomonov A, Zuckerman T, Goralnik L,
Ben-Arieh Y, Rowe JM and Yigla M: Non-Hodgkin’s lymphoma presenting
as an endobronchial tumor: report of eight cases and literature
review. Am J Hematol. 83:416–419. 2008.
|
|
8.
|
Kilgore TL and Chasen MH: Endobronchial
non-Hodgkin’s lymphoma. Chest. 84:58–61. 1983.
|
|
9.
|
Gómez-Román JJ, Pérez-Montes R,
Pérez-Expósito MA, Richard C, Baro J and Val-Bernal JF: Primary
lymphoplasmacytoid lymphoma of the trachea with immunoglobulin G
paraprotein. Pathol Int. 49:1100–1104. 1999.PubMed/NCBI
|
|
10.
|
Chiyo M, Shibuya K, Hoshino H, et al:
Effective detection of bronchial preinvasive lesions by a new
autofluorescence imaging bronchovideoscope system. Lung Cancer.
48:307–313. 2005. View Article : Google Scholar
|
|
11.
|
Sato C, Suzuki H, Watanabe M, Kojima K,
Tsuchida F and Takeda H: Spontaneous regression of
mucosa-associated lymphoid tissue lymphoma of the lung. Nihon
Kokyuki Gakkai Zasshi. 48:677–682. 2010.(In Japanese).
|
|
12.
|
Ueda Y, Matsuo K, Tsushima M, Fujiwara K,
Yonei T and Sato T: A case showing tracheal origin of MALT
(mucosa-associated lymphoid tissue) lymphoma that could be observed
with autofluoresence imaging bronchovideoscope before and after
treatment. JJSRE. 32:162–168. 2010.(In Japanese).
|