|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar
|
|
2
|
Ferlay J, Shin HR, Bray F, Forman D,
Mathers C and Parkin DM: Estimates of worldwide burden of cancer in
2008: GLOBOCAN 2008. Int J Cancer. 127:2893–2917. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yang L: Incidence and mortality of gastric
cancer in China. World J Gastroenterol. 12:17–20. 2006.
|
|
4
|
Hartgrink HH, Jansen EP, van Grieken NC
and van de Velde CJ: Gastric cancer. Lancet. 374:477–490. 2009.
View Article : Google Scholar
|
|
5
|
Wang XN and Liang H: Some problems in the
surgical treatment of gastric cancer. Chin J Cancer. 29:369–373.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Viudez-Berral A, Miranda-Murua C,
Arias-de-la-Vega F, et al: Current management of gastric cancer.
Rev Esp Enferm Dig. 104:134–141. 2012. View Article : Google Scholar
|
|
7
|
Lee JH, Kim KM, Cheong JH and Noh SH:
Current management and future strategies of gastric cancer. Yonsei
Med J. 53:248–257. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wu HL, Tian Q, Peng CW, Liu SP and Li Y:
Multivariate survival and outcome analysis of 154 patients with
gastric cancer at a single Chinese institution. Asian Pac J Cancer
Prev. 12:3341–3345. 2011.PubMed/NCBI
|
|
9
|
Landry CS, Brock G, Scoggins CR, McMasters
KM and Martin RN II: A proposed staging system for gastric
carcinoid tumors based on an analysis of 1,543 patients. Ann Surg
Oncol. 16:51–60. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cammerer G, Formentini A, Karletshofer M,
Henne-Bruns D and Kornmann M: Evaluation of important prognostic
clinical and pathological factors in gastric cancer. Anticancer
Res. 32:1839–1842. 2012.PubMed/NCBI
|
|
11
|
Washington K: 7th edition of the AJCC
cancer staging manual: stomach. Ann Surg Oncol. 17:3077–3079. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sun Z, Wang ZN, Zhu Z, et al: Evaluation
of the seventh edition of American Joint Committee on Cancer TNM
staging system for gastric cancer: results from a Chinese
monoinstitutional study. Ann Surg Oncol. 19:1918–1927. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chae S, Lee A and Lee JH: The
effectiveness of the new (7th) UICC N classification in the
prognosis evaluation of gastric cancer patients: a comparative
study between the 5th/6th and 7th UICC N classification. Gastric
Cancer. 14:166–171. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ahn HS, Lee HJ, Hahn S, et al: Evaluation
of the seventh American Joint Committee on Cancer/International
Union Against Cancer Classification of gastric adenocarcinoma in
comparison with the sixth classification. Cancer. 116:5592–5598.
2010. View Article : Google Scholar
|
|
15
|
Wang W, Sun XW, Li CF, et al: Comparison
of the 6th and 7th editions of the UICC TNM staging system for
gastric cancer: results of a Chinese single-institution study of
1,503 patients. Ann Surg Oncol. 18:1060–1067. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kim SS, Choi BY, Seo SI, et al: The
comparison between 6th and 7th International Union Against
Cancer/American Joint Committee on Cancer Classification for
Survival Prognosis of Gastric Cancer. Korean J Gastroenterol.
58:258–263. 2011.(In Korean).
|
|
17
|
Wang W, Xu DZ, Li YF, et al:
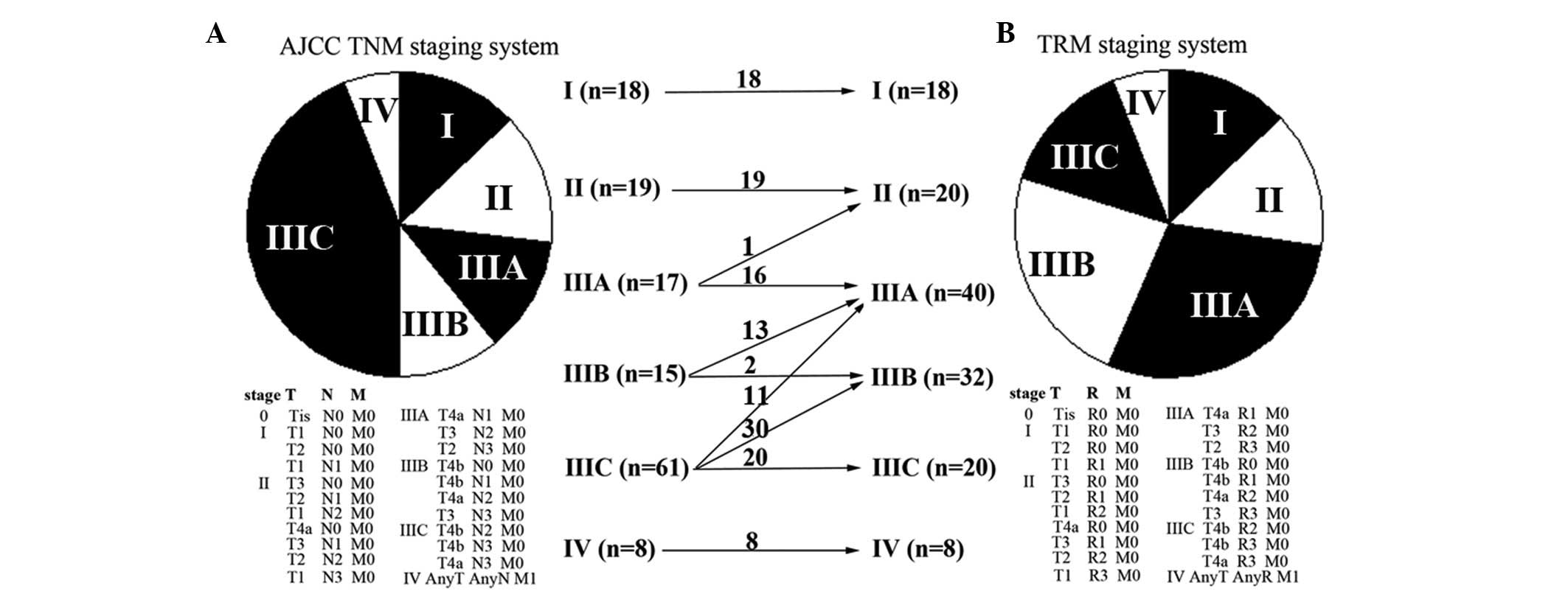
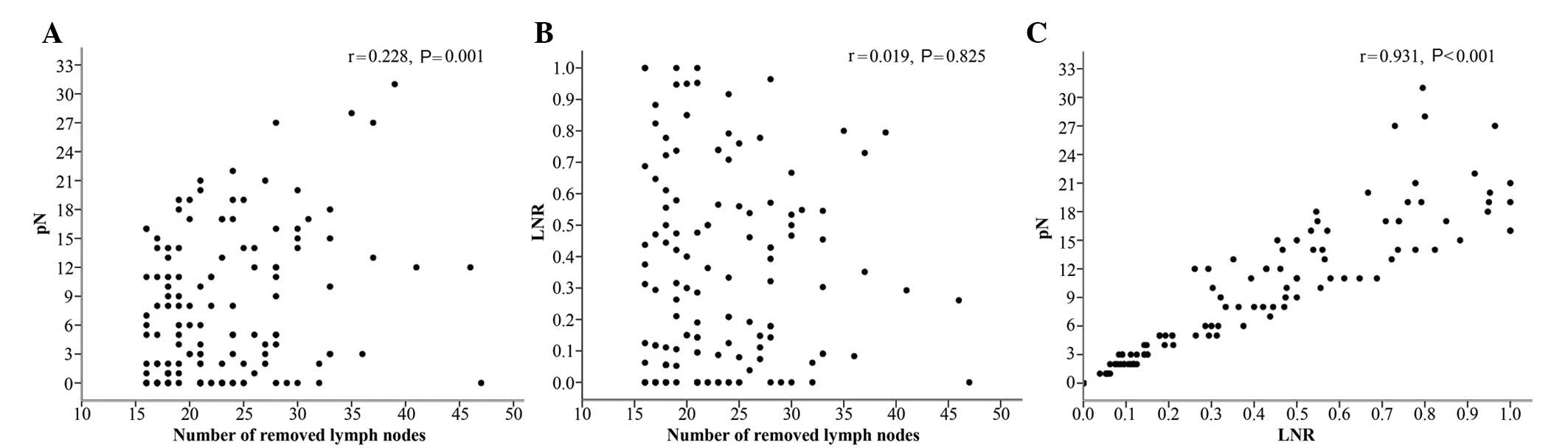
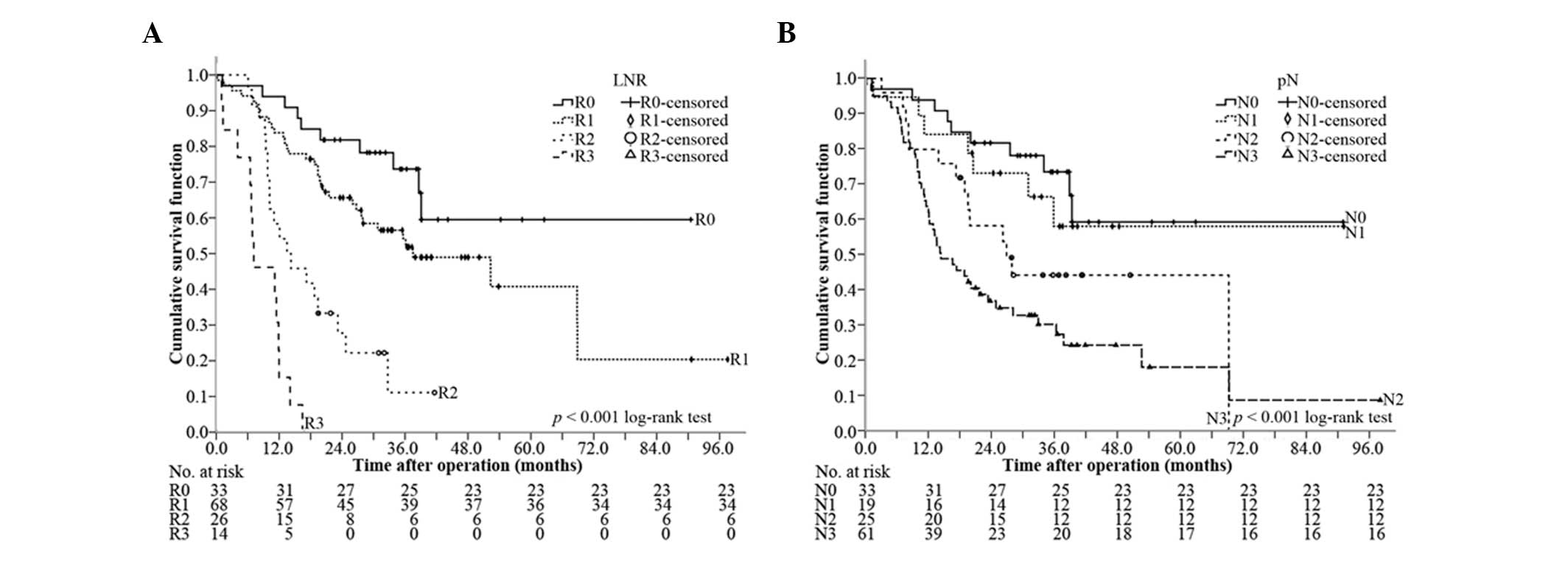
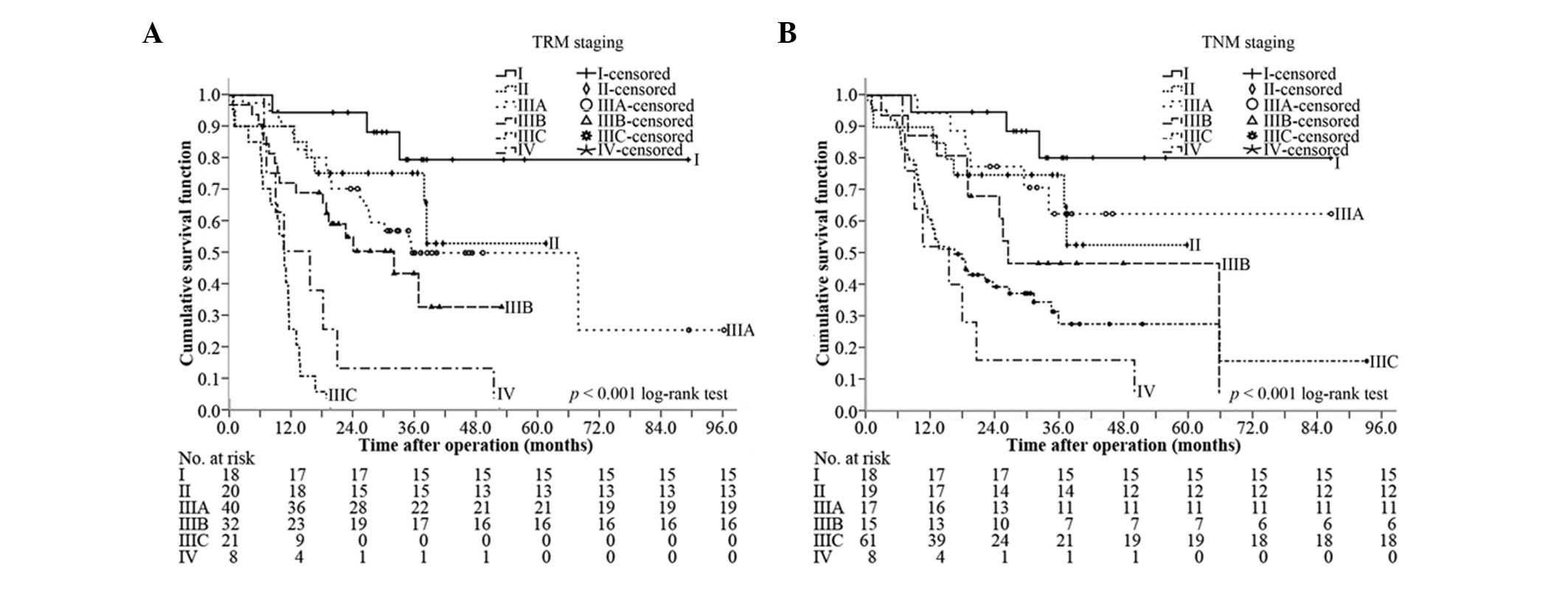
Tumor-ratio-metastasis staging system as an alternative to the 7th
edition UICC TNM system in gastric cancer after D2 resection -
results of a single-institution study of 1343 Chinese patients. Ann
Oncol. 22:2049–2056. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wang J, Dang P, Raut CP, et al: Comparison
of a lymph node ratio-based staging system with the 7th AJCC system
for gastric cancer: analysis of 18,043 patients from the SEER
database. Ann Surg. 255:478–485. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lee SR, Kim HO, Son BH, Shin JH and Yoo
CH: Prognostic significance of the metastatic lymph node ratio in
patients with gastric cancer. World J Surg. 36:1096–1101. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Liu X, Cai H, Shi Y and Wang Y: Prognostic
factors in patients with node-negative gastric cancer: a single
center experience from China. J Gastrointest Surg. 16:1123–1127.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Diaz de Liaño A, Yarnoz C, Aguilar R,
Artieda C and Ortiz H: Rationale for gastrectomy with D2
lymphadenectomy in the treatment of gastric cancer. Gastric Cancer.
11:96–102. 2008.PubMed/NCBI
|
|
22
|
D’Annibale A, Pende V, Pernazza G, et al:
Full robotic gastrectomy with extended (D2) lymphadenectomy for
gastric cancer: surgical technique and preliminary results. J Surg
Res. 166:113–120. 2011.PubMed/NCBI
|
|
23
|
Kim CY and Yang DH: Adjustment of N stages
of gastric cancer by the ratio between the metastatic and examined
lymph nodes. Ann Surg Oncol. 16:1868–1874. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Asoglu O, Karanlik H, Parlak M, et al:
Metastatic lymph node ratio is an independent prognostic factor in
gastric cancer. Hepatogastroenterology. 56:908–913. 2009.PubMed/NCBI
|
|
25
|
Xu DZ, Geng QR, Long ZJ, et al: Positive
lymph node ratio is an independent prognostic factor in gastric
cancer after d2 resection regardless of the examined number of
lymph nodes. Ann Surg Oncol. 16:319–326. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lee SY, Hwang I, Park YS, Gardner J and Ro
JY: Metastatic lymph node ratio in advanced gastric carcinoma: A
better prognostic factor than number of metastatic lymph nodes? Int
J Oncol. 36:1461–1467. 2010.PubMed/NCBI
|
|
27
|
Huang CM, Lin JX, Zheng CH, et al:
Prognostic impact of metastatic lymph node ratio on gastric cancer
after curative distal gastrectomy. World J Gastroenterol.
16:2055–2060. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Feng J, Wu YF, Xu HM, Wang SB and Chen JQ:
Prognostic significance of the metastatic lymph node ratio in T3
gastric cancer patients undergoing total gastrectomy. Asian Pac J
Cancer Prev. 12:3289–3292. 2011.PubMed/NCBI
|
|
29
|
Lemmens V, Dassen AE, van der Wurff A,
Coebergh J and Bosscha K: Lymph node examination among patients
with gastric cancer: variation between departments of pathology and
prognostic impact of lymph node ratio. Eur J Surg Oncol.
37:488–496. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Qiu MZ, Qiu HJ, Wang ZQ, et al: The
tumor-log odds of positive lymph nodes-metastasis staging system, a
promising new staging system for gastric cancer after D2 resection
in China. PLoS One. 7:e317362012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Peng CW, Wang LW, zeng WJ, Yang XJ and Li
Y: Evaluation of the staging system for gastric cancer. J Surg
Oncol. 108:93–105. 2013. View Article : Google Scholar
|