Introduction
Brain metastases are a common type of intracranial
malignancy derived from the transfer of tumor cells outside the
central nervous system to the brain tissue. In a study by
Lu-Emerson and Eichler, brain metastases were reported to occur in
∼20–40% of cancer patients, with an onset age of 50 to
70-years-old. The study reported that 1/3–1/2 of cancer patients
died as a direct result of brain metastases (1). The clinical manifestations of brain
metastasis often insidiously develop within a few weeks, with only
1/4 of patients developing manifestations suddenly. Whole brain
radiation therapy (WBRT) is suitable for multiple brain metastases,
and a previous study has shown that 80% of patients who undergo
WBRT experience a good therapeutic effect. The natural course of
untreated multiple brain metastases is only one month and the
median survival after whole brain irradiation is 4–6 months
(2). The surgery is mainly
administered to patients with single brain metastases and good
bodily functions. In recent years, surgery has been gradually
replaced by stereotactic radiosurgery (SRS). SRS is able to
accurately determine the spatial location of the target metastases
and precisely converge high-energy radiation to the target tissue,
with almost no effect on the surroundings. Focused, highly-targeted
irradiation and the delivery of fractionated CyberKnife therapy is
considered to be an effective treatment for large multiple brain
metastatic tumors. Written informed consent was obtained from the
patient.
Case report
A 46-year old male smoker was admitted to the Center
for Tumor Treatment of the People’s Liberation Army 107th Hospital
(Yantai, Shandong, China) in April 2010. The patient was suffering
with a long-term cough and pain in the chest and back. Using X-ray,
a mass was detected in the right lobe of the lung. Enhanced
computed tomography (CT) scans confirmed the suspicion of lung
cancer and also identified a right adrenal metastasis. The tumor
was clinically staged as T2N0M1 (stage IV). The patient underwent
conformal radiotherapy with 66 Gy/33 F combined with three cycles
of cisplatin and vinorelbine chemotherapy. A good partial remission
was achieved after the administration.
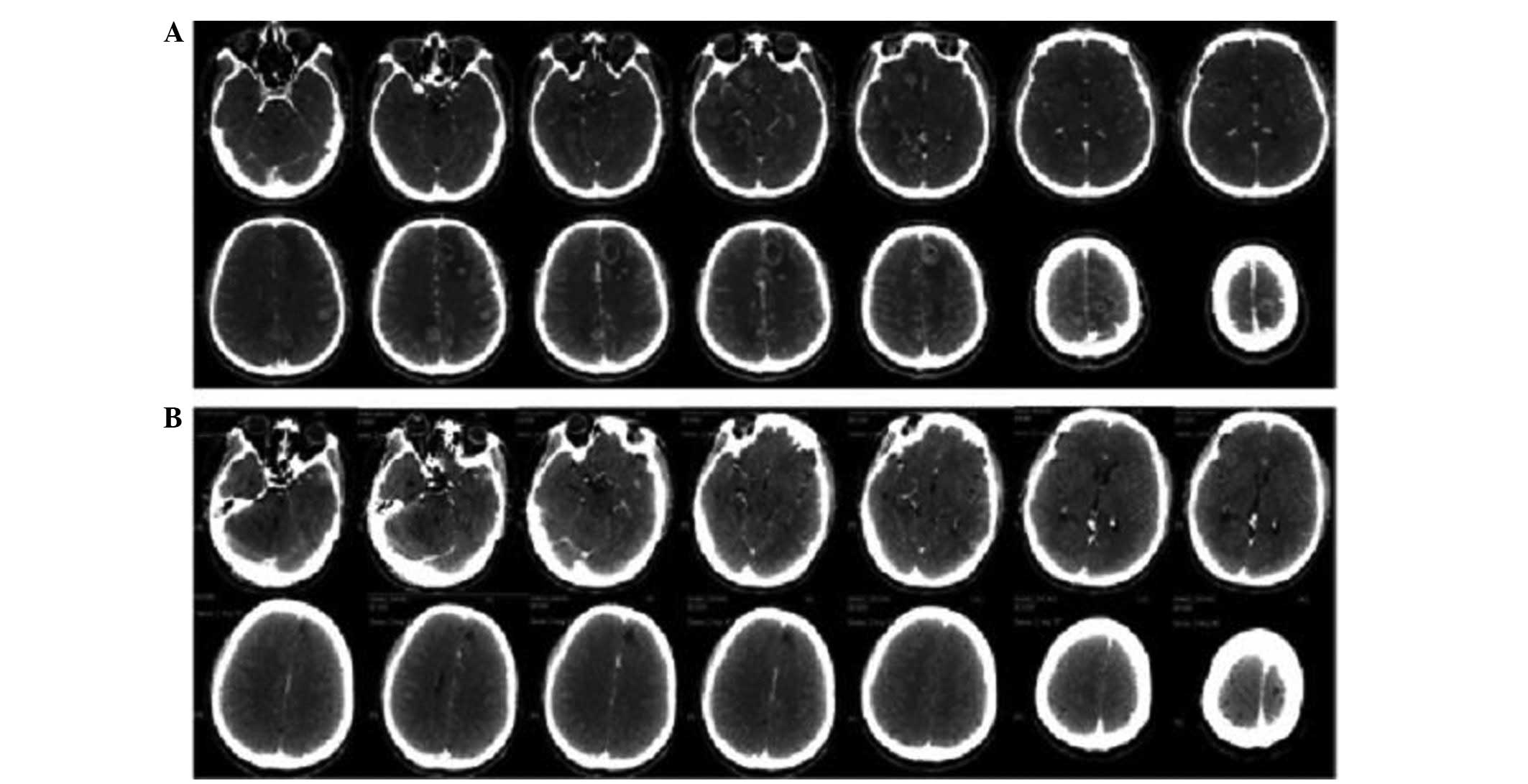
Six months after the initial diagnosis, the patient
experienced severe headaches with frequent vomiting and blurred
vision. An enhanced CT scan of the brain revealed abnormalities
with a double-dosing of intravenous contrast, which demonstrated
that there were no less than 24 lesions scattered in the whole
brain, including the frontal, parietal and temporal lobes and the
brainstem (Fig. 1A). A discussion
was held by experts in the field with regard to the multiple brain
metastases, which were highly suspicious and stemmed from the
primary lung cancer, and surgical treatment was consequently
rejected. The patient received treatment using the CyberKnife
Robotic Radiosurgery System on December 4, 2010, using an 80%
prescription dose line covering 95% of the planning target volume.
A total of 22 Gy was delivered in 3 fractions to the brain
metastases. The modified conformity index was 1.41. During regular
follow-up examinations, the headache symptoms were found to be
markedly alleviated, the vomiting and blurred vision were slowly
eased and there were no side effects from the radiation. The tumor
shrank within 1 month and had completely disappeared within 3
months (Fig. 1B). The patient
succumbed to hepatic metastases 1 year after the CyberKnife
therapy.
Discussion
Brain metastases from systemic cancer are the most
common type of intracranial neoplasm in adults, being almost 10
times more common than primary malignant brain tumors, which cause
a significant burden on the management of patients with advanced
cancer (1). The lungs represent one
of the most frequent sources of metastases to the brain, with a
probability of (36–64%) (3).
Symptoms suffered by the patients include headaches, epilepsy,
focal weakness, numbness or changes in mental status. The prognosis
of patients with brain metastases is not optimistic and the median
survival time is ∼1–2 months if left untreated. The 1-year survival
rate has been recorded as 10.4% (4,5). The
treatment of metastatic brain tumors is complex; not only due to
being able to provide local control and improve neurological
function, but also due to factors such as age, performance and
systemic disease status and the size, volume, location and number
of metastases at presentation (1).
There have been a number of studies describing metastatic brain
tumors being successfully eliminated by surgery, chemotherapy, WBRT
or a combination of modalities (6,7). These
modalities have prolonged the survival time of patients and
improved the neurological outcome. Craniotomy, which allows
immediate relief of symptoms of intracranial hypertension, a
reduction of focal neurological deficits and seizures, or use of a
rapid steroid taper, has become the preferred therapy for
metastatic brain tumors (8). The
majority of studies support surgery as a suitable treatment for
patients with single brain metastases with a mean maximum diameter
of 3.43±0.74 cm, but not for patients with multiple brain
metastases due to more frequent leptomeningeal dissemination
following craniotomy (9,10). Furthermore, the mortality rate of
patients who undergo surgery for brain metastases is ∼2- to 4-fold
higher than that of patients with primary brain tumors (11).
WBRT has been widely used for the management of
brain metastases, particularly multiple brain metastases, for
decades, as it results in the rapid improvement of neurological
symptoms and prolongs survival (12). However, radiation- induced dementia
is a well-known side effect, although it does increase the median
survival time to 4–6 months (2).
SRS, particularly γ-Knife surgery (GKS), affords excellent local
tumor control for between 1 and 10 brain metastases (13,14).
Grandhi et al (15) assessed
the clinical outcomes of 61 patients with ≥10 brain metastases who
underwent SRS at the Leksell γ-Knife Perfexion (LGK PFX) unit
(University of Pittsburgh Cancer Institute, Pittsburg) for the
treatment of 806 tumors (mean, 13.2 lesions). Of the total treated
tumor volume, actuarial freedom from local tumor progression was
94.1% at 3 months after LGK PFX surgery, 90.5% at 6 months and
58.3% at 12 months. It appeared that SRS was conducive to a prompt
response and good outcome. However, SRS has not been applied easily
for multiple large brain metastases due to serious medical
conditions, with increased intracranial pressure or insufficient
marginal dose, although it has been accepted as a general treatment
method for brain metastasis since 1975 (16).
CyberKnife is a robotic radiosurgery system with a
linear particle accelerator (linac), which is coupled with
real-time imaging to track and compensate for the patient’s or
target’s motion. As a relatively non-invasive treatment modality,
CyberKnife demonstrates certain benefits, including a more accurate
target localization and improved dose delivery for the management
of metastatic brain tumors that allows higher biologically
effective dose delivery without increased incidence of toxicity.
Nishizaki et al (17)
produced a retrospective study on 71 patients with 148 metastatic
brain lesions who underwent CyberKnife therapy. A total of 31
patients had multiple lesions (range, 2–7) at the initial
treatment, and 86 lesions achieved local control. The median
survival time was 56 weeks. Overall, 40 patients succumbed to
progressive brain metastases, primary cancers, extracranial
metastases and other diseases, including infection or gastric
bleeding. No patient succumbed as a result of intracranial disease
from new metastases.
However, few studies have demonstrated a marked
change in the typical cohort of patients with 1 to ≥20 brain
metastases. In the present case, the 24 brain metastases
(originating from lung cancer), which were scattered throughout the
whole of the brain, were completely resolved within 3 months
following CyberKnife radiosurgery. No opportunistic recurrence or
metastasis occurred during the follow-up, as revealed by CT imaging
studies. Although the patient succumbed to liver metastasis, the
survival results were comparable to those of published studies. Kim
et al (18) conducted a
study in 26 patients with ≥10 brain metastases; following GKS the
median survival was 34 weeks. Grandhi et al (15) showed that the median survival time
of patients with ≥14 brain metastases after LGK PFX treatment was 3
months compared to 6 months in those with <14 lesions. The
survival time of the present study is similar to that cited in the
study by Nishiazki et al, which revealed a survival time of
∼56 weeks when the patients were treated with CyberKnife (17).
In the present case, the results for the treatment
of multiple brain metastases after CyberKnife surgery with a 7–8 Gy
marginal dose was promising. CyberKnife for metastatic brain tumors
is an effective and safe method for reducing the marginal dose
prescribed for multiple brain metastases and for minimizing the
radiation-related neurotoxicities. In conclusion, CyberKnife, a
focused, highly-targeted radiosurgery and fractionated radiotherapy
is particularly useful for multiple brain metastases. CyberKnife
provides the advantage of the management of local recurrence and a
tolerable complication rate. Although the treatment of brain
metastases has been performed with CyberKnife, the clinical
significance and optimal dose fractionation scheme require further
investigation.
Acknowledgements
This study was supported by grants
from the National Special Issue of the Ministry of Health of China
(No. 2009BX042).
References
|
1.
|
Lu-Emerson C and Eichler AF: Brain
metastases. Continuum; Minneap Minn: 18. pp. 295–311. 2012
|
|
2.
|
DeAngelis LM, Mandell LR, Thaler HT,
Kimmel DW, Galicich JH, Fuks Z and Posner JB: The role of
postoperative radiotherapy after resection of single brain
metastases. Neurosurgery. 24:798–805. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Soffietti R, Ducati A and Rudà R: Brain
metastases. Handb Clin Neurol. 105:747–55. 2012. View Article : Google Scholar
|
|
4.
|
Shimamoto S and Inoue T, Shiomi H, Sumida
I, Yamada Y, Tanaka E and Inoue T: CyberKnife stereotactic
irradiation for metastatic brain tumors. Radiat Med. 20:299–304.
2002.PubMed/NCBI
|
|
5.
|
Smedby KE, Brandt L, Bäcklund Ml and
Blomqvist P: Brain metastases admissions in Sweden between 1987 and
2006. Br J Cancer. 101:1919–1924. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Bellati F, Palaia I, Gasparri ML, Musella
A and Panici PB: First case of isolated vaginal metastasis from
breast cancer treated by surgery. BMC Cancer. 12:4792012.
View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Khan E, Ismail S and Muirhead R: Incidence
of symptomatic brain metastasis following radical radiotherapy for
non-small cell lung cancer: is there a role for prophylactic
cranial irradiation? Br J Radiol. 85:1546–1550. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Vogelbaum MA and Suh JH: Resectable brain
metastases. J Clin Oncol. 24:1289–1294. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Bindal RK, Sawaya R, Leavens ME and Lee
JJ: Surgical treatment of multiple brain metastases. J Neurosurg.
79:210–216. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Siomin VE, Vogelbaum MA, Kanner AA, Lee
SY, Suh JH and Barnett GH: Posterior fossa metastases: risk of
leptomeningeal disease when treated with stereotactic radiosurgery
compared to surgery. J Neurooncol. 67:115–121. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Lassen B, Helseth E, Rønning P, Scheie D,
Johannesen TB, Mæhlen J, Langmoen IA and Meling TR: Surgical
mortality at 30 days and complications leading to recraniotomy in
2630 consecutive craniotomies for intracranial tumors.
Neurosurgery. 68:1259–1269. 2011.PubMed/NCBI
|
|
12.
|
Mayahara H, Sumi M, Ito Y, Sekii S,
Takahashi K, Inaba K, Kuroda Y, Murakami N, Morota M and Itami J:
Effect of chemotherapy on survival after whole brain radiation
therapy for brain metastases: a single-center retrospective
analysis. J Cancer Res Clin Oncol. 138:1239–1247. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Rades D, Kueter JD, Veninga T, Gliemroth J
and Schild SE: Whole brain radiotherapy plus stereotactic
radiosurgery (WBRT+SRS) versus surgery plus whole brain
radiotherapy (OP+WBRT) for 1–3 brain metastases: results of a
matchedpair analysis. Eur J Cancer. 45:400–404. 2009.
|
|
14.
|
Serizawa T, Hirai T, Nagano O, Higuchi Y,
Matsuda S, Ono J and Saeki N: Gamma knife surgery for 1–10 brain
metastases without prophylactic whole-brain radiation therapy:
analysis of cases meeting the Japanese prospective multi-institute
study (JLGK0901) inclusion criteria. J Neurooncol. 98:163–167.
2010.
|
|
15.
|
Grandhi R, Kondziolka D, Panczykowski D,
Monaco EA III, Kano H, Niranjan A, Flickinger JC and Lunsford LD:
Stereotactic radiosurgery using the Leksell Gamma Knife Perfexion
unit in the management of patients with 10 or more brain
metastases. J Neurosurg. 117:237–245. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Han JH, Kim DG, Kim CY, Chung HT and Jung
HW: Stereotactic radiosurgery for large brain metastases. Prog
Neurol Surg. 25:248–260. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Nishizaki T, Saito K, Jimi Y, Harada N,
Kajiwara K, Nomura S, Ishihara H, Yoshikawa K, Yoneda H, Suzuki M
and Gibbs IC: The role of cyberknife radiosurgery/radiotherapy for
brain metastases of multiple or large-size tumors. Minim Invasive
Neurosurg. 49:203–209. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Kim CH, Im YS, Nam DH, Park K, Kim JH and
Lee JI: Gamma knife radiosurgery for ten or more brain metastases.
J Korean Neurosurg Soc. 44:358–363. 2008. View Article : Google Scholar : PubMed/NCBI
|