Introduction
Non-small cell lung cancer (NSCLC) is the leading
cause of mortality from cancer and the most common source of brain
metastases. It is estimated that between 30 and 50% of lung cancer
patients develop metastatic cancer to the brain during the course
of their illness (1). Patients with
untreated brain metastases have a median survival time of ~4 weeks
and almost all succumb to neurological rather than systemic causes
(2). Management and treatment of
metastatic brain tumors are complex and dependent on several
factors, including age, performance status, number of metastases at
presentation and status of systemic disease. Radiation therapy
options for brain metastases include whole brain radiotherapy
(WBRT) and stereotactic radiosurgery (SRS). For a number of years,
WBRT has been the primary brain metastases treatment; however, a
number of studies have reported an unfavorable effect on
neurocognitive function which, in turn, correlates with decreased
quality of life (3,4). By contrast, SRS alone provides great
benefits in managing brain metastases, representing a minimally
invasive treatment with an excellent local control rate,
correlating with a minor risk of neurological dysfunction (5).
Repeat SRS for recurrent metastases is a noteworthy
option, although, few clinical studies support normal brain tissue
tolerance to re-irradiation (6,7).
In the current case report, we present a patient
with brain metastasis of NSCLC who underwent repeat SRS, analyzing
the outcomes (response, survival and toxicity) and the clinical
utility, and comparing our approach with other experiences
described in the literature.
Case report
Clinical presentation and treatment
In April 2010, a 40-year-old male, with a history of
NSCLC (histology, adenocarcinoma) treated from 2008, was referred
to the Department of Radiation Oncology, Tommaso Campanella Cancer
Center (Catanzaro, Italy) for a lesion in the right frontal lobe
measuring 1.4 cm in maximum diameter (Fig. 1A). Based on RTOG criteria, the
patient was eligible for SRS: Lesion measuring <3 cm in maximum
diameter, producing minimal mass effect and ECOG performance
status, 0.
In May 2010, the patient underwent a stereotactic
treatment delivered in a single dose of 24 Gy using a Clinac DBX
600 (Varian Medical Systems Inc., Palo Alto, CA, USA) and was
followed up clinically by serial MRI and CT scans. In September
2010, a complete response to the radiotherapy treatment was
documented by an MRI of the brain.
Disease recurrence
A CT scan revealed a recurrent disease, in the same
area as treated previously, 17 months after the irradiation of the
metastatic brain tumor (Fig. 1B).
At this point, the patient was offered a second SRS treatment as an
alternative to surgery. Following obtaining consent for
re-irradiation, in November 2011, the patient underwent a second
session of radiosurgery, which was delivered in the same manner as
the initial session, but at a single dose of 15 Gy (Fig. 2A and B). In this case, the dose was
selected according to a previous study using the linear quadratic
model to derive information on the cumulative biological effective
tolerance dose (BEDcumulative) that results from
BEDinitial plus BEDre-irradiation(8).
A stable disease, associated with no symptoms or
signs associated with neurological decline, was documented in the
following CT scan and MRI brain controls until July 2012, when a
MRI brain scan again showed a lesion measuring 1 cm in diameter in
the same region and surrounded by an extensive area of vasogenic
edema, compatible with a recurrence of disease.
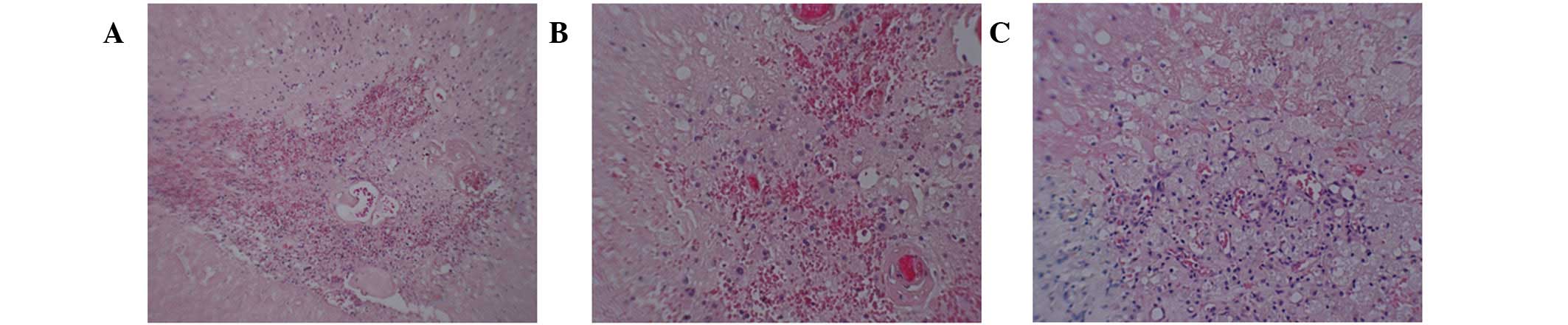
Therefore, in August 2012, the patient underwent
surgery to remove the right frontal lesion. Histological diagnosis
following surgery showed absence of disease and the occurrence of
radionecrosis (Fig. 3A–C).
At present, the patient is receiving treatment with
erlotinib and appears to be in good general condition (ECOG
performance status, 0).
Discussion
When we decided to repeat SRS in the current case,
it was important to scrutinize the existing evidence available
regarding the use of SRS for the treatment of recurrent/progressive
brain metastases. In this case, recurrent brain metastasis was
defined as metastasis that has recurred at the original site of the
brain following initial therapy.
The present patient belongs to category of
individuals who survive long enough to experience recurrence of
previously treated brain metastases but for whom no consensus on
treatment exists, as the majority of studies have focused on newly
diagnosed patients. In addition, few studies have demonstrated the
clinical utility of repeat SRS for brain metastases.
Ammirati et al previously reported that there
is insufficient evidence with regard to repeat SRS to generate
definitive treatment recommendations in patients with
recurrent/progressive brain metastases. Therefore, the treatment
must be individualized based on a patient’s functional status,
extent of disease, volume/number of metastases, recurrence or
progression at the original site, previous treatment and type of
primary cancer (9).
The value of SRS for recurrent brain metastases
remains unclear and only five case studies (with Class III evidence
according to the American Association of Neurological
Surgeons/Congress of Neurological Surgeons criteria) (9) reported in the literature have
demonstrated the clinical utility of repeat SRS and have evaluated
its efficacy in patients whose previous treatment protocol included
radiosurgery. In addition, only three of these case studies provide
survival data from the date of SRS for recurrent disease. Yamanaka
et al(10) and Shuto et
al(11) reported median
survival times from initial SRS of 15 and 22.4 months,
respectively, in patients who repeated SRS for recurrent or newly
developed brain metastases from various types of malignancies.
In a previous study by Chen et al, median
survival from the time of SRS for recurrent brain metastases was 7
months in 45 patients (12). In
addition, in a study by Kwon et al, 43 patients underwent
salvage SRS and the median survival from the time of SRS for
recurrent/progressive disease was 8 months (13). More recently, Mariya et al
reported that repeat SRS is an effective treatment option, leading
to a long survival with a decreased neurological decline (14,15).
The authors analyzed 28 patients who underwent salvage radiosurgery
for recurrent brain metastases from NSCLC showing a median survival
from initial SRS of 26 months and 11 months for post-repeat
SRS.
In our experience, based on these previous studies,
repeat SRS was evaluated as the most effective alternative therapy.
In addition, our patient was included in the most favorable
prognostic group (baseline characteristics: age, <50 years old;
KPS 90–100; 1 intracranial metastasis present and absence of
extracranial metastases) for the existing criteria of a prognostic
classification called Graded Prognostic Assessment, based on a
previous review of the RTOG database (16).
An additional advantage of repeat SRS is the
possibility to administer precisely directed, high-dose irradiation
that tightly conforms to an intracranial target, in order to create
a desired radiobiological response while minimizing radiation dose
to surrounding normal tissue. Our primary end-point was to preserve
the neurocognitive functions of the patient, considering the high
risk of neurological decline with conventional radiotherapy
techniques (3,4).
With regard to neurological complications of repeat
SRS, Bhatnagar et al reported that repeat SRS was performed
with minimal CNS toxicity compared with the baseline in 26 patients
with benign and malignant tumors (17). In the final report of RTOG protocol
90–05, Shaw et al revealed the feasibility of SRS as
retreatment of recurrent primary and metastatic brain tumors
previously irradiated. The authors also showed that the maximally
tolerated SRS dose ranged between 15 and 24 Gy, depending on the
tumor size (18).
In the present case study, progression-free survival
was 18 months starting from the initial radiosurgical treatment and
8 months from post-repeat SRS. The retreatment was well tolerated
by the patient and no acute toxicity was observed. Neurological
status was estimated from medical records, according to the
criteria by Bhatnagar et al, based on the serial changes of
3 neurological symptoms: Seizures, focal deficits and headaches
(17). None of these or any new
symptoms were documented following repeat SRS. In addition, at each
clinical control, neurological status and the severity of
complications were rated according to RTOG CNS toxicity criteria as
grade 0, according to the RTOG/EORTC scoring schema (19).
In addition, clinical chronic use of steroids was
not necessary. Mini-mental state examinations were performed prior
to and soon following the first and second radiotherapy treatment,
and every 3 months during the follow-up, identifying a stable score
ranging between 26 and 30. Repeat SRS was performed to improve
local brain tumor control and reduce the neurological decline risk,
enabling the patient to return to work.
Observations of the current and previous case
studies discussed indicate the clinical usefulness and feasibility
of repeat SRS as salvage treatment for the management of brain
metastases from NSCLC, and may be a valid approach for a selected
group of patients with recurrent brain metastases.
References
|
1
|
Schouten LJ, Rutten J, Huveneers HA and
Twijnstra A: Incidence of brain metastases in a cohort of patients
with carcinoma of breast, colon, kidney, and lung and melanoma.
Cancer. 94:2698–2705. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Patchell RA: The management of brain
metastases. Cancer Treat Rev. 29:533–540. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Aoyama H, Tago M, Kato N, Toyoda T, Kenjyo
M, Hirota S, Shioura H, Inomata T, Kunieda E, Hayakawa K, et al:
Neurocognitive function of patients with brain metastasis who
received either whole brain radiotherapy plus stereotactic
radiosurgery or radiosurgery alone. Int J Radiat Oncol Biol Phys.
68:1388–1395. 2007. View Article : Google Scholar
|
|
4
|
Chang EI, Wefel JS, Hess KR, Allen PK,
Lang FF, Kornguth DG, Arbuckle RB, Swint JM, Shiu AS, Maor MH and
Meyers CA: Neurocognition in patients with brain metastases treated
with radiosurgery or radiosurgery plus whole-brain irradiation: a
randomized controlled trial. Lancet Oncol. 10:1037–1044. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Linskey ME, Andrews DW, Asher AL, Burri
SH, Kondziolka D, Robinson PD, Ammirati M, Cobbs CS, Gaspar LE,
Loeffler JS, et al: The role of stereotactic radiosurgery in the
management of patients with newly diagnosed brain metastases: a
systematic review and evidence-based clinical practice guideline. J
Neurooncol. 96:45–68. 2010. View Article : Google Scholar
|
|
6
|
Dritschilo A, Bruckman JE, Cassady JR and
Belli JA: Tolerance of brain to multiple courses of radiation
therapy. I Clinical experiences. Br J Radiol. 54:782–786. 1981.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Horns J and Webber MM: Retreatment of
brain tumors. Radiology. 88:322–325. 1967. View Article : Google Scholar
|
|
8
|
Mayer R and Sminia P: Reirradiation
tolerance of the human brain. Int J Radiat Oncol Biol Phys.
70:1350–1360. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ammirati M, Cobbs CS, Linskey ME,
Paleologos NA, Ryken TC, Burri SH, Asher AL, Loeffler JS, Robinson
PD, Andrews DW, et al: The role of retreatment in the management of
recurrent/progressive brain metastases: a systemic review and
evidence-based clinical practice guideline. J Neurooncol. 96:85–96.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yamanaka K, Iwai Y, Yasui T, Nakajima H,
Komiyama M, Nishikawa M, Morikawa T and Kishi H: Gamma Knife
radiosurgery for metastatic brain tumor: the usefulness of repeated
Gamma Knife radiosurgery for recurrent cases. Stereotact Funct
Neurosurg. 72(Suppl 1): 73–80. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shuto T, Fujino H, Inomori S and Nagano H:
Repeated Gamma Knife radiosurgery for multiple metastatic brain
tumors. Acta Neurochir (Wien). 146:989–993. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chen JC, Petrovich Z, Giannotta SL, Yu C
and Apuzzo ML: Radiosurgical salvage therapy for patients
presenting with recurrence of metastatic disease to the brain.
Neurosurgery. 46:860–866. 2000.PubMed/NCBI
|
|
13
|
Kwon KY, Kong DS, Lee JI, Nam DH, Park K
and Kim JH: Outcome of repeated radiosurgery for recurrent
metastatic brain tumors. Clin Nerol Neurosurg. 109:132–137. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mariya Y, Sekizawa G, Matsuoka Y, Seki H,
Sugawara T and Sasaki Y: Repeat stereotactic radiosurgery in the
management of brain metastases from non-small cell lung cancer.
Tohoku J Exp Med. 223:125–131. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mariya Y, Sekizawa G, Matsuoka Y, Seki H
and Sugawara T: Outcome of stereotactic radiosurgery for patients
with non-small cell lung cancer metastatic to the brain. J Radiat
Res. 51:333–342. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sperduto CM, Watanabe Y, Mullan J, Hood T,
Dyste G, Watts C, Bender GP and Sperduto P: A validation study of a
new prognostic index for patients with a brain metastases: the
Graded Prognostic Assessment. J Neurosurg. 109(Suppl): 87–89.
2008.PubMed/NCBI
|
|
17
|
Bhatnagar A, Heron DE, Kondziolka D,
Lunsford LD and Flickinger JC: Anaysis of repeat stereotactic
radiosurgery for progressive primary and metastatic CNS tumors. Int
J Radiat Oncol Biol Phys. 53:527–532. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Shaw E, Scott C, Souhami L, Dinapoli R,
Kline R, Loeffler J and Farnan N: Single dose radiosurgical
treatment of recurrent previously irradiated primary brain tumors
and brain metastases: final report of RTOG protocol 90–05. Int J
Radiat Oncol Biol Phys. 47:291–298. 2000.PubMed/NCBI
|
|
19
|
Cox JD, Stetz J and Pajak TF: Toxicity
criteria of the Radiation Therapy Oncology Group (RTOG) and the
European Organization for Research and Treatment of Cancer (EORTC).
Int J Radiat Oncol Biol Phys. 31:1341–1346. 1995. View Article : Google Scholar : PubMed/NCBI
|