Introduction
The treatment options that are available for
metastatic renal cell carcinoma (RCC) are limited due to an
inherent tumor resistance to chemotherapy and radiotherapy
(1). Therefore, as a new treatment
strategy, molecular targeting therapies for metastatic RCC have
been investigated (2). As a result
of the hypervascularity in RCC, the majority of the Food and Drug
Administration-approved molecular targeting therapies are
anti-angiogenic therapies, which block the signals that are
triggered by angiogenic growth factors, including vascular
endothelial growth factor (VEGF) and platelet-derived growth factor
(PDGF). Sorafenib is an anti-angiogenic agent that inhibits
elements of the angiogenesis pathway, including the VEGF receptor
(VEGFR) and the PDGF receptor (PDGFR). Sorafenib also inhibits
certain processes of tumor proliferation, including the Raf/MEK/ERK
pathway, as it is a multikinase inhibitor (3). Since the main mechanism of therapeutic
action is anti-angiogenesis, which shows no direct cytotoxicity,
the therapeutic effect is difficult to evaluate using tumor volume
measurement methods, including the Response Evaluation Criteria In
Solid Tumors (4). Furthermore, the
early identification of the tumor response to sorafenib treatment
is indispensable for selecting optimal personalized treatment
strategies, but at present, no reliable predictors are clinically
available. The mechanisms of action for sorafenib involve
anti-angiogenesis and the inhibition of tumor proliferation. Tumor
proliferation is a useful marker to evaluate the therapeutic effect
and prognosis following therapy in clinical oncology (5,6).
Therefore, the evaluation of tumor proliferation following
sorafenib treatment may reflect the response of the tumor to the
treatment. Histopathological analysis using the Ki-67 labeling
index is a gold standard for the evaluation of tumor proliferation
(7). However, the Ki-67 labeling
index may only be used to evaluate tumor proliferation in biopsy
samples or excised tumor tissues. Thus, a non-invasive method to
evaluate tumor proliferation is required.
18F-fluorothymidine (18F-FLT) positron
emission tomography (PET), which reflects thymidine kinase-1 (TK-1)
activity, is a non-invasive method for detecting tumor
proliferation (8,9). Certain studies have demonstrated the
attenuation of tumor proliferation following radiotherapy or
chemotherapy detected by FLT PET (10–15).
However, the changes in intratumoral FLT distribution following
sorafenib treatment are yet to be clarified. Thus, the present
study assessed whether FLT may be used to evaluate the early tumor
response to sorafenib treatment in an RCC xenograft, and compared
the results with those from an assessment using the tumor
proliferation marker, Ki-67.
Materials and methods
Tumor xenograft model and sorafenib
treatment
Nine-week-old male BALB/c athymic nude mice (Japan
SLC, Inc., Hamamatsu, Japan) were used in the present study.
Approval for the study was obtained from the Laboratory Animal Care
and Use Committee of Hokkaido University (Sapporo, Hokkaido,
Japan). A human RCC xenograft model was established using the human
clear cell RCC (A498) cell line (European Collection of Cell
Cultures, Salisbury, UK), which is a von Hippel-Lindau (VHL)
mutant. The A498 cells were maintained in RPMI-1640 medium
(Invitrogen Life Technologies, Inc., Carlsbad, CA, USA),
supplemented with 10% fetal bovine serum, penicillin-streptomycin
and 0.03% glutamine, and incubated in an atmosphere of 5%
CO2 and 95% air at 37°C. The A498 cells
(1×107 cells/0.1 ml) were subcutaneously inoculated into
the right flank of each mouse. When the tumors grew to 12 mm in
diameter, the mice were randomly assigned to two groups, the day
three and day seven groups (n=10 per group). The mice were then
further assigned to the control and sorafenib-treated subgroups
within each group (n=5 per subgroup; Fig. 1). In the sorafenib-treated groups,
sorafenib (80 mg/kg; Nexavar, Bayer Pharmaceuticals Corporation,
West Haven, CT, USA), in a Cremophor EL (Sigma, St. Louis, MO, USA)
ethanol (Pharmaco Products, Brookfield, CT, USA) and water solution
(12.5:12.5:75) was administered daily by oral gavage. The Cremophor
EL/ethanol/water solution was administered as the vehicle in the
control groups. A tumor growth curve was derived from the day seven
group. The tumor size was measured using a caliper every day from
the first day of treatment, and the tumor volume was calculated
using the following formula: π/6 × larger diameter × (smaller
diameter)2. The change in the tumor volume was
calculated using the following formula: (tumor volume of each day)
− (tumor volume of day 0).
[Methyl-3H(N)]-3′-fluoro-3′-deoxythymidine
(3H-FLT) autoradiography (ARG) Ki-67
immunohistochemistry (IHC) and hematoxylin and eosin (HE)
staining
3H-FLT (specific activity, 74–370
GBq/mmol) was purchased from Moravek Biochemicals Inc. (Brea, CA,
USA). Mice were injected with 0.185 MBq 3H-FLT into the
tail vein. At two hours post-3H-FLT injection, the mice
were sacrificed and the tumors and muscles were immediately
excised. Each excised tumor tissue was then sectioned into 2–3-mm
thick slices to maximize the division surface, then embedded in
Tissue-Tek medium (Sakura Finetechnical Co., Ltd., Tokyo, Japan)
with the calf muscle and frozen in isopentane/dry ice. An adjacent
10-μm cryosection and two adjacent 5-μm cryosections were prepared
with a CM3050-Cryostat (Leica Microsystems, Tokyo, Japan) and used
for ARG, IHC and HE staining, respectively. The 10-μm sections were
placed in a phosphor image plate cassette with a set of calibrated
standards (16), and ARG exposure
was performed for four weeks to detect the distribution of
3H-FLT. The ARG images were analyzed using a
computerized imaging analysis system (FLA 7000 Bio-Imaging
Analyzer; Fuji Photo Film Co., Ltd., Minato-ku, Tokyo, Japan). An
adjacent 5-μm section was immunohistochemically stained for Ki-67
to assess the tumor proliferation. Briefly, following rehydration
and antigen retrieval, endogenous peroxidase activity was blocked
using methanol containing 0.3% hydrogen peroxide. Thereafter, the
sections were incubated with a monoclonal rabbit anti-human Ki-67
antibody (Clone SP6; Thermo Fisher Scientific, Waltham, MA, USA).
The bound antibodies were visualized using the avidin/biotin
conjugate immunoperoxidase procedure with a Histofine SAB-PO kit
(Nichirei Biosciences Inc., Tokyo, Japan) and 3,3′-diaminobenzidine
tetrahydrochloride. The slides were counterstained using Mayer’s
hematoxylin solution (Wako, Osaka, Japan). The IHC images of the
tumor sections that were stained for Ki-67 were captured under a
microscope (Biozero BZ-8000; Keyence Co., Osaka, Japan), and
converted to black and white images using Image J (National
Institutes of Health, Bethesda, MD, USA). For the assessment of the
distribution pattern, the ARG images of 3H-FLT and the
images of the adjacent sections that were stained for Ki-67 by IHC
were visually compared. The remaining adjacent 5-μm sections were
stained with HE to determine the regions of interest (ROIs) for the
quantitative analysis of 3H-FLT using the ARG
images.
Quantitative analysis of
3H-FLT ARG image and Ki-67 IHC
To quantitatively evaluate 3H-FLT
radioactivity, the ROIs were placed to cover the entire tumor
tissue on each ARG image with reference to the HE-stained sections.
The radioactivity in each ROI was calculated using the activity of
the standards and expressed as a percentage of the injected dose
(ID) per gram of tissue following normalization to the animal’s
body weight [(%ID/g) × kg] (16).
For the quantitative analysis of tumor
proliferation, the Ki-67 labeling index, i.e. a percentage of the
number of Ki-67-positive nuclei to the total number of nuclei, was
used. To obtain the Ki-67 labeling index, the numbers of
Ki-67-positive nuclei and nuclei that were stained using Mayer’s
hematoxylin (all nuclei) were counted under a microscope field
(x400 objective magnification, 0.644 mm2 per field)
using Image J. A total of 10 fields per section were randomly
analyzed, excluding the peripheral connective tissue and central
necrotic tissue.
Statistical analyses
All statistical analyses were carried out using
StatView version 5.0 (SAS Institute Inc., Cary, NC, USA). All
values are expressed as mean ± SD. One-way repeated measures
analysis of variance (ANOVA) was used to assess the significant
differences in the trends of the tumor volume changes between the
control and treatment groups (Fig.
2). In the evaluation of 3H-FLT distribution by ARG
and the Ki-67 labeling index (Fig.
4), the Mann-Whitney U test was used to assess the significant
differences between the control and treatment groups on days three
and seven. P<0.05 was considered to indicate a statistically
significant difference.
Results
Tumor volume change
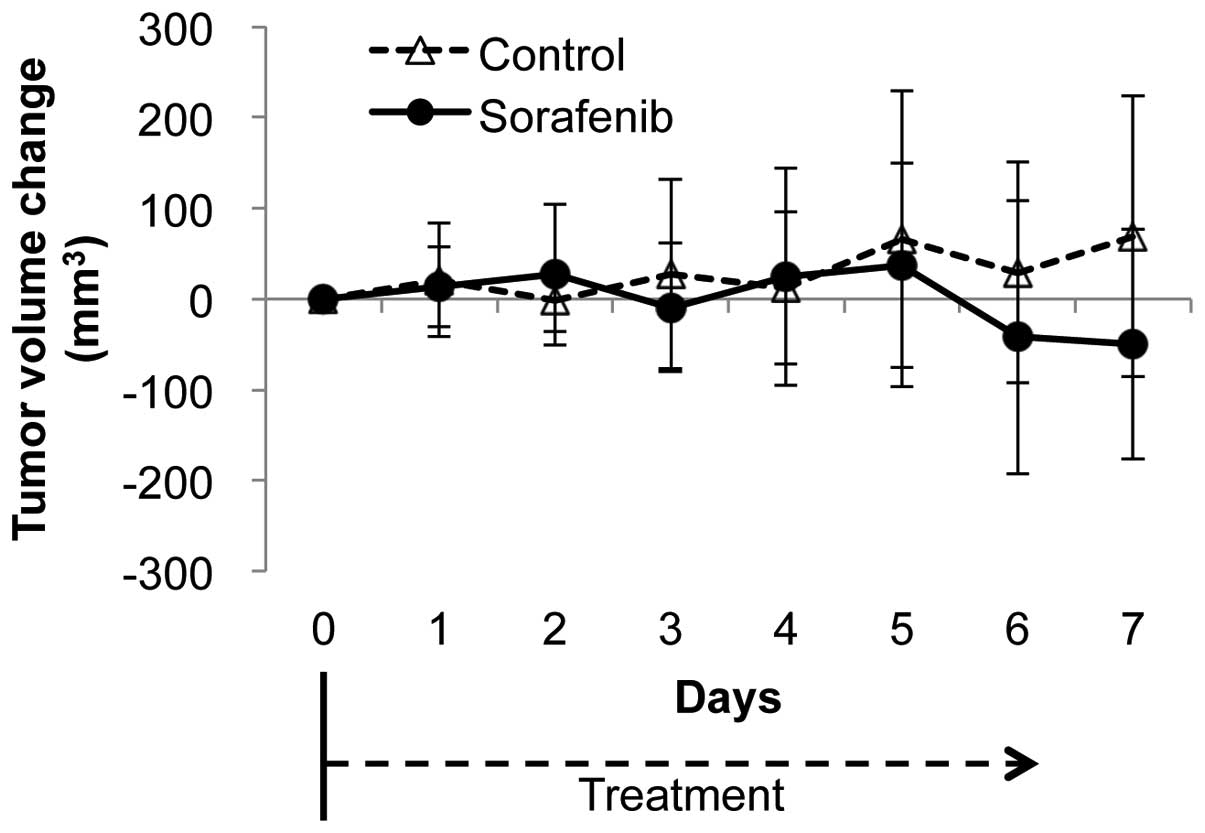
The changes in the tumor volume are shown in
Fig. 2. No statistically
significant differences were observed between the control and
sorafenib-treated groups during the study period until day seven
(P=0.59).
Image comparison between
3H-FLT ARG and Ki-67 IHC
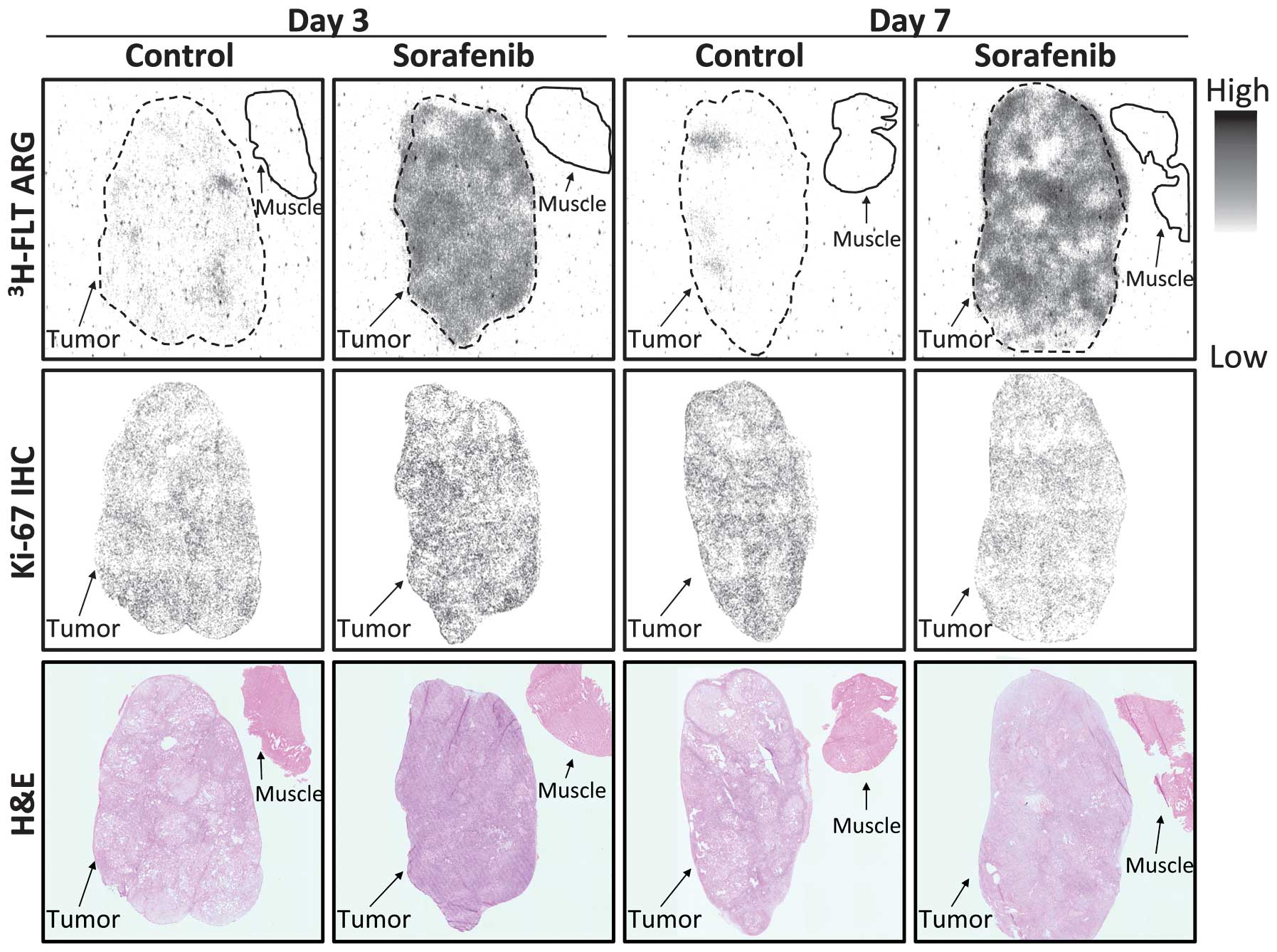
Fig. 3 shows
representative images of 3H-FLT ARG, Ki-67 IHC and HE
staining. In the control groups, the 3H-FLT ARG images
revealed low levels of intratumoral 3H-FLT distribution
on days three and seven, which were similar to those observed in
the muscle. The intratumoral 3H-FLT uptake level was
diffuse and markedly increased in the sorafenib-treated groups
compared with the control groups. There were no significant
differences in the level of intratumoral 3H-FLT
distribution between days three and seven, whereas a more
heterogeneous intratumoral 3H-FLT distribution was
observed on day seven compared with day three in the
sorafenib-treated group. The distribution profiles of the
Ki-67-positive nuclei on days three and seven in the
sorafenib-treated groups were visually similar to those in the
control groups. There were no significant differences in the
distribution level of Ki-67-positive nuclei between days three and
seven in the control and sorafenib-treated groups.
Quantitative analysis of
3H-FLT ARG image and Ki-67 IHC
Fig. 4A shows the
quantitative evaluation of the intratumoral 3H-FLT
distribution on days three and seven following treatment with the
vehicle or sorafenib. The levels of 3H-FLT uptake in the
tumors were 0.74±0.15 and 1.96±0.54 [(%ID/g) × kg] on day three
(P<0.01) and 0.80±0.21 and 2.04±0.42 [(%ID/g) × kg] on day seven
(P<0.01) in the control and sorafenib-treated groups,
respectively. The intratumoral 3H-FLT uptake levels
significantly increased by 2.7- and 2.6-fold on days three and
seven following the treatment with sorafenib, respectively,
compared with the control groups.
Fig. 4B shows the
quantitative evaluation of Ki-67 IHC on days three and seven
following the treatment with the vehicle or sorafenib. The Ki-67
labeling indices in the tumors were 19.1±4.2 and 23.0±7.9% on day
three and 23.1±9.0 and 17.1±3.8% on day seven in the control and
sorafenib-treated groups, respectively. On days three and seven
following the treatment with sorafenib, the Ki-67 labeling indices
were not significantly different from those of the control
groups.
Discussion
A major finding of the present study is that the
level of 3H-FLT uptake diffusely and significantly
increased following the treatment with sorafenib compared with the
control groups (Figs. 3 and
4A), even though the Ki-67-positive
cell distribution, Ki-67 labeling index and tumor volume did not
display significant changes between the sorafenib-treated and
control groups (Figs. 2, 3 and 4B).
At first, the FLT uptake level was expected to decrease in concert
with the suppression of tumor proliferation (Ki-67 labeling index
decrease) by the sorafenib treatment. However, the present findings
unexpectedly revealed that the FLT uptake level in the RCC
xenograft significantly increased following the sorafenib treatment
without significant changes in the tumor proliferation marker level
(Ki-67 labeling index) or the tumor volume.
Sorafenib is a multikinase inhibitor whose action
mechanisms include the inhibition of the tumor proliferative
signaling pathway (17). Therefore,
the proliferation marker and 3H-FLT uptake levels were
expected to decrease following sorafenib treatment in an A498
xenograft. FLT is generally used as a tumor proliferation marker in
clinical oncology (8,9,18).
Numerous studies have demonstrated a decrease in the FLT uptake
level following conventional chemotherapy and, in certain reports,
subsequent to molecular targeted therapy (19). However, in the present study, the
3H-FLT uptake level increased dramatically following the
sorafenib treatment in an A498 xenograft. To the best of our
knowledge, no study has shown an increase in FLT uptake level
during molecular targeted therapy. Only one study has suggested an
increase in FLT uptake level following the cessation of several
days of treatment using the multikinase inhibitor sunitinib malate
in a clinical setting (20).
In addition, the increase in FLT uptake level was
inconsistent with the absence of significant changes in the Ki-67
labeling index in the present study. Recent studies have revealed
the discordance between the level of FLT uptake and other tumor
proliferation markers (21,22). One of the potential causes of the
increase in FLT uptake level without an increase in the level of
proliferation markers is the upregulation of TK-1 activity that
arises from the inhibition of thymidylate synthase (TS). Several
studies have shown that the FLT uptake level reflects TS inhibition
by fluorouracil (5-FU) treatment independent of the tumor
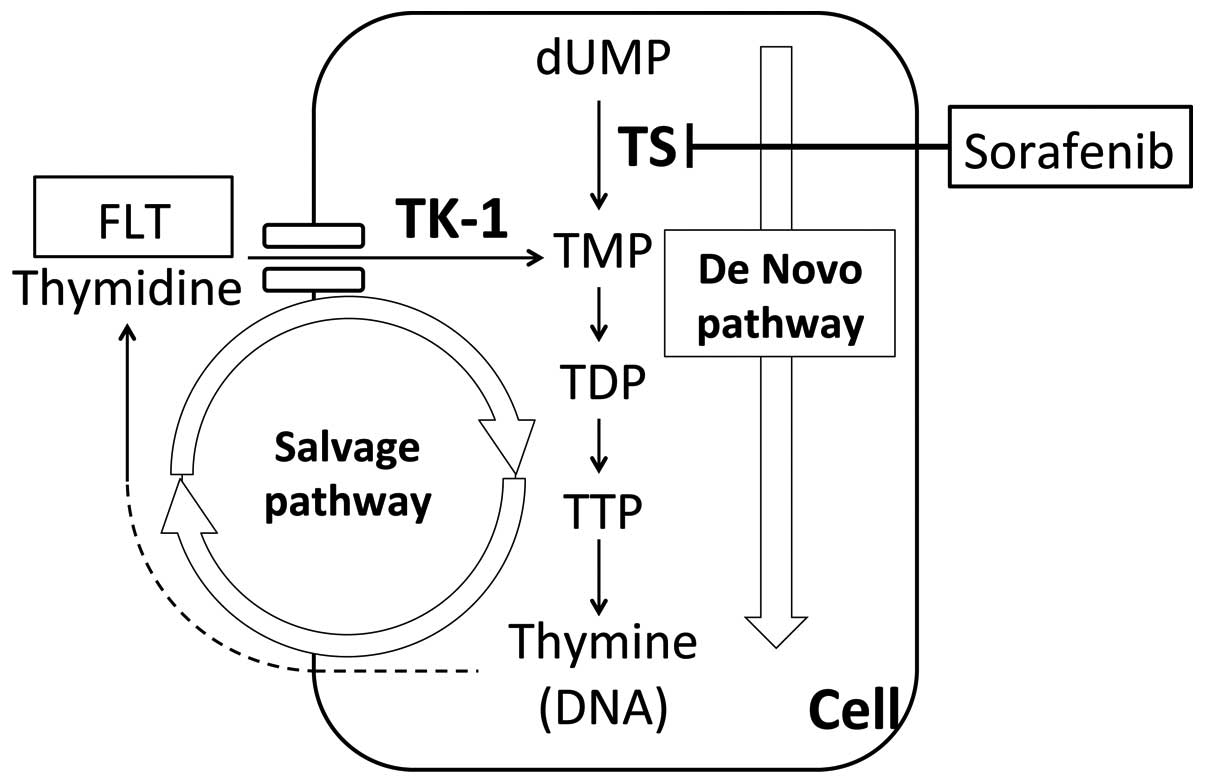
proliferation changes (23,24). A schematic diagram of the thymidine
supply for DNA synthesis is shown in Fig. 5. There are two pathways of thymidine
supply for DNA synthesis, the de novo pathway and the
salvage pathway. TS and TK-1 are critical enzymes in the de
novo and salvage pathways, respectively. When the de
novo pathway is suppressed, the salvage pathway is
compensatorily upregulated to maintain a certain level of thymidine
supply (24,25). Thus, TS inhibition or suppression
increases TK-1 activity and FLT uptake (24).
With regard to the effect of sorafenib on the
thymidine supply pathways, only one study has suggested the
suppression of TS in RCC cells following sorafenib treatment
(26). The increase in the FLT
uptake level following sorafenib treatment in the present study may
have been caused by the TS suppressive effect of sorafenib, which
upregulates the thymidine salvage pathway. The present study
strongly indicated the importance of determining whether the
treatment affects the activity of TS when evaluating the treatment
response by FLT PET.
In addition to the fact that the FLT uptake level
directly reflects TK1 activity but not tumor proliferation, the
technical aspects, including the difference in the samples used for
the evaluation of FLT uptake and Ki-67, should be considered as
another reason for the inconsistency between the level of
3H-FLT uptake and the Ki-67 labeling index. However, in
the present study, tumor-adjacent sections were used for
3H-FLT ARG and Ki-67 IHC image comparison, which enabled
the comparison of the distributions of FLT and Ki-67-positive cells
at a microscopic level. Additionally, in the present ARG
experiments, 3H-FLT was used instead of
18F-FLT, even though 18F-FLT has been
extensively used to determine FLT distribution. The use of
3H-FLT produced clearer images and provided more precise
information on the FLT distribution than that of
18F-FLT, owing to the shorter radiation range of
3H.
In conclusion, the intratumoral 3H-FLT
distribution was significantly increased following sorafenib
treatment in a human RCC xenograft, even though the tumor
proliferation marker Ki-67 labeling index and the tumor volume did
not significantly change. Thus, an increased FLT uptake level
following treatment may indicate the suppression of TS and a
compensatory upregulation of TK-1 activity. Further studies are
required to clarify the mechanisms underlying the increased FLT
uptake following sorafenib treatment, which may lead to the
application of FLT PET for monitoring the treatment effects.
Acknowledgements
The present study was partially supported by the
Project for Developing Innovation Systems: Creation of Innovation
Centers for Advanced Interdisciplinary Research Areas Program from
the Ministry of Education, Culture, Sports, Science and Technology
and the Japanese Government. This study was also partially
supported by JSPS KAKENHI, grant no. 23591732. The authors would
like to thank the staff of the Department of Nuclear Medicine, the
Central Institute of Isotope Science, and the Laboratory of
Veterinary Internal Medicine at Hokkaido University (Sapporo,
Hokkaido, Japan).
Abbreviations:
|
ARG
|
autoradiography
|
|
FLT
|
fluorothymidine
|
|
HE
|
hematoxylin and eosin
|
|
IHC
|
immunohistochemistry
|
|
PDGF
|
platelet-derived growth factor
|
|
PDGFR
|
platelet-derived growth factor
receptor
|
|
RCC
|
renal cell carcinoma
|
|
ROI
|
region of interest
|
|
TS
|
thymidylate synthase
|
|
TK-1
|
thymidine kinase-1
|
|
VEGF
|
vascular endothelial growth factor
|
|
VEGFR
|
vascular endothelial growth factor
receptor
|
|
VHL
|
von Hippel-Lindau
|
References
|
1
|
Rini BI: Vascular endothelial growth
factor-targeted therapy in renal cell carcinoma: current status and
future directions. Clin Cancer Res. 13:1098–1106. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cáceres W and Cruz-Chacón A: Renal cell
carcinoma: molecularly targeted therapy. PR Health Sci J. 30:73–77.
2011.PubMed/NCBI
|
|
3
|
Chang YS, Adnane J, Trail PA, et al:
Sorafenib (BAY 43–9006) inhibits tumor growth and vascularization
and induces tumor apoptosis and hypoxia in RCC xenograft models.
Cancer Chemother Pharmacol. 59:561–574. 2007.
|
|
4
|
Escudier B, Eisen T, Stadler WM, et al;
TARGET Study Group. Sorafenib in advanced clear-cell renal-cell
carcinoma. N Engl J Med. 356:125–134. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Elias JM: Cell proliferation indexes: a
biomarker in solid tumors. Biotech Histochem. 72:78–85. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gerdes J: Ki-67 and other proliferation
markers useful for immunohistological diagnostic and prognostic
evaluations in human malignancies. Semin Cancer Biol. 1:199–206.
1990.
|
|
7
|
Scholzen T and Gerdes J: The Ki-67
protein: from the known and the unknown. J Cell Physiol.
182:311–322. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shields AF, Grierson JR, Dohmen BM, et al:
Imaging proliferation in vivo with [F-18]FLT and positron emission
tomography. Nat Med. 4:1334–1336. 1998.
|
|
9
|
Toyohara J, Waki A, Takamatsu S, Yonekura
Y, Magata Y and Fujibayashi Y: Basis of FLT as a cell proliferation
marker: comparative uptake studies with [3H]thymidine and
[3H]arabinothymidine, and cell-analysis in 22 asynchronously
growing tumor cell lines. Nucl Med Biol. 29:281–287.
2002.PubMed/NCBI
|
|
10
|
Apisarnthanarax S, Alauddin MM, Mourtada
F, et al: Early detection of chemoradioresponse in esophageal
carcinoma by 3′-deoxy-3′-3H-fluorothymidine using preclinical tumor
models. Clin Cancer Res. 12:4590–4597. 2006.PubMed/NCBI
|
|
11
|
Chao KS: Functional imaging for early
prediction of response to chemoradiotherapy:
3′-deoxy-3′-18F-fluorothymidine positron emission tomography - a
clinical application model of esophageal cancer. Semin Oncol. 33(6
Suppl 11): S59–S63. 2006.PubMed/NCBI
|
|
12
|
Chao KS: 3′-deoxy-3′-(18)F-fluorothymidine
(FLT) positron emission tomography for early prediction of response
to chemoradiotherapy - a clinical application model of esophageal
cancer. Semin Oncol. 34(2 Suppl 1): S31–S36. 2007.
|
|
13
|
Leyton J, Latigo JR, Perumal M, Dhaliwal
H, He Q and Aboagye EO: Early detection of tumor response to
chemotherapy by 3′-deoxy-3′-[18F]fluorothymidine positron emission
tomography: the effect of cisplatin on a fibrosarcoma tumor model
in vivo. Cancer Res. 65:4202–4210. 2005.
|
|
14
|
Ullrich RT, Zander T, Neumaier B, et al:
Early detection of erlotinib treatment response in NSCLC by
3′-deoxy-3′-[F]-fluoro-L-thymidine ([F]FLT) positron emission
tomography (PET). PLoS One. 3:e39082008.
|
|
15
|
Kenny L, Coombes RC, Vigushin DM,
Al-Nahhas A, Shousha S and Aboagye EO: Imaging early changes in
proliferation at 1 week post chemotherapy: a pilot study in breast
cancer patients with 3′-deoxy-3′-[18F]fluorothymidine positron
emission tomography. Eur J Nucl Med Mol Imaging. 34:1339–1347.
2007.PubMed/NCBI
|
|
16
|
Zhao S, Kuge Y, Mochizuki T, et al:
Biologic correlates of intratumoral heterogeneity in 18F-FDG
distribution with regional expression of glucose transporters and
hexokinase-II in experimental tumor. J Nucl Med. 46:675–682.
2005.PubMed/NCBI
|
|
17
|
Wilhelm SM, Carter C, Tang L, et al: BAY
43–9006 exhibits broad spectrum oral antitumor activity and targets
the RAF/MEK/ERK pathway and receptor tyrosine kinases involved in
tumor progression and angiogenesis. Cancer Res. 64:7099–7109.
2004.
|
|
18
|
Buck AK, Herrmann K, Shen C, Dechow T,
Schwaiger M and Wester HJ: Molecular imaging of proliferation in
vivo: positron emission tomography with [18F]fluorothymidine.
Methods. 48:205–215. 2009.
|
|
19
|
Barwick T, Bencherif B, Mountz JM and
Avril N: Molecular PET and PET/CT imaging of tumour cell
proliferation using F-18 fluoro-L-thymidine: a comprehensive
evaluation. Nucl Med Commun. 30:908–917. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Liu G, Jeraj R, Vanderhoek M, et al:
Pharmacodynamic study using FLT PET/CT in patients with renal cell
cancer and other solid malignancies treated with sunitinib malate.
Clin Cancer Res. 17:7634–7644. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhang CC, Yan Z, Li W, et al:
[(18)F]FLT-PET imaging does not always ‘light up’ proliferating
tumor cells. Clin Cancer Res. 18:1303–1312. 2012.
|
|
22
|
Chalkidou A, Landau DB, Odell EW,
Cornelius VR, O’Doherty MJ and Marsden PK: Correlation between
Ki-67 immunohistochemistry and 18F-Fluorothymidine uptake in
patients with cancer: A systematic review and meta-analysis. Eur J
Cancer. 48:3499–3513. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lee SJ, Kim SY, Chung JH, et al: Induction
of thymidine kinase 1 after 5-fluorouracil as a mechanism for
3′-deoxy-3′-[18F]fluorothymidine flare. Biochem Pharmacol.
80:1528–1536. 2010.PubMed/NCBI
|
|
24
|
Plotnik DA, McLaughlin LJ, Krohn KA and
Schwartz JL: The effects of 5-fluoruracil treatment on
3′-fluoro-3′-deoxythymidine (FLT) transport and metabolism in
proliferating and non-proliferating cultures of human tumor cells.
Nucl Med Biol. 39:970–976. 2012.
|
|
25
|
Wilson PM, LaBonte MJ, Lenz HJ, Mack PC
and Ladner RD: Inhibition of dUTPase induces synthetic lethality
with thymidylate synthase-targeted therapies in non-small cell lung
cancer. Mol Cancer Ther. 11:616–628. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Takeuchi A, Shiota M, Tatsugami K, et al:
Sorafenib augments cytotoxic effect of S-1 in vitro and in vivo
through TS suppression. Cancer Chemother Pharmacol. 68:1557–1564.
2011. View Article : Google Scholar : PubMed/NCBI
|