Introduction
As an established therapeutic method, ultrasound
(US) is used for bone fracture healing, hyperthermia and the
ablation of solid tumors (1).
Furthermore, in this newly emerging field, US-mediated microbubble
destruction, a noninvasive approach, has been shown to possess
significant potential to increase the permeability of cell
membranes and tissues to various substances. Since US-mediated
microbubble destruction is able to reversibly disrupt biological
barriers, particularly cell membranes, large quantities of
molecules may then be delivered into tumor cells, particularly
drug-resistant cells. The mechanism by which this occurs is
considered to be sonoporation, resulting from oscillations of the
gas bubbles in the media, which cause cavitation close to the cell
surface and subsequent membrane disruption that allows increased
drug internalization (2). It has
been demonstrated that intracellular uptake is greatly enhanced by
diagnostic microbubbles used for US imaging (3–5). At
particular ultrasonic frequencies, microbubbles have been shown to
greatly enhance transient sonoporation (6). These microbubbles, oscillating in the
presence of US, create localized shear stress or ‘microstreaming’
or they may expand and collapse (‘transient cavitation’) to create
intense local heating and pressure (7). This type of transient cavitation
effect is considered to occur more at low frequencies (8). Schlicher et al demonstrated
transient pores (<28 nm diameter) in the plasma membrane of
cells, following exposure to low frequency US (24 kHz) (9).
Prostate cancer (PCa) is one of the most common
types of cancer among the male population of Western countries,
second only to skin cancer (10,11).
Hormonal therapy allows long-lasting and effective control of
cancer-related symptoms at advanced stages. However, in almost all
patients with metastatic PCa, the disease progresses when it
becomes castration-resistant (CRPC) (12). At that stage, second-line endocrinal
therapy and chemotherapy should be administered. In order to
maintain sufficient doses of chemotherapeutic drugs in the
cancerous tissue, all tissues are exposed to various concentrations
of cytotoxic drugs during systemic administration. Combination
therapy is used to optimize anticancer efficacy and reduce the
toxicity and side-effects of drugs upon systemic administration. US
combined with microbubbles (UM) is able to enhance the
intracellular uptake of the cytotoxic drugs by the tumor cells,
particularly the drug-resistant cells.
Sonoporation, electroporation, microinjection and
laser irradiation are all able to enhance the transmembrane
delivery of therapeutic molecules. However, sonoporation is
considered to be a ‘gentle’ technique. Non-inertial cavitation is
generated by the alternate growth and shrinkage caused by contrast
agents (CAs) oscillating, which occurs at low acoustic pressures.
Further complex non-linear interactions appear when the ultrasonic
pressure reaches a certain threshold, and at that time the
microbubble explodes and pores form, which enhances the
intracellular uptake or kills the cells. Overall, inertial
cavitation occurs at relatively high pressure amplitudes and CAs
contract and collapse ‘violently’ (13). Khanna et al, who performed
the first notable study, used US waves to make blood cells release
hemoglobin (14). The study into US
waves by Kinoshita and Hynynen showed that increasing sonoporation
typically lessened cellular viability (15). However, Rodamporn et al
concluded that improved conditions reduced the loss of viability
while maintaining high transfection rates (16). To the best of our knowledge, the
present study is the first to state that low-frequency and
low-energy US are able to reduce the loss of viability while
maintaining high sonoporation in DU145 PCa cells.
Materials and methods
Cell culture
DU145 cells, a human PCa cell line, were obtained
from the Cell Bank of the Chinese Academy of Sciences (Shanghai,
China) and used to study the chemotherapy response at the cellular
level. The cells were maintained in Dulbecco’s modified Eagles
medium (DMEM; Gibco, Grand Island, NY, USA) supplemented with 10%
heat-inactivated fetal bovine serum (FBS; Invitrogen, Carlsbad, CA,
USA) in 5% CO2 humidified air at 37°C. This study was
approved by the ethics committee of Shanghai Jiao Tong University
Affiliated Sixth People’s Hospital (Shanghai, China).
Drugs
Mitoxantrone HCl (MIT; Sigma Aldrich, St. Louis, MO,
USA) was dissolved in phosphate-buffered saline (PBS) at a
concentration of 10 nM and the solution was stored at −20°C until
use. MIT, which was approved by the FDA for hormone refractory PCa
(HRPC) as a palliative treatment in 1996, is a cell cycle
nonspecific agent that inhibits nucleic acid synthesis, leading to
cell death. The dose limiting toxic effects are bone marrow
suppression, leukopenia and thrombocytopenia.
US apparatus
FS-450 ultrasonic processing (Shanghai Institute of
Ultrasound in Medicine, Shanghai, China) with a SonoVue™
microbubble echo-contrast agent (Bracco SpA, Milan, Italy) was
employed as previously described (17). The US irradiation conditions were as
follows: frequency, 21 kHz; power density, 0.113 W/cm2;
instrument exposure time, 2 min at a duty cycle of 70% (i.e., 7 sec
‘on’ time and 3 sec ‘off’ time); and a valid treatment time of 84
sec.
Treatment
The cell suspensions were divided into four
treatment groups: Group A, non-treated (control); group B, UM
treatment; group C, MIT treatment; and group D, combined treatment
with MIT and UM (MIT+UM). DU145 cells (1×106 in 1 ml of
medium) were transferred into 1.5-ml polystyrene test tubes, the
diameter of which was the same as the probe being used. MIT (10
nmol) was added to groups C and D.
Analysis of cell proliferation
Immediately following exposure to US, the cells were
added to a 96-well plate at a density of 5,000 cells/well and
incubated with 5% CO2 at 37°C. Subsequent to 24 h, 50
μl dilution medium containing 10 μl MTT solution (5
mg/ml) was used to replace the medium, and the plate was incubated
for another 4 h until the liquid was removed. The formazan crystals
that formed were dissolved with 150 μl DMSO. Following
agitation for 5 min, the absorbance of each well at a test
wavelength of 570 nm was measured with a microculture plate reader
(Bio-Tek, Winooski, VT, USA). The percentage cell viability was
calculated as ODexposed / ODcontrol ×
100.
Clonogenic assay
The long-term proliferation rate of the treated
cells was measured by plate clonogenic assays. Subsequent to
therapy, 200 cells/well were seeded into a 12-well plate, then
incubated for two weeks to form colonies prior to fixation in 70%
ethanol, staining with crystal violet and counting.
Cell migration assay
The transwell apparatus (Costar, Cambridge, MA, USA)
was used for the cell migration assays. There were 1×104
cells in 100 μl DMEM without FBS in the the upper
polycarbonate membrane insert (pore size, 8 μm), which was
precoated with 24 mg/ml Matrigel (R&D Systems, Minneapolis, MN,
USA), and there was 600 ml DMEM with 10% FBS in the lower
chamber.
Following incubation for 8 h at 37°C in a 5%
CO2 atmosphere, the upper cells were removed with a
cotton swab and the cells adhering to the lower surface were fixed
with 95% alcohol for 15–20 min and stained with crystal violet for
15 min. Finally, the total number of migratory cells was counted
with a microscope.
Analysis of DU145 cell permeability using
calcein with or without UM
Calcein was used as the permeability tracer to
further support our hypothesis that UM increases the absorption of
drugs. Calcein (1 μl, 25 mg/ml; Sigma Aldrich) was added to
each sample just prior to exposure. Following incubation for 1 h at
37°C, the samples were washed three times with PBS, then 10,000
cells/sample were detected by flow cytometry using the CellQuest
Pro software program (BD Biosciences, Franklin Lakes, NJ, USA) with
an excitation wavelength of 492 nm and an emission wavelength of
518 nm (18). The results are
expressed as the percentage of positive cells and fluorescence
intensity with regard to the whole cell population, including any
dead cells.
Statistical analysis
Data are expressed as the mean ± SEM. The
differences among the groups were analyzed using Student’s t-test
or one-way ANOVA. P<0.05 was considered to indicate a
statistically significant difference.
Results
Increasing the efficacy of chemotherapy
(tests of cell proliferation)
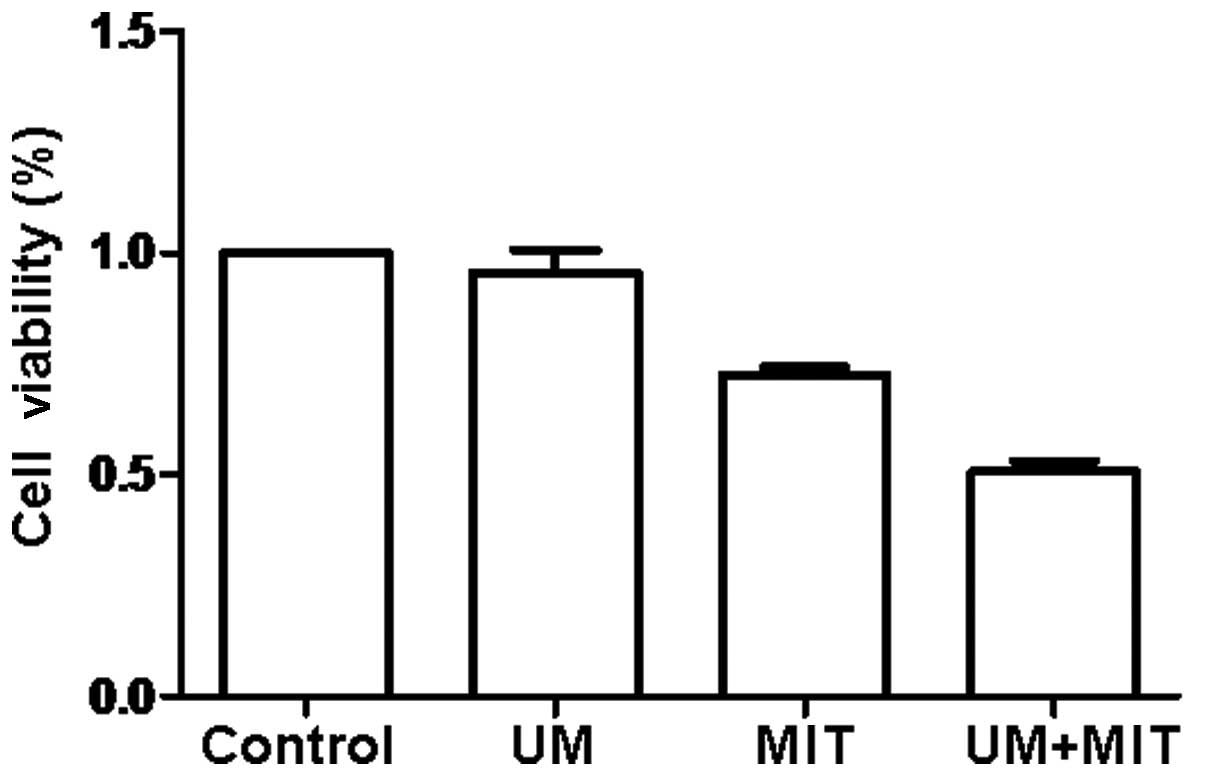
In order to examine the hypothesis that UM is able
to enhance the efficacy of chemotherapy, the cytotoxicity on each
group of the cells from the PCa cell line DU145 was evaluated using
the MTT assay. Fig. 1 shows the
results following incubation for 24 h, which indicated that the
MIT+UM group had clear cytotoxicity compared with the other three
groups. As shown in Fig. 1,
compared with the controls, the cell viability of the UM group did
not decrease (P>0.05), although the cell viability of the MIT
(72.3%) and MIT+UM (50.7%) groups was significantly decreased
(P<0.05). Compared with the MIT group, the cell viability of the
MIT+UM group was significantly decreased (P<0.05).
Viability of the reversibly permeabilized
cells
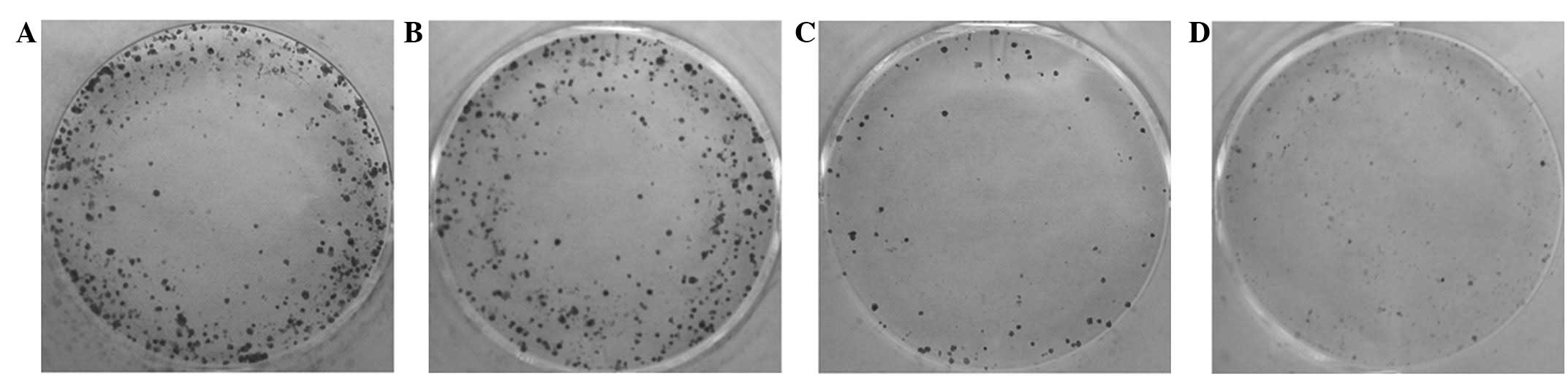
The long-term effects of MIT and UM, alone or in
combination, on the DU145 cells were evaluated with the colony
formation assay. The numbers of cell colonies formed are shown in
Fig. 2. The clonogenicity of the
cells exposed to UM (95.7±7.1) was lower compared with the
untreated cells (102.0±6.6) (Fig.
2). By contrast, the cells exposed to MIT (45.0±6.0) and MIT
combined with UM (18.7±5.5) had significantly lower colony forming
numbers (P<0.05).
Effects on the migration of the DU145
cells
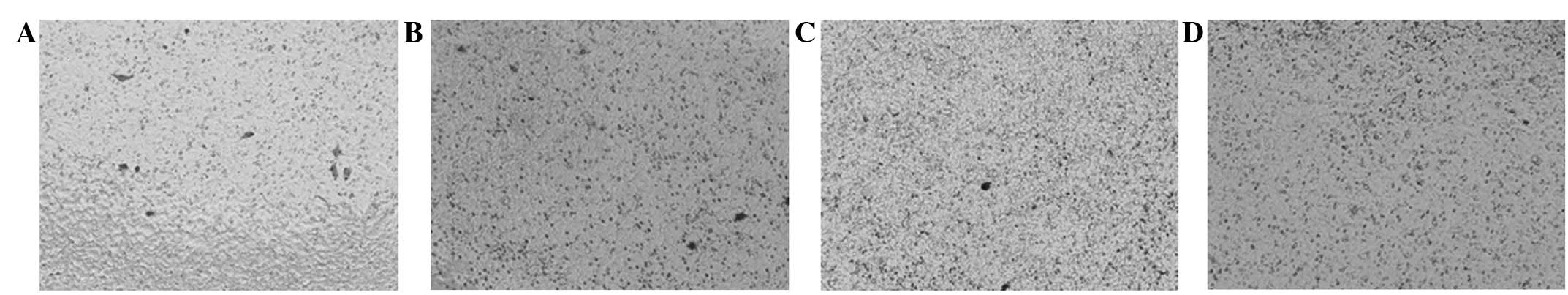
The cell migration ability was assayed using the
transwell apparatus in order to investigate the long-term
biological effects of each treatment on the DU145 cells. The
transmembrane cells of each group are shown in Fig. 3. Compared with the control group,
the invasive ability of the DU145 cells in the UM (45.3±6.5), MIT
(17.7±7.1) and MIT+UM (2.7±2.5) groups was significantly decreased
(all P<0.05; Fig. 3). The
results indicated that UM may enhance the ability of MIT in
decreasing the colony forming ability of cells.
Analysis of sonoporation efficacy
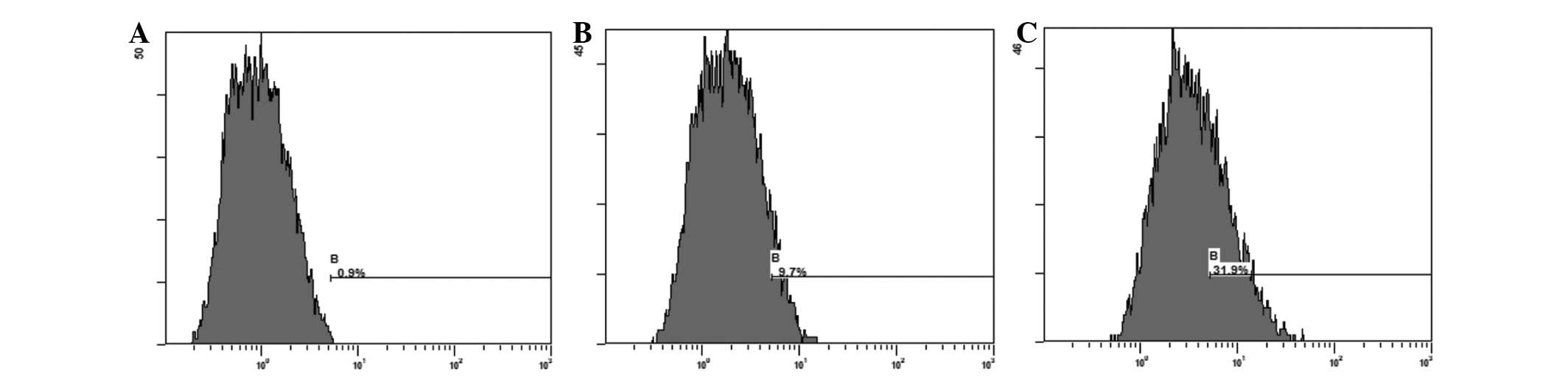
Fig. 4 shows the
percentage of intracellular calcein (a molecular fluorescent probe;
MW, 622.53) induced by sonoporation. The cells treated with UM
(31.26±3.34%) showed an increased percentage of
fluorescence-positive cells compared with the control cells
(9.74±2.55%) following incubation for 1 h (P<0.05).
Discussion
Numerous side-effects follow effective MIT therapy.
Combination therapy is used to optimize anticancer efficacy and
reduce the toxicity and side-effects of drugs upon systemic
administration. With its noninvasive and steerable nature, US is a
useful tool in combined treatment with anti-cancer agents.
Sonoporation has been associated with enhanced drug delivery in
chemotherapy in primary studies concerning cutaneous melanoma
(19,20) lymphoma (21) and oral cancer (22,23).
It appears that there have been few studies focusing on PCa and
combination therapy, and only a small number on the enhancement of
permeability in vivo (24).
The present study is the first to investigate this
strategy in PCa. The results revealed the successful enhancement of
transmembrane MIT transport with the aid of UM, while
simultaneously avoiding significantly affecting cell viability.
This low frequency and low power-based method did not allow the
microbubbles to make contact with the cell membrane immediately and
did not exert significant additional stress on the cell membrane to
cause death-induced pores. Notably, the study demonstrated for the
first time that combining these strategies facilitated the uptake
of MIT by DU145 cells in a number of ways. This alternative
low-cost device may offer some quality of life improvement for
patients, rather than other more expensive techniques, which may be
welcomed by individuals in low-level income brackets. Further
studies to gain a greater understanding of the mechanisms should be
performed prior to this therapeutic method being used in clinical
practice, to identify the most appropriate UM parameters that
increase the efficacy of all types of therapeutic agents in
vivo and are safe for normal tissues. The present study
represents a first step towards combination therapy for PCa.
Acknowledgements
The present study was supported by the
major infrastructure projects of Shanghai Science and Technology
under grant No. 10JC1412600 and by the National Natural Science
Foundation of China (project number, 81271597).
References
|
1.
|
Hensel K, Mienkina MP and Schmitz G:
Analysis of ultrasound fields in cell culture wells for in vitro
ultrasound therapy experiments. Ultrasound Med Biol. 37:2105–2115.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Husseini GA and Pitt WG: The use of
ultrasound and micelles in cancer treatment. J Nanosci Nanotechnol.
8:2205–2215. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Casey G, Cashman JP, Morrissey D, et al:
Sonoporation mediated immunogene therapy of solid tumors.
Ultrasound Med Biol. 36:430–440. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Qin S, Caskey CF and Ferrara KW:
Ultrasound contrast microbubbles in imaging and therapy: physical
principles and engineering. Phys Med Biol. 54:R27–R57. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
van Wamel A, Kooiman K, Harteveld M, et
al: Vibrating micro-bubbles poking individual cells: drug transfer
into cells via sonoporation. J Control Release. 112:149–155.
2006.PubMed/NCBI
|
|
6.
|
Ohl CD, Arora M, lkink R, de Jong N,
Versluis M, Delius M and Lohse D: Sonoporation from jetting
cavitation bubbles. Biophys J. 91:4285–4295. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Juffermans LJ, van Dijk A, Jongenelen CA,
Drukarch B, Reijerkerk A, de Vries HE, Kamp O and Musters RJ:
Ultrasound and microbubble-induced intra- and intercellular
bioeffects in primary endothelial cells. Ultrasound Med Biol.
35:1917–1927. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Hoskins P, Thrush A, Martin K and
Whittingam T: Diagnostic Ultrasound: Physics and Equipment. 2nd
Edition. Cambridge University Press; New York, NY: 2010
|
|
9.
|
Schlicher RK, Radhakrishna H, Tolentino
TP, Apkarian RP, Zarnitsyn V and Prausnitz MR: Mechanism of
intracellular delivery by acoustic cavitation. Ultrasound Med Biol.
32:915–924. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Jemal A, Siegel R, Xu J and Ward E: Cancer
statistics, 2010. CA Cancer J Clin. 60:277–300. 2010. View Article : Google Scholar
|
|
11.
|
Siegel R, Ward E, Brawley O and Jemal A:
Cancer statistics, 2011: the impact of eliminating socioeconomic
and racial disparities on premature cancer deaths. CA Cancer J
Clin. 61:212–236. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Carles J, Castellano D, Climent MÁ, Maroto
P, Medina R and Alcaraz A: Castration-resistant metastatic prostate
cancer: current status and treatment possibilities. Clin Transl
Oncol. 14:169–176. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Mellott AJ, Forrest ML and Detamore MS:
Physical non-viral gene delivery methods for tissue engineering.
Ann Biomed Eng. 41:446–468. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Khanna S, Amso NN, Paynter SJ and Coakley
WT: Contrast agent bubble and erythrocyte behavior in a 1.5-MHz
standing ultrasound wave. Ultrasound Med Biol. 29:1463–1470. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Kinoshita M and Hynynen K: Key factors
that affect sonoporation efficiency in in vitro settings: the
importance of standing wave in sonoporation. Biochem Biophys Res
Commun. 359:860–865. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Rodamporn S, Harris NR, Beeby SP, Boltryk
RJ and Sanchez-Elsner T: HeLa cell transfection using a novel
sonoporation system. IEEE Trans Biomed Eng. 58:927–934. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Bai WK, Wu ZH, Shen E, Zhang JZ and Hu B:
The improvement of liposome-mediated transfection of pEGFP DNA into
human prostate cancer cells by combining low-frequency and
low-energy ultrasound with microbubbles. Oncol Rep. 27:475–480.
2012.PubMed/NCBI
|
|
18.
|
Hao Q, Liu Q, Wang X, Wang P, Li T and
Tong WY: Membrane damage effect of therapeutic ultrasound on
Ehrlich ascitic tumor cells. Cancer Biother Radiopharm. 24:41–48.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Lentacker I, Geers B, Demeester J, De
Smedt SC and Sanders NN: Design and evaluation of
doxorubicin-containing microbubbles for ultrasound-triggered
doxorubicin delivery: cytotoxicity and mechanisms involved. Mol
Ther. 18:101–108. 2010. View Article : Google Scholar
|
|
20.
|
Sonoda S, Tachibana K, Uchino E, et al:
Inhibition of melanoma by ultrasound-microbubble-aided drug
delivery suggests membrane permeabilization. Cancer Biol Ther.
6:1276–1283. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Yoshida T, Kondo T, Ogawa R, et al:
Combination of doxorubicin and low-intensity ultrasound causes a
synergistic enhancement in cell killing and an additive enhancement
in apoptosis induction in human lymphoma U937 cells. Cancer
Chemother Pharmacol. 61:559–567. 2008. View Article : Google Scholar
|
|
22.
|
Iwanaga K, Tominaga K, Yamamoto K, et al:
Local delivery system of cytotoxic agents to tumors by focused
sonoporation. Cancer Gene Ther. 14:354–363. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Maeda H, Tominaga K, Iwanaga K, et al:
Targeted drug delivery system for oral cancer therapy using
sonoporation. J Oral Pathol Med. 38:572–579. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Liu Y, Liu Z, Li T and Ye G: Ultrasonic
sonoporation can enhance the prostate permeability. Med Hypotheses.
74:449–451. 2010. View Article : Google Scholar : PubMed/NCBI
|