Introduction
Radiofrequency ablation (RFA) has been widely
accepted as an alternative treatment for unresectable primary and
metastatic hepatic tumors (1), as
it achieves a satisfactory local response rate and significantly
improves overall survival rates compared with other modalities,
including chemotherapy or percutaneous ethanol injection (2). However, for patients with small or
solitary hepatic tumors (primary or metastatic), RFA is inferior to
hepatic resectioning with a reduced survival benefit (3–5).
Numerous large series studies have shown that RFA is safe, with a
low mortality rate (0–2%) and a low major complication rate (6–9%)
(2,3).
According to recommendations proposed by the Working
Group on Image-Guided Tumor Ablation, major complications of RFA,
including hollow viscera perforation (0.3%) (6), biliary stenosis and skin burns
(3,7), are life threatening if left untreated,
and likely to lead to substantial morbidity and disability,
hospital admission or substantially longer hospitalization. Major
complications, including diaphragmatic perforation and hernia, have
rarely been previously reported. When the target tumor abuts the
diaphragm, the risk of diaphragmatic thermal injury increases, as
the surgeons are unable to dissect the dome of the liver from the
diaphragm, and overlapping ribs and lungs obscure ultrasonic
visualization. The current case report presents a case of
diaphragmatic hernia with perforation of the incarcerated colon in
the thoracic cavity 12 months following hepatic RFA. Written
informed consent was obtained from the patient.
Case report
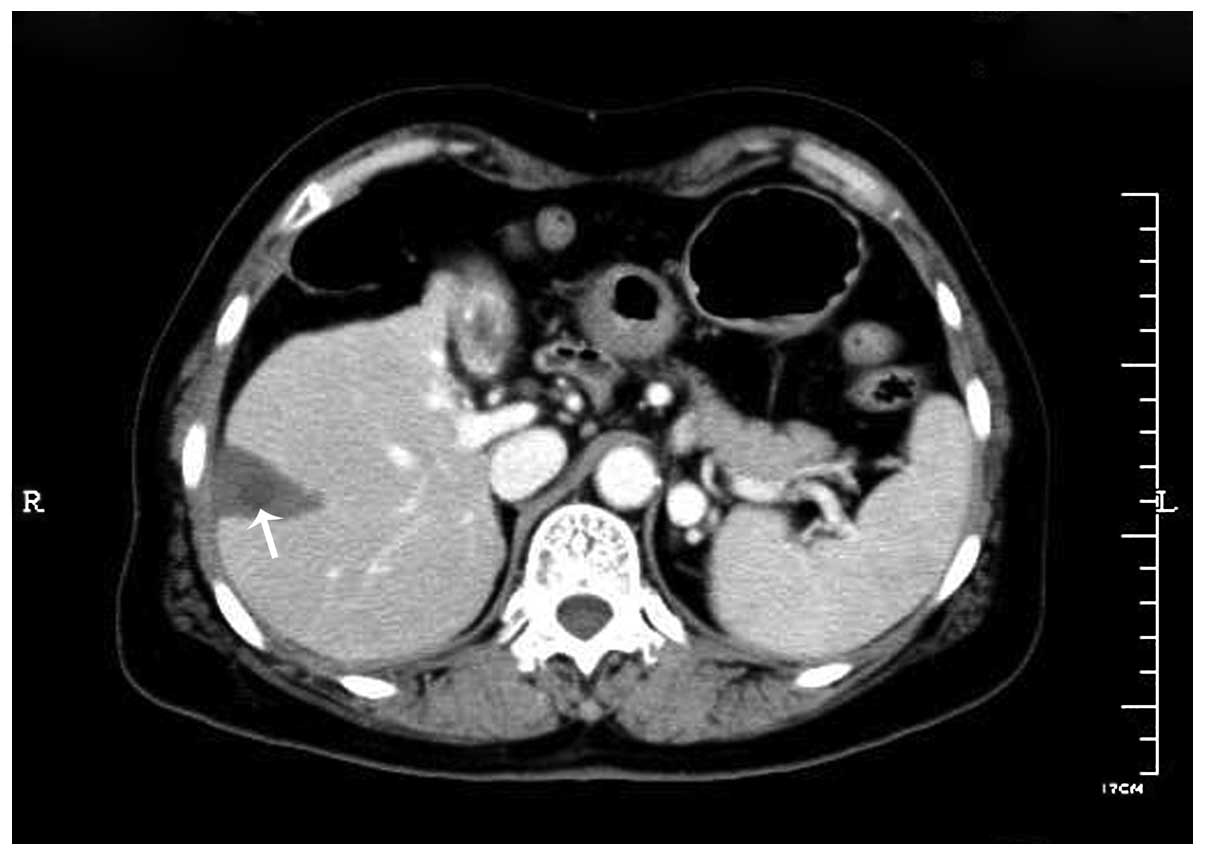
A 61-year-old female was admitted to the Second
Affiliated Hospital of Zhejiang University College of Medicine
(Hangzhou, China) on December 11, 2010, complaining of lower
abdominal pain with nausea, vomiting and constipation. The patient
had a medical history of hypertension, coronary heart disease,
hepatitis B, cirrhosis and hepatic RFA for hepatocellular cancer in
segment VIII of the liver 12 months prior to admission (Fig. 1). During the intervening 12 months,
there was no history of trauma or surgery. An abdominal X-ray
showed an elevation of the right hemidiaphragm and an air-fluid
level in the subphrenic intestine. The patient was initially
diagnosed with an ileus of unknown cause and was managed
conservatively.
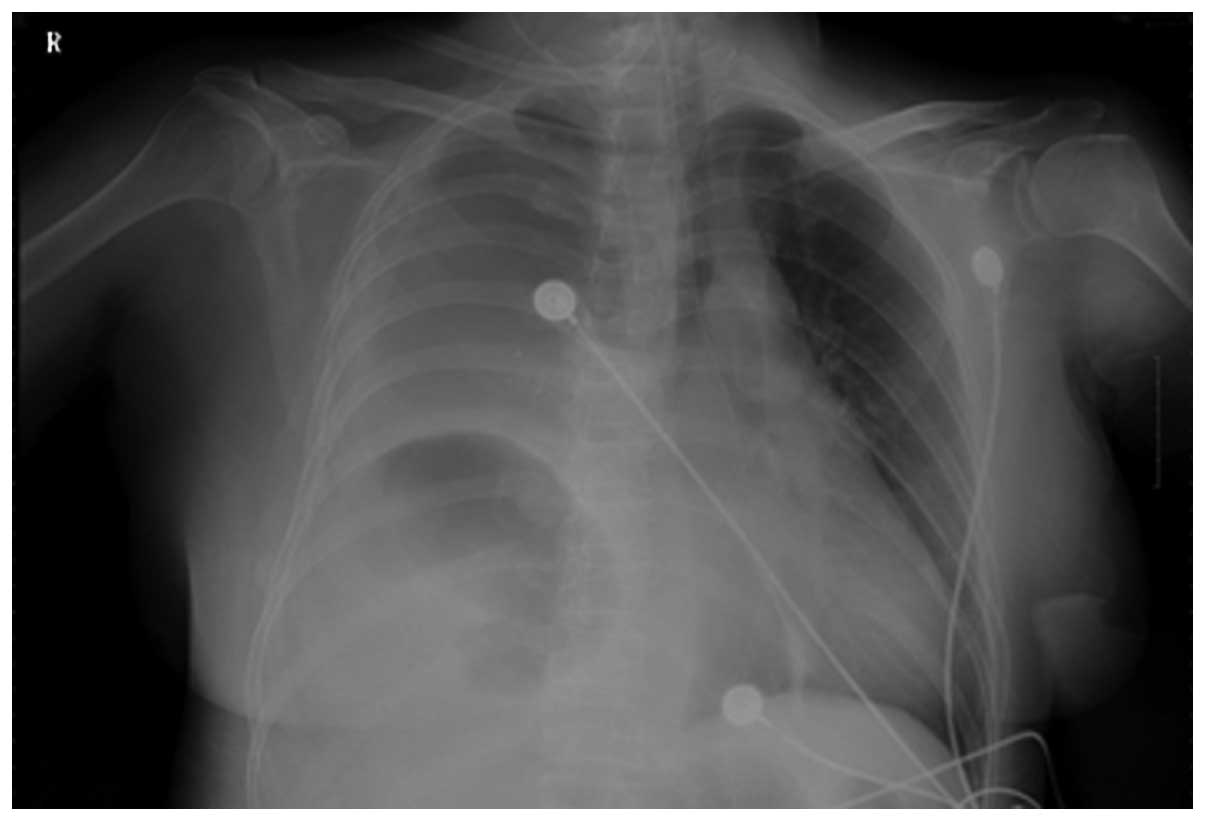
Ten days later, the patient developed respiratory
failure and shock with an onset of acute chest pain and high fever.
The patient was transferred to the ICU for mechanical ventilation
and life support. An emergency chest X-ray revealed a right pleural
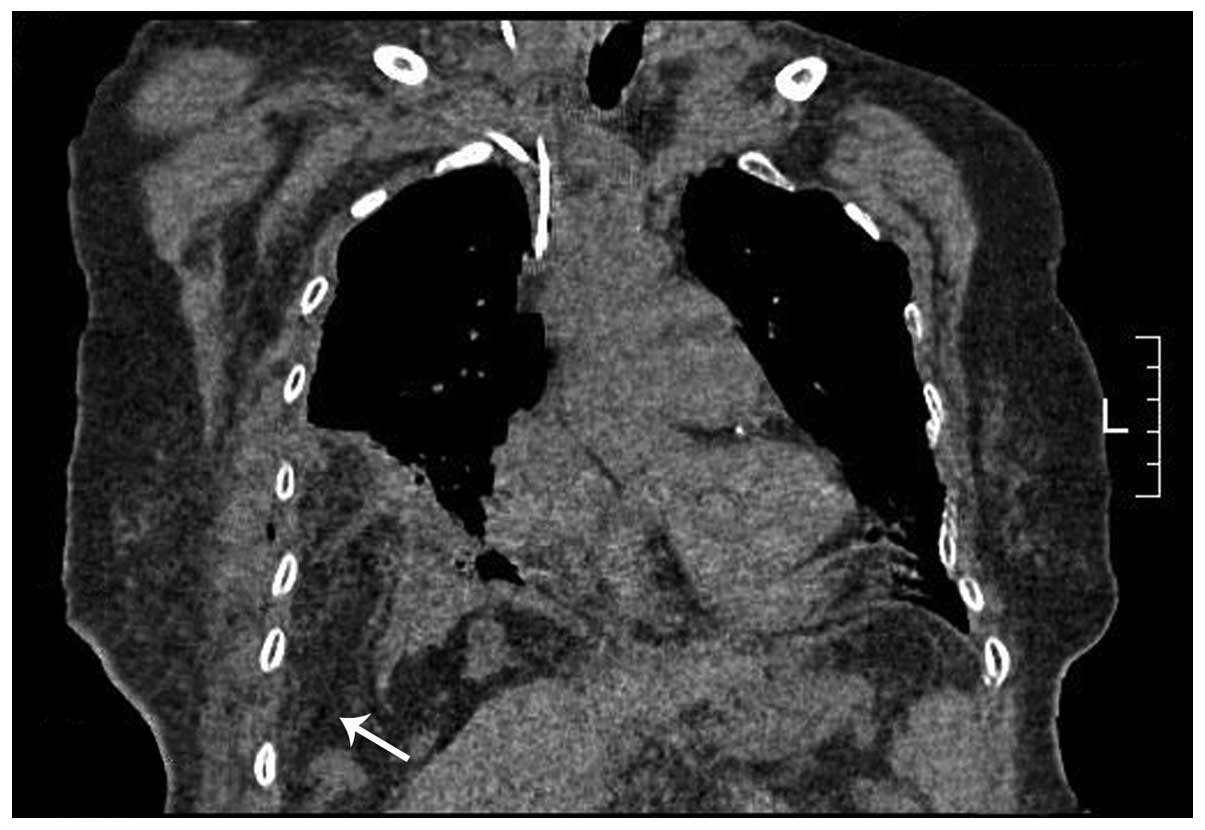
effusion and enlarged bowel in the chest cavity (Fig. 2). Diaphragmatic defect was
visualized by coronal thoracic computed tomography (CT) imaging
(Fig. 3). Closed drainage of the
pleural cavity and antibiotic treatment were administered. Feculent
fluid was drained through a chest tube, indicating that the patient
suffered from a diaphragmatic hernia with incarcerated colon
perforation and pyothorax. Emergency laparotomy was performed and
showed a section of necrotic transverse colon with perforation and
a large quantity of pus in the pleural cavity. It is likely that
infarction and perforation occurred following colon herniation into
the pleural cavity. Following the return of the herniated colon to
the abdomen, a defect in the diaphragm measuring 4 cm in diameter
was found abutting the liver. A spot of thermal focal damage was
located beneath the defect, at the position of the previous RFA
treatment for hepatocellular carcinoma. The perforated diaphragm
was not adherent to the liver, so direct tumor invasion may be
excluded.
In addition, intestinal necrosis was identified 70
cm from the ileocecal valve and the proximal small intestine was
enlarged with gas accumulation. A transverse colectomy with
proximal colostomy, ileum resection with side-to-side anastomosis,
thoracic irrigation and simple suture of the diaphragmatic defect
were completed. The patient recovered well and was discharged from
hospital two months following surgery. Written informed consent was
obtained from the patient for publication of this case report and
the accompanying images.
Discussion
A diaphragmatic hernia is the protrusion of
abdominal structures into the thorax as a result of congenital,
traumatic and iatrogenic defects in the diaphragm. Iatrogenic
defects are not common and may be associated with RFA or abdominal
surgery for organs adjacent to the diaphragm, including the liver,
lung or spleen. Diaphragmatic perforation and herniation are rare
major complications of hepatic RFA. Systematic studies evaluating
the efficacy and safety of RFA for hepatocellular carcinoma
adjacent to the diaphragm or in other hypothesized high-risk
locations have not been described (8–13) and
only eight case reports were found in the previous literature
(14–21). The present case report reviewed a
total of nine reported cases (including the current case) of
diaphragmatic hernia following hepatic RFA (Table I).
 | Table ICharacteristics of nine cases of
diaphragmatic hernia following hepatic RFA. |
Table I
Characteristics of nine cases of
diaphragmatic hernia following hepatic RFA.
| Author (ref) | Year | Age, years | Gender | Tumor size (cm) | Location | Time from RFA to DH
(months) | Treatment |
|---|
| Koda M et
al(14) | 2003 | 61 | F | 2.5 | S8 | 13 | Surgical repair |
| | | | 1 | S8 | | |
| | | | 1.5 | S6 | | |
| Shibuya A et
al(15) | 2006 | 72 | M | 2.8 | S4 and S8 | 34 (18 months
following repeated RFA) | Surgical repair |
| di Francesco F et
al(16) | 2008 | 49 | M | 5.4 | Right lobe | 15 | Surgical repair |
| Nawa T et
al(17) | 2010 | 50 | M | NA | S8 | 20 | Surgical repair
(LS) |
| Pan WD et
al(18) | 2010 | 37 | M | NA | S4 | 5 | Surgical repair
(LS) |
| Boissier F et
al(19) | 2011 | 65 | F | NA | S7 | 7 | Surgical repair and
colectomy |
| | | | | S5 | 1 |
| Singh M et
al(20) | 2011 | 46 | F | 1.5 | S2 and S3 | 19 | Surgical repair
(LS) |
| | | | 1.5 | S5 and S8 | | |
| Yamagami T et
al(21) | 2011 | 71 | F | 2.38 | S7 | 9 | Conservative
treatment |
| Present case | 2011 | 61 | F | 1.5 | S8 | 12 | Surgical repair and
colectomy |
Among the nine cases listed in Table I, the age at diagnosis ranged
between 37–72 years (mean, 56.9 years) and there were five females
and four males. The majority of the primary hepatic tumors were
single lesions measuring ~2 cm in diameter, with the exception of
one tumor of >5 cm (16) in
diameter and multiple lesions were involved in two cases (14,20).
Common locations of targeted lesions were the superior segments in
the right hepatic lobe (S8, S7 and S5) adjacent to the diaphragm.
Treatment details of RFA were not available for every case and in
two cases (14,15), expandable hook-shaped electrodes
were described. Eight cases were performed under ultrasound
guidance and one case was under CT (21). Two cases (15,19)
underwent repeated RFA, with interval times between hepatic RFA and
diaphragmatic herniation ranging between 5–20 months (mean, 13.3
months). The amount of heat delivered to the tumors may be an
additional risk factor, but there have been only two reports of the
use of a peak power of up to 75 (14) and 120 W (21). Early symptoms of ileus, including
nausea, vomiting and intermittent abdominal pain, were present for
a prolonged time in all nine cases and acute chest pain or dyspnea
occurred when abdominal structures suddenly herniated into the
pleural cavity or incarcerated bowel rupture. Only one patient
received conservative treatment without surgery. The remaining
eight patients recovered well following surgical repair (three
cases by laparoscopy) of the diaphragmatic defect with or without
colectomy, and one patient succumbed to hepatic tumor rupture one
month following surgery (14). In
general, two of the nine (22.2%) cases of diaphragmatic hernia
resulted in perforation of the incarcerated colon, respiratory
failure or shock, requiring intensive care treatment followed by
emergency colectomy (19).
Comprehensive analysis of the nine cases
demonstrated specific possibilities leading to diaphragmatic hernia
pursuing diaphragmatic thermal injury following hepatic RFA: Tumor
adjacent to the diaphragm, poor liver function and hepatic
cirrhosis, the use of an expandable type of RFA needle and the
inability to confirm the position of the electrodes, pleural
effusion and other complications with elevated abdominal pressure,
including ascites, ileus and interposition of the intestine between
the liver and diaphragm (Chilaiditi’s sign). The main mechanism of
diaphragmatic hernia associated with RFA is diaphragmatic injury
secondary to thermal or mechanical damage by the needle itself. The
complication is particularly possible if the tumor abuts the
diaphragm (13,14). Mechanical damage caused by the
needle may lead to immediate perforation and thermal damage usually
results in an inflammatory response leading to fibrosis, which
ultimately weakens muscle fibers of the diaphragm and causes the
defect (20). In addition, poor
liver function may prevent the injured tissue from healing
adequately. Complications of hepatic cirrhosis, including ascites
and pleural effusion, may also promote tissue damage (14). The mechanism by which the colon
migrates between the liver and diaphragm (Chilaiditi’s sign) has
not been identified with certainty, but it may occur in patients
with a redundant colon, chronic lung disease (including emphysema)
or liver problems (including cirrhosis and ascites). Chilaiditi’s
sign is generally not associated with symptoms and is most commonly
identified incidentally in normal individuals. However, when
diaphragmatic thermal injury is accompanied with Chilaiditi’s sign,
the latter may facilitate the diagnosis of diaphragmatic
perforation, which may lead to colonic herniation and
strangulation.
To prevent or minimize diaphragmatic thermal injury,
subphrenic artificial ascites (22)
or intraabdominal carbon dioxide insufflation (23) have been indicated as simple and
effective methods to separate the tumor from the diaphragm and to
facilitate ultrasonic visualization, without a clinically confirmed
heat-sink effect (1,22,24).
The early diagnosis of diaphragmatic perforation
following hepatic RFA is often difficult, due to the lack of
sensitivity and specificity of radiographic examination.
Furthermore, diaphragmatic damage or a small perforation with
adherence to the liver may be asymptomatic. Early symptoms,
including nausea, vomiting and chronic abdominal complaints are
often observed (8,16). Nevertheless, diaphragmatic
perforation may remain unidentified unless there is visualization
of abdominal contents herniated into the thoracic cavity and
complicated by ileus with onset of acute dyspnea or chest pain
(19). Elevation of serum markers,
including CPK, LDH isoenzymes and AST, may be of value in
identifying diaphragmatic muscle damage. A diaphragmatic hernia may
be managed by thoracotomy or laparotomy (8). The diaphragmatic defect must be
repaired and reinforced by a prosthetic mesh or closed only by
suturing (8,15,16,18).
If there is necrosis or perforation of incarcerated bowel, bowel
resection is required and antibiotic treatment of pyothorax must be
initiated.
In conclusion, this case report described a case of
diaphragmatic hernia with perforation of the incarcerated colon in
the thoracic cavity 12 months following hepatic RFA, and reviewed
nine previously reported cases of diaphragmatic hernia. The early
diagnosis of diaphragmatic perforation or hernia following hepatic
RFA is often difficult. Clinicians must be aware of diaphragmatic
thermal damage following hepatic RFA for liver tumors adjacent to
the diaphragm, particularly for patients with symptoms of ileus,
dyspnea, chest pain, pleural effusion and right shoulder pain.
Radiologists must be aware of the integrity of the diaphragm to
achieve early diagnosis of diaphragmatic perforation or hernia. We
suggest that surgical repair must be performed once the
diaphragmatic defect has been identified in order to avoid a
diaphragmatic hernia complicated with acute intestinal obstruction
or perforation, which may be lethal without immediate
treatment.
References
|
1
|
Nam SY, Rhim H, Kang TW, et al:
Percutaneous radiofrequency ablation for hepatic tumors abutting
the diaphragm: clinical assessment of the heat-sink effect of
artificial ascites. AJR Am J Roentgenol. 194:W227–W231. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tiong L and Maddern GJ: Systematic review
and meta-analysis of survival and disease recurrence after
radiofrequency ablation for hepatocellular carcinoma. Br J Surg.
98:1210–1224. 2011. View
Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wong SL, Mangu PB, Choti MA, et al:
American Society of Clinical Oncology 2009 clinical evidence review
on radiofrequency ablation of hepatic metastases from colorectal
cancer. J Clin Oncol. 28:493–508. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wu YZ, Li B, Wang T, et al: Radiofrequency
ablation vs hepatic resection for solitary colorectal liver
metastasis: a meta-analysis. World J Gastroenterol. 17:4143–4148.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gravante G, Overton J, Sorge R, et al:
Radiofrequency ablation versus resection for liver tumours: an
evidence-based approach to retrospective comparative studies. J
Gastrointest Surg. 15:378–387. 2011. View Article : Google Scholar
|
|
6
|
Livraghi T, Solbiati L, Meloni MF, et al:
Treatment of focal liver tumors with percutaneous radio-frequency
ablation: complications encountered in a multicenter study.
Radiology. 226:441–451. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Goldberg SN, Charboneau JW, Dodd GD III,
et al; International Working Group on Image-Guided Tumor Ablation.
Image-guided tumor ablation: proposal for standardization of terms
and reporting criteria. Radiology. 228:335–345. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tang Z, Fang H, Kang M, et al:
Percutaneous radiofrequency ablation for liver tumors: Is it safer
and more effective in low-risk areas than in high-risk areas?
Hepatol Res. 41:635–640. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kang TW, Rhim H, Kim EY, et al:
Percutaneous radiofrequency ablation for the hepatocellular
carcinoma abutting the diaphragm: assessment of safety and
therapeutic efficacy. Korean J Radiol. 10:34–42. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Teratani T, Yoshida H, Shiina S, et al:
Radiofrequency ablation for hepatocellular carcinoma in so-called
high-risk locations. Hepatology. 43:1101–1108. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kim YJ, Raman SS, Yu NC, et al:
Radiofrequency ablation of hepatocellular carcinoma: can
subcapsular tumors be safely ablated? AJR Am J Roentgenol.
190:1029–1034. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sartori S, Tombesi P, Macario F, et al:
Subcapsular liver tumors treated with percutaneous radiofrequency
ablation: a prospective comparison with nonsubcapsular liver tumors
for safety and effectiveness. Radiology. 248:670–679. 2008.
View Article : Google Scholar
|
|
13
|
Head HW, Dodd GD III, Dalrymple NC, et al:
Percutaneous radiofrequency ablation of hepatic tumors against the
diaphragm: frequency of diaphragmatic injury. Radiology.
243:877–884. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Koda M, Ueki M, Maeda N and Murawaki Y:
Diaphragmatic perforation and hernia after hepatic radiofrequency
ablation. AJR Am J Roentgenol. 180:1561–1562. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Shibuya A, Nakazawa T, Saigenji K, et al:
Diaphragmatic hernia after radiofrequency ablation therapy for
hepatocellular carcinoma. AJR Am J Roentgenol. 186(Suppl 5):
S241–S243. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
di Francesco F, di Sandro S, Doria C, et
al: Diaphragmatic hernia occurring 15 months after percutaneous
radiofrequency ablation of a hepatocellular cancer. Am Surg.
74:129–132. 2008.PubMed/NCBI
|
|
17
|
Nawa T, Mochizuki K, Yakushijin T, et al:
A patient who developed diaphragmatic hernia 20 months after
percutaneous radiofrequency ablation for hepatocellular carcinoma.
Nihon Shokakibyo Gakkai Zasshi. 107:1167–1174. 2010.(In
Japanese).
|
|
18
|
Pan WD, Zhang JS, Hu PK, Lin Z, Li K and
Xu RY: Delayed diaphragmatic hernia after radiofrequency ablation
for hepatocellular carcinoma: case report and review of the
literature. Zhongguo Wuzhen Xue Zazhi. 31:76922010.
|
|
19
|
Boissier F, Labbé V, Marchetti G, et al:
Acute respiratory distress and shock secondary to complicated
diaphragmatic hernia. Intensive Care Med. 37:725–726. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Singh M, Singh G, Pandey A, et al:
Laparoscopic repair of iatrogenic diaphragmatic hernia following
radiofrequency ablation for hepatocellular carcinoma. Hepatol Res.
41:1132–1136. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yamagami T, Yoshimatsu R, Matsushima S, et
al: Diaphragmatic hernia after radiofrequency ablation for
hepatocellular carcinoma. Cardiovasc Intervent Radiol. 34(Suppl 2):
S175–S177. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Rhim H, Lim HK, Kim YS and Choi D:
Percutaneous radiofrequency ablation with artificial ascites for
hepatocellular carcinoma in the hepatic dome: initial experience.
AJR Am J Roentgenol. 190:91–98. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Raman SS, Aziz D, Chang X, et al:
Minimizing diaphragmatic injury during radiofrequency ablation:
efficacy of intraabdominal carbon dioxide insufflation. AJR Am J
Roentgenol. 183:197–200. 2004. View Article : Google Scholar
|
|
24
|
Kim YS, Rhim H, Choi D and Lim HK: Does
artificial ascites induce the heat-sink phenomenon during
percutaneous radiofrequency ablation of the hepatic subcapsular
area?: an in vivo experimental study using a rabbit model.
Korean J Radiol. 10:43–50. 2009. View Article : Google Scholar : PubMed/NCBI
|