Introduction
Desmoplastic fibroma (collagenous fibroma) is a
distinctive, rare, benign, slow-growing fibroblastic soft-tissue
tumor that was first described by Evans in 1995 (1–3). The
gross characteristics of the tumor are well circumscribed, with
spindle to stellate fibroblasts dispersed in a fibromyxoid or
densely fibrous matrix, with low mitotic activity. The condition
was renamed ‘collagenous fibroma’ a year later by Nielson et
al(4). Nielson replaced the
term ‘desmoplastic fibroma’ with ‘collagenous fibroma’, since
desmoplastic fibroma is misleading and suggests that the lesion
consists of immature tumor cells inducing a desmoplastic response
in host tissues. This opinion was consistent with that of Hasegawa
et al(5).
At present, desmoplastic fibroma of the bone is
considered the intraosseous counterpart of common soft-tissue
desmoid tumors or fibromatoses (2,6).
Desmoplastic fibroma of the bone has a male predominance, occurring
two and a half times more often in males than in females, in
individuals between the ages of 50 and 60 years old (7). Wide local resection is the recommended
treatment. Written informed consent was obtained from the
patient.
Case report
A 66-year-old female presented to The Affiliated
Tumor Hospital of Zhengzhou University (Henan, China) with a firm,
immobile, painless and slow-growing mass of the right medial thigh
that had been apparent for seven years. One week prior to
treatment, the mass became intermittently painful and the movement
of the right knee joint was limited. A physical examination
revealed a 10-cm firm, immobile and tender mass in the right medial
thigh. The temperature and color of the local skin of the mass were
normal. The right knee joint was restricted to a 90° flexion, but
the muscle strength and sensation of the lower limbs was normal.
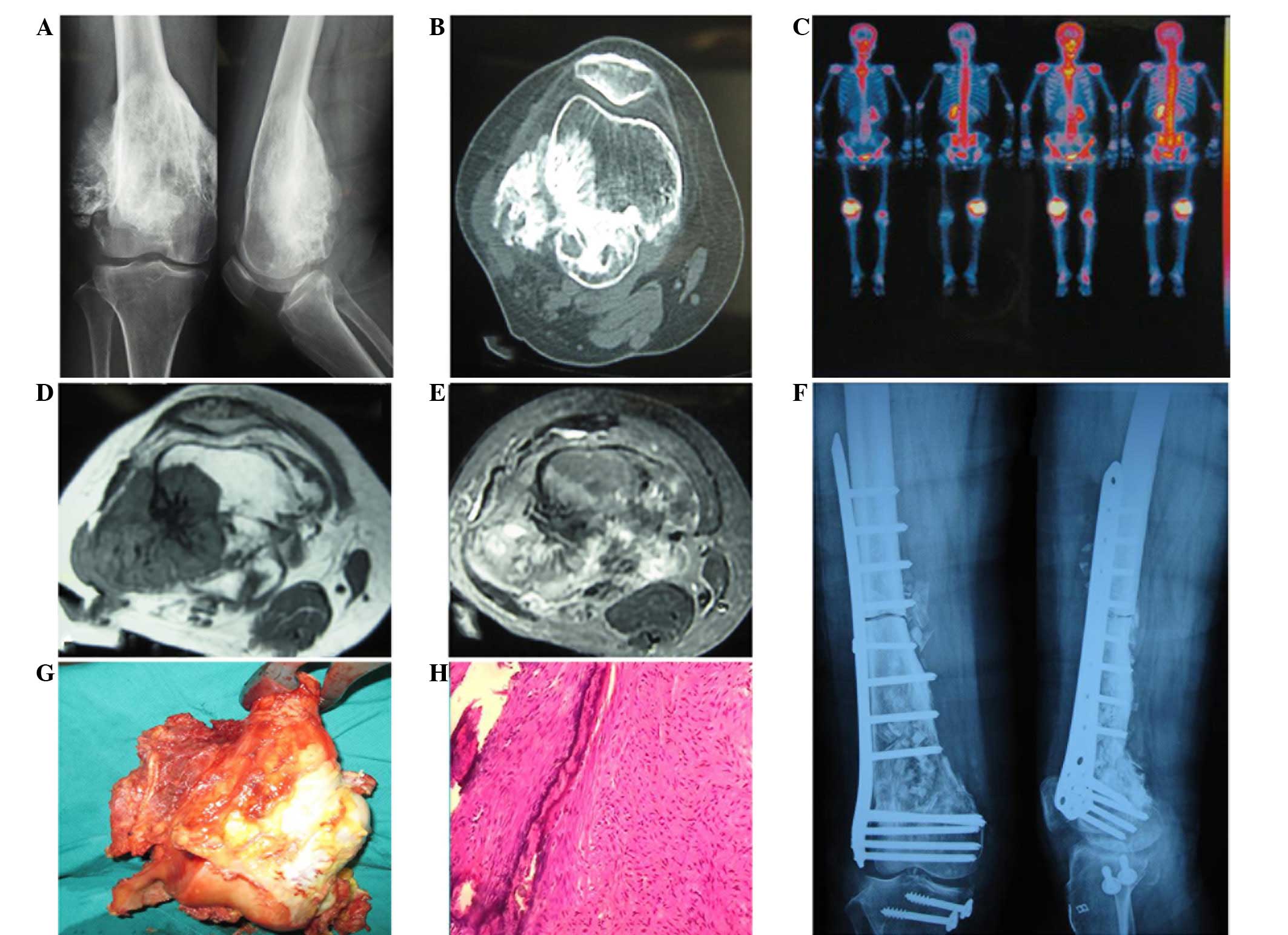
X-rays revealed a high-density lesion of 10 cm in diameter in the
medullary cavity and around the cortical bone of the inferior femur
(Fig. 1A). Computed tomography (CT)
revealed an inhomogeneous soft-tissue mass in the posterolateral
and deep layer of the hamstrings in the right inferior femur.
Calcifications were apparent as multiple small flecks; however,
there was no definite boundary of the calcifications. The lesion
invaded the medullary cavity and the cortical bone (Fig. 1B). Emission-CT (ECT) revealed an
abnormal radioactive distribution as a mass in the right inferior
femur (Fig. 1C). MRI revealed an
irregularly-shaped, expanding lesion in the right inferior femur.
The lesion had a low signal intensity on T1-weighted images, which
was similar to the muscle tissue, and an inhomogeneous hybrid
signal area on T2-weighted images, including a small area of high
signal intensity in the area of low signal intensity (Fig. 1D and E). Bone cortex dissolution and
a periosteal reaction due to new bone formation were detected
locally. A 92×99×96-mm mass was identified in the posterolateral
section of the lesion. The mass adhered to the biceps femoris and
was adjacent to the popliteal artery and vein, but no invasion to
the knee joint cavity was observed. Following an open biopsy, the
mass was confirmed to be a desmoplastic fibroma. The patient
underwent a resection of the tumor and the accompanying bone, which
was then reimplanted using devitalization in vivo,
auto-ilium and homologous allograft bone transplantation, with an
internal fixation by locking the compression plate. This was
followed by a reconstruction of the anterior and posterior cruciate
ligaments and the lateral and medial collateral ligaments under
general anesthesia (Fig. 1F). Gross
examination of the excised specimen revealed a 92×99×96-mm
circumscribed mass involving the majority of the bone and the
adjacent soft tissues of the thigh (Fig. 1G). A microscopic examination
revealed spindle cell and collagen fiber proliferation and collagen
fibers intermixed with spindle cells, with low mitotic activity and
no necrosis in the lesion (Fig.
1H).
Discussion
In 1958, Jaffe (8)
first described desmoplastic fibroma of the bone as a distinct
entity and a kind of osseous fibrous tumor that was previously
unclassified and histologically similar to abdominal desmoid
tumors. Desmoplastic fibroma of the bone is now considered the
intraosseous counterpart of common soft-tissue desmoid tumors or
fibromatoses (6), with a reported
incidence of 0.11–0.13% among primary bone tumors (9). Desmoplastic fibroma is a rare, lytic,
locally aggressive, but non-metastatic benign tumor. Almost any
bone may be affected, but desmoplastic fibroma most often involves
the mandible (22%), femur (15%), pelvic bones (13%), radius (12%)
and tibia (9%) (9). Certain studies
have emphasized that the lesion is osteolytic and does not contain
a significant mineralized matrix, with a favored metaphyseal origin
(10). The metaphysis and
diametaphysis are equally involved, and exclusive diaphyseal
involvement of a tubular bone has been reported as the rarest site
of occurrence (6).
Radiographically, a desmoplastic fibroma is a lytic
tumor. In the long bones, the longest dimension is aligned with the
long axis of the host bone and markedly expands the shaft.
Desmoplastic fibroma usually arises in the metaphysis and may reach
the end of the host bone. The tumor occasionally arises in the
diaphysis and an intraosseous well-defined radiolucent lesion
expansion of the bone, involving the whole circumference or only
part of it, is observed. When the cortex is breached, a soft-tissue
mass may either invade or displace the adjacent muscles. Distinct
periosteal new bone is rare, with the exception of those cases that
are associated with pathological fractures (10). The lesion arising from the center of
the bone has an expanded appearance without any surrounding
periosteal reaction (11). The zone
of transition between the tumor and the normal bone is typically
narrow and well defined, but not sclerotic (12).
In a previous study of desmoplastic fibroma,
cross-sectional imaging revealed a soft-tissue mass in 41% of cases
on CT and in 57% of cases on MRI. The morphological appearance on
the images was that of a relatively slow-growing lesion with focal
aggressive features (6). CT
illustrates the extent of the bone destruction and MRI visualizes
the medullary and soft tissue extent of the tumor (13). CT and MRI are complementary imaging
techniques in cases of suspected desmoplastic fibroma. MRI is
particularly useful and is the preferred imaging modality at
present to delineate desmoplastic fibroma. On MRI, the majority of
soft-tissue masses have a high signal intensity on T2-weighted
images, but in desmoplastic fibroma, T1-weighted images of the mass
exhibit a low signal intensity, while T2-weighted images of the
mass show scattered high-signal areas within a zone of low signal
intensity.
The correlation between MRI and the histological
findings has been described on T2-weighted images; areas of low
signal intensity correspond to abundant collagen fibers and areas
of high signal intensity showing marked enhancement on contrast
T1-images correspond to those areas histologically consisting of
fibroblasts and loose collagen fibers (14). On T1-weighted images, low signal
areas represent areas with low cellularity and abundant collagen
fibers (14).
Desmoplastic fibroma should be diagnosed from other
soft-tissue masses with a low signal intensity on T2-weighted
images, including neurofibroma, cicatricial fibroma, malignant
fibrous histiocytoma, aggressive fibromatosis and calcified masses.
In the absence of calcification, abundant collagen and marked
hypocellularity in a soft-tissue tumor result in a decreased signal
intensity on the T2-weighted pulse sequence (15).
The radiographical appearance of desmoplastic
fibroma is similar to other lytic lesions. The differential
diagnosis includes giant cell tumors, aneurysmal and solitary bone
cysts, hemangioma, fibrous dysplasia, non-ossifying fibroma and
chondromyxoid fibroma. A differentiation should also be made from
primary malignant lesions, including adamantinoma, fibrosarcoma or
metastatic carcinoma.
Histologically, desmoplastic fibroma is similar to a
soft-tissue desmoid tumor. In the present study, a microscopic
examination revealed hypocellular, bland, spindle cell
proliferation, with low mitotic activity and no necrosis. These
cells were associated with a large amount of intercellular collagen
fibers in bundles. The cells and collagen fibers were arranged in a
parallel fashion and in bundles. The lesion exhibited an
infiltrative, destructive pattern with permeation of the bone
marrow spaces, Haversian canals and surrounding soft tissues.
Microscopic infiltrations of the tumor were present beyond the
perceived macroscopic margin.
Evans (3) suggested
that the most significant differential diagnostic consideration was
that of a desmoid tumor, as it may have similar cytological
features and is often locally aggressive. Alberghini et
al(16) reported that
desmoplastic fibroma is a myofibroblastic lesion, ultrastructurally
demonstrating the presence of fibronexus junctions.
Immunohistochemical studies reveal prominent myofibroblastic
differentiation, which typically presents on the cytoplasmic
membranes of the cells, while a desmoid tumor is fibroblastic. This
ultrastructural finding is significant in the differential
diagnosis between a desmoplastic fibroma and a desmoid tumor.
Treatment of desmoplastic fibroma of the bone
includes curettage and intralesional, marginal or wide resection
with or without replacement by allograft, cryosurgery and
amputation in certain cases (17).
Böhm et al(9) studied the
recurrence rate following different methods for the treatment of
desmoplastic fibroma. The recurrence rate (55%) was high in
patients who underwent curettage. By contrast, the recurrence rate
(17%) following the resections was much lower. In 11 of the
patients who underwent wide resections with a minimal follow-up of
three years (mean 6.1 years), no recurrences were reported.
Therefore, wide resection is the ideal treatment for desmoplastic
fibroma (12).
Bertoni et al(18) reported two cases, one in the scapula
and one in the calcaneus, which were treated by thorough curettage
(intralesional excision). The cavity in the calcaneus was
subsequently filled with autogenous cortical grafts. The other four
cases were treated by a wide segmental resection. Of these four
tumors, the one located in the proximal fibula was treated by a
resection only. The tumor in the distal femur required an
endoprosthesis, but subsequently the limb was amputated due to
infection. The tumor of the mid-shaft of the humerus was treated
with a plate and an autogenous cortical graft. The tumor in the
distal fibula was treated with an autogenous cortical graft. In no
case was local recurrence observed during the follow-up. There are
no studies of local recurrence or metastases at present (19,20),
with the longest follow-up time recorded at 12 years. Therefore,
the recommended treatment of collagenous fibroma is local surgical
excision to minimize potential morbidity.
References
|
1
|
Nishio J, Akiho S, Iwasaki H and Naito M:
Translocation t(2;11) is characteristic of collagenous fibroma
(desmoplastic fibroblastoma). Cancer Genet. 204:569–571. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mir-Mari J, Aguirre-Urizar JM,
Berini-Aytés L and Gay-Escoda C: Giant desmoplastic fibroma in the
anterior zone of the maxilla. J Craniofac Surg. 22:2350–2353. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Evans HL: Desmoplastic fibroblastoma. A
report of seven cases. Am J Surg Pathol. 19:1077–1081. 1995.
View Article : Google Scholar
|
|
4
|
Nielsen GP, O’Connell JX, Dickersin GR and
Rosenberg AE: Collagenous fibroma (desmoplastic fibroblastoma): a
report of seven cases. Mod Pathol. 9:781–785. 1996.PubMed/NCBI
|
|
5
|
Hasegawa T, Shimoda T, Hirohashi S, et al:
Collagenous fibroma (desmoplastic fibroblastoma): report of four
cases and review of the literature. Arch Pathol Lab Med.
122:455–460. 1998.PubMed/NCBI
|
|
6
|
Frick MA, Sundaram M, Unni KK, et al:
Imaging findings in desmoplastic fibroma of bone: distinctive T2
characteristics. AJR Am J Roentgenol. 184:1762–1767. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kamata Y, Anazawa U, Morioka H, et al:
Natural evolution of desmoplastic fibroblastoma on magnetic
resonance imaging: a case report. J Med Case Rep. 5:1392011.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jaffe HL: Tumors and Tumorous Conditions
of the Bones and Joints. Lea and Febiger; Philadelphia, PA: pp.
298–303. 1958
|
|
9
|
Böhm P, Kröber S, Greschniok A, et al:
Desmoplastic fibroma of the bone. A report of two patients, review
of the literature and therapeutic implications. Cancer.
78:1011–1023. 1996.PubMed/NCBI
|
|
10
|
Crim JR, Gold RH, Mirra JM, et al:
Desmoplastic fibroma of bone: radiographic analysis. Radiology.
172:827–832. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Godinho FS, Chiconelli JR and Lemos C:
Desmoplastic fibroma of bone. Report of a case. J Bone Joint Surg
Br. 49:560–561. 1967.PubMed/NCBI
|
|
12
|
Abdelwahab IF, Klein MJ, Hermann G, et al:
Osteosarcoma arising in a desmoplastic fibroma of the proximal
tibia. AJR Am J Roentgenol. 178:613–615. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Stefanidis K, Benakis S, Tsatalou E, et
al: Computed tomography and magnetic resonance imaging of
desmoplastic fibroma with simultaneous manifestation in two unusual
locations: a case report. J Med Case Rep. 5:282011. View Article : Google Scholar
|
|
14
|
Shuto R, Kiyosue H, Hori Y, et al: CT and
MR imaging of desmoplastic fibroblastoma. Eur Radiol. 12:2474–2476.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sundaram M, McGuire MH and Schajowicz F:
Soft tissue masses: histologic basis for decreased signal (short
T2) on T2-weighted MR images. AJR Am J Roentgenol. 148:1247–1250.
1987. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Alberghini M, Pasquinelli G, Zanella L, et
al: Desmoplastic fibroblastoma: a light and ultrastructural
description of two cases. Ultrastruct Pathol. 28:149–157. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Rabin D, Ang LC, Megyesi J, et al:
Desmoplastic fibroma of the cranium: case report and review of the
literature. Neurosurgery. 52:950–954. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bertoni F, Calderoni P, Bacchini P and
Campanacci M: Desmoplastic fibroma of bone. A report of six cases.
J Bone Joint Surg Br. 66:265–268. 1984.PubMed/NCBI
|
|
19
|
Shimoyama T, Horie H and Ide F:
Collagenous fibroma (desmoplastic fibroblastoma): a new case
originating in the palate. Dentomaxillofac Radiol. 34:117–119.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Walker KR, Bui-Mansfield LT, Gering SA and
Ranlett RD: Collagenous fibroma (desmoplastic fibroblastoma) of the
shoulder. AJR Am J Roentgenol. 183:17662004. View Article : Google Scholar : PubMed/NCBI
|