Introduction
Meningiomas are the most common intracranial tumors
and include convex, parasagittal, sphenoid ridge and
cerebellopontine angle meningiomas. Parasagittal meningiomas
account for the 17–20% morbidity rate of intracranial meningiomas
and the 33% morbidity rate of parasagittal and falx meningiomas
(1). Surgical resection is the
first choice of treatment for meningiomas. As the paracentral
lobule, central lobe, draining vein, venous sinus and other
important tissues are involved in the microsurgical treatment of
parasagittal meningiomas, serious complications may occur following
tumor resection. The neural function of patients may be affected,
resulting in a reduction of their quality of life. Therefore, the
improvement of surgical techniques is vital for enhancing the
quality of life of meningioma patients (2,3). In
recent years, microscopic techniques in neurosurgery have
progressed and the efficacy of these techniques has been improved
by the development of suitable surgical strategies. In the present
study, 26 patients with large parasagittal meningioma in the
central gyrus region were treated with microsurgery, and the
efficacy of this technique is discussed.
Materials and methods
Patients
A total of 26 patients (17 males and 9 females) with
large parasagittal meningioma in the central gyrus region who were
admitted to the First Affiliated Hospital of Dalian Medical
University (Dalian, Liaoning, China) were studied between 2004 and
2010. This study was conducted in accordance with the Declaration
of Helsinki and was approved by the Ethics Committee of the First
Affiliated Hospital of Dalian Medical University. Written informed
consent was obtained from all participants. The patient age ranged
between 23 and 68 years, with an average age of 46.2 years. Their
clinical courses ranged between 1.5 months and 10 years, with an
average of 10.2 months. Of the 26 patients, 3 had been diagnosed
with a post-operative recurrence of meningioma.
Clinical symptoms
Of the 26 patients, all reported various degrees of
dizziness and headache, 10 presented with epilepsy, 15 with lateral
limb numbness, 16 with hemiparesis, 2 with light coma and 8 with a
positive pathological reflex.
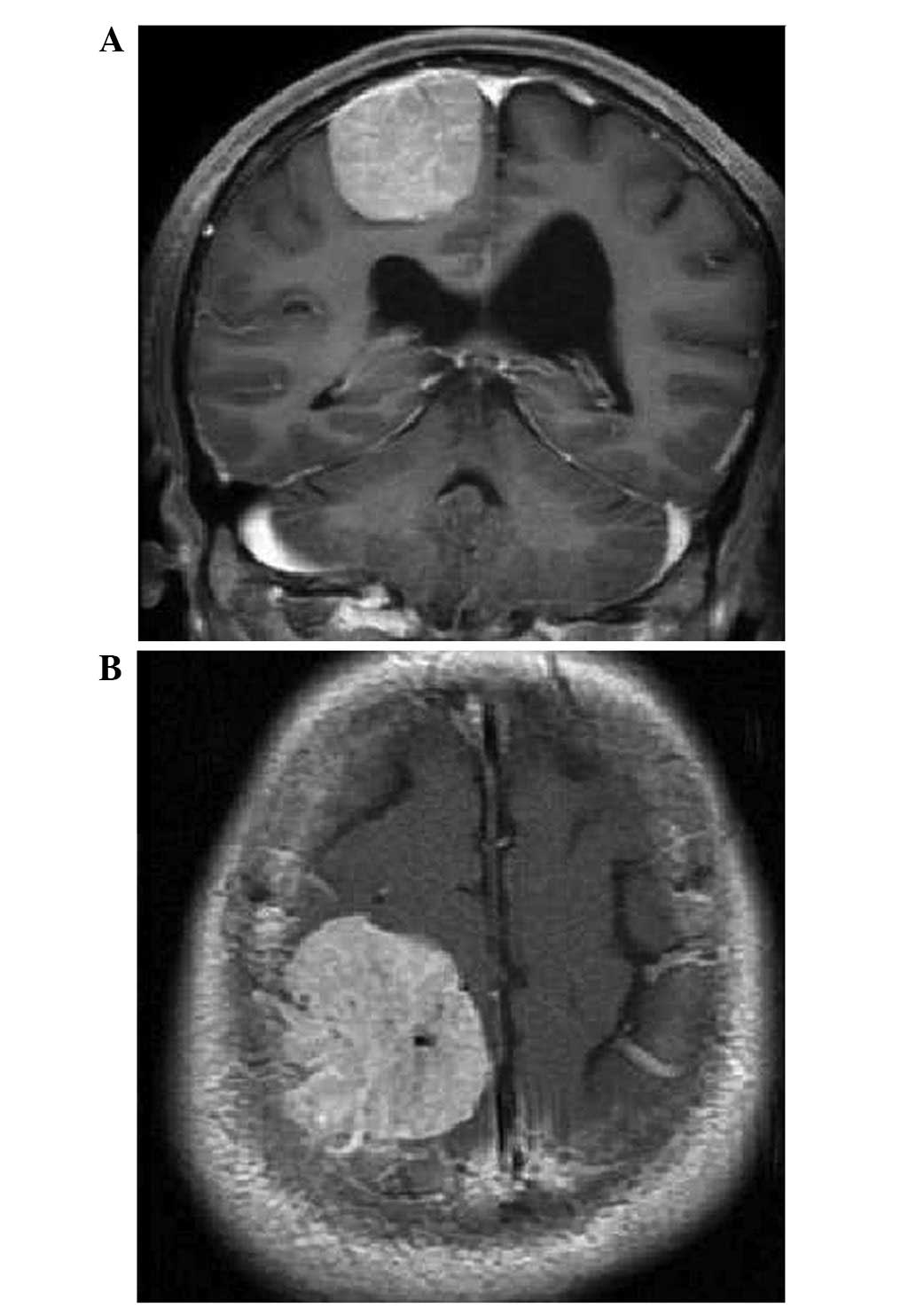
Imaging examination
An X-ray examination was conducted in 10 patients
and there were 8 cases with local cranial hyperostosis. In the 23
patients examined by computed tomography (CT), the central gyrus
sinus presented with a high-density shadow that was round in shape,
with clear boundaries, marked enhancement and surrounding edema.
Certain patients exhibited cranial hyperostosis. Magnetic resonance
imaging (MRI) was performed in all 26 patients. The equal T1 or
slightly high T1, high T2 or slightly high T2 signals were found
with clear boundaries, marked enhancement and surrounding edema in
the lesion site. The maximum diameter of the tumor ranged between
4.0 and 9.6 cm, with an average diameter of 5.6 cm. Digital
subtraction angiography (DSA) was used to examine 12 patients that
presented with large tumors with a rich blood supply. The blood was
being supplied to the parasagittal meningiomas by the external and
internal carotid arteries. Arterial embolization was performed in 3
patients with scalp vascular dilatation. Of the 26 patients, there
were 18 cases with lateral tumors, 8 cases with bilateral tumors
crossing the sagittal sinus, 16 cases with tumors crossing the
Rolandic vein and 10 cases with tumors oppressing the Rolandic
vein.
Microsurgery method
The patients lay in the supine position with their
head fixed in a Mayfield head frame. The microsurgery was conducted
as follows: i) A midline horseshoe-shaped incision was performed
for adequate exposure of the frontal and posterior boundary of
tumor. ii) The dura mater was cut open along the tumor edge,
avoiding damage to the draining vein. Following gradual reduction
of the tumor volume by intratumoral block excision, the tumor
capsule was separated. The tumor tissue outside the sagittal sinus
was removed, then the tumor tissue inside the sagittal sinus and
the invaded sagittal sinus wall were treated. iii) Tumors crossing
the Rolandic vein were removed by block excision to protect the
Rolandic vein. Following a reduction of the tumor size, the
Rolandic vein was stripped. A small amount of tumor tissue may have
remained as it was extremely difficult to strip. The peritumoral
thick vein for compensatory backflow was protected. iv) In patients
with sagittal sinus blockage, the blocked region was removed
following ligation. In cases where the tumor was tightly adhered to
the sagittal sinus, bipolar electrocautery was conducted on the
tumor tissue and sagittal sinus wall. During the surgical
procedure, the electric coagulation power was controlled and the
temperature was lowered with continued flushing water. v) The
eroded skull and meninges were removed. In cases where the skull
was minimally eroded, the inner plate and diploe were resected
without repair.
Results
General information
According to the Simpson grading scale of tumor
resection (4), Simpson grade I, II
or III resection was performed in 8 (30.8%), 12 (46.2%) and 6 (23%)
of 26 patients, respectively, with no perioperative mortalities. In
the 16 cases of pre-operative hemiplegia, 9 patients exhibited
temporary post-operative aggravated hemiplegia or lower limb
paralysis.
Microsurgery effect
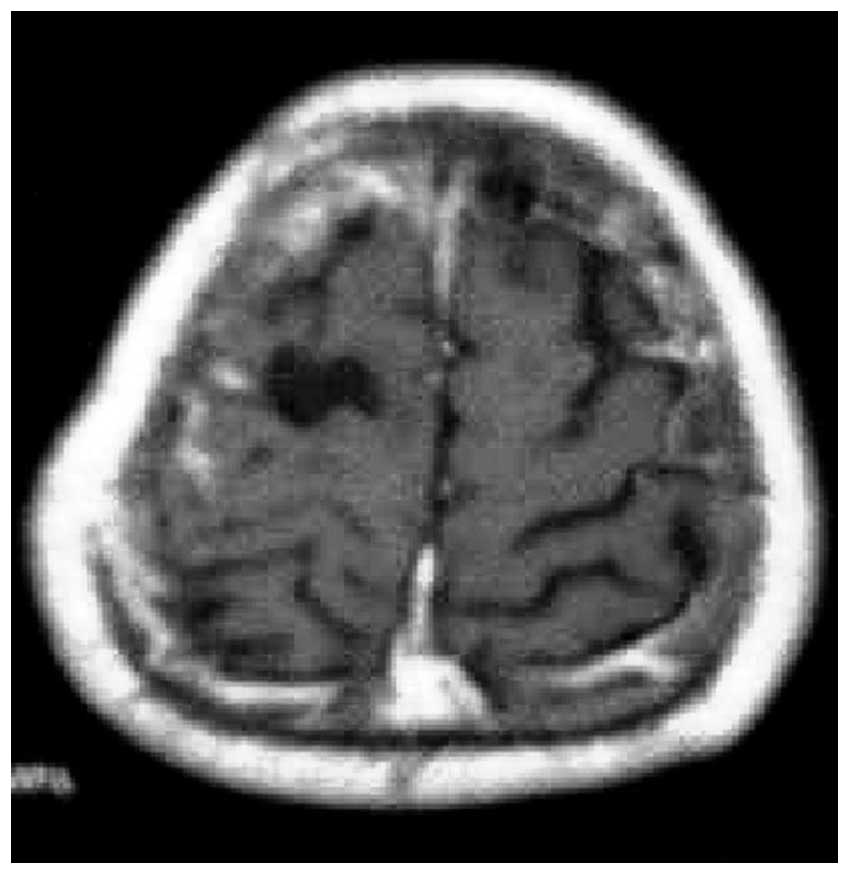
Prior to microsurgery, MRI showed parasagittal
meningioma in the central gyrus region (Fig. 1). Following the total resection of
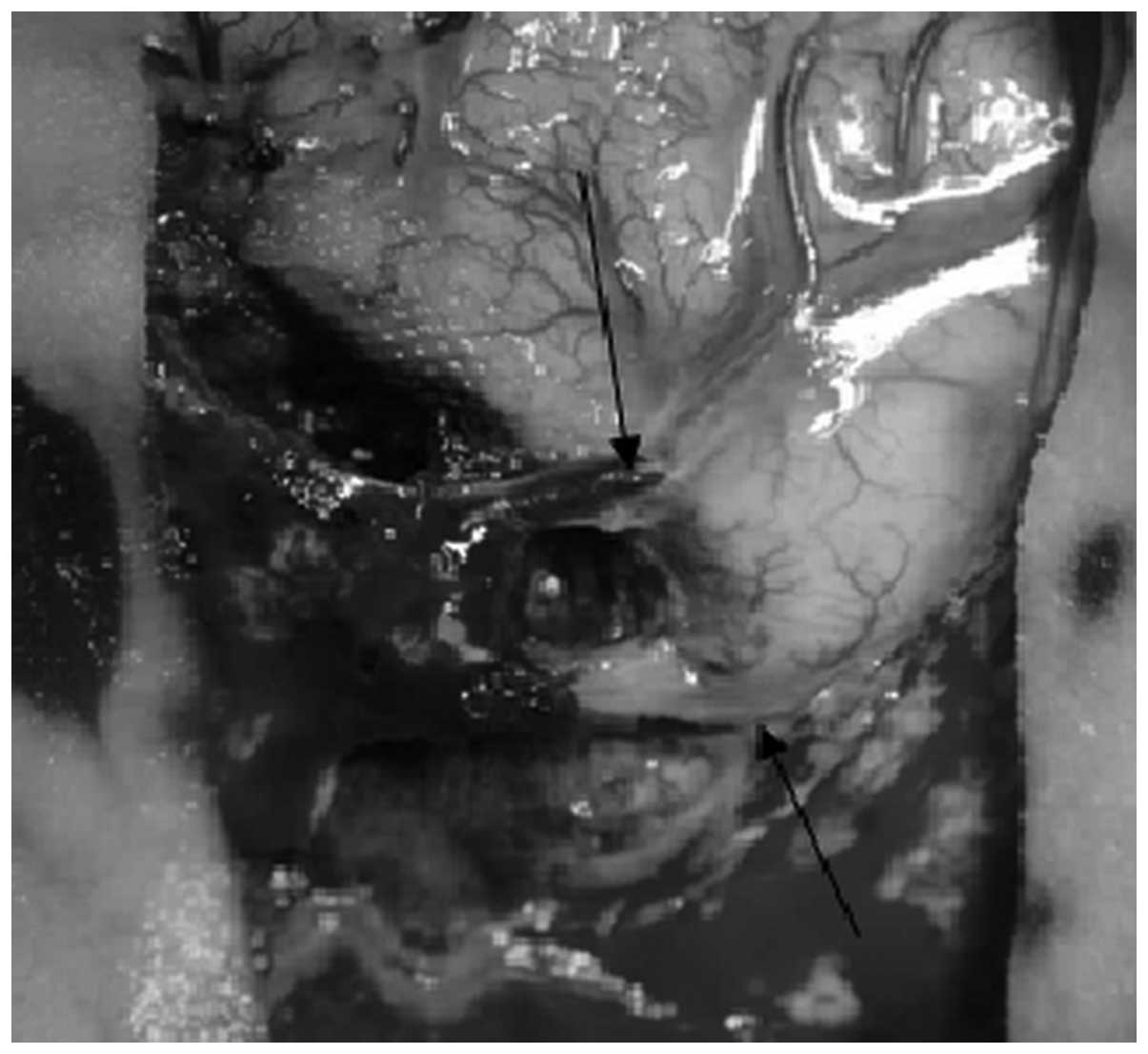
the parasagittal meningioma, the central sulcus veins and superior
cerebral veins flowed under the dura mater for a distance of 2 cm,
then back flowed to the superior sagittal sinus (Figs. 2 and 3). This indicated that, the central sulcus
vein and superior cerebral veins were well retained. Following
active treatment, 6 patients recovered to normal and 3 patients did
not recover (1 case of grade III and 2 cases of grade II) upon
discharge from hospital. In these 3 patients, 1 case (grade III)
had recovered at the four-month follow-up and the other 2 cases had
not fully recovered, but had taken a favorable turn (grade III).
The pathology reports revealed that the number of patients with
endothelial cell-, fiber cell-, psammoma body-, vascular- and
mixed-type tumors was 1, 7, 4, 2 and 1, respectively. No
post-operative recurrence was found in 21 patients during the
follow-up period, which ranged between 8 months and 5 years
(average, 20.3 months).
Discussion
At present, the treatment procedure for parasagittal
meningioma requires the maximization of tumor tissue removal, as
well as improved protection of the central gyrus brain tissue,
Rolandic vein and draining vein, and the effective treatment of the
sagittal sinus (2).
Following the development of modern imaging
technologies and the gradual popularization of CT, MRI and DSA,
parasagittal meningiomas in the central gyrus region may now be
clearly determined and qualitatively diagnosed. However, due to the
position of the tumor, the associated sagittal sinus and draining
vein may be damaged during resection of the tumor, leading to limb
paralysis, severe brain edema and even mortality. The surgical
treatment of parasagittal meningiomas remains difficult, and
methods to maximize the removal of the tumor tissue and minimize
the surgical damage must be developed. Pre-operative imaging
examinations to determine the location, shape, size and blood
supply of the parasagittal meningioma and the relationship between
the tumor and peritumoral tissue and vessels is important during
medical examinations (3,5–7).
Imaging also provides information to aid clinicians in reducing the
surgical risk and the tumor blood supply via embolization (8). CT and MRI examinations are used to
visualize the tumor location, shape and size. MR angiography (MRA),
DSA and CT angiography (CTA) are utilized to determine the position
of the Rolandic vein and tumor blood supply and the status of the
sagittal sinus and collateral circulation (7,10).
These methods are useful for the reduction of intraoperative
bleeding and injury, the protection of the draining vein and the
effective treatment of the associated sagittal sinus.
In the present study, a DSA examination was
performed on 12 patients with large tumors (diameter, >6 cm),
which enabled the generation of a comprehensive understanding of
the tumor blood supply and the states of the sagittal sinus and
peritumoral veins. Pre-operative external carotid artery
embolization was performed on 3 patients with a rich blood supply
from an enlarged external carotid artery. This procedure may be
used to reduce the tumor blood supply and improve the surgical
success rates.
The external and internal carotid arteries provide
the main blood supply to parasagittal meningiomas, and the diploe
and meningeal veins are involved in drainage (2,11,14).
When intracranial pressure is high, the draining vein and sagittal
sinus are compressed, and intracranial vein blood flows out through
the diploe vein, increasing scalp, skull and endocranial
hemorrhaging during craniotomy. In cases where the tumor tissue
adheres to the skull inner plate, opening the bone flap is
extremely difficult and blood loss is likely to be ≥1,000 ml.
Therefore, the control of bleeding during craniotomy is extremely
important for the success of surgical procedures and for improving
the prognosis.
In clinical practice, the measures for controlling
bleeding are as follows (2,8,9): i)
Patients lie in the head-up position and hyperventilation is
conducted under anesthesia. ii) For tumors with a rich blood supply
from the external carotid artery, the end of the superficial
temporal and middle meningeal artery is embolized. After 3–5 days,
resection is performed. iii) Autologous blood transfusion equipment
is used during surgery. iv) Drilling is performed on each side of
the sagittal sinus. The craniotomy is performed using a skull
cutter with an automatic protection function, avoiding the use of
the guide plate and wire saw as much as possible. v) The dura and
sagittal sinus are carefully stripped prior to opening the bone
flap. Sagittal sinus ruptures and damage to the adjacent brain
tissue must be avoided. vi) The blood pressure is controlled during
the surgery (9), with the systolic
blood pressure maintained at <90 mmHg and between 70 and 80 mmHg
when required.
Post-operative complications, including paralysis,
coma, cerebral edema and hemorrhagic infarction, are often
associated with venous system injuries (10,11).
Microsurgery is an important method for the complete resection of
parasagittal meningioma. During the surgical procedure, arteries
providing the blood supply must be treated first, followed by the
treatment of the draining veins (12–14).
Resections must be conducted following the blockage of the sagittal
sinus blood supply. The Rolandic and draining veins and the
peritumoral brain tissue must be protected effectively, and the
associated sagittal sinuses must be treated correctly. These
parameters are the key to a successful surgery. A segment of
draining veins is located under the dura mater and must be
protected when the dura mater is cut. Tumor tissues infiltrated by
the Rolandic veins must be removed by block excision. In the
present study, following the reduction of the tumor mass and
intravenous tension, the Rolandic vein was stripped. As with three
cases from teh present study, a small amount of tumor tissue may
remain as it is extremely difficult to separate the tissue from the
Rolandic vein.
All patients in the present study had large tumors.
Block excision with brain tumor forceps was conducted to remove the
tumor. Following a reduction in the tumor size and intravenous
tension, the tumor capsule was completely removed. During the
separation process, the peritumoral normal brain tissue and the
cerebral pia mater must be effectively protected, and the
aspiration method, which may damage the central gyri, must not be
performed (12–14). In cases where the Rolandic vein is
damaged, venous anastomosis or autogenous vein grafting must be
performed (15). In the present
study, the Rolandic and draining veins in one patient were
identified to infiltrate the tumor tissue and run under the dura
mater for a distance of 2 cm (Figs.
1–2). Block excision was
successfully conducted in this case (Fig. 3).
An appropriate treatment of the involved sagittal
sinuses is extremely important for preventing the post-operative
recurrence of tumors. A complete resection of the tumor with a
reconstruction of the sagittal sinus remains a controversial
process; lateral resection of the sagittal sinus wall followed by
repair with the dura mater, or complete resection of the sagittal
sinus followed by anastomoses with autologous vein or artificial
vessel, have been proposed as suitable methods for this procedure.
However, these measures may lead to higher disability and mortality
rates (16).
In the present study, the sagittal sinus was treated
in accordance with the following principles of treatment: i) In
cases where the tumor has only invaded the outer wall of the
sagittal sinus, electrocautery is performed on the attaching wall
following tumor removal, accompanied by saline washes. ii) If the
tumor has invaded the whole sinusoidal wall or entered the sinus
cavity, the tumor tissue in the sinus cavity and the involved sinus
wall are removed, under conditions of adequate blood source and
controlled blood pressure. The direct suture is conducted on the
small sinus wall gap. If the sinus wall gap is bigger, the
reconstruction of the sinus wall is performed with the fascia or
artificial dura mater, and gelatin sponges and biological glue are
used to reinforce the sinus wall. iii) If the sinus cavity is
completely blocked with a fine peripheral venous return
compensation, the blocked section of the sagittal sinus is removed
together with the tumor (17,18).
During surgery, the peritumoral large draining vein is protected
and the end of the vein is sutured without electrocautery. These
measures may prevent thrombosis formation, which affects the return
compensation of the anastomotic vein. iv) Residual tumor tissue is
treated with γ-Knife or X-Knife radiotherapy to control tumor
growth for an extended period of time (19,20).
In the current study, 6 patients with residual tumors were treated
with this method. No post-operative recurrence was found in 4 of
these patients during the follow-up examinations.
The results of the surgical procedure performed in
the present study include pre-operative imaging evaluations,
skilled microsurgical techniques, effective protection of the
Rolandic veins and treatment of the sagittal sinus, as well as the
avoidance of damage to the cerebral cortex. Together, this protocol
significantly increases the total tumor removal rate and decreases
post-operative recurrence during the microsurgical treatment of
parasagittal meningioma in the central gyrus region.
References
|
1
|
Wang ZC: Diagnosis of neurological
diseases. Neurosurgery. Hubei Science and Technology Press; pp.
595–597. 2005, (In Chinese).
|
|
2
|
Caroli E, Orlando ER, Mastronardi L and
Ferrante L: Meningiomas infiltrating the superior sagittal sinus:
surgical considerations of 328 cases. Neurosurg Rev. 29:236–241.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chen GZ, Chen GM and Song ZH:
Microneurosurgery treatment of parasagittal meningiomas. Zhong Hua
Xian Wei Wai Ke Za Zhi Bian Ji Bu. 29:72–74. 2006.(In Chinese).
|
|
4
|
Simpson D: The recurrent of intracranial
meningimas after surgical treatment. J Neurol Neurosurg Phychiatry.
20:22–39. 1957. View Article : Google Scholar
|
|
5
|
Nowak A and Marchel A: Surgical treatment
of parasagittal and falx meningiornas. Neurol Neurochir Pol.
41:306–314. 2007.
|
|
6
|
Colli BO, Carlotti CG Jr, Assirati JA Jr,
Dos Santos MB, Neder L and Dos Santos AC: Parasagittal meningiomas:
follow-up review. Surg Neurol. 66:S20–S27. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kondziolka D, Mathieu D, Lunsford LD, et
al: Radiosurgery as definitive management of intracranial
meningiomas. Neurosurgery. 62:53–58. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zhang XZ, Wang RZ, Liu Z, et al:
Microneurosurgery treatment of parasagittal meningiomas. Chin J
Microsurg. 19:255–257. 1996.
|
|
9
|
Kozler P, Benes V, Netuka D, Kramár F and
Charvát F: Intracranial meningiomas, standard diagnostic procedure
and results of surgical treatment. Bozhl Chir. 85:431–435. 2006.(In
Czech).
|
|
10
|
Bazzao A, Finocchi V, Romano A, et al:
Role of contrast-enhanced MR venography in the preoperative
evaluation of parasagittal meningioma. Eur Radiol. 15:1790–1796.
2005. View Article : Google Scholar
|
|
11
|
Sindou M, Auque J and Jouanneau E:
Neurosurgery and the intracranial venous system. Acta Neurochir
Suppl. 94:167–175. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Liu Y, Yu ZQ, Li ZL, et al: Microsurgical
strategy for meningioma around central gyrus region. Chin J
Neuromed. 10:296–298. 2011.
|
|
13
|
DiMeco F, Li KW, Casali C, et al:
Meningiomas invading the superior sagittal sinus: surgical
experience in 108 cases. Neurosurgery. 55:1263–1274. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sindou MP and Aivernia JE: Results of
attempted radical tumor removal and venous repair in 100
consecutive meningiomas involving the major dural sinuses. J
Neurosurg. 105:514–525. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hakuba A, Huh CW, Tsujikawa S and
Nishimura S: Total removal of parasagittal meningioma of the
posterior third of sagittal sinus and its repair by autogenous vein
graft: Case report. J Neurosurg. 51:379–382. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhang JY, Wang LZ and Wu AH: Microsurgical
management of petroclival meningiomas. Chin J Neuro Surg. 9:61–63.
2010.
|
|
17
|
Abdel-Aziz KM, Froelieh SC, Dagnew E, et
al: Large sphenoid wing meningiomas involving the cavernous sinus:
conservative surgical strategies for better functional outcomes.
Neurosurgery. 54:1375–1383. 2004. View Article : Google Scholar
|
|
18
|
Menovsky T and De Vries J: Cortical vein
end-to-end anastomosis after removal of a parasagittal meningioma.
Microsurgery. 22:27–29. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Akagami R, Napolitano M and Sekhar LN:
Patient-evaluated outcome after Surgery for basal meningiomas.
Neumsurgery. 50:941–949. 2002.PubMed/NCBI
|
|
20
|
Kondziolka D, Flickinger JC and Perez B:
Judicious resection and/or radiosurgery for parasagittal
meningiomas: outcomes from a multicenter review. Gamma Knife
Meningioma Study Group. Neurosurgery. 43:405–414. 1998. View Article : Google Scholar : PubMed/NCBI
|