Introduction
Nasopharyngeal carcinoma (NPC) is one of the most
common malignant tumors, with its incidence rate ranking first
among head and neck cancers. In China, more than 90% of NPC cases
are pathological type III according to the World Health
Organisation (WHO) criteria, and are sensitive to radiation.
Therefore, for patients who are newly diagnosed and without
metastasis, radiotherapy is the preferred treatment (1). In the last decade, the effect of NPC
radiotherapy has been significantly improved. The local control
rate of early NPC is 70–90%, while that of T3-4 NPC is 50%
(2).
Intensity modulated radiation therapy (IMRT) is a
breakthrough in radiation oncology. It delivers a highly
concentrated dose to the target area to kill tumor cells, while
adjacent healthy tissue is unaffected, which increases the gain
ratio of radiotherapy. The local control rate of T1-3 patients is
>90%, but that of T4 patients is only ∼85%. In certain T4 NPC
patients with intracranial extension, the space between the tumor
and surrounding organs is small, so the radiation dose must be
limited in order to protect the normal tissues and organs. This can
result in local control failure and affect the survival rate
(3).
In order to improve the local control rate and
reduce distant metastasis, many clinical studies of treatment of
locally advanced NPC with radical radiotherapy and chemotherapy
have been performed. Since the results of intergroup 0099 trial
were published (4,5), the treatment strategy of NPC has been
modified significantly and concurrent chemoradiotherapy has been
used as the standard treatment of locally advanced NPC. Induction
plus concurrent chemoradiotherapy is now standard in the treatment
of NPC. A clinical phase II study has shown promising results with
improved distant metastasis-free and overall survival; the choice
of chemotherapy drugs, delivery methods and course number, however,
needs further research. The European Society for Medical Oncology
(ESMO) NPC clinical guidelines (6)
suggest that while chemotherapy is not the standard treatment for
NPC, it improved disease-free survival, suggesting that it may be
used for the treatment of locally advanced NPC.
Arterial infusion chemotherapy has the features of
high local drug concentration and a stronger effect of local tumor
toxicity with low systemic side effects. It is used in the
treatment of a variety of tumors.
The purpose of this study was to investigate the
treatment of NPC patients with intracranial extension with arterial
infusion chemotherapy. The aim was to reduce the volume of the
primary tumor and expand the spatial distance between the tumor and
vital organs. This will improve the dose distribution of IMRT and
meet the target dose requirements while protecting the brain stem
and nerve tissues. It is expected that by improving local
treatment, overall survival (OS) time will also be improved. The
aim was to find a combination providing optimal treatment for
locally advanced NPC.
Materials and methods
General information
Twelve cases of NPC were selected between March and
December 2009. All patients signed informed consent before
treatment. The study was approved by the Ethics Committee of
Zhejiang Cancer Hospital, Hangzhou, China. Pathologically all types
were WHO III, 11 cases were males and 1 case was female. Aged from
38 to 68 years, the average age was 52.7 years. The clinical stages
of all cases demonstrated cavernous sinus and intracranial invasion
indicating UICC 2002 staging T4N0-2M0IVa; the Karnofsky values were
≥80. No patients had serious liver and kidney function, heart
function and coagulation disorders or cerebral hemorrhage or
infarction history.
Methods
Seldinger interventional techniques were used.
Briefly, the patients were incubated percutaneous femoral artery
puncture, catheterization of bilateral carotid artery, then
angiography; next inserted into maxillary artery, ascending
pharyngeal artery and branch of the target lesions. Chemotherapy
drugs (80 mg/m2 cisplatin and 60 mg/m2
epirubicin) were injected the day after interventional therapy and
2,500 mg/m2 5-FU was administered using a chemotherapy
electronic pump for 120 h. There were 21 days per cycle. Two
interventional treatments were conducted prior to radio-therapy.
IMRT was conducted 3 weeks after intervention. During radiotherapy,
two cycles of synchronous single-agent chemotherapy were conducted
(80 mg/m2) (Tables I and
II).
 | Table I.The intensity modulated radiation
therapy (IMRT) target area. |
Table I.
The intensity modulated radiation
therapy (IMRT) target area.
| Target area name | Concept |
|---|
| GTVnx | Including imaging
visible primary tumor site |
| GTVnd | Including imaging
visible and confirmable metastatic cervical lymph nodes |
| GTVrn | Retropharyngeal lymph
node |
| PGTVnx | (GTVnx + GTVrn) +
extroverted 3–5 mm |
| PTVnd | Including (GTVnd +
around high-risk lymph node) + extroverted 3–5 mm |
| CTV1 | PGTVnx+ around
high-risk lymph node |
| PTV1 | CTV1 + extroverted
3–5 mm |
| CTV2 | Including total neck
lymph node drainage area |
| PTV2 | CTV2 + extroverted
3–5 mm |
 | Table II.Radiation dose. |
Table II.
Radiation dose.
| Target area name | Single dose (Gy) | Total dose (Gy) | Number |
|---|
| PGTVnx | 2.3 | 69 | 30 |
| GTVnd | 2.2 | 66 | 30 |
| PTVnd | 2.1 | 63 | 30 |
| PTV1 | 2.0 | 60 | 30 |
| PTV2 | 1.8 | 54 | 30 |
Observation methods and clinical
evaluation
All patients gave routine blood samples and their
liver and kidney function was tested every week before and during
treatment. During treatment, tumor regression, general condition,
mucous membrane and gastrointestinal reactions were checked and
recorded. Nasopharyngoscopy and nasopharynx enhanced MR was
performed before treatment, two weeks after the second
intervention, at the end of radiotherapy, and 3 and 6 months after
radiotherapy. Efficacy was evaluated according to the measurement
standard of the WHO, as follows: Complete remission (CR): tumors
disappear completely, the disappearance time is not less then 4
weeks; partial remission (PR): tumors shrink by more than 50%, the
remission time is 4 weeks or more; no change (NC): tumor shrinkage
does not exceed 50% or increase does not exceed 25%; tumor
progression (PD): tumor increase >25%. Toxicity was evaluated
according to the anticancer drug toxicity standard (CTC3.0).
Results
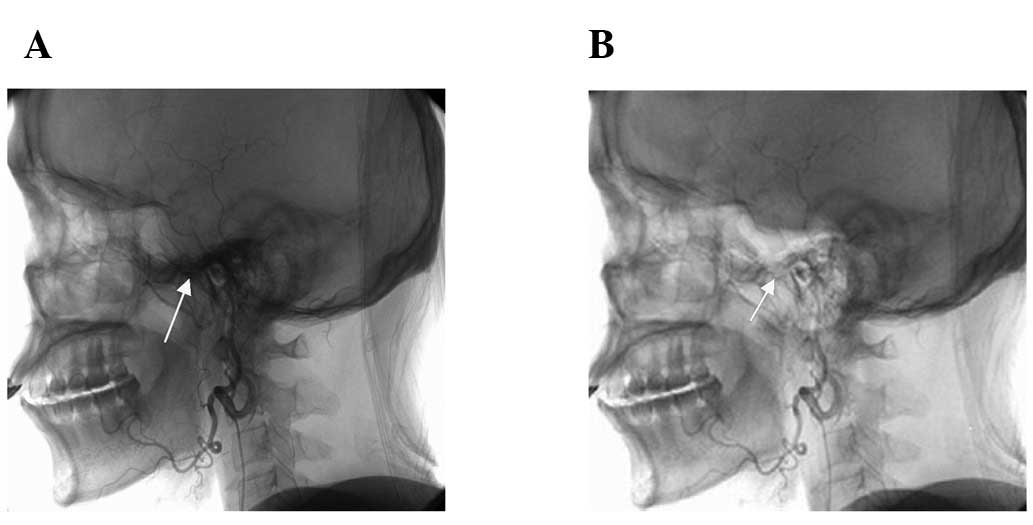
Changes in tumor blood flow
The 12 patients completed two interventional
treatments. Digital subtraction angiography showed that the
internal blood network of NPC reduced following interventional
treatment at different degrees (Fig.
1).
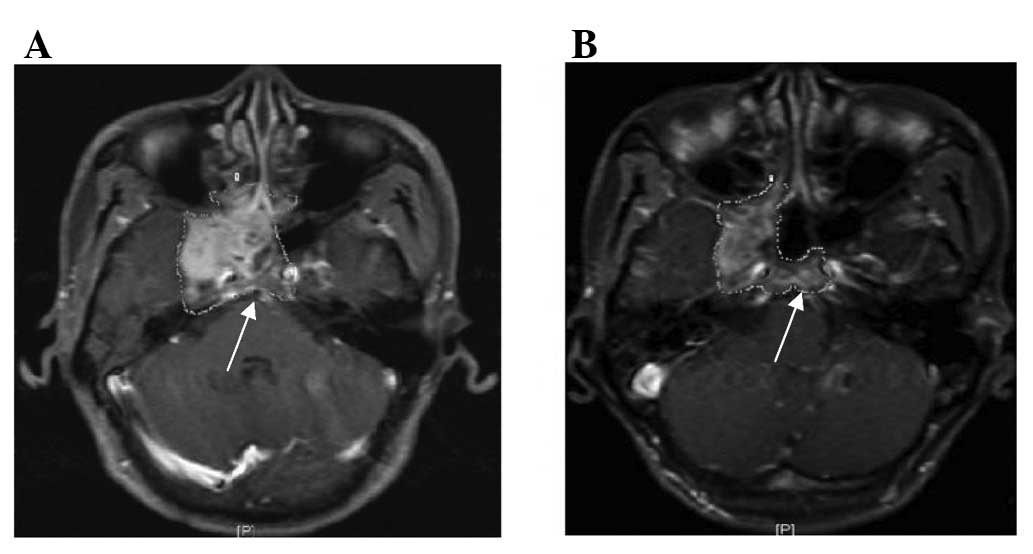
Changes in tumor volume
The average tumor volume of the 12 patients was
decreased from 45,730 to 26,174 mm3 after the second
interventional chemotherapy, the average reduction was 42.76%; the
tumor intracranial total volume was reduced from 9,268 to 4,112
mm3, the average reduction was 55.63%. The distance
between the tumor and the brain stem, optic nerve and optic chiasm
were expanded to 3.5, 5.1 and 5.8 mm from 2.3, 4.4 and 4.6 mm,
respectively (Fig. 2 and Table III). In order to meet the IMRT dose,
95% PTV must meet the dose of the target. The dose changes before
and after intervention are shown in Table V.
 | Table III.Tumor volume changes and locations
before and after interventional therapy. |
Table III.
Tumor volume changes and locations
before and after interventional therapy.
| Case | Tumor volume
(mm2) | Intracranial tumor
volume (mm2) | Brain stem distance
(mm) | Optic nerve distance
(mm) | Optic chiasm distance
(mm) |
|---|
|
|
|
|
|
|---|
| Before | After | Before | After | Before | After | Before | After | Before | After |
|---|
| 1 | 50760 | 33072 | 10025 | 4361 | 2.1 | 3.5 | 3.8 | 4.7 | 4.0 | 5.2 |
| 2 | 67488 | 34920 | 16256 | 4782 | 1.2 | 4.0 | 3.2 | 4.5 | 3.8 | 6.5 |
| 3 | 61344 | 48396 | 15991 | 4330 | 1.5 | 3.1 | 3.1 | 4.2 | 3.8 | 5.2 |
| 4 | 35424 | 25200 | 6548 | 3356 | 2.6 | 3.6 | 5.5 | 5.5 | 4.2 | 5.0 |
| 5 | 43332 | 24312 | 6452 | 4233 | 3.0 | 3.8 | 3.8 | 4.3 | 4.1 | 5.4 |
| 6 | 32760 | 13872 | 5598 | 3945 | 3.0 | 3.7 | 4.8 | 5.0 | 4.8 | 5.3 |
| 7 | 47160 | 24288 | 8256 | 3476 | 2.5 | 3.3 | 5.3 | 5.8 | 5.5 | 6.3 |
| 8 | 69456 | 36132 | 13526 | 4621 | 1.2 | 2.8 | 3.3 | 4.8 | 4.4 | 6.0 |
| 9 | 39960 | 6780 | 6058 | 2935 | 2.3 | 4.6 | 4.8 | 5.2 | 5.5 | 6.5 |
| 10 | 23736 | 14964 | 7856 | 5046 | 3.2 | 3.5 | 5.2 | 5.6 | 4.8 | 5.2 |
| 11 | 50220 | 30360 | 6880 | 3821 | 2.2 | 2.9 | 5.3 | 5.5 | 5.2 | 6.1 |
| 12 | 27120 | 21792 | 7770 | 4438 | 2.8 | 3.2 | 4.7 | 6.1 | 5.1 | 6.9 |
| Average | 45730 | 26174 | 9268 | 4112 | 2.3 | 3.5 | 4.4 | 5.1 | 4.6 | 5.8 |
 | Table V.Dose change of organs at risk before
and after interventional therapy. |
Table V.
Dose change of organs at risk before
and after interventional therapy.
| Target area
name | Before chemotherapy
MDL (Gy) | Interventional
chemotherapy MDL (Gy) | Drop ratio (%) |
|---|
| Brain stem | 66.2 | 56.1 | 15.26 |
| Optic chiasm | 60.3 | 53.6 | 11.11 |
| Optic nerve | 46.5 | 40.2 | 13.55 |
| Temporal lobe | 72.6 | 66.1 | 8.95 |
Evaluation of tumors
At the end of radiotherapy the tumor situation was
as follows: 6 CR cases, 5 PR cases and 1 PD case (distant
metastasis appeared during radiotherapy, so treatment was changed
to local palliative irradiation and systemic chemotherapy).
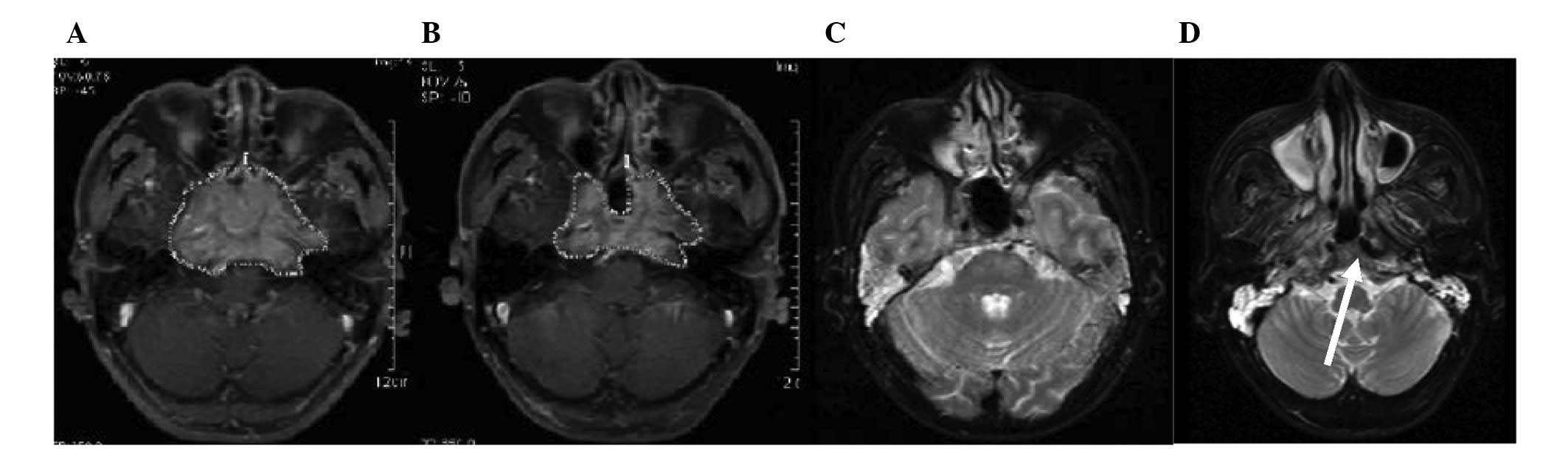
Follow-up
Three months after radiotherapy, the patients were
followed up and 7 cases of CR, 3 cases of PR, 1 case of PD and 1
case of CR were found. One patient succumbed to nasopharyngeal
ulcer hemorrhage. The nasopharynx and intracranial have a large
tumor volume, tumor regression after interventional chemotherapy,
nasopharyngeal mucosa reached grade IV at the end of radiotherapy
and the local secondary infection failed to control, the ulcers
invaded neck blood vessels and caused hemorrhage causing mortality
(Fig. 4). The patients were
followed up 2 years later. The OS and progression-free survival
(PFS) rates were 83.3 and 75%, respectively. One patient succumbed
to nasopharyngeal ulcer hemorrhage, one succumbed to distant
metastasis to multiple organs, and one patient recurred. However,
there was no spinal cord, brain tissue or cranial nerve damage in
any of the cases.
Discussion
IMRT is a revolution in radiation oncology
technology, which has significantly improved treatment for NPC
compared with conventional radiotherapy, although it still has a
higher risk for T4 patients (7),
particularly for T4 NPC patients with intracranial extension, whose
tumor and vital organs (brain stem, optic nerve, optic chiasm and
temporal lobe) are closely connected. Limiting the radiation dose
protects the normal tissues and organs but may result in an
insufficient dose to treat the tumor and lead to local control
failure. Conversely, if the dose is too high it may lead to serious
brain, spinal cord and neurological complications in the
surrounding healthy organs (8). An
insufficient dose to the tumor or excessive dose to normal tissue
is a major obstacle for radiotherapy doctors. Induction
radiotherapy plus concurrent chemotherapy has been shown to improve
OS and local control rates of NPC (9–12).
Interventional chemotherapy has become one of the treatments of a
variety of tumors with the development of interventional
techniques. Drugs injected directly into the tumor nutrient vessels
with interventional chemotherapy increase the local concentration
several times more than drugs injected systemically (13). Selective arterial chemotherapy can
destroy a large number of cancer cells in a short period, which not
only shrinks the tumor volume, reduces the hypoxic cells and
improves the sensitivity of radiotherapy, but also expands the
space between the tumor and other organs to implement IMRT
radiotherapy.
This study showed that the primary tumor volume was
reduced by 42.76% following two doses of interventional
chemotherapy, and the intracranial tumor volume was reduced by
55.63%. The distance from the brain stem, optic nerve and optic
chiasm were increased by 1.2, 0.7 and 1.2 mm, respectively. This
resulted in a smaller GTVnx target. By ensuring the sufficient
therapeutic dose to the tumor, the dosage in the brain stem, optic
chiasm, optic nerve and temporal lobe were decreased by 15.26,
11.11, 13.55 and 8.95%.
The patients tolerated treatment well and had no
serious grade IV adverse reactions to stop treatment. Compared to
another study on conventional PF (DDP + 5-Fu) systemic induction
chemotherapy (14), the patients
did not have hematological toxicity, gastrointestinal tract, liver
or kidney damage. At the end of radiotherapy, there were 6 cases of
tumor CR (50%) and 11 cases of CR plus PR (91.6%). Two years after
radiotherapy, OS was 83.3% and PFS was 75%. After interventional
chemotherapy, all patients presented grade II and above
nasopharyngeal mucositis, 7 cases of grade III (58.3%) and 1 case
of grade IV (8.3%). One patient succumbed to nasopharyngeal ulcer
hemorrhage, tumor shrinkage in nasopharynx and intracranial after
interventional chemotherapy was evidient, and nasopharyngeal mucosa
appeared grade IV at the end of radiotherapy. Local secondary
infection failed to control, the ulcers invaded neck blood vessels
and caused hemorrhage and mortality.
According to research, T4 NPC patients with
intracranial extension were given induction chemotherapy followed
by IMRT plus concurrent chemotherapy with good success. This
treatment method controlled tumors and protected the surrounding
tissues and organs, which is a good choice for locally advanced T4
NPC patients. The OS and PFS were acceptable according to the
2-year follow-up. However, to help reduce the distant metastasis
and local recurrence, long-term observation is required.
References
|
1.
|
Qiu C, Yang N, Tian G, et al: Weight loss
during radiotherapy for nasopharyngeal carcinoma: a prospective
study from northern China. Nutr Cancer. 63:873–879. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Yi JL, Gao L, Huang XD, et al:
Nasopharyngeal cancinoma treated by radical radiotherapy alone:
Ten-year experience of a single institution. Int J Radial Oncol
Biol Phys. 65:161–168. 2006.PubMed/NCBI
|
|
3.
|
Lu T, Zhao C, Wu SX, et al: Retrospective
analysis of 934 primary nasopharyngeal cancinoma (NPC) patients
treated with conventional external-beam radiotherapy alone.
Zhonghua Zhong Liu Za Zhi. 60(suppl): 508–509. 2004.(In
Chinese).
|
|
4.
|
Al-Sarraf M, Le Blanc M, Giri PG, et al:
Chemoradiotherapy versus radiotherapy in patients with advanced
nasopharyngeal cancer. Phase III randomized intergroup study 0099.
J Clin Oncol. 16:1310–1317. 1998.PubMed/NCBI
|
|
5.
|
Al-Sarraf M, Le Blanc M, Giri PG, et al:
Superiority of five year survival with chemo-radiotherapy (CT-RT)
vs. radiotherapy in patients (Pts) with locally advanced
nasopharyngeal cancer (NPC). Intergroup (0099) (SWOG 8892, RTOG
8817, ECOG 2388) phase III study: final report. Proc Am Soc Clin
Oncol. 20:227a(abstract 905). 2001.
|
|
6.
|
Chan ATC and Felip E: Nasopharyngeal
cancer: ESMO clinical recommendations for diagnosis, treatment and
follow-up. Ann Oncol. 20(Suppl 4): 123–125. 2009.
|
|
7.
|
Kam MK, Teo PM, Chau RM, et al: Treatment
of nasopharyngeal cancinoma with intensity-modulated radiotherapy:
the Hong Kong experience. Int J Radiat Oncol Biol Phys.
60:1440–1450. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Ngan RK, Yiu HH, Cheng HK, et al: Central
nervous system metastasis from nasopharyngeal carcinoma: a report
of two patients and a review of the literature. Cancer. 94:398–405.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Baujat B, Audry H, Bourhis J, et al:
Chemotherapy in locally advanced nasopharyngeal carcinoma: an
individual patient data meta-analysis of eight randomized trials
and 1753 patients. Int J Radiat Oncol Biol Phys. 64:47–56. 2006.
View Article : Google Scholar
|
|
10.
|
Airoldi M, Gabriele AM, Gazaro M, et al:
Induction chemotherapy with cispltin and epirubicin followed by
radiotherapy and concurrent cisplatin in locally advanced
nasopharyngeal carcinoma observed in a non-endemic population.
Radiother Oncol. 92:105–110. 2009. View Article : Google Scholar
|
|
11.
|
Palazzi M, Orlandi E, Bossi P, et al:
Futher improvement in outcomes of nasopharyngeal carcinoma with
optimized radiotherapy and induction plus concomitant chemotherapy:
an update of the Milan experience. Int J Radiat Oncol Biol Phys.
74:774–780. 2009. View Article : Google Scholar
|
|
12.
|
Hui EP, Ma BB, Leung SF, et al: Randomized
phase II trial of concurrent cisplatin-radiotherapy with or without
neoadjuvant docetaxel and cisplatin in advanced nasopharyngeal
carcinoma. J Clin Oncol. 27:242–249. 2009. View Article : Google Scholar
|
|
13.
|
Meng ZW, He EH, Meng ZL, et al: Timing
changes of apoptosis and proliferating cells nuclear antigen after
intra-arteiral infusion chemotherapy for nasopharyngeal carcinoma.
Lin Chuang Er Bi Yan Hou Ke Za Zhi. 14:35–37. 2000.(In
Chinese).
|
|
14.
|
Hu F, Chen X, Jiang F, et al: Phase II
trial of neoadjuvant chemotherapy plus concomitant chemotherapy and
intensity modulated radiotherapy with adjuvant chemotherapy for
locally advanced nasopharyngeal carcinoma. Zhejiang Med J.
36:836–839. 2010.(In Chinese).
|